Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6141
Peer-review started: October 26, 2021
First decision: December 17, 2021
Revised: December 27, 2021
Accepted: April 28, 2022
Article in press: April 28, 2022
Published online: June 26, 2022
Processing time: 233 Days and 12.2 Hours
In recent years, the cosmetic intervention related infections caused by nontuberculous mycobacteria (NTM) are increasing as the informal cosmetic treatments are performed. However, many dermatologists are inexperienced in the diagnosis and management of similar cases. Here we report a case of subcutaneous infection caused by Mycobacterium abscessus (M. abscessus) following cosmetic injections of botulinum toxin.
A 53-year-old woman presented with multiple abscesses and nodules on her forehead and both temporal sites for half a month after cosmetic injections of botulinum toxin. Her lesions did not show any alleviation after 2-wk prescription of antibiotics. Laboratory examinations indicated that she had no sign of immunodeficiency and the whole body of computed tomography did not find any systemic infection or diseases. The pathology of skin tissue showed inflammatory cell infiltration with the negative results of Periodic acid Schiff (PAS) and Acid-fast staining and the culture yielded no microbiome. Afterwards, the puncture on abscess was performed and M. abscessus was successfully isolated. The pathogen was identified by acid-fast staining and DNA sequencing. The patient was treated with the strategy of clarithromycin, ofloxacin, and amikacin according to the result of drug sensitivity test and got complete remission of the lesions.
The case presents the whole process of diagnosis and management of NTM infection after cosmetic intervention and highlights the diagnostic thoughts. In a word, the mycobacterium infection should be aware in patients after cosmetic performance.
Core Tip: The article reports a case of subcutaneous infection caused by Mycobacterium abscessus after cosmetic intervention. We present the medical history and whole process of diagnosis and management of the case and made a literature review of similar infections. The paper is trying to provide some more experience for dermatologists.
- Citation: Deng L, Luo YZ, Liu F, Yu XH. Subcutaneous infection caused by Mycobacterium abscessus following cosmetic injections of botulinum toxin: A case report. World J Clin Cases 2022; 10(18): 6141-6147
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6141.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6141
Nontuberculous mycobacteria (NTM) refer to mycobacteria other than Mycobacterium tuberculosis and leprosy with the common involved organs of the lung, bone, soft tissues, skin, and lymph nodes[1]. Mycobacterium abscessus (M. abscessus) is one of the common pathogens in NTM, which is a fast-growing mycobacterium causing skin and soft tissue infections. Meanwhile, the atypical mycobacterial infections are increasing at injection-related sites as the informal cosmetic treatments are performed, which deserves the attention of the cosmetic and medical supervision[2-4]. The case presented here is a subcutaneous infection caused by M. abscessus following cosmetic injections of botulinum toxin.
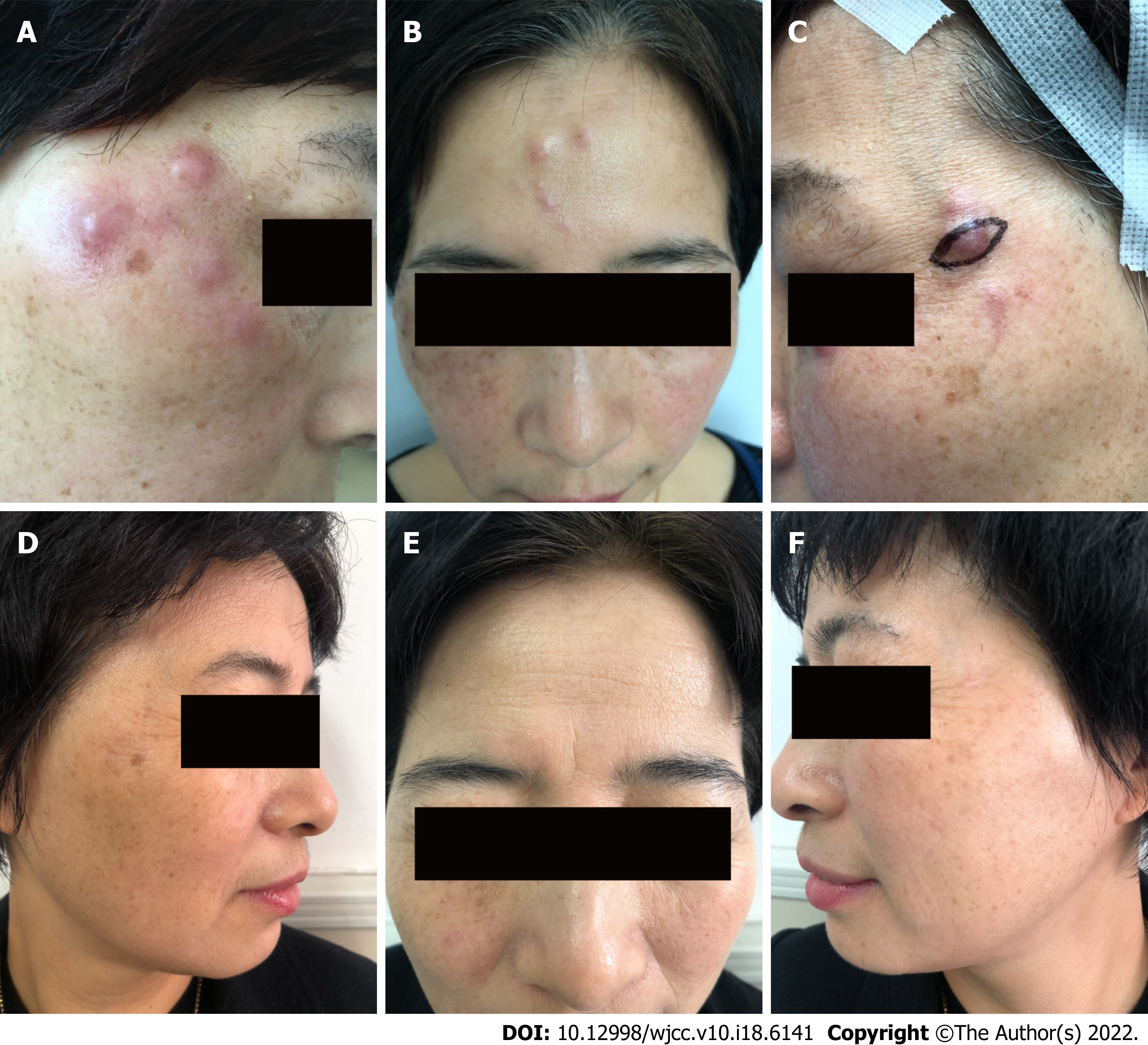
A 53-year old female patient visited our department with the complaint of multiple nodules for half a month on the forehead and both temporal sites after the injection of botulinum toxin (Figure 1A-C).
The lesions initially presented with erythema after 10 d of the injection then developed to nodules and abscesses after half a month. The patient did not have any concomitant symptoms such as fever, cough, fatigue, sweats, or diarrhea. She was prescribed with antibiotics for 2 wk without alleviation of the lesions.
The patient did not have any underlying disease or take any drugs in the past.
Nothing special.
Physical examination indicated multiple red papules, nodules, and abscesses on the forehead and both temporal sites with a diameter of 1-3 cm.
The routine blood, urine, and stool tests as well as kidney and liver function tests were in normal levels. The levels of C3, C4 and C-reactive protein were normal. The patient was negative for syphilis, HIV, antinuclear antibodies, and rheumatoid factor. CD3 and CD4 counts were done to check for any immunodeficiency and were within normal limits (Supplementary Table 1).
Computed tomography (CT) of the whole body did not find any systemic infection or diseases.
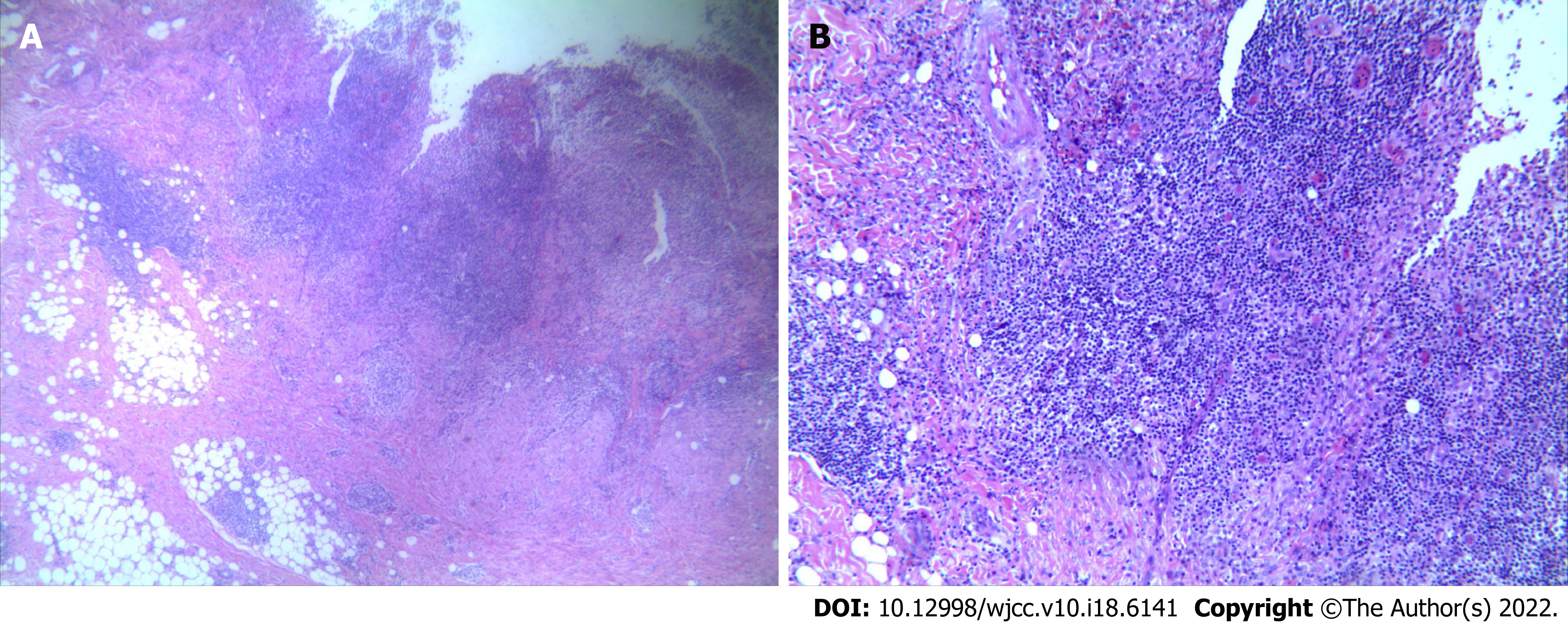
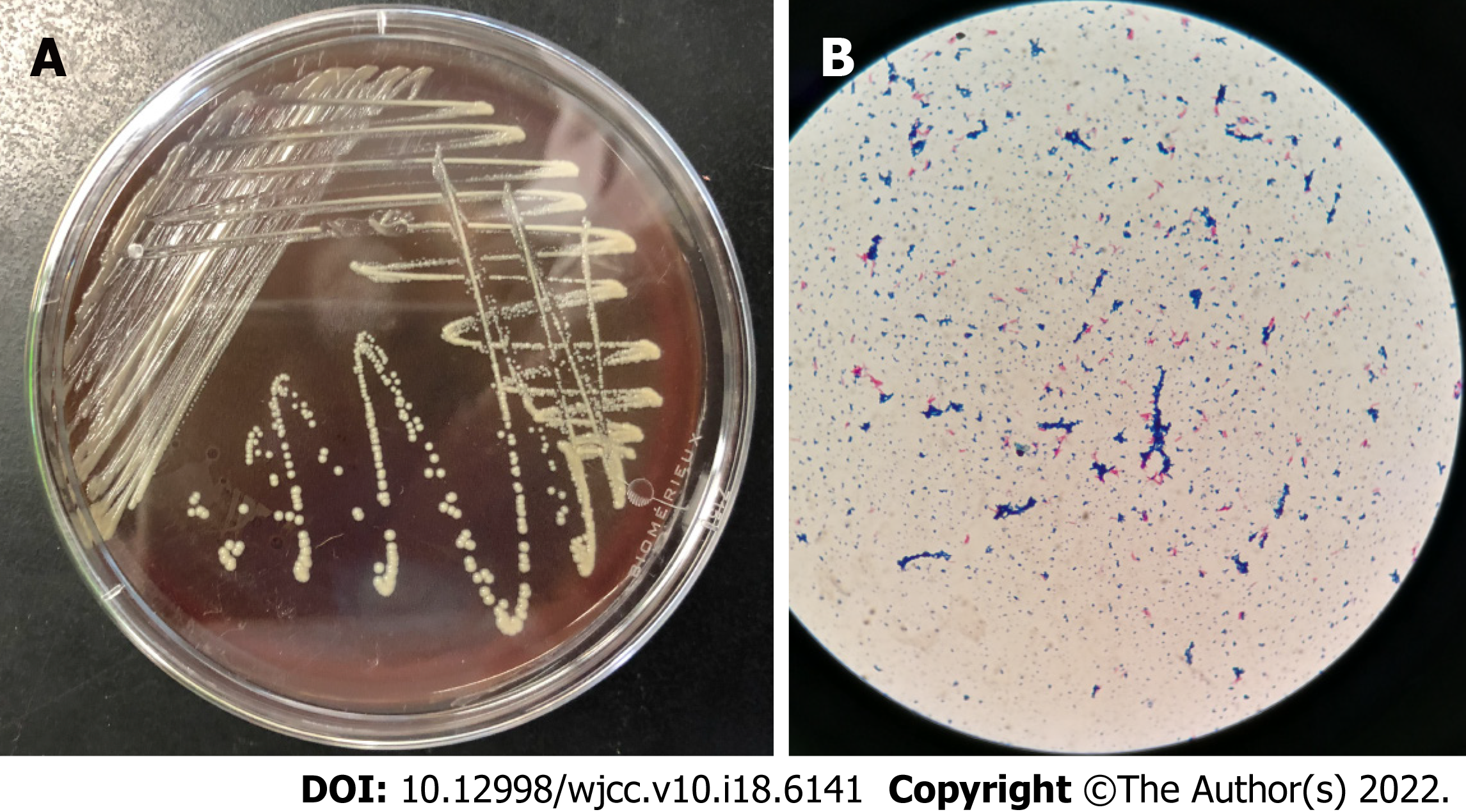
The patient underwent skin biopsy on the nodules of left temporal site. The pathology of skin tissue showed a large number of inflammatory cells including neutrophils, lymphocytes, and multinucleated giant cells distributed in the derma (Figure 2A and 2B). However, periodic acid Schiff (PAS) and acid-fast staining were negative. Meanwhile, the skin tissue did not yield any microbiome after culture on different media for bacteria, fungus, or mycobacterium. Considering the low biopsy- and culture-positive rate of some microorganisms, a puncture on abscess of right temporal site was further performed. Gray-white colonies were yielded after being cultured on Mycobacterium Roche's Medium (MRM) for 5 days at 35 °C (Figure 3A). Meanwhile, the pus was positive for acid-fast staining and M. abscessus was identified by DNA sequencing (Figure 3B). The drug sensitivity test indicated that the microbiome was sensitive to clarithromycin, moxifloxacin, azithromycin, cefoxitin, and amikacin, and was resistant to isoniazid, streptomycin, dapsone, and rifampicin (Supplementary Table 2).
The patient was initially intramuscularly injected with amikacin 0.2 g and given oral clarithromycin 0.25 g twice a day for 2 wk and then adjusted to moxifloxacin 0.4 g per day and clarithromycin 0.25 g twice a day because of dizziness and vomiting caused by amikacin.
The patient did not show any side effects and presented complete remission of the lesions during the subsequent treatment for 7 mo (Figure 1D-F).
With the development of un-standard invasive performance in cosmetic industry, related iatrogenic complications are increasing in the last two decades. Injection pain, local edema, erythema, and transient nausea are common complications with mild symptoms. Life-threatening complications are rarely seen, while severe idiosyncratic reactions can cause patients to die from shock and pseudoaneurysm of the superficial temporal artery may break and cause bleeding to death[5]. Infections are also common complications, which usually can be easily cured with empiric antibiotic therapy. However, atypical mycobacterial infections are increasing these years and resistant to regular antibiotic treatment. To meet the challenge of NTM diagnosis and management, we should learn more about it. In Table 1, previous cases of mycobacterial infections caused by cosmetic performance are reviewed[2-4,6-14], the results of which are consistent with the previous studies[1]. It is common to be seen in female patients aged 25 to 45 years. This phenomenon can be attributed to the fact that these people are more often seeking invasive cosmetic performance.
| No | Ref. | Sex/Age (yr) | Duration after injection (mo/wk/d) | Skin symptoms | Site of infection | Culture | Treatment and course | Outcome |
| P1 | The present case | F/53 | Botulinum toxin (1.5 mo) | Erythematousnodules | Cheek, forehead | M. abscessus | Clarithromycin, moxifloxacin, amikacin 2/d (7 mo) | Cure |
| P2 | Chen et al[2] | F/32 | Botulinum toxin (2 mo) | Nodules and abscesses | Forehead and periorbial areas | M. abscessus | Clarithromycin 250 mg 2/d, rifampicin 450 mg 1/d, and ethambutol 250 mg 3/d (3 mo) | Cure |
| P3 | Chen et al[2] | F/34 | Botulinum toxin (10 d) | Painful papules and nodules | Lower jaw, malar, and temple regions | M. abscessus | Clarithromycin 250 mg 2/d, rifampicin 450 mg 1/d (6 mo) | Cure |
| P4 | Mello et al[3] | F/28 | Sunflower oil, deoxycholate, sinetrol, and caffeine subcutaneous application (4 wk) | Pain and erythema | Abdomen and flanks | M. lentiflavum | Clarithromycin, 500 mg 2/d and levofloxacin 500 mg 1/d (8 mo) | Cure |
| P5 | Tan et al[4] | F/36.6 (28-45) (5 cases) | Autologous fat grafting for cosmetic breast augmentation (20 d) | Erythema, breast contour disruption, breast asymmetry | Breast | M. Fortuitum (2), M. abscessus (1), and M. chelonei (2) | Clarithromycin 500 mg 2/d, amikacin 800 mg 1/d, and imipenem 500 mg 4/d (54 wk) Azithromycin 500 mg 1/d, ethambutol 750 mg 1/d, rifampicin 600 mg 1/d (6 mo), and surgical debridement | Cure |
| P6 | Yeon et al[6] | F/34 | Botulinum toxin (3.5 mo) | Erythematousnodules | Left mandible | M. immunogemom | Clarithromycin 500 mg 2/d (7 m) | Cure |
| P7 | Fang et al[7] | F/28 | Botulinum toxin (2 wk) | Erythemaand painful nodules | Lower extremities | M. abscessus | Clarithromycin, moxifloxacin, and rifampicin (6 mo) | Cure |
| P8 | Thanas arnaksorn et al[8] | F/42 | Botulinum toxin (5 wk) | Erythematous nodules | Frontalis area and right orbicularis oculi area | Histopathologically confirmed | Clarithromycin 500 mg/d and levofloxacin500 mg/d (6 mo) | Cure |
| P9 | Saeb-Lima et al[9] | F/45 | Botulinum toxin (5 mo) | Erythematousplaques and nodules | Procerus muscle zone and the pars externa of orbicularis oculi muscle | Histopathologically confirmed | Clarithromycin, azithromycin, and rifampicin (40 d) | Cure |
| P10 | Hammond et al[10] | F/40 | Lipofilling (2 mo) | Multiple painful nodules | Buttock | M. chelonae | Clarithromycin 500 mg 2/d (2.5 mo), ciprofloxacin 500mg 2/d (3 mo), and surgery | Cure |
| P11 | Yoo et al[11] | F/56 | Filler injections (3 mo) | Nodules | Cheek | M. volinskyi | Doxycycline 100 mg 2/d and ciprofloxacin 750 mg 6/d (5 mo) | Cure |
| P12 | Fiore et al[12] | F/31 | Poly-L-lactic acid (3 mo) | Erythematous nodules | Cheek | M. mucogenicum | Ciprofloxacin 500 mg and clarithromycin 500 mg 2/d (6 mo) | Cure |
| P13 | Eustace et al[13] | M/28 | Hair transplant (2 mo) | Nodules | Sculp | M. abscessus | Clarithromycin 250 mg 2/d, doxycycline 100 mg 1/d (3 mo), and drainage | Cure |
| P14 | Yang et al[14] | F/29 | Facial injection with autologous fat (9 mo) | Abscesses | Temporal and lower orbital regions | M. abscessus | Moxifloxacin, clarithromycin, and ethambutol (12 mo) | Cure |
The rare pathogen of M. abscessus is the main mycobacteria isolated from lesions cultured, which can involve the skin, soft tissue, and lymph nodes in immunocompetent or immunosuppressed patients[1,15]. The cutaneous infection caused by M. abscessus generally occurs following surgery, subcutaneous injection, or acupuncture[16]. Because M. abscessus has a hydrophobic biofilm, by which M. abscessus can be resistant to disinfectants and heavy metals, and lead to nosocomial infections[17]. The lesions of the patient presented here develop at the injected point of botulinum toxin. We suspected that the infection may be caused by the non-standard aseptic operation and injection, surgery, equipment contamination, or intraoperative infection. Iatrogenic infections have become one of the common causes of fast-growing mycobacterial infection because of the unstandardized aseptic operation during injection and surgery causing an increase in opportunistic infections and great pain to patients. Therefore, when managing such cases, attention should be paid to these agents.
The skin lesions can be the initial symptoms or secondary to disseminated infections, which often present with multiple papules, herpes, nodules, erythema, or abscesses[1]. The initial symptoms of our patient presented as multiple erythema then developed to nodules and abscess. She was prescribed with multiple antibiotics but without remission of the lesions. The unspecific infection caused by fungus, M. tuberculosis, or NTM was suspected. Finally, the patient was diagnosed as having subcutaneous infection caused by M. abscessus. The golden standard for diagnosing NTM infections is histopathology and mycobacteria culture. Acid-fast staining is the most convenient and common laboratory test, while PCR sequencing and DNA chip technology have emerged as fast and accurate methods in identifying NTM[15]. However, the acid-fast staining of nodule of this patient was negative and did not yield any culture on MRM. Fortunately, the puncture fluid of abscess was positive for acid-fast staining and M. abscessus was yielded and identified by PCR sequencing. Therefore, once NTM infection is clinically suspected, multiple specimens should be tested by histopathology, culture, and molecular biology identification. The successful diagnosis of this patient depended on the awareness of mycobacterial infections and attitude of insistence.
NTM are intracellular colonies whose high hydrophobicity on the cell surface and cell wall permeability barrier make them resistant to traditional anti-tuberculosis drugs and difficult to treat[17]. M. abscessus is the most resistant strain of mycobacterium, and is highly resistant to traditional anti-tuberculosis drugs; hence, it needs to be tested for drug susceptibility when yielding positive cultures. M. abscessus is often sensitive to clarithromycin, amikacin, and cefoxitin. However, a single drug is easy to induce drug resistance according to the guidelines of the American Thoracic Society and the American Society of Infectious Diseases, therefore the combination of two kinds of sensitive drugs is recommended for treatment until the lesions are completely healed[18]. Meanwhile, drug susceptibility testing needs to be performed once culture of NTM is yielded to ensure the effective treatment.
NTM infection should be aware in patients with refractory lesions, particularly followed by cosmetic procedure. Moreover, the drug sensitivity test needs to be performed to obtain early diagnosis and appropriate treatment to avoid dissemination and deformity.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Corvino A, Italy; Hosoya S, Japan; Malekzadegan A, Iran S-Editor: Xing YX L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Chirasuthat P, Triyangkulsri K, Rutnin S, Chanprapaph K, Vachiramon V. Cutaneous nontuberculous mycobacterial infection in Thailand: A 7-year retrospective review. Medicine (Baltimore). 2020;99:e19355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Chen X, Jin Y, Torres KMT, Li B, Zhuo F, Ding X, Cai L, Zhang J, Zhou C. Mycobacterium abscessus cutaneous infection secondary to botulinum toxin injection: A report of 2 cases. JAAD Case Rep. 2019;5:982-984. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Mello RB, Moreira DN, Pereira ACG, Lustosa NR. Cutaneous infection by Mycobacterium lentiflavum after subcutaneous injection of lipolytic formula. An Bras Dermatol. 2020;95:511-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Tan LC, Li XY, Lu YG. Nontuberculous Mycobacteria Infection After Autologous Fat Grafting for Cosmetic Breast Augmentation. Ann Plast Surg. 2020;85:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Skaf GS, Domloj NT, Salameh JA, Atiyeh B. Pseudoaneurysm of the superficial temporal artery: a complication of botulinum toxin injection. Aesthetic Plast Surg. 2012;36:982-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Yeon J, Chan RCF, Fallah H. Infection with Mycobacterium immunogenum following botulinum toxin injection. Australas J Dermatol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Fang RY, Sun QN. Mycobacterium abscessus infections following injection of botulinum toxin. J Cosmet Dermatol. 2020;19:817-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Thanasarnaksorn W, Rattakul B, Suvanasuthi S, Sutthipisal N. Botulinum toxin type A injection-related suppurative granuloma: a case report. J Cosmet Laser Ther. 2019;21:422-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Saeb-Lima M, Solis-Arreola GV, Fernandez-Flores A. Mycobacterial infection after cosmetic procedure with botulinum toxin a. J Clin Diagn Res. 2015;9:WD01-WD02. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Hammond SE, Al-Bayati A, Joumblat N, Salgado CJ. Mycobacterium Chelonae Infection of the Buttocks Secondary to Lipofilling: A Case Report and Review of the Literature. Aesthetic Plast Surg. 2017;41:1150-1154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Yoo SJ, Lee KH, Jung SN, Heo ST. Facial skin and soft tissue infection caused by Mycobacterium wolinskyi associated with cosmetic proc edures. BMC Infect Dis. 2013;13:479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Fiore R 2nd, Miller R, Coffman SM. Mycobacterium mucogenicum infection following a cosmetic procedure with poly-L-lactic acid. J Drugs Dermatol. 2013;12:353-357. [PubMed] |
| 13. | Eustace K, Jolliffe V, Sahota A, Gholam K. Cutaneous Mycobacterium abscessus infection following hair transplant. Clin Exp Dermatol. 2016;41:768-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Yang P, Lu Y, Liu T, Zhou Y, Guo Y, Zhu J, Jia C, Chen L, Yang Q. Mycobacterium abscessus Infection After Facial Injection With Autologous Fat: A Case Report. Ann Plast Surg. 2017;78:138-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ Jr, Winthrop K; ATS Mycobacterial Diseases Subcommittee; American Thoracic Society; Infectious Disease Society of America. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175:367-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3867] [Cited by in RCA: 4189] [Article Influence: 232.7] [Reference Citation Analysis (0)] |
| 16. | Suganeswari G, Shah D, Anand AR. Intravitreal piperacillin-tazobactam in endophthalmitis caused by Mycobacterium abscessus in silico n e-filled eye: A case report. Indian J Ophthalmol. 2020;68:1471-1473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Henry F, Piérard-Franchimont C, Piérard GE. [Clinical case of the month. Rev Med Liege. 2005;60:7-10. [PubMed] |
| 18. | Lyu J, Jang HJ, Song JW, Choi CM, Oh YM, Lee SD, Kim WS, Kim DS, Shim TS. Outcomes in patients with Mycobacterium abscessus pulmonary disease treated with long-term injectable drugs. Respir Med. 2011;105:781-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 79] [Article Influence: 5.6] [Reference Citation Analysis (0)] |