Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6039
Peer-review started: December 13, 2021
First decision: February 14, 2022
Revised: March 1, 2022
Accepted: April 21, 2022
Article in press: April 21, 2022
Published online: June 26, 2022
Processing time: 185 Days and 14.3 Hours
Most complex renal stones are managed primarily with percutaneous nephrolithotomy (PCNL). However, PCNL is still a great challenge for surgeons because of poor comprehension on complex adjacent structures. Novel techniques are required to assist in planning and navigation.
To apply and evaluate the Hisense computer-assisted surgery (CAS) system in PCNL.
A total of 60 patients with complex renal stones were included. Thirty patients in the CAS group had three-dimensional (3D) virtual models constructed with the CAS system. The model assisted in planning and navigating in the CAS system. Thirty patients in the control group planned and navigated as standard PCNL, without the application of the CAS system. Success rate of one attempt, operation time, initial stone-free rate, decrease in hemoglobin, and complications were collected and analyzed.
There were no statistically significant differences in the baseline characteristics or planning characteristics. The success rate of one puncturing attempt (90% vs 67%, P = 0.028) and the initial stone-free rate (87% vs 63%, P = 0.037) were significantly higher in the CAS group. However, there were no statistically significant differences in the operation time (89.20 ± 29.60 min vs 92.33 ± 33.08 min, P = 0.859) or in the decrease in hemoglobin (11.07 ± 8.32 g/L vs 9.03 ± 11.72 g/L, P = 0.300) between the CAS group and the control group. No statistically significant differences in the incidence of complications (Clavien-Dindo grade ≥ 2) were found.
Compared with standard PCNL, CAS-assisted PCNL had advantages in terms of the puncturing success rate and stone-free rate. The Hisense CAS System was recommended to assist in preoperative planning and intraoperative navigation for an intuitive, precise and convenient PCNL.
Core Tip: Consisting of construction, display, simulation and measurement functions, the Hisense computer-assisted surgery (CAS) system is a novel and all-around software based on new generation of three-dimensional (3D) reconstruction. Compared with standard percutaneous nephrolithotomy (PCNL), CAS-assisted PCNL had advantages in terms of the puncturing success rate and stone-free rate. The CAS System was recommended to assist in preoperative planning and intraoperative navigation for an intuitive, precise and convenient PCNL.
- Citation: Qin F, Sun YF, Wang XN, Li B, Zhang ZL, Zhang MX, Xie F, Liu SH, Wang ZJ, Cao YC, Jiao W. Application of a novel computer-assisted surgery system in percutaneous nephrolithotomy: A controlled study. World J Clin Cases 2022; 10(18): 6039-6049
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6039.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6039
Renal stones, including large stones and multiple stones, are a common and intractable urological disease. Percutaneous nephrolithotomy (PCNL) has been recommended as the first-line treatment for renal stones that are larger than 2 cm[1,2]. In other cases of renal stones, PCNL is also an alternative treatment. However, it is difficult to achieve surgical competence in PCNL, especially for complex renal stones such as staghorn stones and multiple stones. Therefore, a great quantity of training is required for young surgeons. The study of the learning curve of a single surgeon suggested that competence in PCNL was reached after treating 60 cases and was excellent after treating 115 cases[3].
For excellent PCNL, novel techniques, including visual needles[4], three-dimensional (3D) printing[5], lasers[6], electromagnetic tracking[7] and virtual reality (VR)[8], are emerging to assist surgeons in understanding the regional anatomy and establishing percutaneous tracts. 3D reconstruction is also a novel technique[9] and has showed preliminary advantages in PCNL[10]. The structures around the stones are reconstructed from two-dimensional (2D) clinical imaging pictures to form 3D models for further display, planning and navigation. These models provide a comprehensive view to show the 3D relationship between the stones and adjacent structures, which cannot be provided by traditional 2D imaging, such as fluoroscopy, ultrasound (US) and computed tomography (CT).
The Hisense computer-assisted surgery (CAS) system, consisting of construction, display, simulation and measurement functions, is a software based on 3D reconstruction. The system has been applied in pediatric hepatectomy[11] and gastrectomy[12] and is helpful for accurate preoperative planning and intraoperative navigation. In the present study, we applied the CAS system in PCNL and first compared CAS-assisted PCNL (the CAS group) and standard PCNL (the control group) to evaluate the system.
It is a retrospective study. From October 2019 to October 2020, patients with complex renal stones, confirmed by preoperative computed tomography urography (CTU) and managed by PCNL in the Urological Department of the Affiliated Hospital of Qingdao University, were retrospectively enrolled in the study. Complex renal stones were defined as partial staghorn stones, complete staghorn stones or multiple stones. However, patients with history of operations, introduction of ureteral stents or nephrostomy tubes, existence of other disorders in the ipsilateral kidney, or absolute operative contraindications were excluded.
Thirty patients who met the selection criteria and underwent CAS-assisted PCNL were included as the CAS group. In CAS-assisted PCNL, patients had 3D virtual models constructed with the CTU images by the CAS system (Hisense Medicine, Qingdao, China), and the model assisted in planning and navigating in the CAS system. At the same time, 103 patients met the selection criteria and underwent standard PCNL. They were ranked according to the medical record number, and the first 30 patients were included into the study as the control group in a 1:1 ratio to the patients in the CAS group using the random number method. In standard PCNL, 2D axial, sagittal and coronal images from CTU aided in planning and navigating, without the application of the CAS system.
All surgeries were performed by the same surgical team. Ethics approval was obtained from the Ethics Committee of the Affiliated Hospital of Qingdao University (QYFYWZLL26370). Informed consent was obtained from all the patients for this study.
The CTU images, including the unenhanced, arterial, venous, and excretory phases, were obtained by a 64 multidetector row CT scanner (Siemens, Germany) with 1-mm step intervals. The scan delay times for the arterial, venous, and excretory phases were 25, 60, and 600-900 s, respectively, after intravenous injection of contrast material. Patients were advised to hold their breath in inspiration during the process.
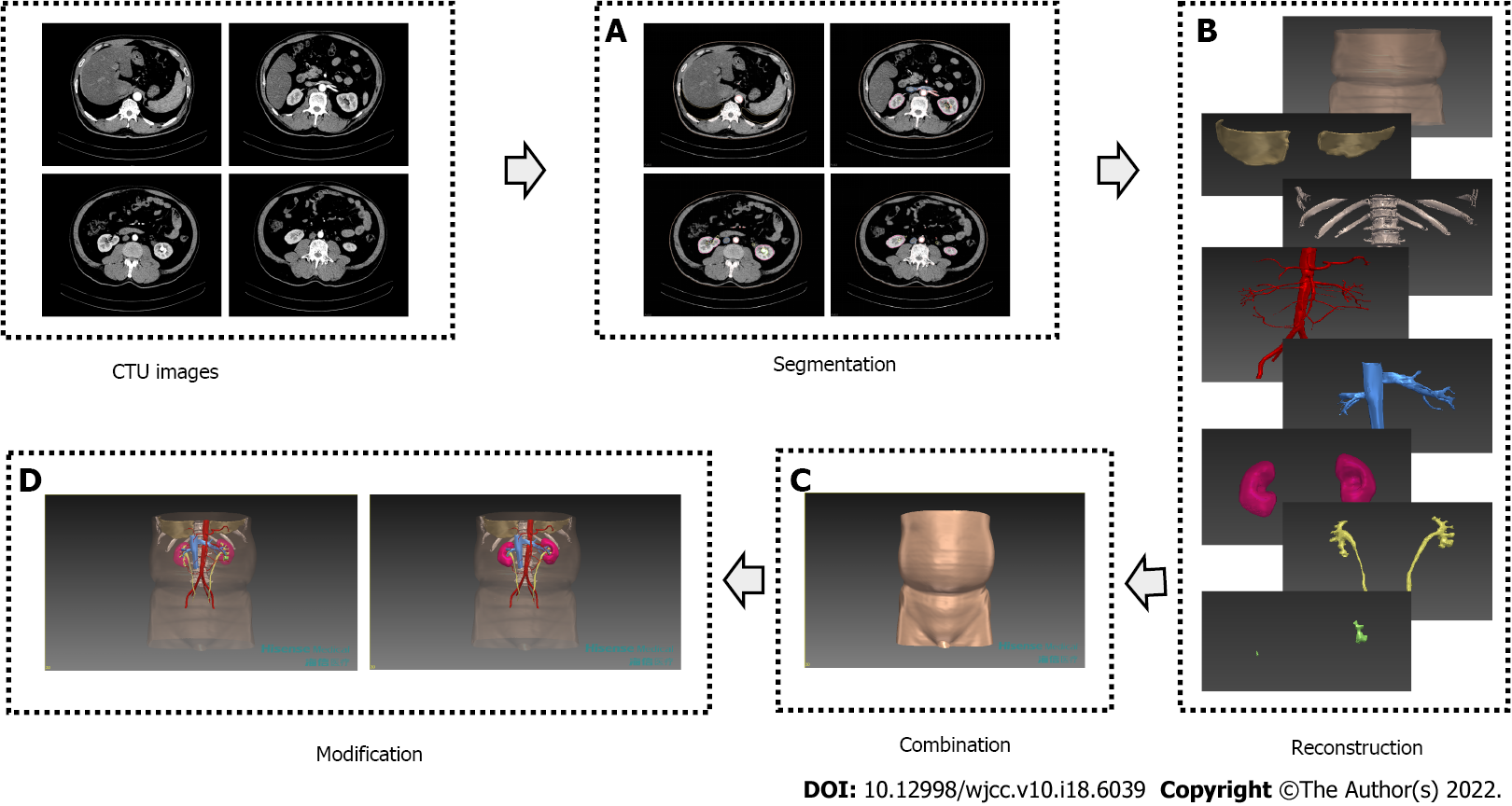
Construction of 3D virtual model: Four-phase images of the CTU were exported in Digital Imaging and Communications in Medicine format and were imported into the Hisense CAS system: (1) Segmentation: Stones, renal collecting system, ureters, renal parenchyma, renal vascular system, bottom of the thoracic cavity, spine, ribs, and skin were segmented from the images of different phases by the technique of region growing and threshold segmentation; (2) Reconstruction: The system processed the segmented structures for the 3D reconstruction of separate models using the techniques of maximum intensity projection, multiple planar reformation, curved planar reconstruction and volume rendering; (3) Combination: These separate models were registered and were integrated into a fusion model; and (4) Modification: After noise reduction, smoothing, dyeing and diaphaneity adjustments of each structure in the fusion model, a final 3D virtual model was obtained (Figure 1).
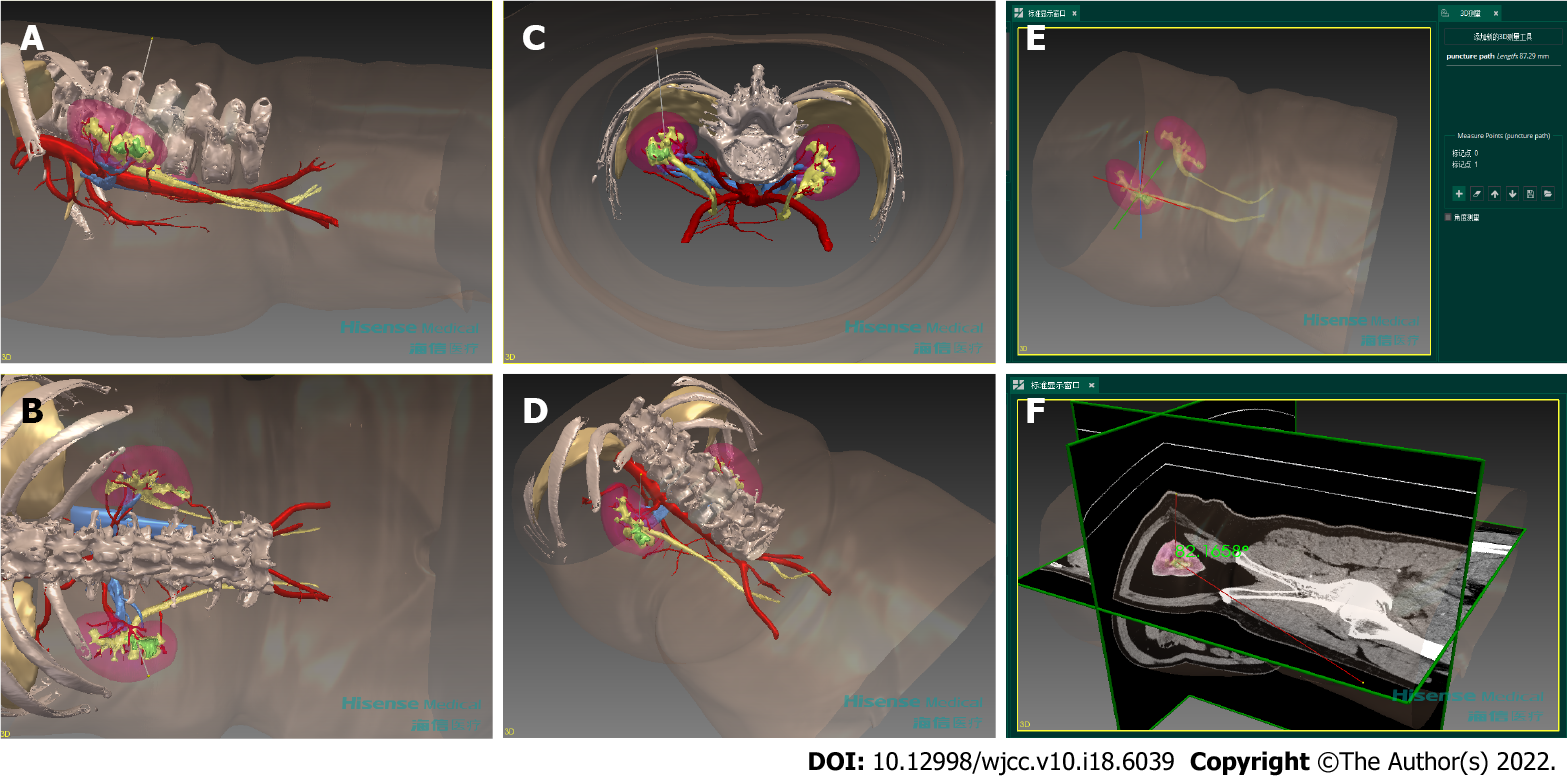
Planning for PCNL: With the simulation and measurement function of the CAS system, urological surgeons planned for the PCNL using the 3D virtual models. The planning was divided into three parts: the determination of ideal entry calyx, ideal puncture path and tract number: (1) Ideal entry calyx, where the nephoscope enters the collecting system, is defined as the calyx that is accessible to the renal pelvis and has the smallest length, the largest infundibular width, and the most "favorable calyces"[13]. A favorable calyx is defined as a calyx whose angle from the entry calyx is larger than 95°[14]. Stones in the renal pelvis and favorable calyces can be easily cleared from the ideal entry calyx. (2) The puncture path is the tract starting at the surface of the skin and ending at the boundary of the entry calyx. And ideal puncture path should have the shortest distance from the skin to the ideal entry calyx and should pass through the thinnest renal parenchyma, with the protection of adjacent vessels and organs. We moved virtual puncture path to find the ideal puncture path and recorded its depth (distance a) and direction (Figure 2). The direction was indicated by the angle between ideal puncture path and the axial plane (angle a), coronal plane (angle b), and sagittal plane (angle c). The intersection between ideal puncture path and skin is the puncture point. Then, we recorded the position of the point by the latitudinal distance to the posterior midline of the body (distance b) and the longitudinal distance to the inferior margin of the ipsilateral twelfth rib (distance c). And (3) Tract number. There are often no significant residual stones after the PCNL with one tract, based on above ideal entry calyx and puncture path. The second entry calyx and puncture path were needed to establish another tract when significant residual stones were present. The planning process of the second tract was the same as that of the first tract. A third tract was not established for the concern of increased injuries and bleeding. Repeated simulation could be performed if previous planning was not satisfactory.
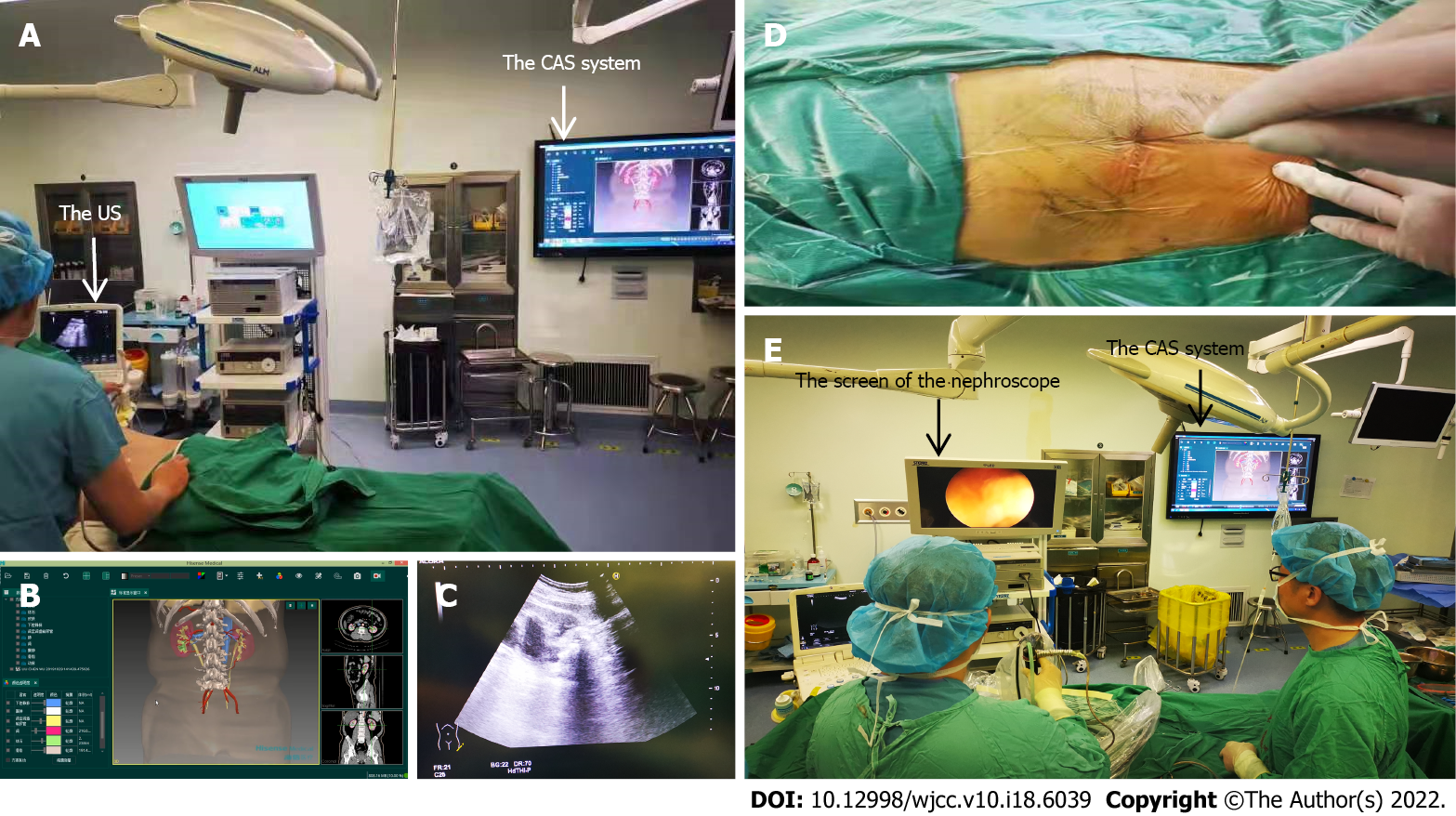
Navigation for PCNL: The 3D model and PCNL plan obtained from the CAS system were applied to navigate the PCNL. During the puncture phase, we first located the actual puncture point with distances b and c. Then, we set the direction of the puncture needle by angles a, b and c. With the help of the US (Hitachi, Japan), we punctured ideal entry calyx from the actual puncture point along the direction of the puncture needle, and the puncture depth was approximately the distance a. US was mainly used to verify the position of ideal entry calyx and to adjust the puncture path. Tract number was determined as mentioned in the PCNL plan. The puncture process was performed while the patients were in inspiration. During the tract dilation phase and the stone removal phase, it was the same as a standard PCNL. During all phases, the 3D model was shown on the screen using the display function of the CAS system. The 3D model could be magnified, rotated and translated to meet surgeons' requests. Stones, the collecting system, adjacent vessels and organs could be viewed in all directions to find stones and to avoid injuries (Figure 3).
After general anesthesia, the patient was placed in the lithotomy position, and a ureteral catheter was placed for artificial hydronephrosis. Then, the patient was placed into the prone position and underwent main surgical procedure, including puncture phase, tract dilation phase and stone removal phase, with the help of the US. The tract was dilated to 24F. A 6F ureteral stent and a 14F nephrostomy tube were placed at the end of the surgery. CT was performed within 1 mo after the surgery. "Stone-free" was defined as no stone fragments or residual fragments present that more than 4 mm in diameter.
Age, gender, body mass index (BMI), dilation of the collecting system, as well as side, type, density and sectional area of stones were recorded as the baseline characteristics. Entry calyx, tract length and tract number were recorded as the planning characteristics. Finally, the success rate of one attempt, operation time, initial stone-free rate, decrease in hemoglobin and complications (Clavien-Dindo grade ≥ 2) were analyzed. Initial stone-free rate was the proportion of patients who were "stone-free" after the first-stage PCNL.
Continuous data, expressed as the mean and standard deviation (SD), were analyzed by Student’s t test or the Mann-Whitney U test. Categorical variables, shown as the number and percentage, were analyzed by the chi-square or Fisher’s exact test. Statistical analyses were performed using SPSS version 23. P < 0.05 was regarded as statistically significant.
Sixty patients were included in the study: 30 in the CAS group and 30 in the control group. There were no statistically significant differences in age, gender, BMI, malformation of the collecting system, dilation of the collecting system, stone side, stone type, stone density or stone sectional area between the two groups (Table 1).
| Characteristics | CAS group (n = 30) | Control group (n = 30) | P value |
| Age, yr, mean ± SD | 52.30 ± 14.37 | 49.57 ± 13.58 | 0.452 |
| Gender, n (%) | 0.301 | ||
| Male | 14 (47) | 18 (60) | |
| Female | 16 (53) | 12 (40) | |
| BMI, kg/m2, mean ± SD | 25.24 ± 3.58 | 25.29 ± 5.12 | 0.968 |
| Dilation of the collecting system1, n (%) | 0.635 | ||
| No or mild | 18 (60) | 20 (66) | |
| Moderate | 8 (27) | 5 (17) | |
| Severe | 4 (13) | 5 (17) | |
| Stone side, n (%) | 0.426 | ||
| Left | 17 (57) | 20 (67) | |
| Right | 13 (43) | 10 (33) | |
| Stone type, n (%) | 0.434 | ||
| Partial staghorn stone | 4 (13) | 8 (27) | |
| Complete staghorn stone | 6 (20) | 5 (17) | |
| Multiple stone | 20 (67) | 17 (56) | |
| Stone density, Hounsfield units, mean ± SD | 915.15 ± 334.85 | 824.69 ± 245.73 | 0.238 |
| Stone sectional area, mm2, mean ± SD | 562.95 ± 405.58 | 497.59 ± 566.88 | 0.174 |
There were 6 upper calyces, 17 middle calyces, and 7 Lower calyces selected to be the entry calyces in the CAS group, while there were 3 upper calyces, 22 middle calyces, and 5 lower calyces selected to be the entry calyces in the control group. Most surgeries were completed with one tract (87% vs 90%) in the CAS group and the control group. The tract lengths in the CAS group and the control group were 76.03 ± 13.26 mm and 82.53 ± 17.58 mm, respectively. No statistically significant differences were found in the planning characteristics between the two groups (Table 2).
A total of 27/30 punctures in the CAS group and 20/30 in the control group were successful after just one attempt. The success rate of one puncturing attempt was significantly higher in the CAS group (90% vs 67%, P = 0.028). 26/30 surgeries in the CAS group and 19/30 in the control group achieved "stone-free", and the initial stone-free rate was significantly different between the two groups (87% vs 63%, P = 0.037). However, there were no statistically significant differences in the operation time (89.20 ± 29.60 min vs 92.33 ± 33.08 min, P = 0.859) or the decrease in hemoglobin (11.07 ± 8.32 g/L vs 9.03 ± 11.72 g/L, P = 0.300) between the CAS group and the control group. Bleeding necessitating blood transfusion was observed in 1 patient in the CAS group and 1 patient in the control group. Urinary tract infection necessitating therapeutic antibiotics or enhanced supportive therapy was observed in 2 patients in the CAS group and 2 patients in the control group. No injuries to adjacent structures were observed in the two groups. There were no statistically significant differences in the incidence of these complications (Table 3).
| Characteristics | CAS group (n = 30) | Control group(n = 30) | P value |
| Success rate of one puncturing attempt, n (%) | 27 (90) | 20 (67) | 0.028 |
| Operation time, min, mean ± SD | 89.20 ± 29.60 | 92.33 ± 33.08 | 0.859 |
| Decrease in hemoglobin, g/L, mean ± SD | 11.07 ± 8.32 | 9.03 ± 11.72 | 0.300 |
| Bleeding1, n (%) | 1 (3) | 1 (3) | 1.000 |
| Urinary tract infection1, n (%) | 2 (7) | 2 (7) | 1.000 |
| Injury1, n (%) | 0 (0) | 0 (0) | - |
| Initial stone-free rate, n (%) | 26 (87) | 19 (63) | 0.037 |
Most complex renal stones are managed primarily with PCNL[15]. Preoperative planning based on CTU is recommended[16], and intraoperative navigation with fluoroscopy or US is commonly used. However, PCNL is still a great challenge for surgeons because of low stone-free rate and high complication rate[17]. The most critical step to meet the challenge is the establishment of perfect tracts from the skin to the entry calyces. For higher stone free rate and lower complication rate, we applied this CAS system into PCNL, especially to establish the tract.
Traditional studies tended to perform preoperative planning with 2D CT images[18]. It was difficult to display overall 3D views in the simulation processes and the 3D precise measurements of each parameter. The surgeon had to reconstruct an overall view in mind, which relied on a long-team learning and was easily influenced by subjective judgment. The CAS system displayed a direct and objective 3D model for planning. The size, number, shape, position and adjacent structures of stones were evaluated in a panoramic view, and ideal entry calyces were selected. During the simulation, 3D puncture paths from the skin to the calyces were placed and were adjusted to obtain minimal injury to adjacent vessels and organs. It is obvious that measurement with 2D CT images cannot provide direct data of the 3D structures. The calculation method for 3D data obtained from 2D CT in PCNL was reported[19], but the process was also complex. In the CAS system, selected lengths or angles in 3D space were automatically measured and recorded with the parameters. The 3D planning from the CAS system assisted surgeons in making more precise surgeries.
The intraoperative navigation for PCNL was traditionally provided by fluoroscopy or US. The repetitive use of fluoroscopy or US was needed to make suitable percutaneous tracts. Novel techniques have helped reduce the radiation exposure and improve the accuracy during navigation, such as laser-guided puncture[6], ureteroscopy-assisted puncture[20], puncture with visual needles[4], marker-based tracking with iPADs[21] and electromagnetic tracking[7]. Navigation of the CAS system was mainly dependent on preoperative planning parameters rather than intraoperative techniques, which is different from the traditional imaging and novel techniques mentioned above. In addition, during the operation, the shape and position of stones and adjacent structures in display also gave reference to the location and adjustment of the tract. Perfect preoperative preparation and intraoperative reference reduced the repetitive use of fluoroscopy or US during the operation, especially when surgeons made percutaneous tracts. Navigation from the CAS system simplified the process for PCNL, making it more convenient. Surgeons also received less radiation exposure when the use of fluoroscopy was reduced.
The CAS system assisted PCNL in the preoperative planning and intraoperative navigation, and construction of a 3D model was a fundamental process. Initial 3D models were constructed from the excretory phase of contrast CT or CTU. Although adjacent structures were indistinct and incomplete, those models showed the relationship between stones and the collecting system, resulting in a low number of punctures[22]. The new generation of 3D reconstruction usually collects images from four phases of CTU. Structures were segmented from the phase in which they were most distinct. In particular, because of the clear display of renal arteries, segmental arteries and main branches, which did not exist in previous 3D renal pelvis model[22], injury to the renal artery system was generally avoided. In addition, noise reduction, smoothing and dyeing made structures more distinct from each other, and the transparency adjustments of the skin, kidney and collecting system made stones clearer, which improved the visual effect[23].
At present, a few studies have reported the application of the new generation of 3D reconstruction in PCNL. Tsaturyan et al[23] described technical details of 3D reconstruction in 3 patients. Li et al[9] reported 3D reconstruction in a cohort of 15 patients and provide reference in planning strategy and evaluation indicators. But these pilot studies did not include a control group. The study of Huang et al[10] seemed to be the only controlled study, in which they verified the advantages of the technique in reducing number of punctures, number of tracts and volume of bleeding. Compared with our study, they had a larger sample size, but they adopted dual-source CT in the control group, which was not a standard imaging method. Besides, extra softwares were often used for post-processing procedures after 3D reconstruction in mentioned studies. 3D reconstruction and post-processing procedures were all performed in the CAS system in our study.
The perioperative characteristics showed the preliminary advantages of the CAS system. In the present study, demographic characteristics and stone characteristics that may influence the stone-free rate[24] were analyzed, and the patients in the two groups were relatively homogeneous without significant differences. Because of the absence of preoperative ipsilateral lesions or operations and the absence of second-stage surgeries, the initial stone-free rate accurately reflected the efficiency of the first-stage surgeries. The CAS group obtained a higher initial stone-free rate. Under the limitation of tract number, establishing efficient tracts to remove as many stones as possible is helpful to improve the stone-free rate[5]. We think that the display of the 3D models in the CAS system helped surgeons understand the 3D relationship between structures, which was conducive to the establishment of efficient tracts. In addition, accurate 3D measurement enabled the morphometry to be applied to the establishment of efficient tracts. For example, the angle between the entry calyx and the calyx to be reached is an independent predictive factor for accessing a particular calyx[14]. Therefore, we compared the measured data of the included angles of calyces to select ideal entry calyces. We also found a significantly higher success rate of one attempt in the CAS group, and this may be related to extra help from the CAS system. The quantitative planning data and intuitive reference of the 3D models increased the success rate of one attempt in the CAS group. Infection, bleeding and injury were major complications of PCNL[25], but most of these complications could be treated with conservative management[26]. Therefore, we focused on complications whose Clavien-Dindo grade ≥ 2. The CAS system seemed to help reduce bleeding due to the visualization of the renal vascular system, but no significant differences were found in the incidence of any complication. More patients are needed to explore the influence of the system on the development of complications.
We applied an intuitive, precise and convenient computer-assisted surgery system in PCNL and the new generation of 3D reconstruction was the key technique. The controlled study showed advantages in terms of the puncturing success rate and stone-free rate. In the future, resident training and patient care education may benefit from the system. The system and planning parameters will also promote the combination with other techniques and the application of novel techniques such as VR[8] and robot-assisted surgery[27] in PCNL. However, there are several limitations in this study. Patients were in the supine position when the CTU images were obtained, but they were in the prone position during the surgery. There was a change in the organ position between the two positions, which may alter the tract angles and injury rates[28]. Patients were advised to hold their breath for still preoperative images, but respiratory movement during the surgery could not be avoided. The system failed to provide the data and images in real time. Therefore, we reserved ultrasound to observe respiratory movement and the deformation of tissues for adjustments during surgery. In addition, further study is required due the lack of data from the tract dilation phase and stone removal phase. More patients should be included to explore the influence of the system on the development of complications. The system adds additional costs and procedures to the treatment, which need to be reduced and simplified to promote the clinical application of the system.
With multiple functions of the Hisense CAS system, an intuitive, precise and convenient PCNL could be achieved. The 3D construction of the model was the first and fundamental step, in which the new generation of 3D reconstruction was the key technique. This controlled study demonstrated the advantages of CAS-assisted PCNL in terms of the success rate of using only one puncturing attempt and the initial stone-free rate over standard PCNL. The System was recommended to assist in preoperative planning and intraoperative navigation for PCNL.
Percutaneous nephrolithotomy (PCNL) is still a great challenge for surgeons because of poor comprehension on complex adjacent structures.
Novel techniques are required to assist in planning and navigation.
To apply and evaluate the Hisense computer-assisted surgery (CAS) system in PCNL.
A total of 60 patients with complex renal stones were included. CAS-assisted PCNL (the CAS group) and standard PCNL (the control group) were compared in a retrospective study. Success rate of one attempt, operation time, initial stone-free rate, decrease in hemoglobin, and complications were collected and analyzed.
The success rate of one puncturing attempt (90% vs 67%, P = 0.028) and the initial stone-free rate (87% vs 63%, P = 0.037) were significantly higher in the CAS group. Compared with standard PCNL, CAS-assisted PCNL had advantages in terms of the puncturing success rate and stone-free rate.
The Hisense CAS System was recommended to assist in preoperative planning and intraoperative navigation for an intuitive, precise and convenient PCNL.
Consisting of construction, display, simulation and measurement functions, the CAS system is a novel and all-around software based on new generation of three-dimensional (3D) reconstruction. Compared with standard PCNL, CAS-assisted PCNL had advantages in terms of the puncturing success rate and stone-free rate. The CAS System was recommended to assist in preoperative planning and intraoperative navigation for an intuitive, precise and convenient PCNL.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gadelkareem RA, Egypt; Shahriari M, Iran; Șurlin VM, Romania S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Pradère B, Doizi S, Proietti S, Brachlow J, Traxer O. Evaluation of Guidelines for Surgical Management of Urolithiasis. J Urol. 2018;199:1267-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 2. | Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, Knoll T. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol. 2016;69:475-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 775] [Cited by in RCA: 1094] [Article Influence: 109.4] [Reference Citation Analysis (0)] |
| 3. | Allen D, O'Brien T, Tiptaft R, Glass J. Defining the learning curve for percutaneous nephrolithotomy. J Endourol. 2005;19:279-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 86] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Zhang J, Kang N, Jiang Y, Zhang J. Microperc with self-assembled fr 4.85 visual needle and ureteral access sheath. J Invest Surg. 2021;1-8. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Xu Y, Yuan Y, Cai Y, Li X, Wan S, Xu G. Use 3D printing technology to enhance stone free rate in single tract percutaneous nephrolithotomy for the treatment of staghorn stones. Urolithiasis. 2020;48:509-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Wu J, Zhou P, Luo X, Hao Z, Lu C, Zhang H, Zhou T, Xu S. Novel laser positioning navigation to aid puncture during percutaneous nephrolithotomy: a preliminary report. World J Urol. 2019;37:1189-1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Rodrigues PL, Vilaça JL, Oliveira C, Cicione A, Rassweiler J, Fonseca J, Rodrigues NF, Correia-Pinto J, Lima E. Collecting system percutaneous access using real-time tracking sensors: first pig model in vivo experience. J Urol. 2013;190:1932-1937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Farcas M, Reynolds LF, Lee JY. Simulation-Based Percutaneous Renal Access Training: Evaluating a Novel 3D Immersive Virtual Reality Platform. J Endourol. 2021;35:695-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Li H, Chen Y, Liu C, Li B, Xu K, Bao S. Construction of a three-dimensional model of renal stones: comprehensive planning for percutaneous nephrolithotomy and assistance in surgery. World J Urol. 2013;31:1587-1592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Huang YS, Zhu XS, Wan GY, Zhu ZW, Huang HP. Application of simulated puncture in percutaneous nephrolithotomy. Eur Rev Med Pharmacol Sci. 2021;25:190-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Zhang G, Zhou XJ, Zhu CZ, Dong Q, Su L. Usefulness of three-dimensional(3D) simulation software in hepatectomy for pediatric hepatoblastoma. Surg Oncol. 2016;25:236-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Liu H, Wang F, Liu B, Zheng Z, Zhao J, Zhang J. Application of three-dimensional reconstruction with a Hisense computer-assisted system in upper pancreatic lymph node dissection during laparoscopic-assisted radical gastrectomy. Asian J Surg. 2021;44:730-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Mishra S, Sabnis RB, Desai M. Staghorn morphometry: a new tool for clinical classification and prediction model for percutaneous nephrolithotomy monotherapy. J Endourol. 2012;26:6-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | Guglielmetti GB, Danilovic A, Torricelli FC, Coelho RF, Mazzucchi E, Srougi M. Predicting calyceal access for percutaneous nephrolithotomy with computed tomography multiplanar reconstruction. Clinics (Sao Paulo). 2013;68:892-895. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Ghani KR, Andonian S, Bultitude M, Desai M, Giusti G, Okhunov Z, Preminger GM, de la Rosette J. Percutaneous Nephrolithotomy: Update, Trends, and Future Directions. Eur Urol. 2016;70:382-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 144] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 16. | Thiruchelvam N, Mostafid H, Ubhayakar G. Planning percutaneous nephrolithotomy using multidetector computed tomography urography, multiplanar reconstruction and three-dimensional reformatting. BJU Int. 2005;95:1280-1284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 57] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Desai M, De Lisa A, Turna B, Rioja J, Walfridsson H, D'Addessi A, Wong C; Rosette On Behalf Of The Croes Pcnl Study Group J. The clinical research office of the endourological society percutaneous nephrolithotomy global study: Staghorn vs nonstaghorn stones. J Endourol. 2011;25:1263-1268. [RCA] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 112] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 18. | Fang YQ, Wu JY, Li TC, Zheng HF, Liang GC, Chen YX, Hong XB, Cai WZ, Zang ZJ, Di JM. Computer tomography urography assisted real-time ultrasound-guided percutaneous nephrolithotomy on renal calculus. Medicine (Baltimore). 2017;96:e7215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Akand M, Buyukaslan A, Servi S, Civcik L. A hypothetical method for calculation of the access point, direction angle and access angle for percutaneous nephrolithotomy. Med Hypotheses. 2019;124:101-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Lima E, Rodrigues PL, Mota P, Carvalho N, Dias E, Correia-Pinto J, Autorino R, Vilaça JL. Ureteroscopy-assisted Percutaneous Kidney Access Made Easy: First Clinical Experience with a Novel Navigation System Using Electromagnetic Guidance (IDEAL Stage 1). Eur Urol. 2017;72:610-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 21. | Rassweiler-Seyfried MC, Rassweiler JJ, Weiss C, Müller M, Meinzer HP, Maier-Hein L, Klein JT. iPad-assisted percutaneous nephrolithotomy (PCNL): a matched pair analysis compared to standard PCNL. World J Urol. 2020;38:447-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 22. | Brehmer M, Beckman MO, Magnusson A. Three-dimensional computed tomography planning improves percutaneous stone surgery. Scand J Urol. 2014;48:316-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Tsaturyan A, Bellin A, Barbuto S, Zampakis P, Ntzanis E, Lattarulo M, Kalogeropoulou C, Liatsikos E, Kallidonis P; Collaborators. Technical aspects to maximize the hyperaccuracy three-dimensional (HA3D™) computed tomography reconstruction for kidney stones surgery: a pilot study. Urolithiasis. 2021;49:559-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Biswas K, Gupta SK, Tak GR, Ganpule AP, Sabnis RB, Desai MR. Comparison of STONE score, Guy's stone score and Clinical Research Office of the Endourological Society (CROES) score as predictive tools for percutaneous nephrolithotomy outcome: a prospective study. BJU Int. 2020;126:494-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, Tefekli A; CROES PCNL Study Group. The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: indications, complications, and outcomes in 5803 patients. J Endourol. 2011;25:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 543] [Article Influence: 38.8] [Reference Citation Analysis (1)] |
| 26. | Kyriazis I, Panagopoulos V, Kallidonis P, Özsoy M, Vasilas M, Liatsikos E. Complications in percutaneous nephrolithotomy. World J Urol. 2015;33:1069-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 27. | Oo MM, Gandhi HR, Chong KT, Goh JQ, Ng KW, Hein AT, Tan YK. Automated Needle Targeting with X-ray (ANT-X) - Robot-assisted device for percutaneous nephrolithotomy (PCNL) with its first successful use in human. J Endourol. 2021;35:e919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 28. | Marchini GS, Berto FC, Vicentini FC, Shan CJ, Srougi M, Mazzucchi E. Preoperative planning with noncontrast computed tomography in the prone and supine position for percutaneous nephrolithotomy: a practical overview. J Endourol. 2015;29:6-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |