Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6333
Peer-review started: February 9, 2022
First decision: March 23, 2022
Revised: March 24, 2022
Accepted: April 22, 2022
Article in press: April 22, 2022
Published online: June 26, 2022
Sporadic Creutzfeldt-Jakob disease (sCJD) is a prion disease characterized as a fatal transmissible neurodegenerative disorder. Dizziness is often the first pre
A 76-year-old man presented with bilateral sudden hearing impairment and dizziness for 10 d. He was taking medications for hypertension and diabetes. He denied any difficulty with activities of daily living or hearing impairment before the onset of symptoms. Pure tone audiometry showed bilateral severe hearing impairment. Brain magnetic resonance imaging (MRI) and laboratory tests were within normal limits. Given his diagnosis of sudden sensory hearing loss, the patient received corticosteroid treatment but it was ineffective. Two weeks later, he complained of aggravated gait impairment, disorientation, and cognitive impairment. Repeat brain MRI showed diffuse cortical high signal intensities on diffusion-weighted imaging. In cerebrospinal fluid analysis, the real-time quaking-induced conversion assay was positive, and 14-3-3 protein was detected in the by western blotting. Considering all the data, we diagnosed probable sCJD, and the patient’s symptoms rapidly progressed into akinetic mutism.
For patients with abrupt bilateral hearing impairment, especially in the elderly, various differential diagnoses, including sCJD, should be considered.
Core Tip: Hearing impairment as an initial manifestation of Creutzfeldt-Jakob disease is rare. However, it should be regarded as a differential diagnosis in an elderly patient with bilateral hearing impairment unresponsive to standard corticosteroid treatment. Repeat brain imaging including diffusion-weighted imaging and cerebrospinal fluid analysis will be helpful for diagnosis.
- Citation: Na S, Lee SA, Lee JD, Lee ES, Lee TK. Creutzfeldt-Jakob disease presenting with bilateral hearing loss: A case report. World J Clin Cases 2022; 10(18): 6333-6337
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6333.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6333
Sporadic Creutzfeldt-Jakob disease (sCJD) is a prion disease characterized as a fatal transmissible neurodegenerative disorder[1]. The key features of sCJD are rapidly progressive dementia and diverse symptoms including myoclonus, pyramidal and extrapyramidal symptoms, cerebellar disturbance, visual symptoms, and akinetic mutism. Among them, it is known that the most commonly reported presenting symptom is cognitive decline. In other presentations, dizziness is also often the first presenting symptom of sCJD, but hearing loss as an early manifestation is very rare[2]. Herein, we report a case of acute bilateral sensorineural hearing loss as the first manifestation of sCJD.
A 76-year-old man presented with bilateral sudden hearing impairment and dizziness for 10 d.
The hearing impairment first developed on the left side and then rapidly progressed to bilateral. He also reported dizziness that was aggravated by positional changes and accompanied by a slight gait imbalance, but he could walk without assistance.
He was taking medications for hypertension and diabetes for over ten years. He denied any difficulty with activities of daily living or hearing impairment before the onset of symptoms.
No special history of personal and family.
The patient revealed no spontaneous nystagmus or gaze-evoked nystagmus. The bedside head impulse test was unremarkable. The other cranial nerves were unremarkable, and there was no limb ataxia.
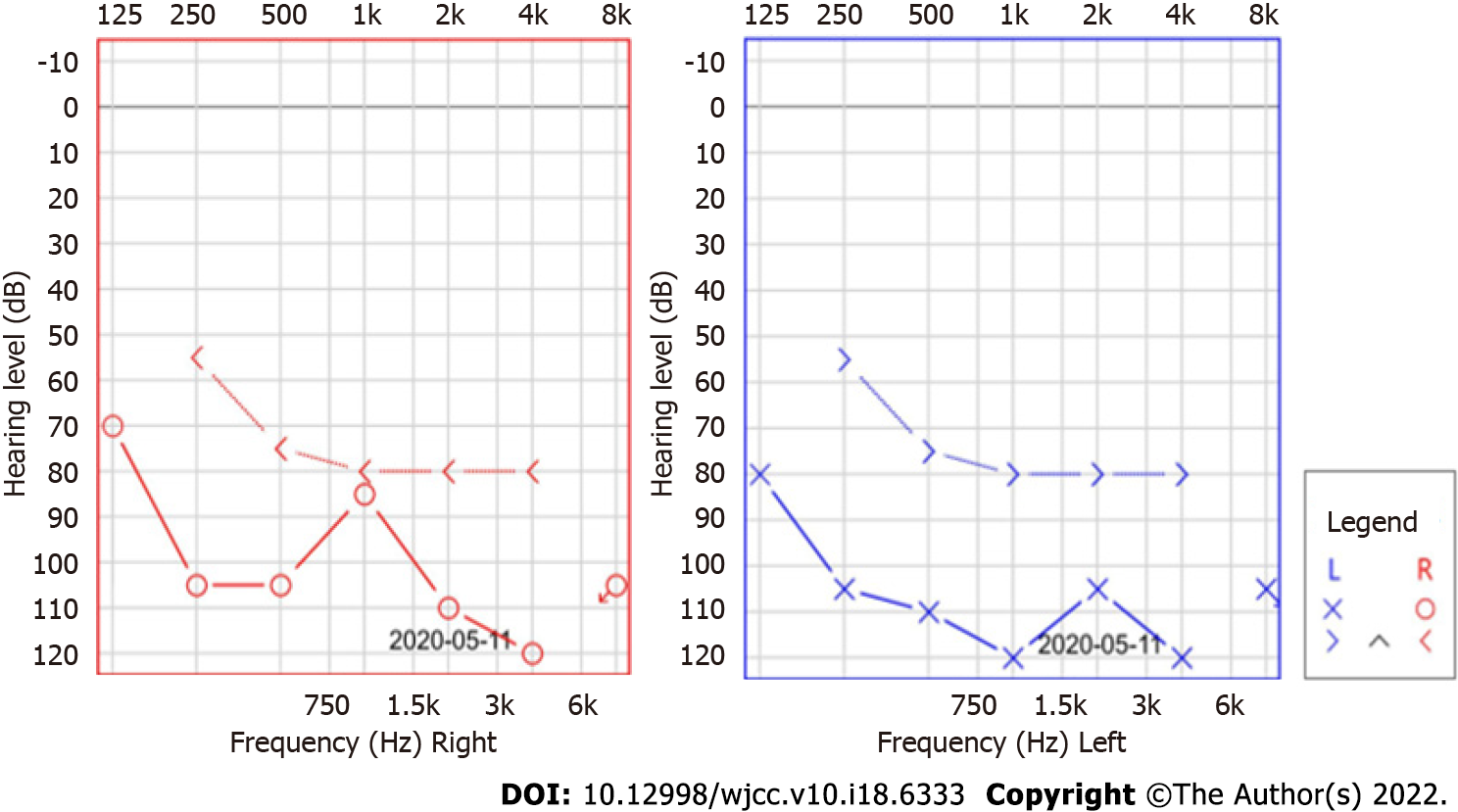
Laboratory tests including routine blood tests, autoimmune studies, thyroid function tests, and antibodies of the paraneoplastic syndrome were unremarkable except for an HbA1c of 8.1% and hyperglycemia. Pure tone audiometry (PTA) showed bilateral severe hearing impairment (Figure 1).
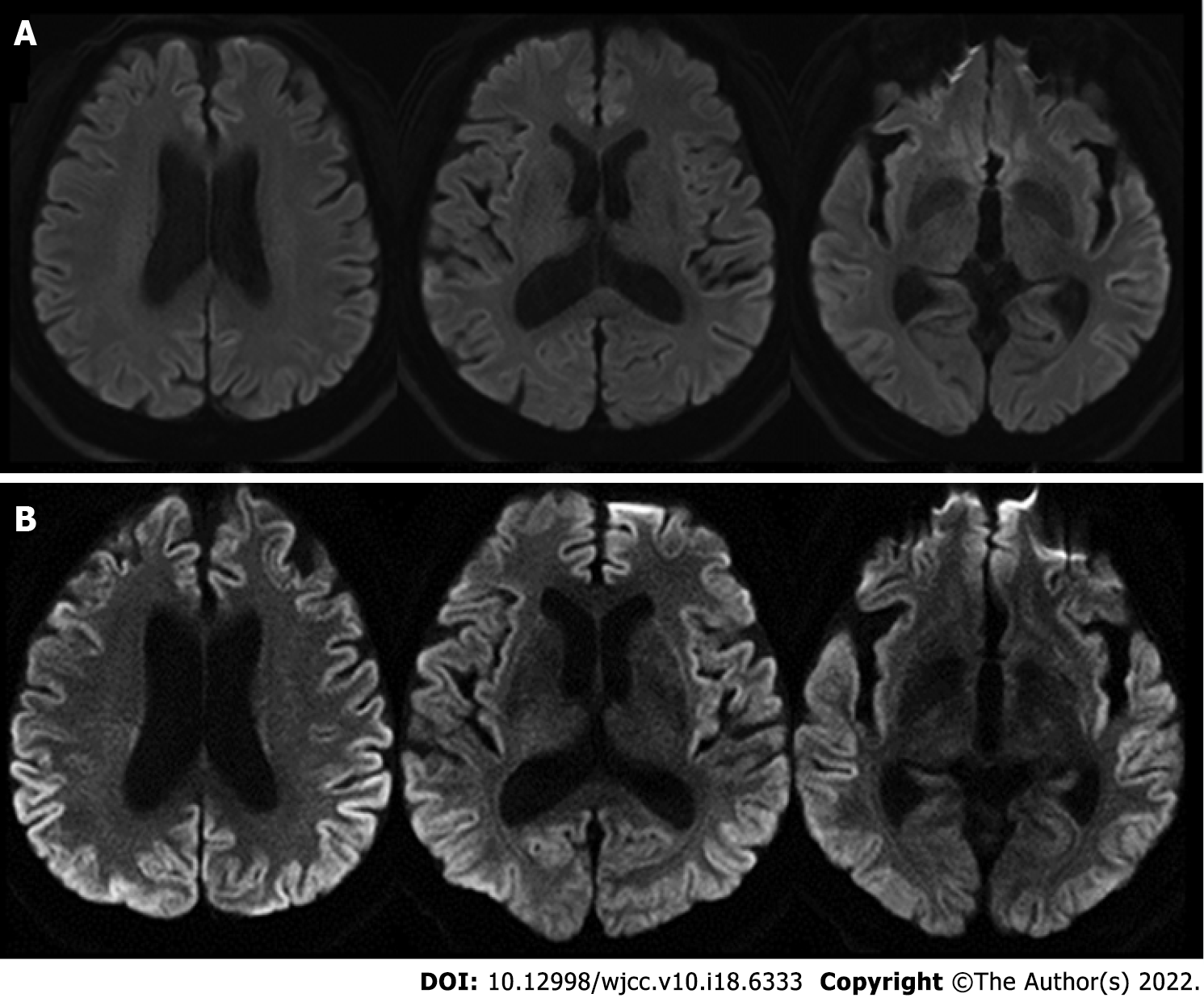
Brain magnetic resonance imaging (MRI) was within normal limits (Figure 2A).
Given his diagnosis of sudden sensory hearing loss, the patient received corticosteroid treatment (prednisolone 60 mg/d for 10 d and tapering) but it was ineffective. Two weeks later, however, he complained of aggravated gait impairment, word-finding difficulty, disorientation, and cognitive impairment. Repeat brain MRI showed high signal intensities in the frontal, temporal, parietal, and occipital cortices on diffusion-weighted imaging (Figure 2B). Cerebrospinal fluid (CSF) analysis re
Considering all the data, we diagnosed probable sCJD. The amended diagnostic criteria added that the combination of cognitive decline, positive CSF RT-QuIC, and one or more typical CJD symptoms can draw the diagnosis of probable sCJD[3]. Because he had never undertaken neurosurgery dealing with a dura mater and the genetic analysis revealed that there was no mutation or polymorphism of the prion gene, we excluded the possibility of familial CJD or iatrogenic CJD. Moreover, our patient revealed a positive RT-QuIC test and met the criteria of probable sCJD.
Because of the characteristics of sCJD, the intractable rapidly progressive dementia[1], he received conservative care.
The patient’s symptoms rapidly progressed into akinetic mutism within only two months after the onset of bilateral hearing impairment.
This patient presented with an abrupt onset of bilateral hearing impairment and dizziness as the first manifestation of sCJD. Although he only complained of otologic symptoms and was diagnosed initially with bilateral sensorineural hearing loss, the patient then developed additional neurologic symptoms including cognitive decline and prominent gait imbalance, which rapidly progressed. The amended diagnostic criteria of sCJD area that the combination of positive CSF RT-QuIC and progressive cognitive impairment or any of typical CJD symptoms can draw the diagnosis of probable sCJD[3]. Our patient revealed a positive RT-QuIC test and met the criteria of probable sCJD. The possibilities of familial or iatrogenic CJD were excluded because there was no mutation or polymorphism of the prion gene and he had no history of epidemiological evidence. Although the etiology of sCJD has been unknown, many researchers assumed that the prion disease might be initiated by the stochastic misfolded cellular prion protein or mutations in the prion protein gene at ongoing neurogenesis areas[4].
Hearing impairment as an early symptom of sCJD has been described in a few reports[5,6]. Those patients were elderly, older than 65 years, and first complained of only suddenly developed bilateral hearing impairment and subjective unsteadiness. Our patient’s hearing loss were also bilateral and unresponsive to steroid treatment. Postmortem studies in sCJD have revealed that the prion protein deposition in the brainstem is symmetrical and starts in the early stage of sCJD[7]. These neuropathologic characteristics account for the bilaterality of the hearing impairment in patients with sCJD.
The authors of a previous report conducted a brain MRI at the initial presentation, and it was within normal limit[5]. Our patient showed imaging findings that reflected his complaints and symptoms of sCJD. At his first visit when he complained of only hearing impairment and vague dizziness, the brain MRI was unremarkable. After other symptoms developed, however, repeat brain MRI revealed characteristic high signal intensities of the bilateral cerebral cortices, which were a clue for the diagnosis of sCJD.
Among the presenting symptoms of our patient, the dizziness was nonspecific and vague, but the hearing impairment was abrupt and very severe. Furthermore, the hearing difficulty was broad, from low to high frequency. When a patient with cognitive decline is suspected of having hearing difficulty, an appropriate evaluation is difficult because laboratory tests, such as pure tone audiometry, cannot be obtained without patient cooperation, and an accurate history of onset time and the pattern of the hearing impairment is needed. In sCJD, the most common presenting symptom is cognitive decline[3]. Thus, even if hearing impairment occurs in the early stage of sCJD, evaluations for the presence of hearing symptoms and otologic function under rapidly progressive cognitive decline are difficult. In our patient, however, the history of hearing impairment and the result of PTA were reliable because the patient did not complain of cognitive impairment at presentation.
The patient presented with sudden onset hearing impairment and dizziness, followed by progressive cognitive impairment and confusion. Repeat brain MRI revealed characteristic findings of sCJD, and the RT-QuIC test was positive. For patients with abrupt bilateral hearing impairment, especially in the elderly, various differential diagnoses, including sCJD, should be considered. Moreover, when sCJD is suspected, close follow-up with thorough history taking and neurologic examinations and repeated workups that include brain diffusion-weighted imaging and CSF analysis will be helpful.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Korean Neurological Association.
Specialty type: Clinical neurology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang YJ, China; Xie Q, China S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Collins SJ, Lawson VA, Masters CL. Transmissible spongiform encephalopathies. Lancet. 2004;363:51-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 187] [Cited by in F6Publishing: 192] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 2. | Rabinovici GD, Wang PN, Levin J, Cook L, Pravdin M, Davis J, DeArmond SJ, Barbaro NM, Martindale J, Miller BL, Geschwind MD. First symptom in sporadic Creutzfeldt-Jakob disease. Neurology. 2006;66:286-287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 104] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Hermann P, Laux M, Glatzel M, Matschke J, Knipper T, Goebel S, Treig J, Schulz-Schaeffer W, Cramm M, Schmitz M, Zerr I. Validation and utilization of amended diagnostic criteria in Creutzfeldt-Jakob disease surveillance. Neurology. 2018;91:e331-e338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 59] [Article Influence: 9.8] [Reference Citation Analysis (1)] |
| 4. | Iacono D, Ferrari S, Gelati M, Zanusso G, Mariotto S, Monaco S. Sporadic Creutzfeldt-Jakob Disease: Prion Pathology in Medulla Oblongata-Possible Routes of Infection and Host Susceptibility. Biomed Res Int. 2015;2015:396791. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Bigelow DC, Eisen MD, Yen DM, Saull SC, Solomon D, Schmidt DE. Otolaryngological manifestations of Creutzfeldt-Jakob disease. Arch Otolaryngol Head Neck Surg. 1998;124:707-710. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Salazar R, Cerghet M, Ramachandran V. Bilateral hearing loss heralding sporadic Creutzfeldt-Jakob disease: a case report and literature review. Otol Neurotol. 2014;35:1327-1329. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Iwasaki Y, Hashizume Y, Yoshida M, Kitamoto T, Sobue G. Neuropathologic characteristics of brainstem lesions in sporadic Creutzfeldt-Jakob disease. Acta Neuropathol. 2005;109:557-566. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |