Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6319
Peer-review started: January 15, 2022
First decision: April 8, 2022
Revised: April 10, 2022
Accepted: April 24, 2022
Article in press: April 24, 2022
Published online: June 26, 2022
Processing time: 152 Days and 16.4 Hours
Trauma is a common cause of pancreatic duct disruption. Surgical treatment is recommended in current clinical guidelines for adult pancreatic injury because non-surgical treatments have higher risks of serious complications or even death compared with surgical treatment.
A 22-year-old woman was admitted to Tiantai People’s Hospital of Zhejiang Province after 1-h duration of abdominal pain and distension following trauma. The diagnosis was “traumatic pancreatic rupture”. The patient’s symptoms were not severe, her vital signs were stable, and signs of peritonitis were not obvious. Therefore, conservative treatment could be considered, with the possibility of emergency surgery if necessary. After 2 mo of conservative treatment with duct drainage, the pancreatic duct healed spontaneously with no significant complications.
We report a case of pancreatic duct disruption in the head and neck caused by trauma that was treated conservatively and healed spontaneously, providing a new choice for clinical practice. For isolated pancreatic injury with rupture of the pancreatic duct in the head and neck, conservative treatment under close obse
Core Tip: In this study, we report a case of pancreatic duct disruption in the head and neck caused by trauma that was treated conservatively and which healed spontaneously, providing a new basis for clinical practice. For isolated pancreatic injury with rupture of the pancreatic duct in the head and neck, conservative treatment under close observation is feasible.
- Citation: Mei MZ, Ren YF, Mou YP, Wang YY, Jin WW, Lu C, Zhu QC. Spontaneous healing after conservative treatment of isolated grade IV pancreatic duct disruption caused by trauma: A case report. World J Clin Cases 2022; 10(18): 6319-6324
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6319.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6319
Trauma is a common cause of pancreatic duct disruption. Surgical treatment is recommended in current clinical guidelines for adult pancreatic injury because, compared with surgical treatment, non-surgical treatments have higher risks of serious complications or even death[1,2]. In this study, we report a case of pancreatic duct disruption in the head and neck caused by trauma that was treated conservatively and which healed spontaneously.
A 22-year-old female patient was admitted to Tiantai People’s Hospital of Zhejiang Province on 13 July 2020 after 1-hour duration of abdominal pain and distension following trauma.
The patient experienced sudden-onset persistent and unbearable abdominal pain, radiating to the lower back, with abdominal distension and nausea, and without vomiting, coma, dizziness, headache, chest tightness, shortness of breath, bloody vomiting, or hemoptysis. The trauma resulted from impact with bicycle handlebars on the upper abdomen during an electrical bicycle accident 1 h earlier.
She had no other complaints. Her sleep and appetite were normal, and her excretion and egestion were both normal.
The patient had an unremarkable medical history.
The patient grew up in her locality, denied any contact with contaminated water or radiation exposure, and did not smoke or consume alcohol. She had no gestational history, and her annual menstruation cycle was 13/year (q 4-6 wk/duration: 20-30 d).
Physical examination findings on admission: body temperature: 37.2 ℃, respiratory rate: 20 breaths/min, blood pressure: 118/63 mmHg, and heart rate: 103 beats/min. The patient had a clear mind, low mood, flat and soft abdomen, tenderness in the upper abdomen, no obvious rebound pain, bowel sounds: 2/min, and no shifting dullness. No other significant abnormalities were observed.
Serum amylase concentration: 1258 U/L (upper limit of normal: 135 U/L), white blood cell count: 17.8 × 109/L, neutrophils: 82%, red blood cell count: 4.51 × 1012/L, hemoglobin: 143 g/L, platelet count: 211 × 109/L, C-reactive protein: < 0.499 mg/L, and procalcitonin: < 0.02 ng/mL; liver and kidney function was normal, the levels of plasma lactate was normal.
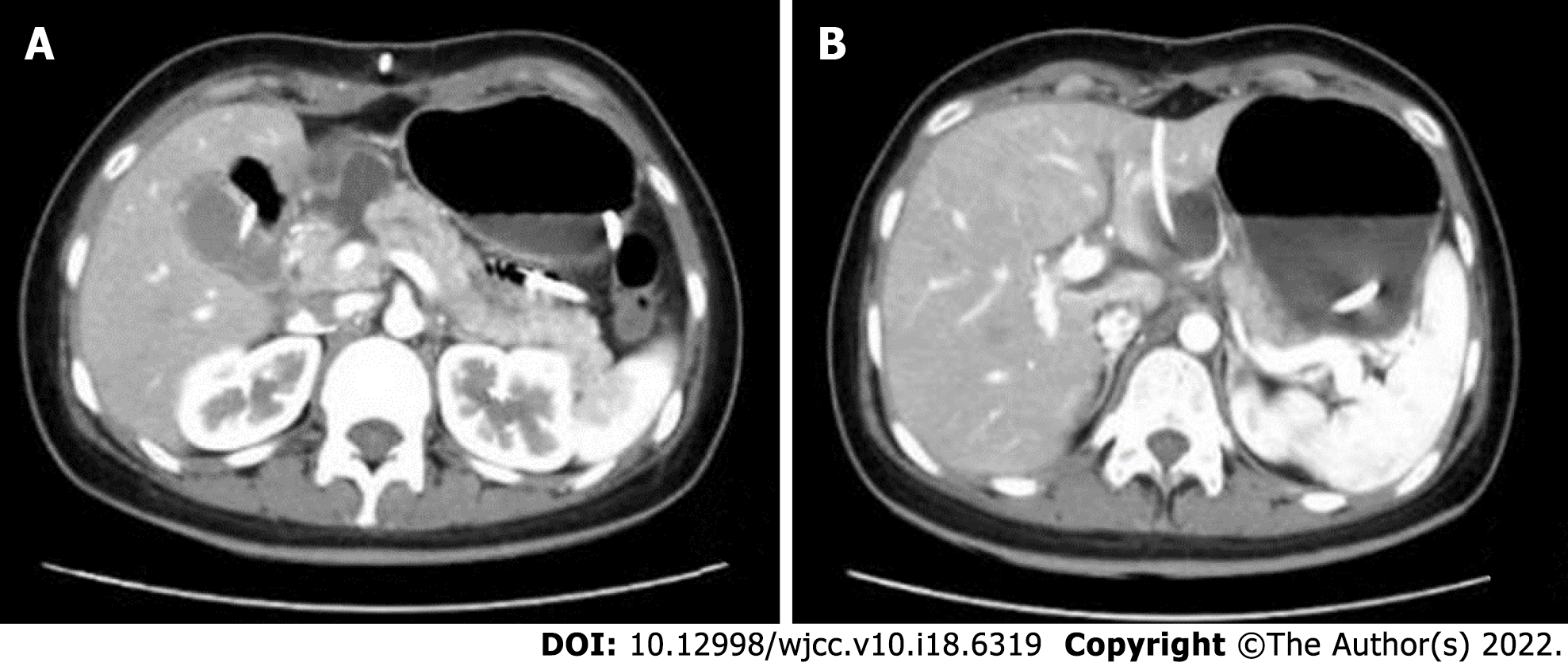
Abdominal computed tomography (CT): The pancreatic head/neck was full in shape, and small lamellar high-density shadows were seen at the anterior edge, with a CT value of 64 HU. There was no edema and thickening of bilateral anterior renal fascia and no peritoneal or retroperitoneal effusion. The lesion was not significantly enhanced during contrast-enhanced CT, and some surrounding low-density exudative shadows were observed (Figure 1).
The diagnosis was “traumatic pancreatic rupture”.
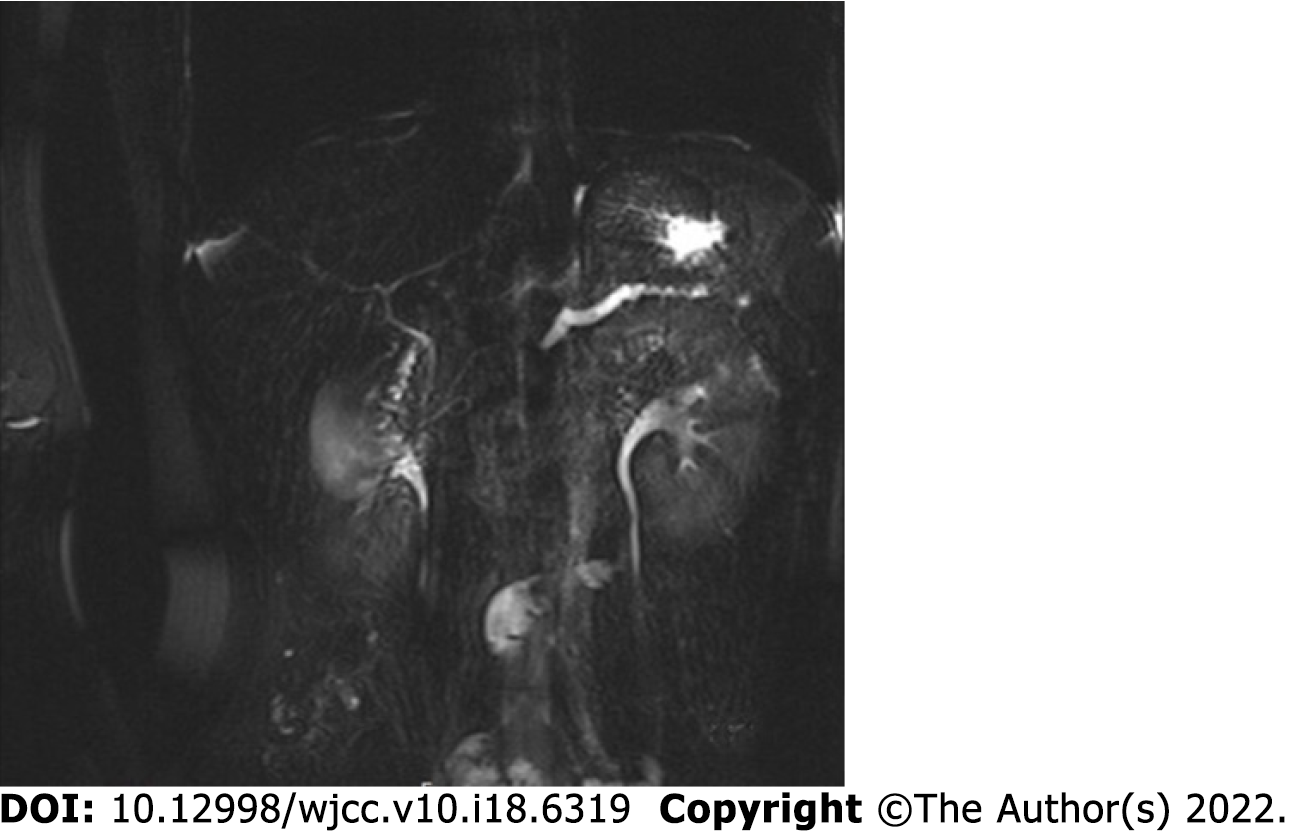
The patient was informed that her condition was critical, and there were indications for emergency surgery; however, the patient’s symptoms were not severe, her vital signs were stable, and signs of peritonitis were not obvious. Therefore, conservative treatment could be considered, with the possibility of emergency surgery if necessary. The patient was then treated with fasting, gastrointestinal decompression, acid control, digestive enzyme inhibition, anti-inflammation, and fluid replacement. After treatment, her abdominal pain was relieved. Abdominal CT on 14 July 2020 revealed lamellar high-density shadows in the pancreatic head and neck, with no significant increase in fluid collection, and with obvious exudative shadows around the pancreas; fluid accumulation was evident in the abdominal cavity. Conservative treatment was continued, and the patient’s condition gradually improved. A naso-intestinal tube was placed for enteral feeding on 20 July 2020, which was well-tolerated. Repeat ultrasonography on 23 July 2020 revealed local fluid collection in the neck of the pancreas measuring approximately 60 mm × 46 mm × 38 mm and no obvious fluid accumulation in the abdominal cavity. Therefore, catheter drainage of the peripancreatic fluid collection was performed, and approximately 300 mL of pale bloody fluid was removed. Repeat abdominal CT on 24 July 2020 revealed local dissection of the pancreatic head/neck, encapsulated effusion in the form of a pseudocyst measuring 17 mm × 31 mm, and a small amount of fluid in the abdominopelvic cavity (Figure 2). The patient was transferred to Zhejiang Provincial People's Hospital for follow-up treatment on 27 July 2020, during which inflammatory indices were normal, and serum total amylase reached a maximum of 932 U/L (upper limit of normal: 135 U/L), with no significant fluid exiting the drain. Abdominal CT was repeated and revealed that the pancreatic head/neck was morphologically swollen, with increased surrounding encapsulated fluid. Ultrasound-guided peripancreatic catheter drainage by transperitoneal was performed again, and 300 mL of clear pancreatic fluid was removed. The serum amylase concentration decreased to normal after this drainage. On 24 August 2020, puncture pancreatography visualized the distal pancreatic duct. On 25 August 2020, endoscopic retrograde cholangiopancreatography (ERCP) was performed to place a pancreatic duct stent. The pancreatic duct in the pancreatic head was circular in shape and was not connected with the pancreatic duct in the pancreatic body/tail. Therefore, the pancreatic duct stent could not be placed.
The main pancreatic duct was not dilated by transpuncture tube angiography, and there was no obvious liquid dark areas around the pancreas; therefore, the puncture drain was removed. Re-examination on 10 November 2020 revealed that the patient had no discomfort and no abnormalities on physical examination. The serum amylase concentration was 44 U/L. Magnetic resonance cholangiopancreatography (MRCP) suggested slightly dilated pancreatic ducts in the pancreatic tail (Figure 3).
The pancreas is a retroperitoneal organ with a deep and hidden location, and pancreatic injury occurs in only 0.4%-6.0% of abdominal trauma cases[1]. The pancreas is located in front of the first and second lumbar vertebrae; therefore, injury is often caused by direct action on the spine owing to crushing force from the upper abdomen, mostly sustained in the pancreatic body. Approximately 39% of pancreatic injuries are associated with pancreatic duct disruption[2]. Isolated pancreatic injury is even more rare, comprising less than 3% of cases[3].
The level of serum amylase has little significance for the early diagnosis of pancreatic trauma. Serum amylase cannot be increased in about 40% of patients, and it can also be increased in non-pancreatic injury and intestinal injury[4]. Adamson et al[5] conducted a retrospective study on 1821 patients with trauma. The level of serum amylase or lipase increased in 116 patients, and only 8 patients finally identified pancreatic trauma. The significance of serum amylase or lipase in the diagnosis of pancreatic trauma is limited, and it also depends on the necessary imaging examination. Currently, CT is the first-line technique for evaluating pancreatic injury. CT is easy to perform, and its high imaging quality, clear display of the pancreatic contours and peripancreatic bleeding, and the option for multiplanar reconstruction, can achieve a diagnostic accuracy rate of > 80%. However, there are limitations in the diagnosis of pancreatic duct disruption, and the accuracy rate needs to be improved by dynamic review[6]. In this case, we performed dynamic CT review to clarify the presence of pancreatic duct disruption. According to the American Association for the Surgery of Trauma (AAST) classification of pancreatic injuries, injuries involving the pancreatic duct are classified as grade III or IV injuries, as outlined in Table 1[7]. For hemodynamically stable patients, MRCP can be performed when further clarification of pancreatic duct integrity is needed during follow-up treatment. MRCP has the advantages of being noninvasive and providing accurate pancreatic duct imaging. In this case, complete rupture of pancreatic neck was well established by computed tomography (Figure 2A), so we did not perform MRCP. ERCP can lead to a series of complications, such as bleeding, perforation, and iatrogenic pancreatitis, and is more often used for treatment. This patient’s admission serum amylase concentration was significantly elevated, and the diagnosis of pancreatic duct disruption was confirmed when the elevated amylase finding was combined with the dynamic CT review.
| Grade1 | Type of injury | Description of injury |
| I | Hematoma | Minor contusion without duct injury |
| Laceration | Superficial laceration without duct injury | |
| II | Hematoma | Major contusion without duct injury or tissue loss |
| Laceration | Major laceration without duct injury or tissue loss | |
| III | Laceration | Distal transection or parenchymal injury with duct injury |
| IV | Laceration | Proximal transection or parenchymal injury involving ampulla |
| V | Laceration | Massive disruption of pancreatic head |
The management of pancreatic injuries is controversial and based on small retrospective studies. There are no randomized studies addressing this issue. Based on the available class III evidence, the Eastern Association for the Surgery of Trauma recommended drainage for Grade 1 and Grade 2 injuries and resection with drainage for Grade 3 or higher[8]. Siboni et al[3] study found nonoperative mana
Mohseni et al[9] research showed pancreatic resection for the treatment of grade III and IV penetrating pancreatic injury is not associated with a significant decrease in mortality but is associated with a significant increase in hospital length of stay. Drainage alone of the pancreatic bed may be a viable option, even for high-grade injuries[9]. For traumatic pancreatic injury, the optimal treatment strategy can be formulated only when the patient’s vital signs, abdominal signs, degree of pancreatic injury, and the presence of surrounding organ injury are considered comprehensively.
Recently, the use of endoscopic stenting of the pancreatic duct for the successful treatment of pancreatic duct disruption has been increasingly reported[10]. In a recently published report showing patients with pancreatic trauma who had received pancreatic stents undergoing ERCP 0-15 d after the trauma, the stents were removed after 4-8 wk and at follow-up between 6-24 mo. Endoscopic stent treatment may avoid emergency pancreatic resection and should always be considered in the management of patients with traumatic pancreatic duct injury[11]. When the patient is admitted to our hospital, the condition of this case was stable, so we did not chose pancreatic duct stent implantation. Compared with pancreatic resection, which is highly invasive and affects patients’ quality of life, endoscopic treatment is undoubtedly a new treatment strategy and is gradually gaining more attention.
In this case, after 2 mo of conservative treatment with duct drainage, the pancreatic duct healed spontaneously with no significant complications. This case provides a new consideration for clinical practice: In isolated pancreatic injury with rupture of the pancreatic duct in the head and neck, conservative treatment under close observation is feasible. In young and fit populations with stable hemodynamics, no signs of peritonitis, and no obvious active bleeding on abdominal CT, conservative treatment can be considered first, combined with dynamic CT review and fluid drainage. Endoscopic pancreatic duct stenting can then be considered if appropriate because, in some cases, the pancreatic duct can heal spontaneously.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lin F, China; Verde F, Italy S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 2. | Ding WW, Wang K, Liu BC, Xi FC, Wang ZM, Li WQ, Li JS. Management of pancreatic trauma: A report of 136 cases. Zhongguo Shiyong Waike Zazhi. 2018;38:782-785. |
| 3. | Siboni S, Kwon E, Benjamin E, Inaba K, Demetriades D. Isolated blunt pancreatic trauma: A benign injury? J Trauma Acute Care Surg. 2016;81:855-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Mahajan A. Current Status of Role of Serum Amylase and Lipase to Triage Blunt Pancreatic Trauma? J Clin Diagn Res. 2016;10:PL02. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Adamson WT, Hebra A, Thomas PB, Wagstaff P, Tagge EP, Othersen HB. Serum amylase and lipase alone are not cost-effective screening methods for pediatric pancreatic trauma. J Pediatr Surg. 2003;38:354-7; discussion 354. |
| 6. | Li RH. Manifestations and Diagnostic Value of Multi-slice Spiral CT in Patients with Emergency Pancreatic Trauma. Zhongguo CT He MRI Zazhi. 2017;15:88-90. [DOI] [Full Text] |
| 7. | Coccolini F, Kobayashi L, Kluger Y, Moore EE, Ansaloni L, Biffl W, Leppaniemi A, Augustin G, Reva V, Wani I, Kirkpatrick A, Abu-Zidan F, Cicuttin E, Fraga GP, Ordonez C, Pikoulis E, Sibilla MG, Maier R, Matsumura Y, Masiakos PT, Khokha V, Mefire AC, Ivatury R, Favi F, Manchev V, Sartelli M, Machado F, Matsumoto J, Chiarugi M, Arvieux C, Catena F, Coimbra R; WSES-AAST Expert Panel. Duodeno-pancreatic and extrahepatic biliary tree trauma: WSES-AAST guidelines. World J Emerg Surg. 2019;14:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 8. | Bokhari F, Phelan H, Holevar M, Brautigam R, Collier B, Como JJ, Clancy K, Cumming JK, Cullinane D, Smith L; on behalf of the Eastern Association for the Surgery of Trauma Practice Management and Guidelines. EAST Guidelines for the Diagnosis and Management of Pancreatic Trauma. Published 2009. Accessed June 6, 2016. Available from: http://www.east.org/education/practicemanagement-guidelines/pancreatic-trauma-diagnosis-and-management-of-pancreatic-trauma. |
| 9. | Mohseni S, Holzmacher J, Sjolin G, Ahl R, Sarani B. Outcomes after resection versus non-resection management of penetrating grade III and IV pancreatic injury: A trauma quality improvement (TQIP) databank analysis. Injury. 2018;49:27-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Kottapalli DC, Devashetty S, Suryanarayana VR, Kilari M, Ismail MD, Mathew P, Chetty PK. Complete pancreatic duct disruption in an isolated pancreatic injury: successful endoscopic management. Oxf Med Case Reports. 2016;2016:44-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Björnsson B, Kullman E, Gasslander T, Sandström P. Early endoscopic treatment of blunt traumatic pancreatic injury. Scand J Gastroenterol. 2015;50:1435-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |