Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6247
Peer-review started: December 7, 2021
First decision: January 25, 2022
Revised: February 12, 2022
Accepted: April 20, 2022
Article in press: April 20, 2022
Published online: June 26, 2022
Processing time: 191 Days and 12.8 Hours
Embedded foreign bodies in the tongue are rarely seen in clinical settings. An untreated foreign body can cause a granuloma which often presents as an enlarged tongue mass. However, if foreign body ingestion status is unknown, physical examination and magnetic resonance imaging (MRI) tend to lead to suspicion of tongue cancer, especially in older patients. Thus, differential diagnosis of an enlarged tongue mass is important, especially because it is closely related to the choice of treatment method.
A 61-year-old woman was admitted to the hospital with pain and noticeable swelling in the tongue that had persisted for over 1 mo. She had no previous medical history. MRI revealed abnormal signal intensities that were indicative of a neoplasm. Thus, the oral surgeon and radiologist arrived at a primary diagnosis of tongue cancer. The patient visited the Ear Nose and Throat Department for further consultation and underwent an ultrasound examination of the tongue. The ultrasonography was consistent with a linear hyperechoic foreign body which was indicative of an embedded foreign body (bone) in the tongue, even though the patient denied any history of foreign body ingestion. Complete surgical enucleation of the lesion was conducted. The mass which included a fish bone was completely removed. The post-operative pathological examination confirmed that the mass was a granuloma containing collagen fibers, macrophages and chronic inflammatory cells. The patient recovered without complications over a 2 mo follow-up period.
We report a rare case of foreign body granuloma in the tongue that was primarily diagnosed as tongue cancer. The MRI and ultrasound examinations revealed a piece of bone in the left lateral aspect of the tongue. The granuloma, which contained a fish bone, was completely removed via surgery and confirmed via biopsy. Differential diagnosis of the enlarged tongue mass was critical to the selection of treatment method.
Core Tip: This case report concerns an older adult referred to our Ear Nose and Throat Department with an enlarged tongue mass and a primary diagnosis of tongue cancer after magnetic resonance imaging (MRI). A review of the MRI data and oral ultrasound examination diagnosed a foreign body granuloma, confirmed by surgery and postoperative pathological examination. Oral ultrasound and/or computed tomography are critical in terms of differential diagnosis; certain MRI features may provide clues guiding diagnosis of a foreign body granuloma.
- Citation: Jiang ZH, Xv R, Xia L. Foreign body granuloma in the tongue differentiated from tongue cancer: A case report. World J Clin Cases 2022; 10(18): 6247-6253
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6247.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6247
The introduction of a foreign body into the tongue can occasionally occur as food is being chewed. In most situations this can lead to pain, swelling and irritation[1]. Such foreign bodies can usually be identified and diagnosed via visual inspection, especially if they are not buried in the muscle layer[2]. A clear history of foreign body introduction into the mouth, as well as a timely visit to the physician, can be conducive to the diagnosis[3]. Penetration of the tongue by a foreign substance can cause an acute inflammatory response and foreign bodies that remain in place may elicit a granulomatous inflammatory response[4]. The cause of granuloma in the tongue can be difficult to ascertain, especially without a clear history of foreign body ingestion. In this paper, we describe the case of a foreign body granuloma in the tongue of a Chinese woman. The initial diagnosis was tongue cancer but further examination revealed a foreign body in the tongue which was removed via surgery.
A 61-year-old woman was admitted to the Ear Nose and Throat (ENT) Department of our hospital complaining of pain and noticeable swelling of the tongue.
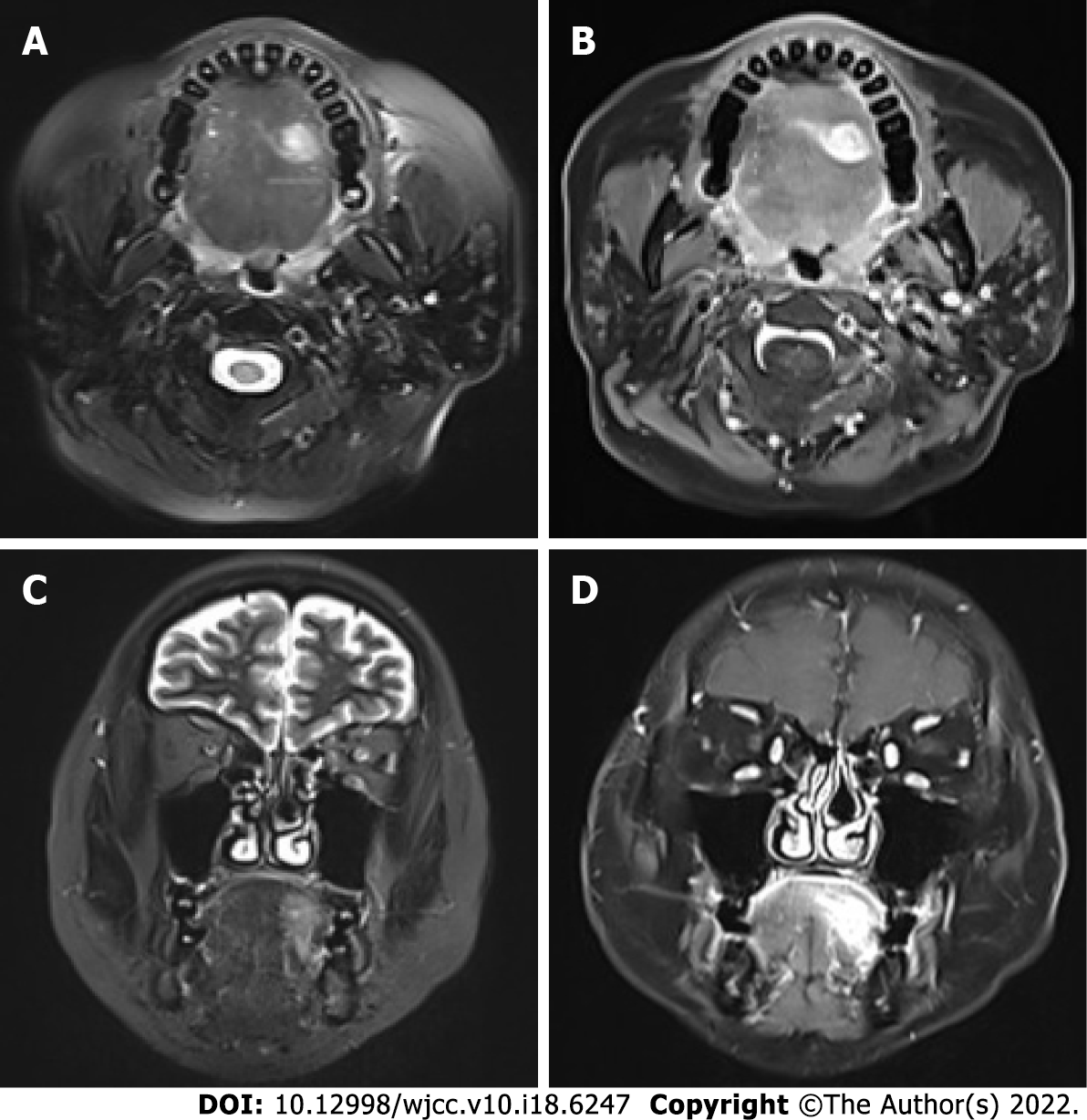
The patient sought out a general practitioner because of pain and noticeable swelling in the tongue that persisted for over 1 mo. She was given a short course of antibiotics which provided no symptom relief. The patient was referred to the Department of Stomatology, where an oral surgeon prescribed oral maxillofacial magnetic resonance imaging (MRI). The imaging revealed abnormal signal intensities, as shown in Figure 1, which are indicative of tongue cancer. The patient then visited the ENT Department for further consultation.
The patient had no previous medical history.
There was no specific personal and family history.
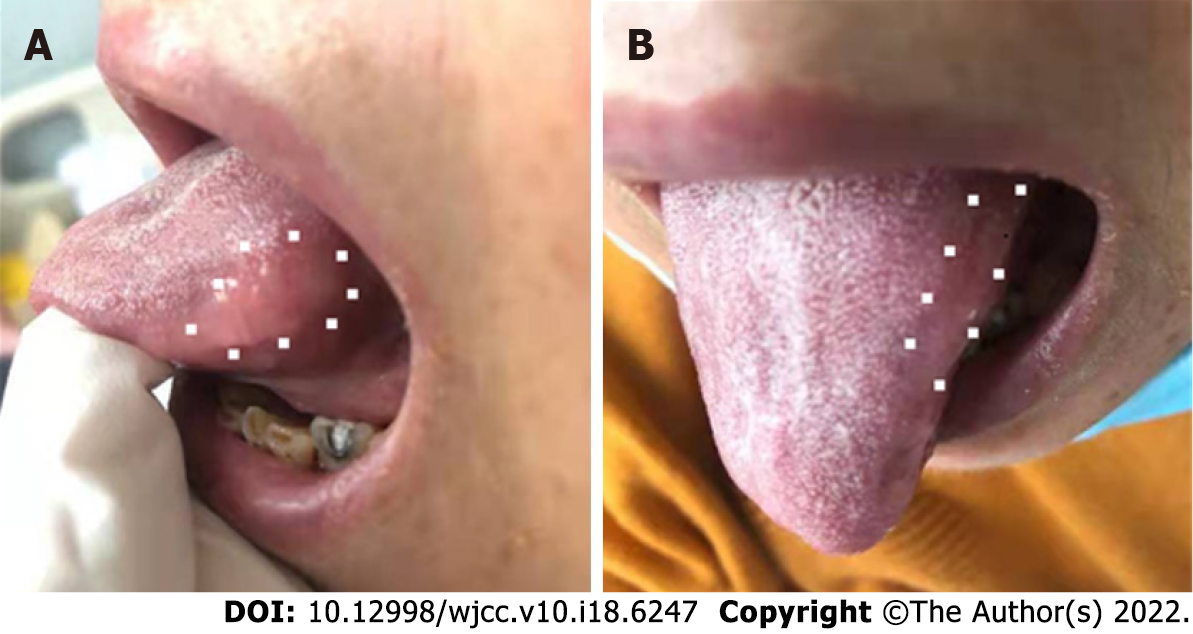
Intraoral examination showed mild swelling in a longitudinal 2 cm × 1.5 cm area on the left lateral aspect of the tongue. A hardened nodule with an ill-defined margin was found on the tongue. The nodule was the same color as the surrounding tongue tissue (normal color) and no clearly identifiable foreign bodies were observed on the tongue as shown in Figure 2.
The results of routine tests of complete blood count, kidney function and liver function were normal.
The oral maxillofacial MRI showed abnormal and ill-defined signal intensities on the left side of the tongue (size: 1.6 cm × 1.2 cm × 2.0 cm; Figure 1) and multiple swollen cervical lymph nodes (up to 0.7 cm in size, in the submaxillary region and carotid sheath). The primary diagnosis was tongue cancer as reported by the specialists in the Department of Radiology. However, the doctors in the ENT Department reviewed the MRI images and considered the possibility of foreign body granuloma for two reasons. First, granuloma and cancer can have similar imaging features; and second, the shadow seemed to indicate that the tongue tissue was protected from foreign bodies, as shown by images taken in the transverse plane. During the initial clinical interview the patient denied a history of foreign body ingestion. To differentiate between the two possibilities, further examinations were conducted.
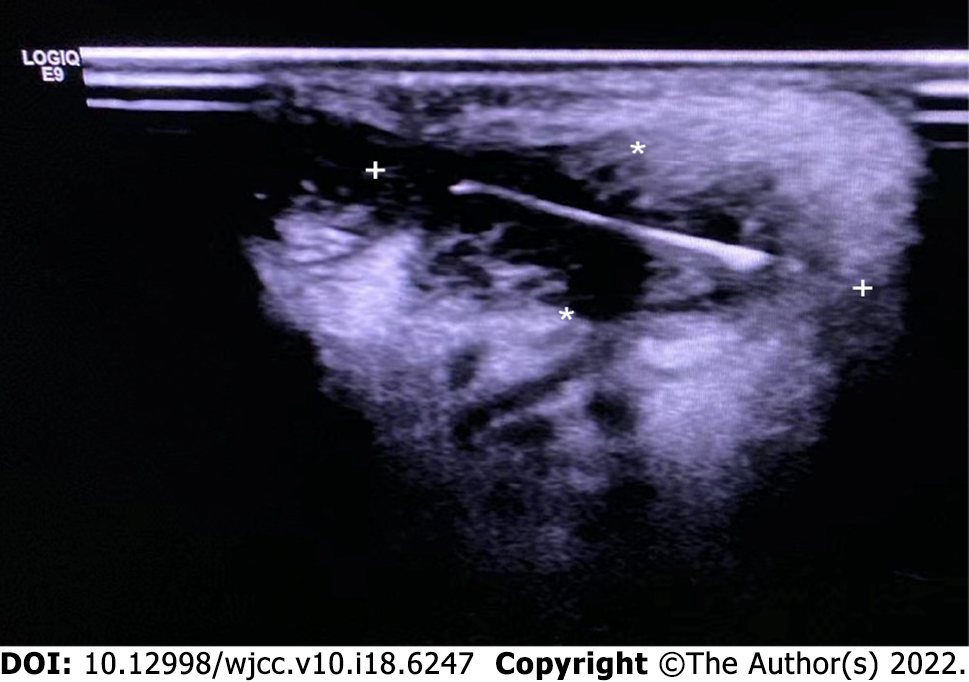
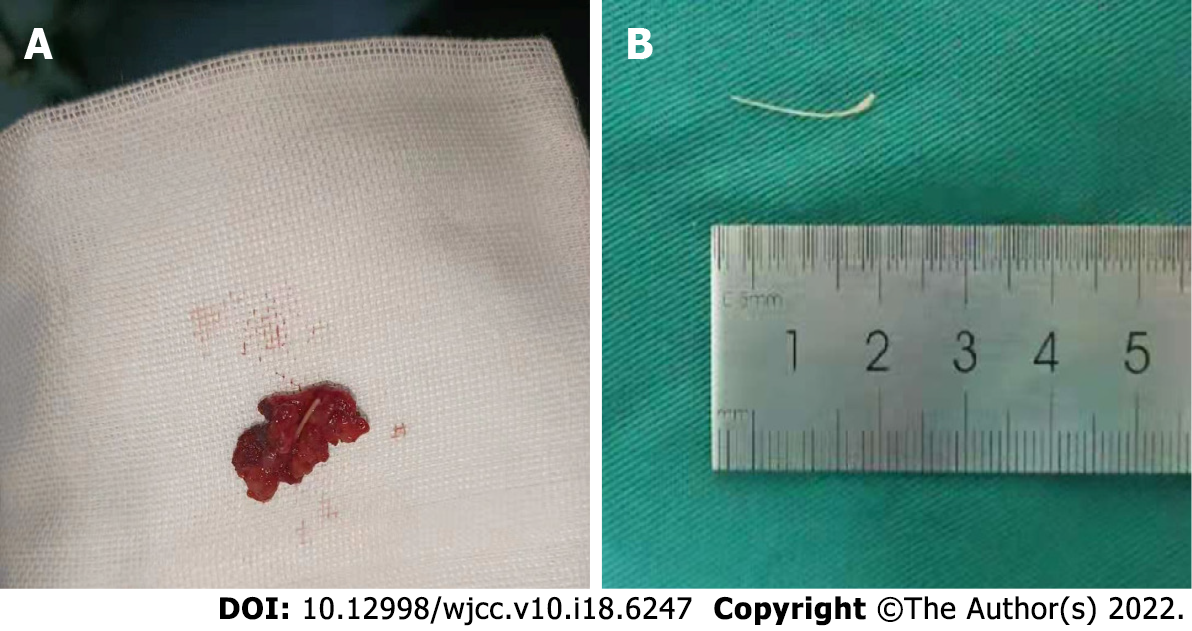
The patient was referred for ultrasound examination of the tongue. The ultrasound device used a linear probe with a 13-MHz transducer. The acoustic picture was consistent with a linear hyperechoic foreign body, specifically a piece of bone, as shown in Figure 3. When asked about the possibility of fish bone ingestion or another foreign body in the tongue, the patient could not recall whether she had recently eaten fish. However, her daughter recalled that a meal containing fish (with bones) might have been served to the patient 2 mo prior to seeking medical assistance. Complete surgical enucleation of the lesion was then conducted. The mass with the fish bone was completely removed without compromising the capsule (Figure 4A), and no hemorrhagic accident occurred. The fish bone was 1.5 cm in length (Figure 4B). Post-operative pathological examination showed that the lesion was a granuloma containing collagen fibers, macrophages and chronic inflammatory cells.
Foreign body (fish bone) granuloma in the tongue.
After the surgery, the patient received antibiotics (ceftriaxone) with systemic steroids and the post-operative recovery was uneventful. The patient was discharged on the third post-operative day.
The patient recovered well and there were no complications during the 2-mo follow-up period.
A diagnosis of tongue cancer is often considered in older adults with an enlarged tongue nodule/mass and localized pain[5]. The many differential diagnoses of a tongue mass include an inflammatory lesion and schwannoma[1]. A diagnosis of a granuloma attributable to an embedded foreign body is rare when there is no clear history of foreign body ingestion or oral trauma[6]. In the present case, the differential diagnosis of an irregular nodule with a smooth surface included cavernous hemangioma, anaplastic large-cell lymphoma, endophytic squamous cell carcinoma and Kaposi sarcoma of the tongue[7-10]. Differential diagnosis is important as cancer treatment and enucleation of a foreign body granuloma differ greatly in terms of surgical preparation, operation, tongue reconstruction and patient consultation[11-13].
MRI is the preferred diagnostic modality for evaluating tongue cancer because abnormal MRI signals have been strongly associated with pathological findings[14]. However, MRI is not an ideal modality for differentiating tongue cancer from embedded foreign body granuloma with foreign body[15]. The signals associated with tongue cancer are hyperintensity in a T2-weighted image (WI) and heterogeneous enhancement in an enhanced T1 WI, similar to granuloma[14,16]. In the present case, the fish bone (shown by hypointense signals in both the T1 and T2 WIs) was difficult to detect by MRI[17], and not surprisingly the primary diagnosis of tongue cancer was consistent with the abnormalities found in the tongue by MRI and with the swollen cervical lymph nodes. Besides this, shifting of metal fragments under the effects of MRI can result in potential damage of vital structures. If the doubt of a metal foreign body is present, the contraindications of MRI should be considered[18].
Several studies used ultrasound to detect a suspected embedded foreign body in the tongue[3,4,6]. The foreign bodies, which included a pequi spine, metal wire, and fish bone were visualized and localized accurately, demonstrating the utility of ultrasound for guiding therapeutic interventions. Multislice computerized tomography (CT) and cone beam CT also seem useful for visualizing embedded foreign bodies, although CTs have poor performance in terms of detecting wood[15]. Thus, when an embedded foreign body is suspected in a patient with an enlarged tongue mass, ultrasonography and CT can play an important role in the differential diagnosis[19].
In our case, the lesion was “walled off” on transverse images (Figure 2). This might indicate that the mass was “delimited” by a capsule. A similar sign was observed in an early case report of a patient with foreign body granuloma[16]. Thus, this sign might be a useful indicator of the need for further examinations (other than MRI). However, this issue requires further investigation.
We reported the case of a woman with an enlarged tongue mass initially diagnosed with tongue cancer. The ENT specialists reviewed the MRI data and corrected the diagnosis to ‘foreign body in the tongue’ based on oral ultrasound examination. The granuloma containing the fish bone was completely removed during surgery and post-operative pathological examination confirmed that the lesion was a granuloma. In cases with an enlarged tongue mass, oral ultrasound and/or CT examinations are important for differential diagnosis, to facilitate selection of the appropriate treatment method.
The authors acknowledge the colleagues for participating in this study. We are deeply indebted to the patient who participated in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Saleem S, Pakistan; Zahed M, Iran S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Patel KS. Foreign body in the tongue: an unusual site for a common problem. J Laryngol Otol. 1991;105:849-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Kumagai K, Hirose Y, Yoshida S. Woman With Foreign Body on Her Tongue. Ann Emerg Med. 2018;72:e121-e122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Pigott DC, Buckingham RB, Eller RL, Cox AJ. Foreign body in the tongue: a novel use for emergency department ultrasonography. Ann Emerg Med. 2005;45:677-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Pereira RMA, de Oliveira Afonso Pereira PC, Rodrigues VC, de Andrade LFB, de Carvalho EM, Júnior HM. Foreign Body Granuloma in the Tongue by a Pequi Spine. Case Rep Dent. 2020;2020:8838250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Tagliabue M, Belloni P, De Berardinis R, Gandini S, Chu F, Zorzi S, Fumagalli C, Santoro L, Chiocca S, Ansarin M. A systematic review and meta-analysis of the prognostic role of age in oral tongue cancer. Cancer Med. 2021;10:2566-2578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 6. | Lin CJ, Su WF, Wang CH. A foreign body embedded in the mobile tongue masquerading as a neoplasm. Eur Arch Otorhinolaryngol. 2003;260:277-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Kripal K, Rajan S, Ropak B, Jayanti I. Cavernous hemangioma of the tongue. Case Rep Dent. 2013;2013:898692. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Fatahzadeh M, Schwartz RA. Oral Kaposi's sarcoma: a review and update. Int J Dermatol. 2013;52:666-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Mangold AR, Torgerson RR, Rogers RS. Diseases of the tongue. Clin Dermatol. 2016;34:458-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 10. | Tang W, Wang Y, Yuan Y, Tao X. Assessment of tumor depth in oral tongue squamous cell carcinoma with multiparametric MRI: correlation with pathology. Eur Radiol. 2022;32:254-261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Mannelli G, Arcuri F, Agostini T, Innocenti M, Raffaini M, Spinelli G. Classification of tongue cancer resection and treatment algorithm. J Surg Oncol. 2018;117:1092-1099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 12. | Konishi M, Fujita M, Shimabukuro K, Wongratwanich P, Verdonschot RG, Kakimoto N. Intraoral Ultrasonographic Features of Tongue Cancer and the Incidence of Cervical Lymph Node Metastasis. J Oral Maxillofac Surg. 2021;79:932-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Teo DT, Loy AH, Goh YH, Chan YM. Head and neck cancer after foreign body ingestion. Ann Acad Med Singap. 2004;33:379-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Ong CK, Chong VF. Imaging of tongue carcinoma. Cancer Imaging. 2006;6:186-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Javadrashid R, Fouladi DF, Golamian M, Hajalioghli P, Daghighi MH, Shahmorady Z, Niknejad MT. Visibility of different foreign bodies in the maxillofacial region using plain radiography, CT, MRI and ultrasonography: an in vitro study. Dentomaxillofac Radiol. 2015;44:20140229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Chen H. A tongue granuloma due to a fishbone mimicking a neoplasm: ultrasound-guided differential diagnosis. Ultraschall Med. 2011;32 Suppl 1:S1-S2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Wang A, Zhou Y, Huang Q. A fish bone induced aortic arch pseudoaneurysm in a male patient: A case report. Medicine (Baltimore). 2019;98:e16486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Caraiani C, Petresc B, Dong Y, Dietrich CF. Contraindications and adverse effects in abdominal imaging. Med Ultrason. 2019;21:456-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Kim JP, Kwon OJ, Shim HS, Kim RB, Kim JH, Woo SH. Analysis of Clinical Feature and Management of Fish Bone Ingestion of Upper Gastrointestinal Tract. Clin Exp Otorhinolaryngol. 2015;8:261-267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |