Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6298
Peer-review started: December 25, 2021
First decision: February 8, 2022
Revised: February 21, 2022
Accepted: April 27, 2022
Article in press: April 27, 2022
Published online: June 26, 2022
Processing time: 173 Days and 23.9 Hours
Complicated crown-root fracture is considered a severe dental trauma and is unlikely to heal without treatment. Usually, dentists have to remove the loose coronal fragment of the fractured tooth and treat the remaining part with multidisciplinary approaches. However, we observed spontaneous healing of fracture in two pediatric cases with a history of complicated crown-root fractures over 4 years ago.
In case 1, a 12-year-old boy complained of pain at tooth 11 following an accidental fall 1 d ago. Clinical examination showed a crack line on the crown of tooth 11. Cone beam computed tomography (CBCT) images of tooth 11 showed signs of hard tissue deposition between the fractured fragments. The patient recalled that tooth 11 had struck the floor 1 year ago without seeking any other treatment. In case 2, a 10-year-old girl fell down 1 d ago and wanted to have her teeth examined. Clinical examination showed a fracture line on the crown of tooth 21. CBCT images of tooth 21 also showed signs of hard tissue deposition between the fractured fragments. She also had a history of dental trauma 1 year ago and her tooth 11 received dental treatment by another dentist. According to her periapical radiograph at that time, tooth 21 was fractured 1 year ago and the fracture was overlooked by her dentist. Both of these two cases showed spontaneous healing of complicated crown-root fractures. After over 4 years of follow-up, both fractured teeth showed no signs of abnormality.
These findings may provide new insights and perspectives on the management and treatment of crown-root fractures in children.
Core Tip: Crown-root fracture is a severe dental trauma involving the enamel, dentin, cementum, and periodontal ligament. The mobile coronal fragment usually needs to be removed or reattached with bonding agent depending on the extent of the injury. Spontaneous healing with hard tissues has been rarely reported in crown-root fracture so far. In this report, we present two clinical cases with spontaneous healing of complicated crown-root fractures of permanent central incisors in children with over 4 years of follow-up, which may provide new insights and perspectives on the management and treatment of crown-root fractures.
- Citation: Zhou ZL, Gao L, Sun SK, Li HS, Zhang CD, Kou WW, Xu Z, Wu LA. Spontaneous healing of complicated crown-root fractures in children: Two case reports. World J Clin Cases 2022; 10(18): 6298-6306
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6298.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6298
Crown-root fracture originates from the crown and extends apically in an oblique direction[1]. It is usually caused by fall, fight, traffic accident, or foreign bodies[2]. It is reported that the incidences of crown-root fractures are 2% in the deciduous teeth and 5% in the permanent dentition[3]. According to the International Association of Dental Traumatology (IADT) guidelines for the management of traumatic dental injuries, the options for the treatment of complicated crown-root fractures with pulpal exposure include partial pulpotomy, root canal therapy, gingivectomy, orthodontic extrusion, surgical extrusion, root submergence, and extraction with immediate or delayed implant-retained crown restoration or a conventional bridge[4]. Due to the complexity of crown-root fracture, its treatment is not always the same and different dentists may choose different treatments.
In this report, we present two clinical cases with spontaneous healing of complicated crown-root fractures of permanent central incisors in children. In both of these two cases, the fractured fragments healed spontaneously with hard tissue deposition around the fracture lines, which suggested that dentists may have more treatment options when dealing with crown-root fracture.
Case 1: A 12-year-old boy was referred to our department complaining of pain at his maxillary right central incisor following an accidental fall 1 d ago.
Case 2: A 10-year-old girl visited our department with her parents after she fell 1 d ago, complaining of pain at her maxillary left central incisor.
Case 1: The patient recalled that this tooth once struck the floor when he fell approximately 1 year ago, and he did not seek any treatment then due to the absence of symptoms.
Case 2: According to the patient’s dental history, tooth 11 was fractured 1 year ago and was treated with injectable Root Canal Paste (Vitapex, Morita, Japan) for apexification and composite resin being placed in chamber by a local general dentist. During the examination after that injury, the general dentist did not find any responsive sign and symptoms of injury for tooth 21.
Case 1: The patient was medically healthy without taking any medications.
Case 2: Medical history of this patient was noncontributory.
Cases 1 and 2: There were no specific family health histories.
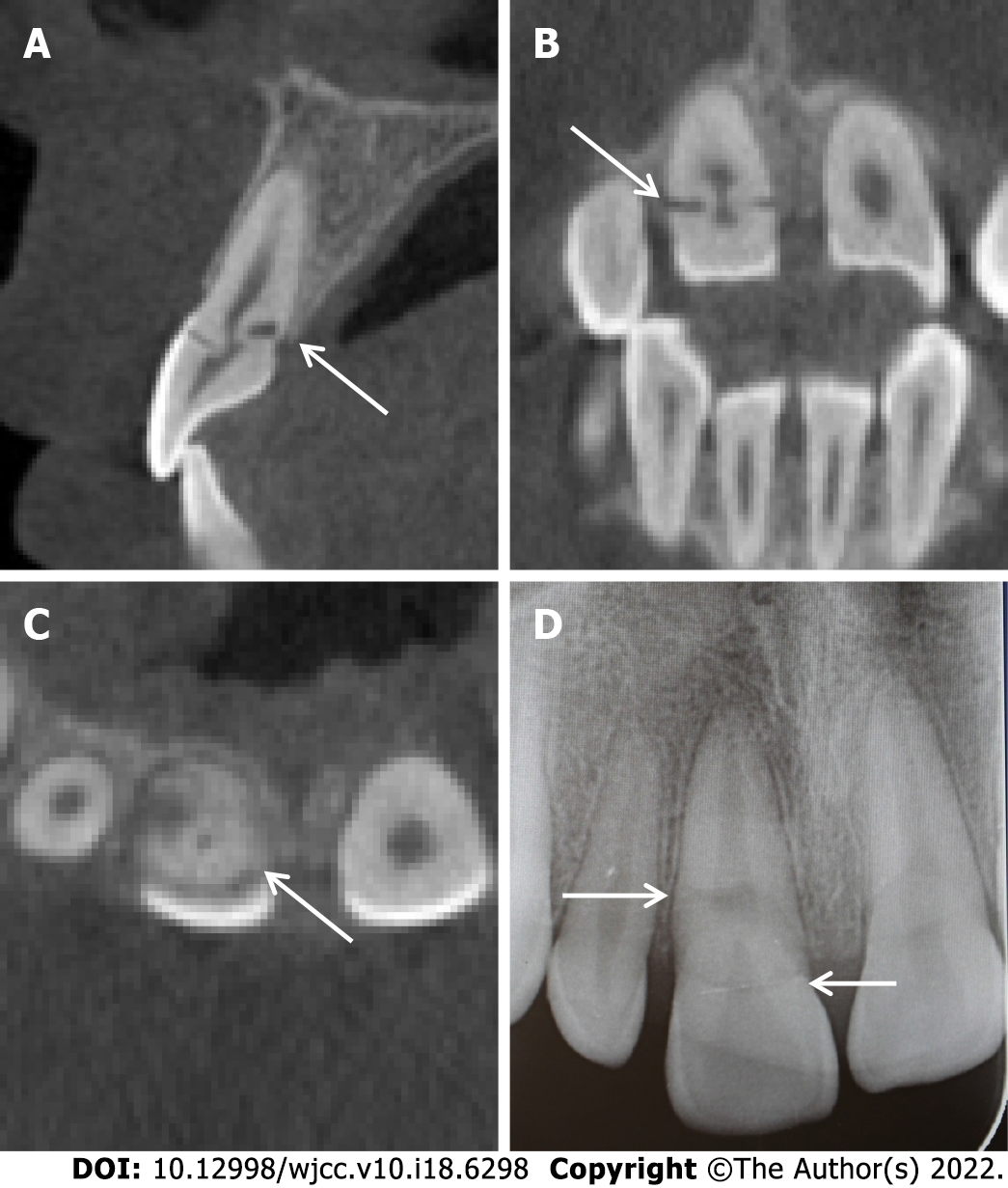
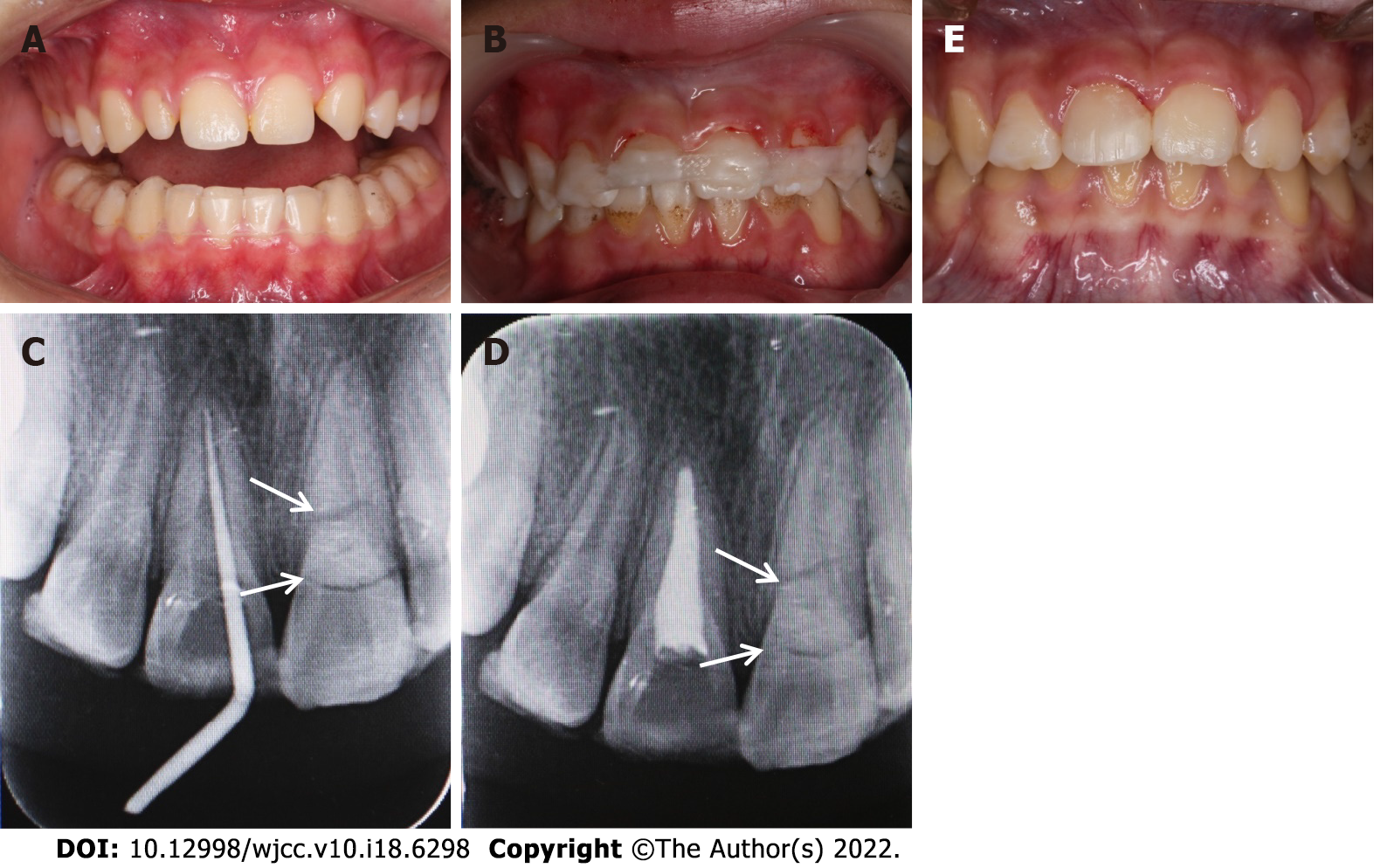
Case 1: Clinical examination showed that tooth 11 was responsive to palpation and had bleeding from the gingival crevice (Figure 1A) but showed no displacement and no increased mobility. Using a dental probe without any pressure, a crack line was detected on the crown of tooth 11, which was slightly below the gingival margin. Cold test showed no response.
Case 2: Extra-oral examinations were normal. Intra-oral examination showed that there was a complicated crown fracture in tooth 11 with discolored crown and pulp chamber being filled by resin from the lingual surface. Tooth 21 exhibited class I mobility and a facial fracture line below the gingival margin was detected by a probe without any pressure. Tooth 21 was responsive to cold test and palpation (Figure 1B).
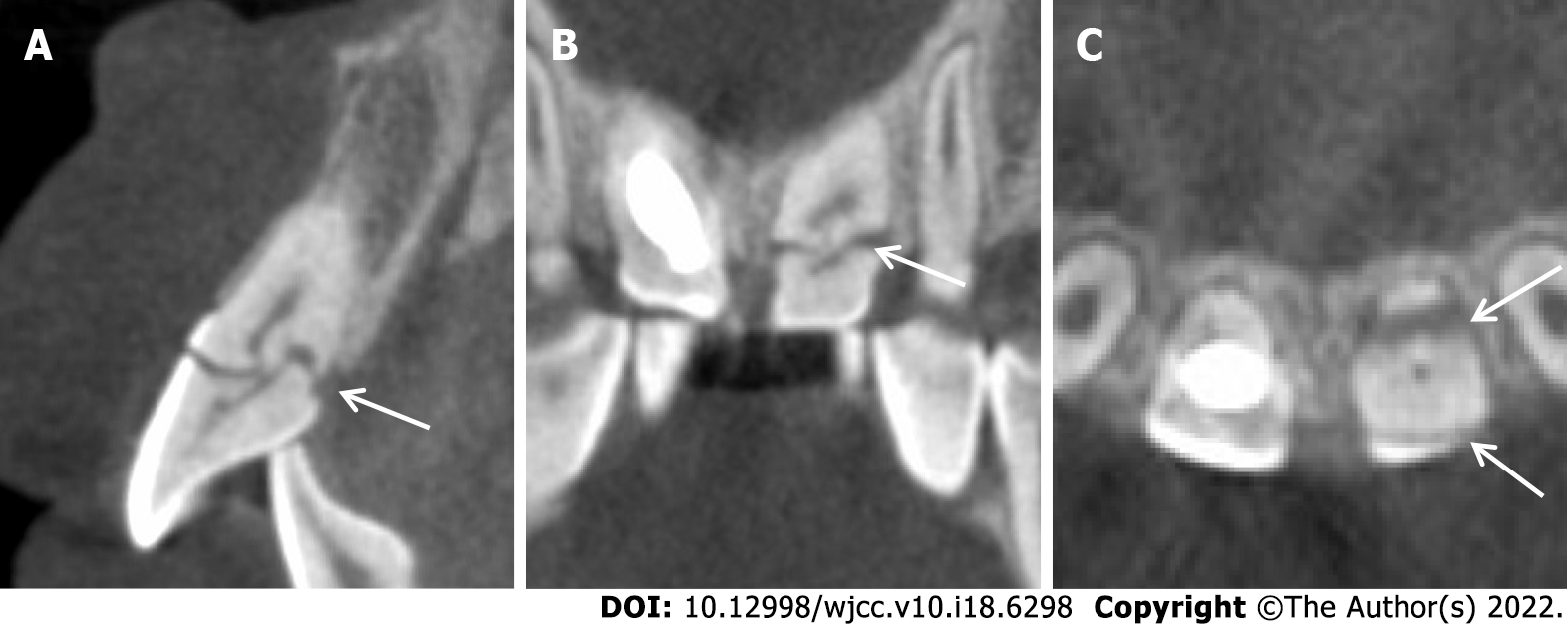
Case 1: Cone beam computed tomography (CBCT) images showed an oblique crown-root fracture line extending from the labial surface of the tooth 11 to the palatal alveolar ridge, which is approximately 3.8 mm below the palatal gingival margin. Surprisingly, the images also showed signs of hard tissue deposition between the fractured fragments (Figure 2).
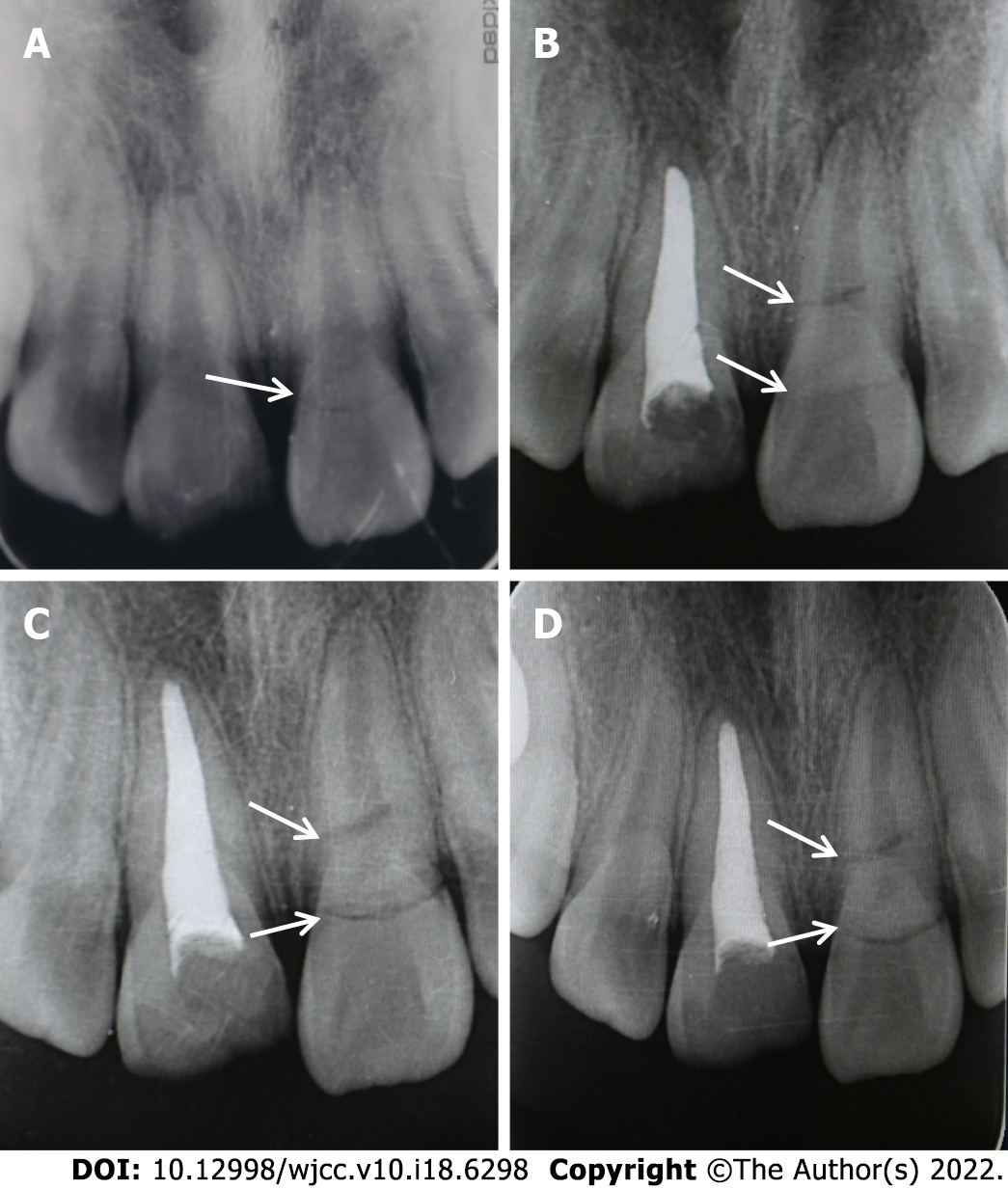
Case 2: CBCT images of tooth 21 showed an oblique crown-root fracture line starting from the labial surface and extending palatally below the alveolar ridge for approximately 3.5 mm beneath the palatal gingival margin (Figure 3), which resulted in the abnormal mobility of the coronal fragment. Interestingly, it also showed signs of hard tissue deposition at the pulpal side between the fractured fragments, indicating a healing process for the pre-existing fracture in tooth 21. Upon reviewing the radiographs taken 1 year ago after the first injury, the fracture line on tooth 21 was noticed (Figure 4). Since the patient never complained of any symptoms on tooth 21, and the periapical radiograph showed no signs of abnormality, the fracture was overlooked by the general dentist.
Based on the history and findings of the imaging examinations, tooth 11 was diagnosed as complicated crown-root fractures (old fracture spontaneous healing).
Based on the history and findings of the imaging examinations, tooth 11 was diagnosed as complicated crown fractures and tooth 21 was diagnosed as complicated crown-root fractures (old fracture spontaneous healing).
At this point, since there were no other signs and clinical symptoms, and the coronal fragment was not loose, the patient was recommended to wear a mandible occlusal pad for 2 wk with periodical revisit and special attention of not re-injuring the tooth (Figure 5A).
During the current visit, tooth 21 was stabilized with a flexible fiber splint (RTD Quartz Splint™, France, Figure 5B) and a mandible occlusal pad was placed for 2 wk. Three months later, the splint was removed and the root canal of tooth 11 was completed after obturation with gutta-percha and sealer (Figure 5C and D). Tooth 11 was then restored with resin composite 1 wk later (Figure 5E). Tooth 21 showed normal mobility and normal response in the pulp sensibility test. There were no discoloration or radiographic signs of periapical lesions at this point and no further treatment was applied.
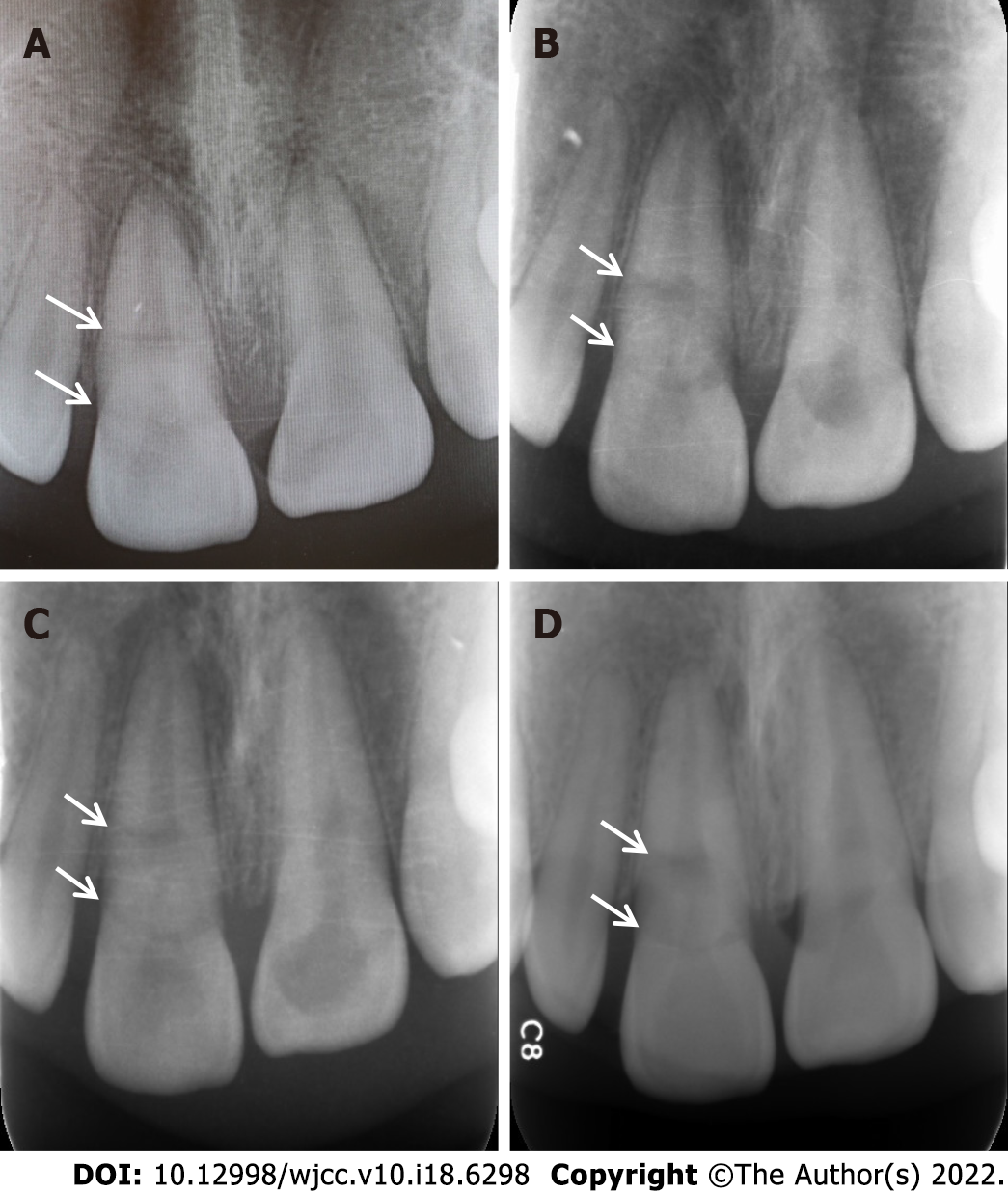
During the periodical monitoring of the pulp condition every 3 mo for 1 year, the tooth showed normal color and mobility and became responsive to pulp sensibility test (Figure 1C). Radiographic examination revealed that the fracture line became blurred gradually (Figure 6A). The patient was followed annually for 3 years, and there were no signs of abnormality on tooth 11. The periapical radiographs also appeared to be normal (Figure 6B-D).
At 1-year follow up visit, tooth 21 remained stable and was responsive to pulp test. The periapical radiograph of tooth 21 revealed no signs of periapical abnormality and no significant change of the fracture line (Figure 7A). The patient was not followed until 4 years later. Clinical examination on tooth 21 revealed no sign of abnormality. The coronal fragment was not loose, and the CBCT image of tooth 21 showed signs of healing (Figure 7B-D).
Crown-root fracture is a severe dental trauma involving the enamel, dentin, cementum, and periodontal ligament[5,6]. According to the classifications of Andreasen, it can be classified as complicated crown-root fracture if there is pulpal involvement and non-complicated crown-root fracture if there is no pulpal involvement[7]. In the case of complicated crown-root fracture, complications, e.g., pulp necrosis, apical periodontitis, and root resorption, may occur if the pulp is left untreated[8,9]. The mobile coronal fragment usually needs to be removed or reattached with bonding agent depending on the extent of the injury. Multidisciplinary care is usually required for the treatment of crown-root fracture. While relatively common in root fractures, spontaneous healing with hard tissues has been rarely reported in crown-root fracture so far[10-12]. This is probably due to the severe pulp injury and the connections of the fracture in the coronal portion with the oral cavity, leading to inevitable microbial contamination in the pulp and subsequent pulpal necrosis[13-15].
Inorganic compound accounts for 95% of the enamel[16], and fracture on the enamel is unlikely to heal. That is the reason why the enamel fragments were still separated by a narrow radiolucent line in the CBCT images, and we can still detect a fracture on the labial surface of the enamel clinically. To some extent, the two cases are analogous to root fractures in the cervical third except for the fracture on the enamel. Healing of crown-root fractures is the healing of the dentine and cementum, which is similar to the healing of root fractures. According to Andreasen and Hjorting-Hensen, healing of root fractures can be classified into four types[17]: (1) Calcified tissue wound healing; (2) Healing by interposition of connective tissue; (3) Healing by interposition of bone and connective tissue; and (4) Healing by interposition of granulation tissue. The most desirable outcome is the calcified tissue wound healing. In these two cases, it is likely that calcified tissue wound healing occurred since CBCT showed deposition of radiopaque tissues between the separated fragments. In addition, both teeth exhibited response in the pulp test during the follow-up examination, which can demonstrate the reparative dentin formation and calcified tissue wound healing.
Due to the bacterial invasion from the gingival sulcus, the reported incidence of tooth survival for root fractures in the cervical third is only 30%[18]. In these two cases, the fracture was closer to gingival sulcus than most root fractures, and the labial fracture lines were located in the gingival sulcus. Thus, it is intriguing how and why the pulp survived in these two cases. Based on the age of the patients, it is possible that the initial injuries occurred during the later phase of the maxillary central incisors eruption when the tooth roots were still immature. At that moment, the cervical region of the enamel was still covered by the junctional epithelium, which seals the fracture from the oral cavity. The junctional epithelium and the pulp also contain immune cells (e.g., neutrophils, lymphocytes, macrophages, and mast cells) that can protect the pulp against the microbes near the gingival sulcus[16,19]. Moreover, pulpal vitality after injury might be maintained by the stability of the oblique fracture line, which is in consistent with our clinical finding that there is no severe displacement of coronal fragment after injury. Finally, the immature teeth have more sufficient blood supply with a large amount of stem cells that can promote and accelerate healing. All these favorable factors provided an ideal circumstance to maintain the vitality of the pulp. The vital pulp and the intact periodontal ligament contain large number of odontoblasts and cementoblasts[19], which might contribute to the deposition of hard tissue matrix between the fragments and the healing of the fractures.
There are still some limitations in this study. The use of the mandibular pad in treatments was not based on the IADT guidelines. Instead, the treatment was based on a previous study[20]. Further research is needed to compare different treatments.
In this case report, we observed hard tissue healing without any intervention in two pediatric cases of crown-root fracture, suggesting that spontaneous healing with hard tissue deposition may occur in pediatric patients with complicated crown-root fractures and minimal displacement. It should be emphasized that conservative treatments with regular follow-up should be preferred for cases of children after trauma.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): D, D
Grade E (Poor): E
P-Reviewer: Abu Hasna A, Brazil; Hamzah SH, Malaysia; Heboyan A, Armenia; Kukiattrakoon B, Thailand; Mehta V, India; Nath SG, India; Slutzky Goldberg I, Israel S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Gao CC
| 1. | Mokhtari S, Hajian S, Sanati I. Complicated Crown-root Fracture Management Using the 180-degree Rotation Method. Int J Clin Pediatr Dent. 2019;12:247-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Andreasen JO, Andreasen FM, Andresson L. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 4th ed. Oxford: Blackwell Publishing, 2007. |
| 3. | Andreasen JO. Etiology and pathogenesis of traumatic dental injuries. A clinical study of 1,298 cases. Scand J Dent Res. 1970;78:329-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 61] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Diangelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, Sigurdsson A, Andersson L, Bourguignon C, Flores MT, Hicks ML, Lenzi AR, Malmgren B, Moule AJ, Pohl Y, Tsukiboshi M; International Association of Dental Traumatology. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28:2-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 290] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 5. | Alves MD, Tateyama MA, Pavan N, Queiroz AF, Nunes M, Endo MS. Multidisciplinary Approach to Complicated Crown-root Fracture Treatment: A Case Report. Oper Dent. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Sanaei-Rad P, Hajihassani N, Jamshidi D. Management of a complex traumatic dental injury: Crown, crown-root, and root fracture. Clin Case Rep. 2020;8:2504-2509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Yu H, Zhu H. The management of a complicated crown-root fracture incorporating modified crown-lengthening surgery. Br Dent J. 2021;230:217-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Marcenes W, al Beiruti N, Tayfour D, Issa S. Epidemiology of traumatic injuries to the permanent incisors of 9-12-year-old schoolchildren in Damascus, Syria. Endod Dent Traumatol. 1999;15:117-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 153] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 9. | Heboyan AG, Vardanyan AR, Avetisyan AA, Margaryan MM, Azatyan VY, Yesayan LK, Sharimanyan LA, Martirosyan KH. Rare clinical case of tooth root external resorption as a delayed post-traumatic complication. New Armenian Med J. 2018;12:92-97. |
| 10. | Artvinli LB, Dural S. Spontaneously healed root fracture: report of a case. Dent Traumatol. 2003;19:64-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Görduysus M, Avcu N, Görduysus O. Spontaneously healed root fractures: two case reports. Dent Traumatol. 2008;24:115-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Ranka M, Shah J, Youngson C. Root fracture and its management. Dent Update. 2012;39:530-532, 535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Andreasen FM, Andreasen JO. Root fractures. Textbook and Color atlas of traumatic injuries to the teeth. 3rd ed. Copenhagen: Munksgaard, 1994: 279-313. |
| 14. | Trope M, Chivian N, Sigurdsson A, Vann W. Traumatic injuries. In: Cohen S, Burns RC. Pathways of the pulp. 8th ed. St. Louis: Mosby, 2002: 603-649. |
| 15. | Marinčák D, Doležel V, Přibyl M, Voborná I, Marek I, Šedý J, Žižka R. Conservative Treatment of Complicated Crown Fracture and Crown-Root Fracture of Young Permanent Incisor-A Case Report with 24-Month Follow-Up. Children (Basel). 2021;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Zero DT, Zandona AF, Vail MM, Spolnik KJ. Dental caries and pulpal disease. Dent Clin North Am. 2011;55:29-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Andreasen JO, Hjorting-Hansen E. Intraalveolar root fractures: radiographic and histologic study of 50 cases. J Oral Surg. 1967;25:414-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 18. | Abbott PV. Diagnosis and Management of Transverse Root Fractures. J Endod. 2019;45:S13-S27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Lindhe J, Lang NP, Karring T. Clinical periodontology and implant dentistry. 5th ed. Oxford: Blackwell Publishing, 2008. |
| 20. | Zhang HW, Li Y, Zhang Z. The clinical study of vacuum-formed jaw-pillow used for teeth fixing in children with traumatic anterior teeth. Yati Yasui Yazhoubing Xue Zazhi. 2014;34:488-490. |