Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5810
Peer-review started: December 1, 2021
First decision: January 12, 2022
Revised: January 13, 2022
Accepted: April 22, 2022
Article in press: April 22, 2022
Published online: June 16, 2022
Processing time: 190 Days and 6.5 Hours
Wernicke encephalopathy is a rare but potentially fatal adverse event caused by thiamine deficiency. Reports of non-alcoholic Wernicke encephalopathy due to malignancy are scarce in the literature, with those reported mainly being on haematological cancer, followed by gastrointestinal cancer. As a result, there is considerable under-recognition and delay in the diagnosis and treatment of Wernicke encephalopathy in oncology departments. To our knowledge, there has been no report of Wernicke encephalopathy in a patient with esophageal cancer while receiving radiotherapy.
A 64-year-old man presented to the oncology outpatient clinic with a history of dysphagia for 2 mo, and was diagnosed with locally advanced esophageal squamous cell carcinoma (stage IIIB). Radiotherapy was initiated to alleviate dysphagia due to malignant esophageal stenosis; however, the patient exhibited consciousness disturbances starting on day 10 of radiotherapy. Brain magnetic resonance imaging indicated the development of Wernicke encephalopathy. Subsequent treatment with thiamine led to rapid improvement in the patient’s neurological symptoms.
Wernicke encephalopathy may develop in non-alcoholic patients undergoing radiotherapy for esophageal cancer. Early diagnosis and sufficient thiamine supplementation during radiotherapy are essential.
Core Tip: Wernicke encephalopathy is a neuropsychiatric disorder resulting from thiamine deficiency. It is frequently associated with alcoholism and is challenging to diagnose in non-alcoholic patients. Only scarce reports of Wernicke encephalopathy accompanying cancer have been reported, mainly in haematological malignancies followed by gastrointestinal malignancies. There have been no reports about Wernicke encephalopathy accompanying esophageal cancer. Here we report the first case of Wernicke encephalopathy in an esophageal cancer patient receiving radiotherapy. It is presented to emphasize that early nutritional evaluation and diagnosis are important. Prompt thiamine supplementation is the key to preventing permanent neurological damage.
- Citation: Zhang Y, Wang L, Jiang J, Chen WY. Non-alcoholic Wernicke encephalopathy in an esophageal cancer patient receiving radiotherapy: A case report. World J Clin Cases 2022; 10(17): 5810-5815
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5810.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5810
Wernicke encephalopathy is an acute or subacute neuropsychiatric disorder secondary to thiamine (vitamin B1) deficiency. It is characterized by the classical triad of ophthalmoplegia, gait ataxia, and altered mental status[1-3], which, however, presents in only 10%-16% of the cases[1,3,4]. Chronic alcoholism is the most common predisposing factor for thiamine deficiency, followed by malnutrition or decreased thiamine absorption secondary to hyperemesis gravidarum, gastrointestinal disease, prolonged fasting, prolonged parenteral nutrition support, hemodialysis, or malignant disease[5-9]. Compared to alcoholic Wernicke encephalopathy, non-alcoholic Wernicke encephalopathy may be prone to diagnostic delays owing to its atypical clinical presentation and the interval between symptom onset and clinical diagnosis[10]. To the best of our knowledge, there have been no reports of Wernicke encephalopathy occurring in cases of esophageal cancer. Moreover, the most common predisposing factors for non-alcoholic Wernicke encephalopathy in cancer include gastrectomy, chemotherapy, or end-stage of life; radiotherapy is rarely documented. Herein, we describe the first case of non-alcoholic Wernicke encephalopathy accompanying esophageal cancer in a patient receiving radiotherapy.
A 64-year-old man was admitted to our hospital with complaints of progressive difficulty in swallowing.
The patient’s symptoms started 2 mo prior, with recurrent episodes of difficulty in swallowing. He could ingest fluids with ease, but semi-liquid foods only with difficulty. He also reported feeling fatigued.
There was no remarkable medical history. He had a history of smoking for 20 years, but no history of alcohol or drug consumption.
The patient had a disease-free personal and family history.
The patient was emaciated and had a body mass index of 19.88 kg/m2. There were no mental status changes, cerebellar symptoms, or abnormal eye movements. No clinical ophthalmoplegia or encephalopathy was detected. The other items of the physical examination were normal.
Blood biochemistry revealed mild hypoproteinemia (36 g/L). The results of routine blood and urine tests and arterial blood gas analysis were normal.
An esophagogastroscopy revealed a significant esophageal tumor located 26-33 cm from the upper incisors, and biopsy results indicated squamous cell carcinoma. Chest contrast-enhanced computed tomography (CT) revealed thickening of the middle and lower esophageal wall with luminal stenosis. The abdominal CT findings were unremarkable. As per the eighth edition of the Union for International Cancer Control staging, the final diagnosis was locally advanced esophageal squamous cell carcinoma, clinical stage cT3N2M0 (stage IIIB).
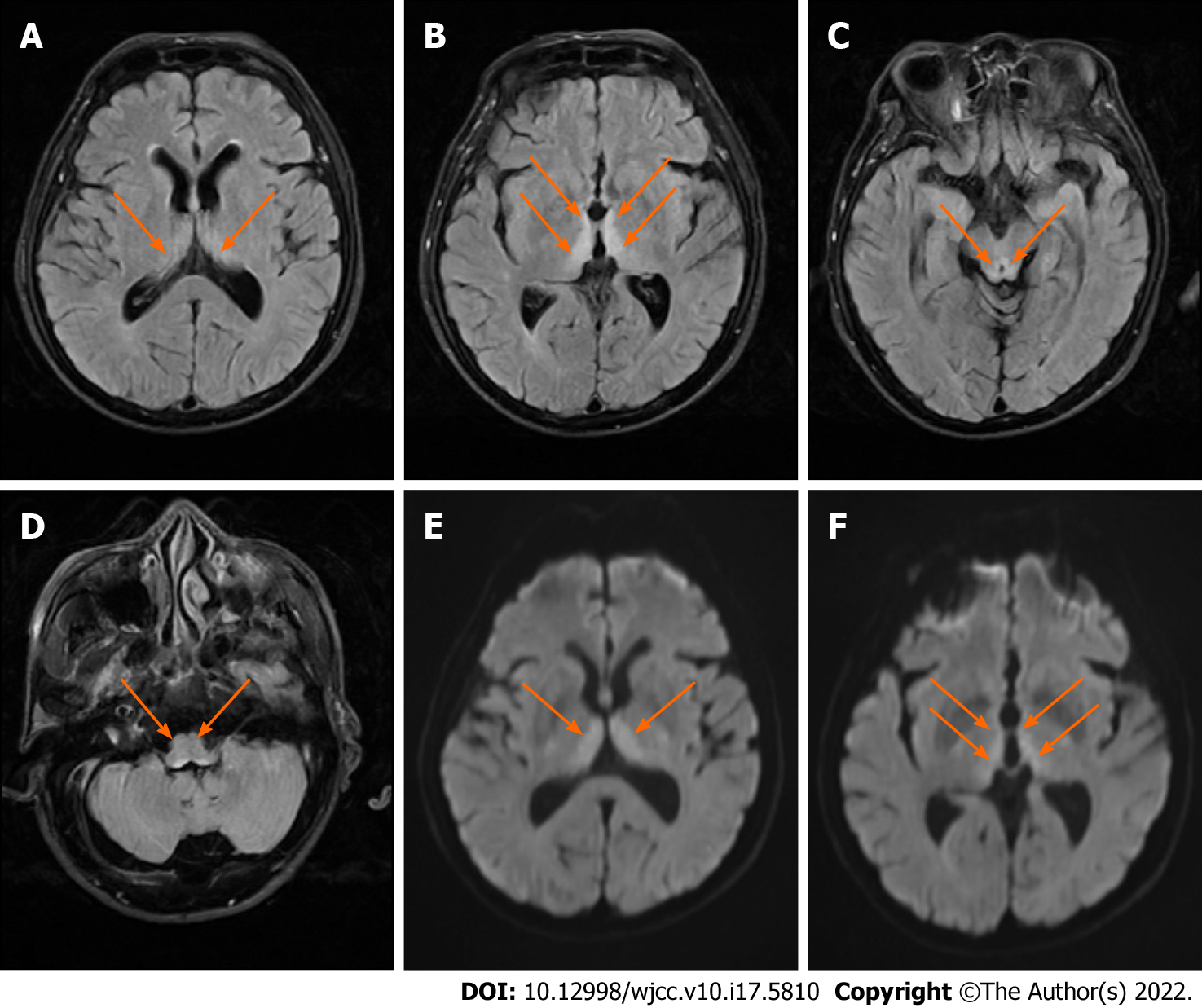
The patient refused surgery or chemotherapy. In order to alleviate dysphagia due to malignant esophageal stenosis, he received 60 Gy of local radiotherapy in 30 fractions without concurrent chemotherapy. Repeated vomiting and dorsalgia occurred during radiotherapy, without diarrhea. A parenteral nutritional supplement including high glucose but no thiamine was administered. On day 8 of radiotherapy, the dysphagia status was markedly improved. From day 10 of radiotherapy, the patient gradually displayed apathy, disorientation, and passivity; was disinterested in his surroundings; and slept abundantly. On neurological examination, he was minimally responsive to verbal and painful stimuli, uncooperative for the finger-to-nose examination, had a slow pupillary response to light, and a Glasgow coma scale score of 10. This was followed by the onset of lethargy on day 12 of radiotherapy. An emergency brain CT scan performed immediately was normal. Brain magnetic resonance imaging (MRI) showed bilateral symmetrical hyperintensities in the dorsal thalamus, the periventricular region of the third ventricle, and around the cerebral aqueduct as seen on T2-weighted imaging, fluid-attenuated inversion recovery (FLAIR), and diffusion-weighted imaging (DWI) (Figure 1).
At first, the signs and symptoms rendered cerebrovascular disease or metastatic brain tumors as the most probable diagnosis. However, after combining the clinical manifestations and typical brain MRI findings, a final diagnosis of Wernicke encephalopathy secondary to thiamine deficiency was made.
We started immediate intravenous thiamine replacement therapy at a dose of 500 mg/d for 3 d, followed by 200 mg for a week, and one tablet of 100 mg oral thiamine per day.
The patient regained consciousness within 3 d. After 5 d, his mental status improved, and he could understand simple commands. At discharge, the patient’s neurological symptoms were improved significantly. Neurological examination at the 2-mo follow-up was normal, except for mild memory impairment.
Wernicke encephalopathy is a neurological disorder resulting from the deficiency of thiamine, and is commonly related to the chronic abuse of alcohol[1,2]. Recently, the incidence of non-alcoholic Wernicke encephalopathy has been increasing, and malignancy is one of the attributable causes. The most common type of malignancy reported with non-alcoholic Wernicke encephalopathy is haematological, followed by gastrointestinal neoplasms. There have been no studies reporting cases of Wernicke encephalopathy in patients with esophageal cancer thus far.
Thiamine cannot be synthesized in the human body, and hence is mainly derived from food. Therefore, any kind of malnutrition lasting for more than 3-4 wk depletes the thiamine reserve[11]. Esophageal cancer is often accompanied by malnutrition due to dysphagia and declined appetite. The potential for subclinical thiamine deficiency should be considered despite the absence of changes in the mental state[12].
In patients with cancer, Wernicke encephalopathy can occur after surgery, during chemotherapy, or at the end of life. It is extremely rare in patients receiving radiotherapy based on existing reports, and there is no guidance on whether radiotherapy can accelerate thiamine deficiency. It needs to be confirmed by more studies in the future. We concluded that chronic malnutrition caused by repeated dysphagia and vomiting was the main reason for Wernicke encephalopathy in our patient. Therefore, a total nutritional evaluation and prophylactic thiamine supplementation are major preventative and therapeutic measures for impaired dietary intake in non-surgical esophageal cancer patients from the time of diagnosis, especially before radiotherapy.
The classically described clinical triad of ophthalmoplegia, ataxia, and mental disturbances is often absent in Wernicke encephalopathy. Therefore, a non-alcoholic patient presenting with atypical clinical manifestations can frequently be misdiagnosed. Day et al[13] reported underdiagnosis rates of 68% and 94% in alcoholic and non-alcoholic Wernicke encephalopathy, respectively. Delayed diagnosis and treatment can lead to the progression of the disease. As per recommendations, the diagnosis of Wernicke encephalopathy is made when two of the following signs are present: (1) Dietary deficiencies; (2) eye signs; (3) cerebellar dysfunction; and (4) either an altered mental state or a mild memory impairment[8]. In our patient, the clinical suspicion of Wernicke encephalopathy was delayed as the patient was a non-alcoholic, and disturbance of consciousness was the only manifestation.
MRI is currently considered the most valuable method for the diagnosis of non-alcoholic Wernicke encephalopathy, especially the FLAIR sequence which has a 93% specificity[14]. The common MRI findings for non- alcoholic Wernicke encephalopathy are hyperintense signals in the dorsal medial thalamic nuclei, periaqueductal gray area, and the third or fourth ventricles as seen on DWI, T2-weighted imaging, and FLAIR sequence[1,11,15,16]. In our patient, there were no obvious abnormalities on CT, but typical findings were detected on MRI, similar to that in current literature reports. Therefore, it is important to detect Wernicke encephalopathy in the early stages of the disease using MRI, since CT has a low sensitivity in the acute phase. Wernicke encephalopathy should be considered as one of the common differential diagnoses when patients develop unexplained altered mental status during radiotherapy while admitted to the Department of Oncology.
Thiamine plays a major role in glucose metabolism. The administration of glucose may thus accelerate the consumption of thiamine and hasten the onset of Wernicke encephalopathy. Our patient received no thiamine, but received continuous glucose solutions as a part of his parenteral nutrition supplement, which is consistent with that reported in the literature[17-19]. Therefore, glucose should be used with caution.
Once a diagnosis of Wernicke encephalopathy is suspected, it is advisable to administer thiamine as early as possible to prevent permanent neurological damage[20]. Although there are no published guidelines for the treatment of Wernicke encephalopathy in non-alcoholics patients, intravenous thiamine supplementation in the acute stage is currently recommended. Several researchers recommend that patients be treated with a high-dose thiamine regimen, consisting of 500 mg thiamine every 8 h intravenously for at least 2-3 d, followed by 250 mg thiamine once a day intravenously for 5 d[21]. In our patient, there was significant improvement in his mental state, but mild cognitive impairment remained due to the late diagnosis of the condition. Therefore, our objective in reporting this case is to emphasize the importance of early nutritional evaluation and diagnosis, so that lasting neurological sequelae can be avoided in patients with Wernicke encephalopathy.
Our case illustrates that Wernicke encephalopathy can occur in non-alcoholic patients with esophageal cancer. Clinicians should keep in mind that patients with esophageal cancer and underlying malnutrition are at a high risk of Wernicke encephalopathy. Nutritional evaluation and diagnosis are necessary at the earliest possible instance. Any clinical suspicion of Wernicke encephalopathy should be treated promptly with thiamine supplementation to prevent permanent neurological damage.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nyamuryekung'e MK, Tanzania; Zhang X, United States S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yan JP
| 1. | Sinha S, Kataria A, Kolla BP, Thusius N, Loukianova LL. Wernicke Encephalopathy-Clinical Pearls. Mayo Clin Proc. 2019;94:1065-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 84] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 2. | Vogrig A, Zanoni T, Moretto G. Nystagmus and Lower Extremity Hyperalgesia After Colectomy. JAMA. 2016;316:1488-1489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Harper CG, Giles M, Finlay-Jones R. Clinical signs in the Wernicke-Korsakoff complex: a retrospective analysis of 131 cases diagnosed at necropsy. J Neurol Neurosurg Psychiatry. 1986;49:341-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 423] [Cited by in RCA: 433] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 4. | Zuccoli G, Gallucci M, Capellades J, Regnicolo L, Tumiati B, Giadás TC, Bottari W, Mandrioli J, Bertolini M. Wernicke encephalopathy: MR findings at clinical presentation in twenty-six alcoholic and nonalcoholic patients. AJNR Am J Neuroradiol. 2007;28:1328-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 118] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Arita T, Komatsu S, Kosuga T, Konishi H, Morimura R, Murayama Y, Kuriu Y, Shiozaki A, Ikoma H, Nakanishi M, Ichikawa D, Okamoto K, Otsuji E. [Laparoscopic Gastrostomy for a Patient with Wernicke's Encephalopathy after Gastrectomy--A Case Report with a Literature Review]. Gan To Kagaku Ryoho. 2015;42:2037-2039. [PubMed] |
| 6. | D'Ettorre M, Rosa F, Coppola A, Mele C, Alfieri S, Doglietto GB. Postoperative suspected Wernicke's encephalopathy in a rectal cancer patient: a case report. J Palliat Care. 2012;28:290-292. [PubMed] |
| 7. | Zafar A. Wernicke's encephalopathy following Roux en Y gastric bypass surgery. Saudi Med J. 2015;36:1493-1495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Galvin R, Bråthen G, Ivashynka A, Hillbom M, Tanasescu R, Leone MA; EFNS. EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol. 2010;17:1408-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 394] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 9. | Sriram K, Manzanares W, Joseph K. Thiamine in nutrition therapy. Nutr Clin Pract. 2012;27:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 10. | Dhir S, Tarasenko M, Napoli E, Giulivi C. Neurological, Psychiatric, and Biochemical Aspects of Thiamine Deficiency in Children and Adults. Front Psychiatry. 2019;10:207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 136] [Cited by in RCA: 139] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 11. | Zuccoli G, Pipitone N. Neuroimaging findings in acute Wernicke's encephalopathy: review of the literature. AJR Am J Roentgenol. 2009;192:501-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 192] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 12. | Yoshioka A, Sato I, Onishi H, Ishida M. Subclinical thiamine deficiency identified by pretreatment evaluation in an esophageal cancer patient. Eur J Clin Nutr. 2021;75:564-566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Day GS, del Campo CM. Wernicke encephalopathy: a medical emergency. CMAJ. 2014;186:E295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Guler A, Alpaydin S, Sirin H, Calli C, Celebisoy N. A non-alcoholic Wernicke's encephalopathy case with atypical MRI findings: Clinic vs radiology. Neuroradiol J. 2015;28:474-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Manzo G, De Gennaro A, Cozzolino A, Serino A, Fenza G, Manto A. MR imaging findings in alcoholic and nonalcoholic acute Wernicke's encephalopathy: a review. Biomed Res Int. 2014;2014:503596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 16. | Zuccoli G, Santa Cruz D, Bertolini M, Rovira A, Gallucci M, Carollo C, Pipitone N. MR imaging findings in 56 patients with Wernicke encephalopathy: nonalcoholics may differ from alcoholics. AJNR Am J Neuroradiol. 2009;30:171-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 176] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 17. | Jin J, Mulesa L, Carrilero Rouillet M. Trace Elements in Parenteral Nutrition: Considerations for the Prescribing Clinician. Nutrients. 2017;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 18. | Harada D, Nakayama M. Influence of Glucose Dosage in Parenteral Nutrition on Body Thiamine Levels in Rats. Int J Med Sci. 2019;16:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Gralak MA, Dębski B, Drywień M. Thiamine deficiency affects glucose transport and β-oxidation in rats. J Anim Physiol Anim Nutr (Berl). 2019;103:1629-1635. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Smith H, McCoy M, Varughese K, Reinert JP. Thiamine Dosing for the Treatment of Alcohol-Induced Wernicke's Encephalopathy: A Review of the Literature. J Pharm Technol. 2021;37:107-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Ho PA, York A, Rustad JK, Felde A, Stern TA. Non-Alcohol-Related Wernicke's Encephalopathy: Diagnosis and Treatment. Prim Care Companion CNS Disord. 2021;23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |