Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5816
Peer-review started: December 15, 2021
First decision: January 26, 2022
Revised: January 31, 2022
Accepted: April 4, 2022
Article in press: April 4, 2022
Published online: June 16, 2022
Processing time: 175 Days and 17.9 Hours
Vertical root fracture (VRF) is one of the most common reasons for tooth extraction, although various methods have been applied for saving teeth with VRF.
This case report describes a woman who had a sinus tract on the labial gingiva of the left maxillary central incisor for past two months. Periodontal probing revealed an 8–10 mm deep, narrow, isolated pocket on the palatal side of the tooth. Clinical and radiographic examination confirmed a longitudinal root fracture. A new approach using a combination of resin and iRoot BP Plus through intentional replantation was used for the treatment of the tooth. At one-year follow-up, the tooth remained asymptomatic with normal periodontal probing depth, and radiographic images showed almost normal bone and periodontal structures around the root.
This new approach may be developed as an effective method for saving teeth with VRF.
Core Tip: This case report proposes a new approach for the treatment of teeth with vertical root fracture (VRF) using both resin and iRoot BP Plus through intentional replantation. This approach may be developed as an effective method to save teeth with VRF.
- Citation: Zhong X, Yan P, Fan W. New approach for the treatment of vertical root fracture of teeth: A case report and review of literature. World J Clin Cases 2022; 10(17): 5816-5824
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5816.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5816
Vertical root fracture (VRF) is a longitudinally oriented fracture of the root and can be classified as an incomplete or complete VRF based on the degree of separation of the fragments according to Leubke’s classification[1-4]. VRF is a serious complication with poor prognosis in endodontically treated teeth. The overall prevalence of VRF reported in retrospective studies is 3%–5%, but the prevalence of VRF in endodontically treated teeth is approximately 3.69%–25%[1,3]. Even if extraction is usually the first choice of management for teeth with VRF, various other methods to preserve the teeth have also been described in many case reports, such as using adhesive composite resin[4-6], CO2 and Nd:YAG laser[7], mineral trioxide aggregates (MTAs)[8,9] and biodentine[10,11].
Adhesive composite resin is commonly used to bond fractured segments owing to their superior adhesive strength. Intentional replantation combined with bonding of fractured segments using adhesive composite resin has been reported as a successful treatment method for preserving teeth with VRF. Despite this, owing to the poor tissue attachment to the resin surface, deep and narrow periodontal pockets along the bonded fracture could easily recur.
iRoot BP Plus is a ready-to-use calcium silicate-based bioceramic material suitable for repairing various root canal perforations or resorptions because of its ability to induce tissue attachment and mineralization[12-15]. Based on its excellent biological features, iRoot BP Plus is an ideal material for repairing VRF. However, the bond strength between iRoot BP Plus and dentin is not as strong as that of the adhesive composite resin when holding the fractured segments in position[16].
Based on these concerns, in the present case combination of adhesive composite resin and iRoot BP Plus was used to repair a VRF through intentional replantation. This new approach may be developed as an effective method for saving teeth with VRF. This case report was prepared according to the Preferred Reporting Items for Case Reports in Endodontics (PRICE) 2020[17].
A 27-year-old Chinese woman was referred to our department for treatment of pustules on the labial gingiva of the maxillary anterior teeth.
The pustule occurred two months ago, and the patient reported that tooth #9 (left maxillary central incisor) had undergone root canal treatment (RCT) and full crown restoration several years ago.
The patient denied any relevant past medical history.
No relevant personal and family history.
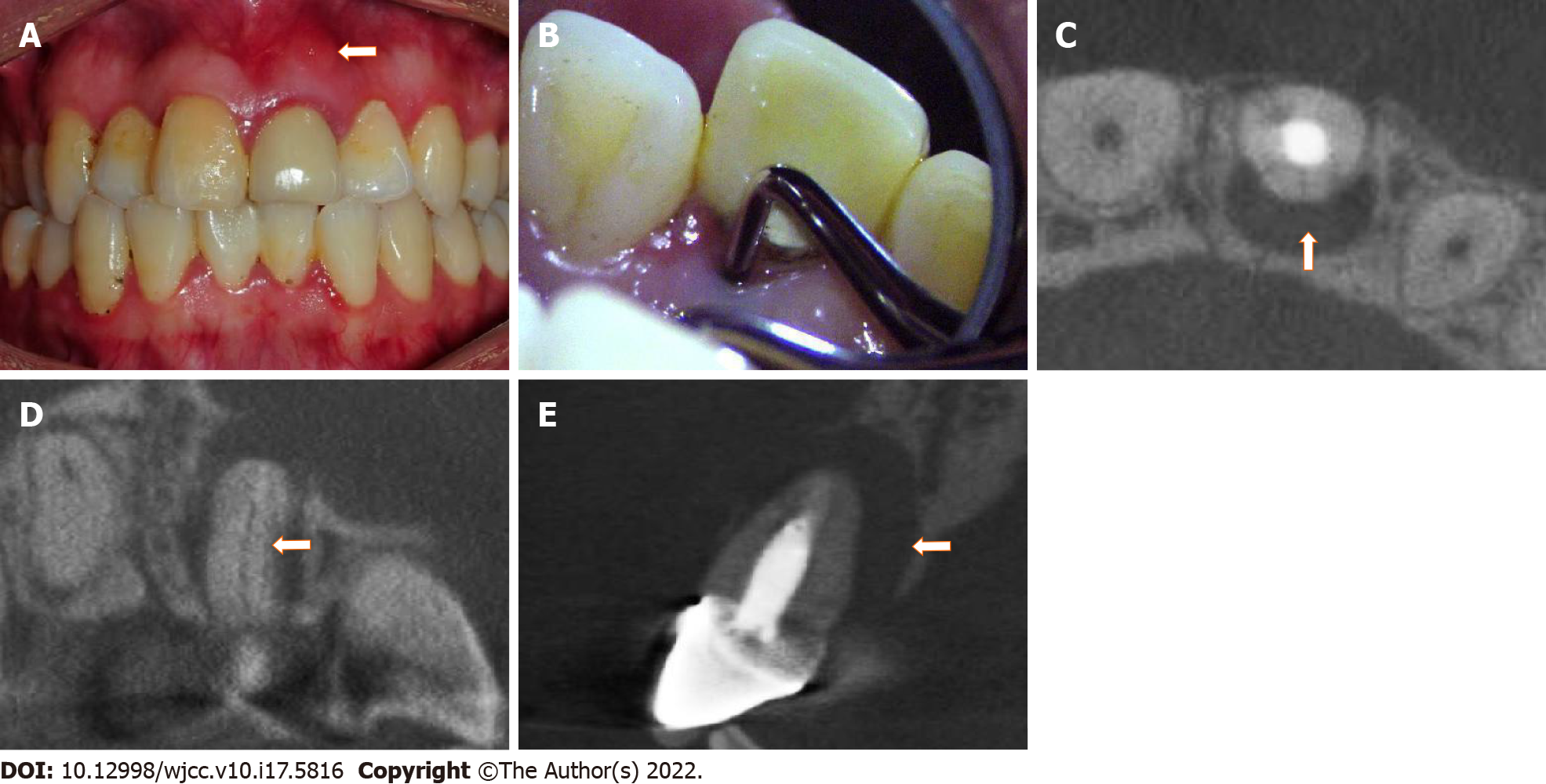
Intraoral examination revealed that tooth #9 was restored with a full crown and that there was a sinus tract on the labial gingival mucosa near the apical area of tooth #9 (Figure 1A). The tooth was sensitive to vertical percussion and did not respond to thermal testing. Periodontal probing revealed an 8–10 mm deep narrow isolated pocket on the palatal side of the tooth (Figure 1B).
The results of laboratory examinations were within normal range.
Cone beam computed tomography (CBCT) (J Morita Corporation, Kyoto, Japan) images confirmed that the tooth had undergone RCT, and a vertical fracture line on the palatal side of the root was identified from the cervical area to the apex (Figure 1C and D). Furthermore, there was a large area of bone destruction around the apical and palatal sides of the root (Figure 1E).
Based on clinical and CBCT examinations, the final diagnosis of tooth #9 was VRF.
After communicating with the patient, the intentional replantation method was selected for the treatment of the tooth, and informed consent was obtained. However, the prognosis of this treatment was unpredictable at the moment. The timeline of the treatment and review of this case is summarized in Table 1.
| Treatment or review | Fracture treatment and intentional replantation | One-month review | Three months review | Six-months review | One-year review |
| Date | 2020-09-17 | 2020-10-16 | 2020-12-16 | 2021-03-14 | 2021-09-15 |
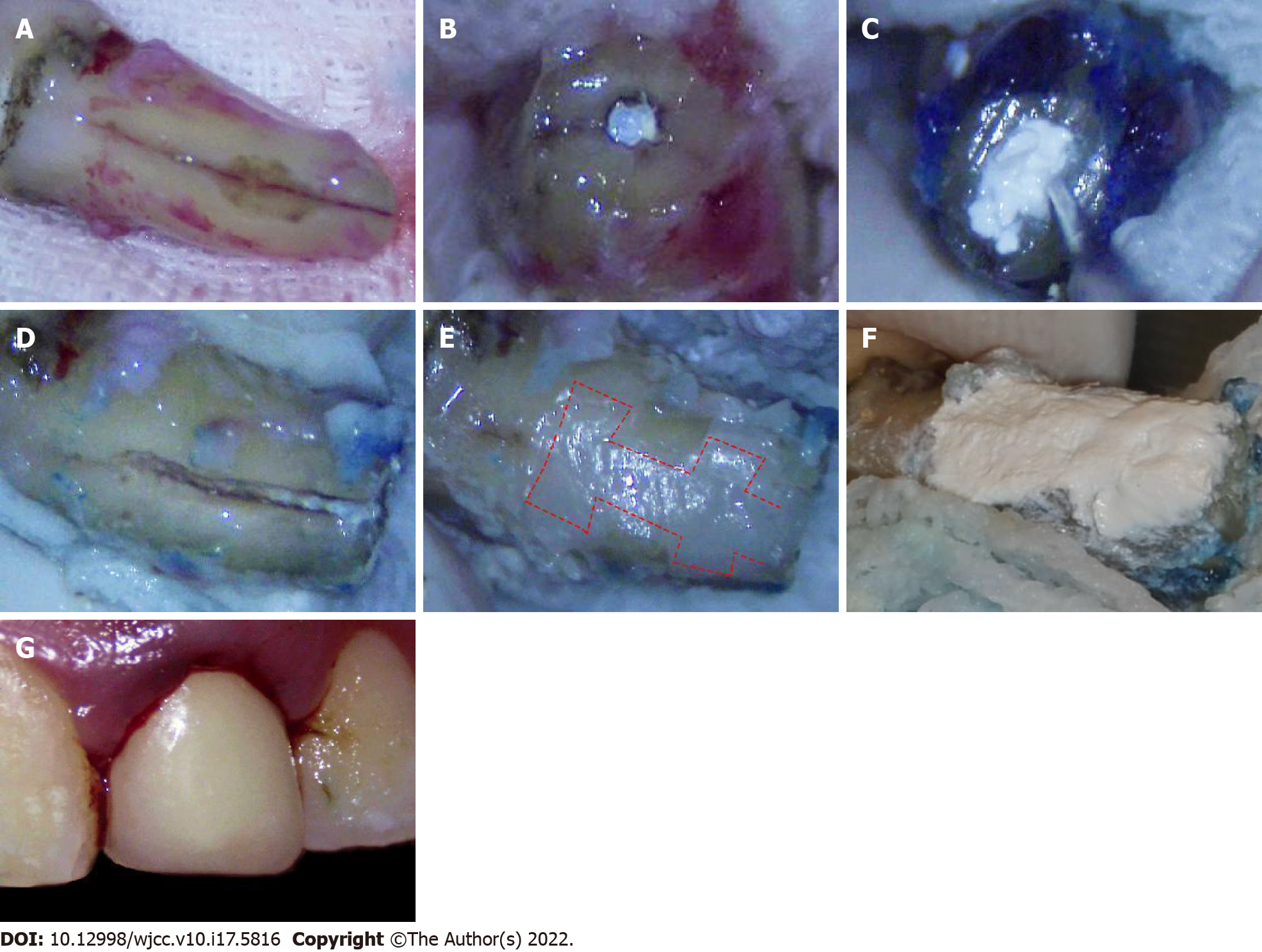
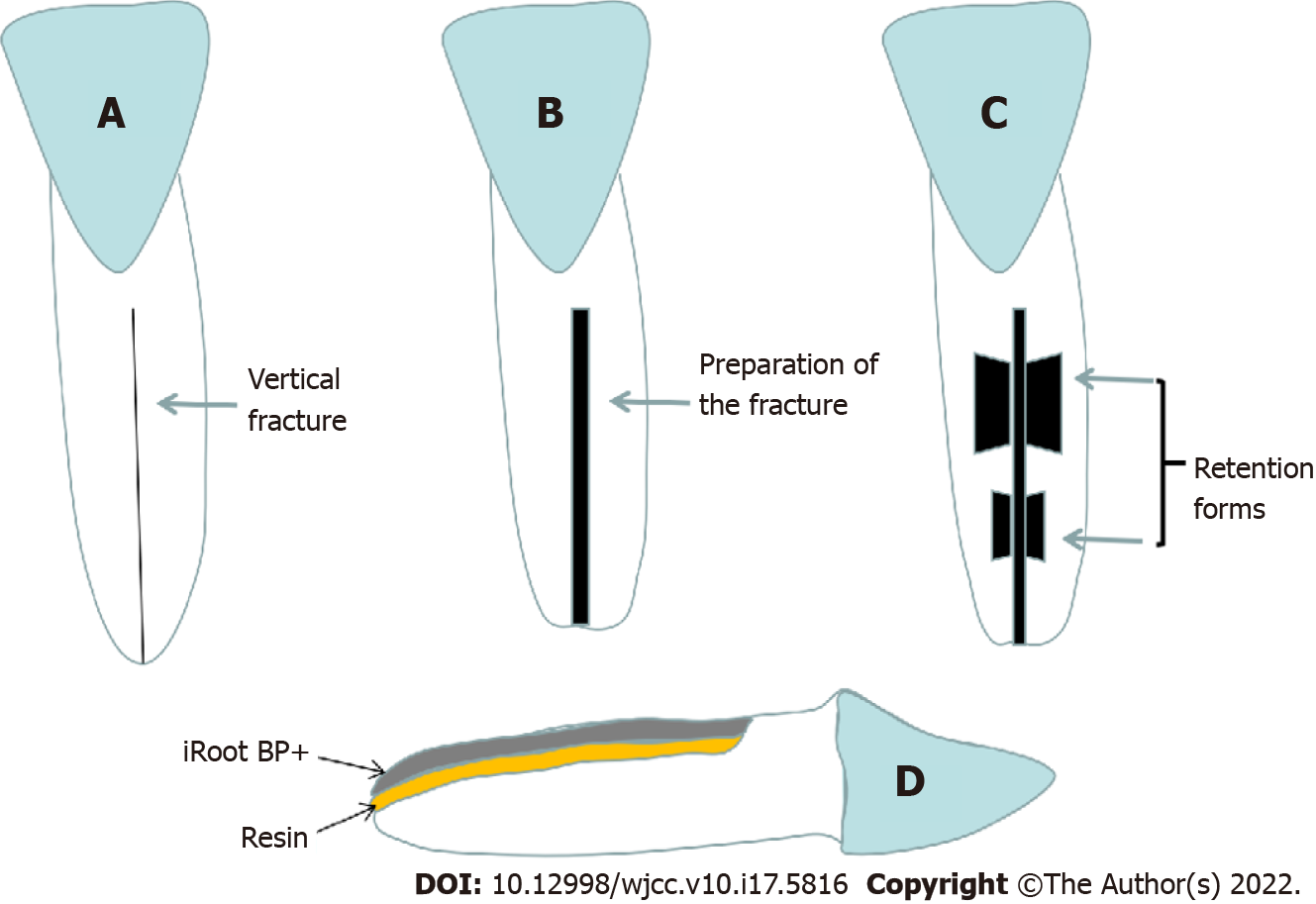
After local anesthesia, tooth #9 was extracted carefully with dental forceps only touching the crown of the tooth, and then the root of the tooth was covered with wet gauze saturated with normal saline throughout the procedure. The vertical fracture line was observed under a dental microscope (Zumax Medical Co. Ltd., Suzhou, China) after granulation tissue was carefully removed using a curette (Figure 2A). The apical 3 mm of the root was excised (Figure 2B). A 3-mm retrograde canal cavity was prepared using an ultrasonic tip and filled with iRoot BP Plus (Innovative Bioceramix Inc., Vancouver, Canada) (Figure 2C). The vertical fracture line was then evenly enlarged to approximately 1.5 mm in width using a high-speed handpiece with a fissure bur along the fracture line (Figure 2D). To enhance fixation strength, two trapezoidal retention forms were prepared on both sides of the fracture line at the coronal 1/3 and apical 1/3 of the line. The width of the outer side of the trapezoidal retention form was approximately 3 mm and the width of the inner side was approximately 2 mm. The depth of the retention form was approximately 2 mm. After applying the bonding agent, a light-cure composite resin (Ketac Molar Easymix; 3M ESPE, St Paul, MN) was filled into the fracture line and retention form (Figure 2E). After the resin was cured, the surface resin was removed to a depth of approximately 1 mm using a fissure bur, and the rest of the resin surface was covered with iRoot BP Plus (Figure 2F). The tooth was then cleaned with normal saline and replanted into the root socket using gentle pressure (Figure 2G). The tooth was splinted to the adjacent teeth using a ligation wire. The occlusion was checked after replantation, and using occlusal adjustment, early contact in centric occlusion and lateral or protrusive movements were avoided. Posttreatment, oral hygiene instructions were provided to the patient.
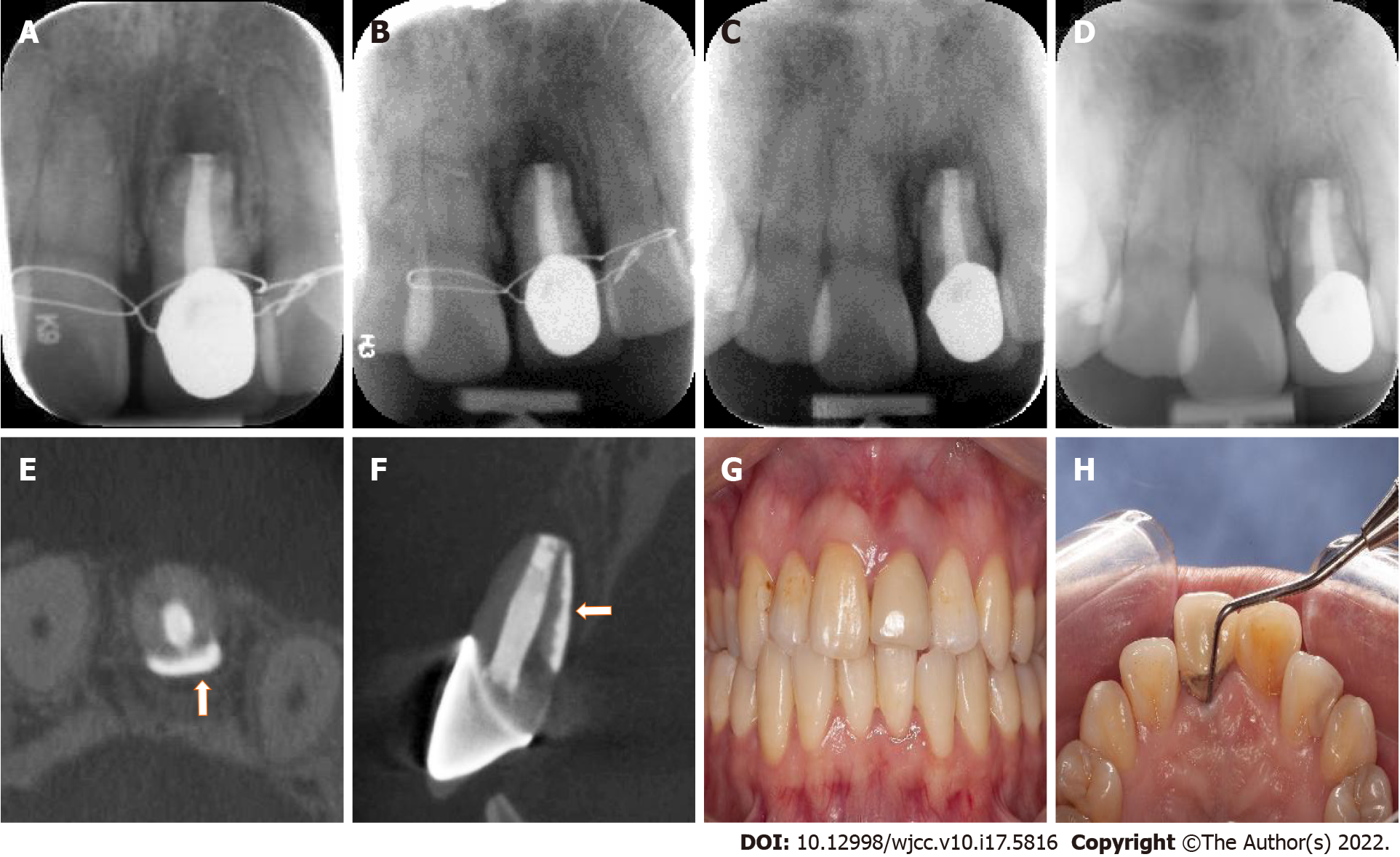
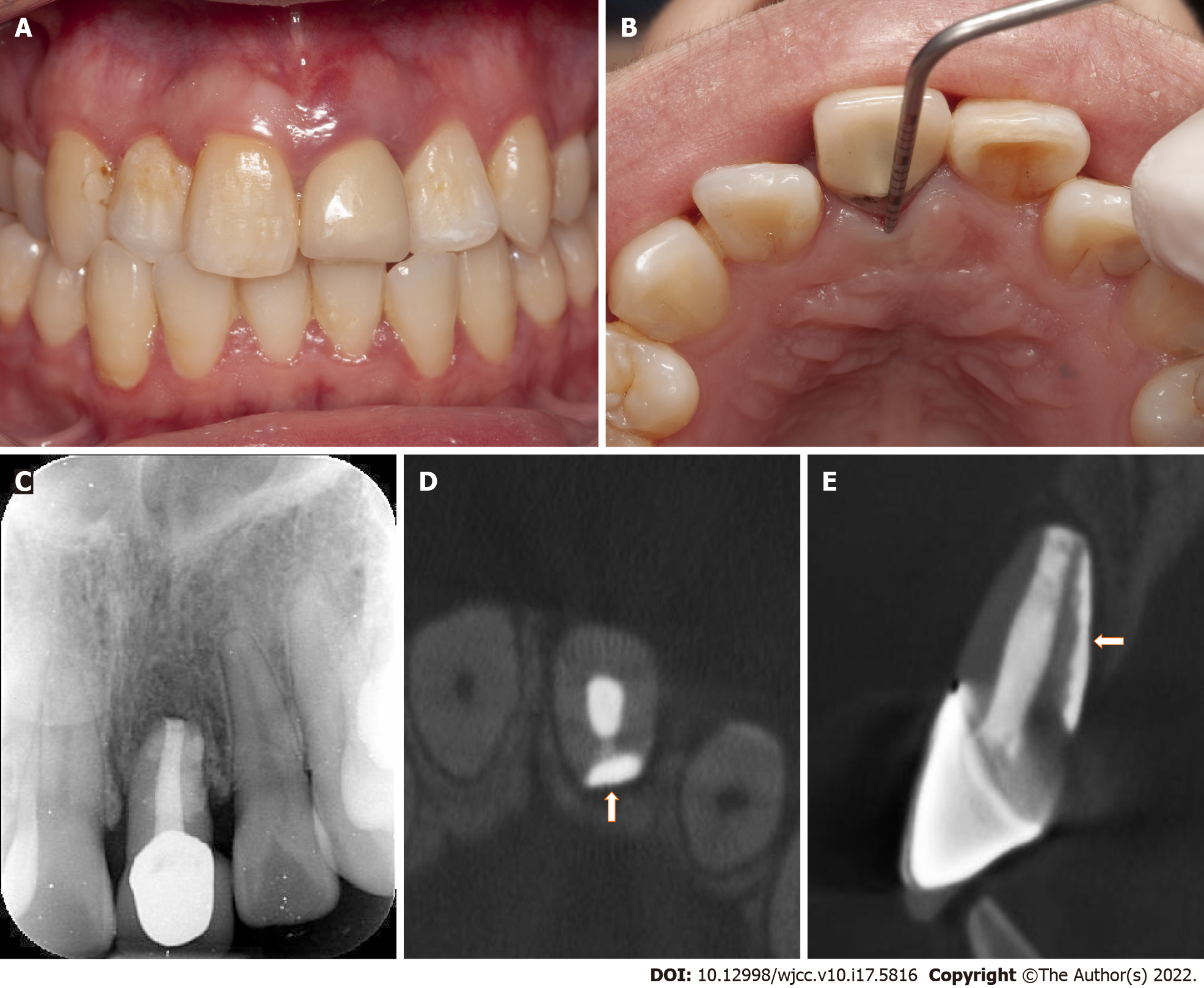
An immediate postoperative radiograph (Kavo Focus, Tuusula, Uusima, Finland) was obtained to confirm the correct position of tooth #9 (Figure 3A). The follow-up examinations were scheduled at one month, three months, six months, and one year after the treatment. At the one-month follow-up, the mobility of tooth #9 returned to the normal range and the ligation wire was removed. The radiograph showed slightly reduced apical radiolucency (Figure 3B). At three-month recall, the radiograph revealed that the periapical and periodontal radiolucency was significantly reduced (Figure 3C). At six-month follow-up, radiography and CBCT revealed significant bone regeneration around the root (Figure 3D-F). The tooth was asymptomatic, with a normal gingival appearance, periodontal probing depth, and mobility (Figure 3G and H). At the one-year follow-up, the tooth remained asymptomatic with normal gingival appearance, periodontal probing depth, and mobility (Figure 4A and B). The radiograph, together with the CBCT image, showed almost normal bone and periodontal structures around the root (Figure 4C-E), and the patient was satisfied with the treatment outcome.
Intentional replantation is regarded as the last option for the treatment of periodontitis, pulpitis, and post-traumatic cases, and is defined as the intentional removal of a tooth and replantation into original socket, and fixation in situ after evaluation and treatment[18]. This procedure allows the extracted tooth to be treated extraorally, and the infected tissue to be thoroughly removed under a microscope[6]. In the present case, the left maxillary central incisor was vertically fractured and a large amount of granulation tissue was found around the fracture line and apex. To remove the infected tissue and repair the fracture more accurately, an intentional replantation method was used for the treatment. After tooth extraction, both the root apex and fracture line were cleaned and treated.
Factors that may affect the prognosis of VRF treatment include the reattachment of periodontal tissue, alveolar bone regeneration, proper sealing of the fracture line, and prevention of refracture. The use of adhesive composite resin has been widely reported in the literature for the treatment of VRF[4-6,19-23]. The ideal bonding and repair material for VRF should have the following features to allow periodontal tissue attachment: sufficient fixation strength, short setting time, easy application, hydrophilicity, bacteriostaticity, and biocompatibility[24]. Recently, 4-methacryloxyethyl trimellitate anhydride/methyl methacrylate-tri-n-butylborane (4-META/MMA-TBB) resin, a self-cure adhesive resin cement, has been primarily used for splinting mobile teeth or treating fractured teeth with successful reconstruction outcomes[6,23]. In addition to the advantages of adhesive properties to dentin, Tanaka et al[24] reported that 4-META/MMATBB resin adheres to cementum by inducing the formation of hybridized cementum in the short term, which can provide a good seal for bonding vertically fractured roots. However, Sugaya et al[25] found no cementum-like hard tissue formation on the 4-META/MMA-TBB resin surface, and it was difficult to control polymerization of the material.
In contrast, the endodontic reparation cement ProRoot MTA[8,9] and Biodentine[10,11] have also been used for the treatment of VRF. These materials showed an effective seal against dentin and cementum and could promote biological repair and regeneration of periodontal tissue. Compared with MTA, Biodentine has a shorter setting time, is resistant to hydrolysis during setting, and releases more calcium and silicon, which is beneficial for the mineralization of bone and dentin[11]. Similarly, iRoot BP Plus is a hydrophilic calcium silicate-based bioceramic material. iRoot BP Plus has excellent mechanical properties, sealing ability, and antibacterial activity[15,26]. Moreover, iRoot BP Plus exhibits outstanding biological characteristics. Mahmood et al[27] reported high biocompatibility and desired repair of pulpal and periodontal tissues after iRoot BP Plus treatment of lateral perforations in the roots of rat incisors. Due to the biocompatibility of iRoot BP Plus and the satisfactory bonding strength of the adhesive composite resin, this study combined these two materials to repair vertical fractures. Furthermore, repeated stress overloading can result in fatigue failure of the tooth structure. Even normal functional stresses might result in VRF in case of tooth structure with reduced mechanical properties caused by aging, pulp necrosis, and endodontic therapy[28]. It is crucial to enhance the fixation strength of the vertical fracture line during the treatment of VRF to reduce the possibility of future refracture. However, even though composite resin has a stronger bonding strength than bioceramic materials[29], fixation strength is also closely related to the shape of the defect. Studies have confirmed that the retention form is necessary to improve fixation strength, and the design of the retention form could effectively increase the contact area and enhance the retention force of the repair materials[30]. Consequently, two trapezoidal retention forms were prepared on both sides of the fracture line to obtain a higher fixation strength and reduce the possibility of future refracture (Figure 5). After the fracture line and retention form were filled with resin, a thin layer of surface resin was evenly removed, and iRoot BP Plus was applied on top of it so that both, bonding strength and a pro-osteogenic surface could be achieved. In addition, occlusal adjustment was performed to facilitate the recovery of the replanted tooth.
The difference in the follow-up period may have influenced the judgment of the treatment results. Through a follow-up study of 1000 cases treated by endodontic surgery, Rud et al[31] reported that a standard follow-up should be at one year after the operation because most changes take place within the first year after the operation, and very few cases that are successful at the one-year recall shift to questionable or failed treatment outcomes in subsequent follow-ups[31]. Therefore, one-year follow-up in this case might be sufficient to demonstrate the primary treatment outcome, although a longer observation period is still necessary.
In summary, the new approach in this study successfully combined the resin and bioceramic material to repair VRF through a retention form on both sides of the fracture and the intentional replantation method. Additional clinical applications and longer observation times are necessary to further test the outcomes of this approach. This approach may provide a new treatment design for VRF.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Chinese Stomatological Association, No. 010515.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Garg P, India; Kukiattrakoon B, Thailand S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Liao WC, Chen CH, Pan YH, Chang MC, Jeng JH. Vertical Root Fracture in Non-Endodontically and Endodontically Treated Teeth: Current Understanding and Future Challenge. J Pers Med. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (2)] |
| 2. | Colleagues for excellence. Cracking the cracked tooth code: detection and treatment of various longitudinal tooth fractures. Chicago: American Association of Endodontics; 2008. |
| 3. | Dhawan A, Gupta S, Mittal R. Vertical root fractures: An update review. J Res Dent. 2014;2:107-113. [DOI] [Full Text] |
| 4. | Kallel I, Moussaoui E, Chtioui F, Douki N. Diagnosis and Managment of Maxillary Incisor with Vertical Root Fracture: A Clinical Report with Three-Year Follow-Up. Case Rep Dent. 2018;2018:4056390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Kawai K, Masaka N. Vertical root fracture treated by bonding fragments and rotational replantation. Dent Traumatol. 2002;18:42-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Okaguchi M, Kuo T, Ho YC. Successful treatment of vertical root fracture through intentional replantation and root fragment bonding with 4-META/MMA-TBB resin. J Formos Med Assoc. 2019;118:671-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Arakawa S, Cobb CM, Rapley JW, Killoy WJ, Spencer P. Treatment of root fracture by CO2 and Nd:YAG lasers: an in vitro study. J Endod. 1996;22:662-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Taschieri S, Tamse A, Del Fabbro M, Rosano G, Tsesis I. A new surgical technique for preservation of endodontically treated teeth with coronally located vertical root fractures: a prospective case series. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e45-e52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Taschieri S, Bortolin M, Weinstein T, Del Fabbro M. Preservation of an injured vital tooth using ultrasonic device and mineral trioxide aggregate. Minerva Stomatol. 2011;60:467-477. [PubMed] |
| 10. | Hadrossek PH, Dammaschke T. New treatment option for an incomplete vertical root fracture--a preliminary case report. Head Face Med. 2014;10:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 11. | Baranwal HC, Singh N, Kumar N, Garg R, Yadav J, Tripathi R. New Approach in the Management of Vertical Root Fracture with the Help of Biodentine and CBCT. Case Rep Dent. 2020;2020:2806324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Lee GW, Yoon JH, Jang JH, Chang HS, Hwang YC, Hwang IN, Oh WM, Lee BN. Effects of newly-developed retrograde filling material on osteoblastic differentiation in vitro. Dent Mater J. 2019;38:528-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Yang Y, Xia B, Xu Z, Dou G, Lei Y, Yong W. The effect of partial pulpotomy with iRoot BP Plus in traumatized immature permanent teeth: A randomized prospective controlled trial. Dent Traumatol. 2020;36:518-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Mahgoub N, Alqadasi B, Aldhorae K, Assiry A, Altawili ZM, Tao Hong. Comparison between iRoot BP Plus (EndoSequence Root Repair Material) and Mineral Trioxide Aggregate as Pulp-capping Agents: A Systematic Review. J Int Soc Prev Community Dent. 2019;9:542-552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Jeevani E, Jayaprakash T, Bolla N, Vemuri S, Sunil CR, Kalluru RS. "Evaluation of sealing ability of MM-MTA, Endosequence, and biodentine as furcation repair materials: UV spectrophotometric analysis". J Conserv Dent. 2014;17:340-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Hursh KA, Kirkpatrick TC, Cardon JW, Brewster JA, Black SW, Himel VT, Sabey KA. Shear Bond Comparison between 4 Bioceramic Materials and Dual-cure Composite Resin. J Endod. 2019;45:1378-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Nagendrababu V, Chong BS, McCabe P, Shah PK, Priya E, Jayaraman J, Pulikkotil SJ, Setzer FC, Sunde PT, Dummer PMH. PRICE 2020 guidelines for reporting case reports in Endodontics: a consensus-based development. Int Endod J. 2020;53:619-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 18. | Wang L, Jiang H, Bai Y, Luo Q, Wu H, Liu H. Clinical outcomes after intentional replantation of permanent teeth: A systematic review. Bosn J Basic Med Sci. 2020;20:13-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Oztürk M, Unal GC. A successful treatment of vertical root fracture: a case report and 4-year follow-up. Dent Traumatol. 2008;24:e56-e60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Moradi Majd N, Akhtari F, Araghi S, Homayouni H. Treatment of a vertical root fracture using dual-curing resin cement: a case report. Case Rep Dent. 2012;2012:985215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Arikan F, Franko M, Gürkan A. Replantation of a vertically fractured maxillary central incisor after repair with adhesive resin. Int Endod J. 2008;41:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Dogan MC, Akgun EO, Yoldas HO. Adhesive tooth fragment reattachment with intentional replantation: 36-month follow-up. Dent Traumatol. 2013;29:238-242. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Unver S, Onay EO, Ungor M. Intentional re-plantation of a vertically fractured tooth repaired with an adhesive resin. Int Endod J. 2011;44:1069-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Tanaka S, Sugaya T, Kawanami M, Nodasaka Y, Yamamoto T, Noguchi H, Tanaka Y, Ikeda T, Sano H, Sidhu SK. Hybrid layer seals the cementum/4-META/MMA-TBB resin interface. J Biomed Mater Res B Appl Biomater. 2007;80:140-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Sugaya T, Tomita M, Motoki Y, Zaman K, Miyaji H, Kawanami M. Periodontal tissue repair after sealing of the gap in vertical root fracture. Odontology. 2017;105:202-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Elshamy FM, Singh G, Elraih H, Gupta I, Idris FA. Antibacterial Effect of New Bioceramic Pulp Capping Material on the Main Cariogenic Bacteria. J Contemp Dent Pract. 2016;17:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Mahmood Talabani R, Taha Garib B, Masaeli R. The Response of the Pulp-Dentine Complex, PDL, and Bone to Three Calcium Silicate-Based Cements: A Histological Study in an Animal Rat Model. Bioinorg Chem Appl. 2020;2020:9582165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Tang W, Wu Y, Smales RJ. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010;36:609-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 284] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 29. | Kaup M, Dammann CH, Schäfer E, Dammaschke T. Shear bond strength of Biodentine, ProRoot MTA, glass ionomer cement and composite resin on human dentine ex vivo. Head Face Med. 2015;11:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 30. | Gilboe DB, Teteruck WR. Fundamentals of extracoronal tooth preparation. Part I. Retention and resistance form. 1974. J Prosthet Dent. 2005;94:105-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Rud J, Andreasen JO, Jensen JE. A follow-up study of 1,000 cases treated by endodontic surgery. Int J Oral Surg. 1972;1:215-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 133] [Article Influence: 2.5] [Reference Citation Analysis (0)] |