Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6192
Peer-review started: November 7, 2021
First decision: January 11, 2022
Revised: January 18, 2022
Accepted: April 29, 2022
Article in press: April 29, 2022
Published online: June 26, 2022
Processing time: 221 Days and 14.4 Hours
Spontaneous esophageal rupture or Boerhaave's syndrome is a rare and acute disease with a high incidence of misdiagnosis and mortality. Here, we aimed to explore the clinical characteristics, diagnosis, treatment, and prognosis of spon
The clinical features of the patient with spontaneous esophageal rupture misdiagnosed earlier as pleural effusion were retrospectively analyzed and the reasons for misdiagnosis are discussed based on a current review of the literature. The patient was admitted to a local hospital due to shortness of breath accompanied by vomiting and abdominal distension for five hours. Based on the computed tomography (CT) scan analysis, clinically, right pleural effusion was diagnosed. However, the patient was unwilling to undergo right closed thoracic drainage. The patient also had intermittent fevers against infection, and during the course of treatment, he complained of chest pain, following which, he was transferred to our hospital. Grapefruit-like residue drainage fluid was observed. Re-examination of the chest CT scans suggested the presence of spontaneous perforation in the upper left esophagus. Therefore, the patient underwent an urgent esophageal hiatus repair. Unfortunately, the patient died of infection and respiratory failure due to progressive dyspnea after surgery.
Spontaneous esophageal rupture is a rare disease associated with high fatality. The patients do not present typical clinical symptoms and the disease progresses rapidly. This case report highlights the importance of a dynamic review of chest CT scan, not only for the initial identification of segmental injury but also for prioritizing subsequent treatment strategies. Moreover, we have presented some clues for clinicians to recognize and diagnose spontaneous esophageal rupture at rare sites (upper-esophageal segment) through this case report of spontaneous esophageal rupture that caused the patient's death. We have also summarized the reasons for the misdiagnosis and lessons learned.
Core Tip: Spontaneous esophageal rupture is a rare disease associated with high fatality. We report a case of spontaneous esophageal rupture misdiagnosed earlier as pleural effusion at an early stage and investigated the causes of its misdiagnosis, along with our experience during diagnosis and treatment. This case report also highlights the importance of a dynamic chest computed tomography review, not only for initial identification of the injured segment but also for prioritizing subsequent treatment strategies. Moreover, we also provide clues for clinicians to recognize and diagnose spontaneous esophageal rupture at a rare site (upper-esophageal segment) by reporting this case.
- Citation: Tan N, Luo YH, Li GC, Chen YL, Tan W, Xiang YH, Ge L, Yao D, Zhang MH. Presentation of Boerhaave’s syndrome as an upper-esophageal perforation associated with a right-sided pleural effusion: A case report. World J Clin Cases 2022; 10(18): 6192-6197
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6192.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6192
Spontaneous esophageal rupture refers to the full-thickness rupture of the esophageal wall caused by indirect trauma, non-foreign bodies, non-esophageal, and/or adjacent organ disease; it is also known as Boerhaave’s syndrome[1]. While the incidence of this disease is low, it is easily misdiagnosed at an early stage and progresses rapidly. After the occurrence of an esophageal rupture, due to negative pressure in the pleural cavity, the stomach contents easily enter the mediastinum and thorax, which often causes serious mediastinum infection and empyema in the early stages. If not treated promptly, severe sepsis rapidly develops into multiple organ failure and even death, which is an emergency during thoracic surgery[2]. Therefore, the associated mortality rate is extremely high. Thus, correctly diagnosing spontaneous esophageal rupture in the early stage is of great importance for the survival of patients with spontaneous esophageal rupture.
Herein, we report a case of spontaneous esophageal rupture misdiagnosed earlier as pleural effusion at an early stage and investigated the causes of its misdiagnosis, along with our experience during diagnosis and treatment. We also highlight the importance of reviewing dynamic chest computed tomography (CT) scans for the diagnosis of spontaneous esophageal rupture.
An 84-year-old male was admitted to a local hospital, with complaints of shortness of breath, abdominal distension, and vomiting.
The patient was admitted to a local hospital, with complaints of shortness of breath, abdominal distension, and vomiting. He did not vomit again during his stay at the hospital.
Based on the evidence, the patient was diagnosed with pleural effusion and recommended to undergo right closed thoracic drainage; however, the patient's family refused given his advanced age. Therefore, antibiotics were prescribed to prevent infection. However, after treatment, blood inflammatory indicators were significantly elevated and did not improve [white blood cell (WBC) count: 19.40 × 109/L; C-reactive protein (CRP): 304.90 mg/L] (Table 1). The patient also suffered from intermittent fevers and over time, complained of chest pain. After eight days, the patient was transferred to our hospital.
| Date | T (℃) | WBC | GR% | N | Hb | CRP | PCT | cTnI | Myo | BNP | Antibiotic |
| February 26, 20211 | 36.1 | 12.15 | 86.2 | 10.5 | 108 | 13.96 | 132.7 | 154.5 | 40.6 | Unclear | |
| March 5, 20211 | 38 | 19.4 | 93.7 | 18.2 | 95 | 304.9 | 6.51 | 27.7 | 151.2 | 325.9 | Unclear |
| March 7, 20212 | 37.8 | 20.36 | 95.5 | 19.4 | 84 | 211.24 | 31.26 | 5816 | Imipenem+ | ||
| Linezolid | |||||||||||
| March 9, 20212 | 36.8 | 15.44 | 92.8 | 14.3 | 76 | 163.9 | 9.37 | 4354 | Imipenem+ | ||
| Linezolid | |||||||||||
| Imipenem+ | |||||||||||
| March 10, 20212 | 36.9 | 13.88 | 89.3 | 12.4 | 81 | 177.82 | 7.28 | Linezolid+ | |||
| Fluconazole | |||||||||||
| March 13, 20212 | 36.6 | 10.78 | 95 | 10.2 | 94 | Sulperazon | |||||
| March 15, 20212 | 36.9 | 10.3 | 90.2 | 9.3 | 83 | Sulperazon | |||||
| March 19, 20212 | 36.5 | 16.62 | 95.8 | 15.9 | 78 | Sulperrazon |
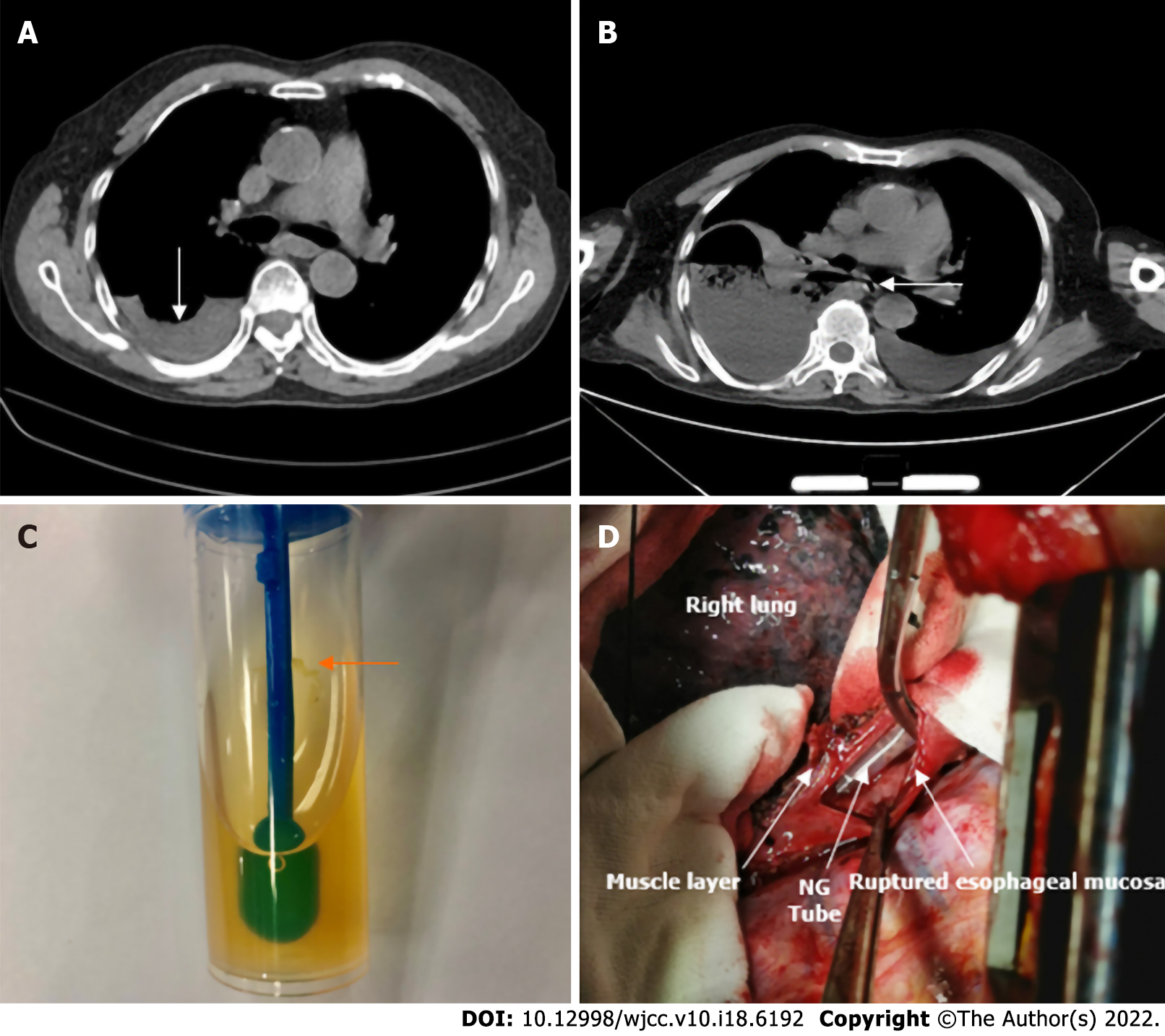
After admission, the patient agreed to undergo right closed thoracic drainage and grapefruit-like residue drainage fluid was observed (Figure 1C). During the physical examination, subcutaneous emphysema of the right chest wall with crepitus was detected.
The patient had no history of lung diseases.
No similar disease was identified in his family.
His vital signs were stable and no other specific symptoms were noted.
The initial routine blood examination results showed that both WBC count and CRP levels were slightly elevated (WBC: 12.15 x 109/L, CRP: 13.96 mg/L, Table 1).
During hospitalization, laboratory tests also indicated an increase in inflammatory markers.
The chest CT scan showed the presence of a small amount of fluid in the right pleural cavity (Figure 1A). Thus, chest CT scanning was repeated. Right-sided pleural effusion with right lung distension insufficiency and perforation of the upper left esophagus were observed (Figure 1B).
Considering the above signs and symptoms, the patient was diagnosed with spontaneous perforation of the upper left esophagus, and an urgent esophageal hiatus repair was performed.
During surgery, a right lateral thoracic incision was made. The patient's right chest wall, muscles, and fascia were severely congested and edematous, along with a ruptured esophagus (Figure 1D).
Unfortunately, due to deterioration of his condition, the patient died from infection and respiratory failure.
Spontaneous esophageal rupture, a rare and life-threatening disease, was first reported by Rokicki M in 1724, and to date, a mere 50 cases have been reported in the literature[3]. Based on an epidemiological survey for this disease in Iceland, it has a low incidence of 31 per million per year[4]. Moreover, several studies confirm that men are more prone to morbidity than women and that the highest risk group included those in the 40-60 years age group[5]. Spontaneous esophageal rupture caused by vomiting followed by a large meal often precipitates secondary bacterial infections, which contribute to 50% of the total mortality[6]. Therefore, early diagnosis and surgical treatment are important in the treatment of this disease.
Although many cases of spontaneous esophageal rupture have been reported, the lack of specific symptoms of this condition continues to pose a challenge[7]. Mackler's triad comprising an acute presentation of retching or vomiting, lower chest pain, and surgical emphysema, is a clinical manifestation with relatively high specificity for the diagnosis of spontaneous esophageal rupture. However, its incidence is only about 14%[8,9]. Other signs, which are non-specific, including hemo
To the best of our knowledge, spontaneous esophageal rupture often occurs in the thoracic esophagus and its incidence in the upper thoracic esophagus is relatively rare. The reasons for this are broadly described as follows: the myometrium of the esophagus is divided into two, the inner ring and the outer longitudinal layer. Approximately 2 mm thick elastic fibers are sandwiched between the two layers. Owing to the lack of coherence in the anatomical structure of the esophagus, a sudden rise in intra-esophageal pressure (up to 290 mmHg) can lead to rupture at this altered anatomical structure of the esophagus[11]. While esophageal rupture occurs most commonly in the lower third of the left thoracic segment of the esophagus (80%), it is less frequent in the right esophagus, the upper thoracic, and ventral segments of the esophagus[12]. Among the physical signs, right pleural effusion is also uncommon. In the case of the upper thoracic esophageal perforation, prevertebral or subcutaneous air may be present[13]. Herein, we reported in detail, a case of a spontaneous esophageal rupture in the upper thoracic esophagus, with no obvious signs and symptoms in the early stage. Due to the lack of an early dynamic chest CT review, this disease was misdiagnosed.
Collectively, the reasons for the misdiagnosis were as follows: first, the on-admission chest CT report was only suggestive of a right-sided hydropneumothorax, inconsistent with CT presentation in most reports; additionally, chest pain began later during the course of disease progression, along with a lack of other typical manifestations. Finally, upper thoracic esophageal perforation is a rare site of esophageal rupture and the dynamic chest CT scan was not reviewed during hospitalization, thereby leading to early misdiagnosis and a consequent delay in appropriate treatment.
This case report highlights the importance of a dynamic chest CT review, not only for initial identification of the injured segment but also for prioritizing subsequent treatment strategies. Moreover, we also provide clues for clinicians to recognize and diagnose spontaneous esophageal rupture at a rare site (upper-esophageal segment) by reporting this case of spontaneous esophageal rupture and summ
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Choi YS, South Korea; He D, China S-Editor: Ma YJ L-Editor: Webster JR P-Editor: Ma YJ
| 1. | Maurya VK, Sharma P, Ravikumar R, Bhatia M. Boerhaave's syndrome. Med J Armed Forces India. 2016;72:S105-S107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Garas G, Zarogoulidis P, Efthymiou A, Athanasiou T, Zacharakis E. Spontaneous esophageal rupture as the underlying cause of pneumothorax: early recognition is crucial. Journal of Thoracic Disease. 2014;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Rokicki M, Rokicki W, Rydel M. Boerhaave's Syndrome- Over 290 Yrs of Surgical Experiences. Polski przeglad chirurgiczny. 2016;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Vidarsdottir H, Blondal S, Alfredsson H, Geirsson A, Gudbjartsson T. Oesophageal perforations in Iceland: a whole population study on incidence, aetiology and surgical outcome. Thoracic & Cardiovascular Surgeon. 2010;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 5. | Marshall W B. Boerhaave syndrome: a case report. AANA Journal. 2002;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Brauer R B, Liebermann-Meffert D, Stein H J, Bartels H, Siewert JR. Boerhaave's syndrome: analysis of the literature and report of 18 new cases. Diseases of the Esophagus. 1997;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 82] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Wang J, Wang D, Chen J. Diagnostic challenge and surgical management of Boerhaave's syndrome: a case series. J Med Case Rep. 2021;15:553. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Spapen J, De Regt J, Nieboer K, Verfaillie G, Honoré PM, Spapen H. Boerhaave's Syndrome: Still a Diagnostic and Therapeutic Challenge in the 21st Century. Case Rep Crit Care. 2013;2013:161286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 9. | Carrozza F, Dragean C. Spontaneous Esophageal Rupture or Boerhaave's Syndrome. J Belg Soc Radiol. 2020;104:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | O'Kelly F, Lim KT, Cooke F, Ravi N, Reynolds JV. An unusual presentation of Boerhaave Syndrome: a case report. Cases J. 2009;2:8000. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Maier A, Pinter H, Anegg U, Fell B, Sankin O, Tomaselli F. Boerhaave's syndrome: a continuing challenge in thoracic surgery. Hepatogastroenterology 2001. [RCA] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Rassameehiran S, Klomjit S, Nugent K. Right-sided hydropneumothorax as a presenting symptom of Boerhaave's syndrome (spontaneous esophageal rupture). Proc (Bayl Univ Med Cent). 2015;28:344-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Korn O, Oñate JC, López R. Anatomy of the Boerhaave syndrome. Surgery. 2007;141:222-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |