Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4676
Peer-review started: November 27, 2021
First decision: January 12, 2022
Revised: January 27, 2022
Accepted: March 16, 2022
Article in press: March 16, 2022
Published online: May 16, 2022
Processing time: 167 Days and 2.5 Hours
Esophageal cancer is a common cause of cancer-related death worldwide. Cutaneous metastasis of esophageal squamous cell carcinoma is rare, particularly in diffuse skin metastasis.
In this case report, we describe an 82-year-old male who was diagnosed with esophageal squamous cell carcinoma. The tumor was staged as T4N3M1 (Stage IVB). The pathological findings revealed poorly differentiated squamous cell carcinoma of the esophagus. Four months after diagnosis, the patient began chemotherapy, and symptoms were relieved after four cycles of chemotherapy. After that, the patient returned home without a systematic physical examination. One year after diagnosis, the patient realized that the skin of the abdominal wall was hard and rough without pain, and the color became darker than normal skin. Thirteen months after diagnosis, a biopsy of the patient’s abdominal lesion revealed that the skin metastasis was derived from the esophagus. Then the patient received two cycles of apatinib combined with docetaxel, but the abdominal lesion worsened. Two cycles of nivolumab were administered, but the patient eventually died of multiple organ failure.
This report highlights cutaneous metastasis as a late and untreatable metastasis of esophageal cancer.
Core Tip: Cutaneous metastasis from esophageal carcinoma is rare, especially esophageal squamous cell carcinoma. We present a patient with squamous cell carcinoma of the esophagus and metastasis to diffuse cutaneous tissue. Second-line chemotherapy and immunological checkpoint inhibitor treatment were not effective, and this patient only achieved a 4-mo survival time after cutaneous metastasis.
- Citation: Zhang RY, Zhu SJ, Xue P, He SQ. Cutaneous metastasis from esophageal squamous cell carcinoma: A case report. World J Clin Cases 2022; 10(14): 4676-4683
- URL: https://www.wjgnet.com/2307-8960/full/v10/i14/4676.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i14.4676
Esophageal carcinoma accounts for 3.2% of all new cancer cases worldwide[1]. In China, the estimated number of esophageal carcinoma cases in 2015 was 0.37 million[2]. Different from European and North American countries, the main pathological type of Chinese patients with esophageal cancer is squamous cell carcinoma, while this is merely 30% in North American countries[3].
Cutaneous metastasis from esophageal carcinoma is rare, and its prevalence is less than 1%[4]. Lookingbill et al[5] conducted a retrospective study of 4020 cutaneous metastasis patients and found only three primary esophageal squamous cell carcinoma cases. We present a patient with squamous cell carcinoma of the esophagus and metastasis to diffuse cutaneous tissue. This patient only achieved a 4-mo survival time after cutaneous metastasis.
An 82-year-old male presented to our clinic and complained of dysphagia and loss of appetite, accompanied by diffuse cutaneous metastasis.
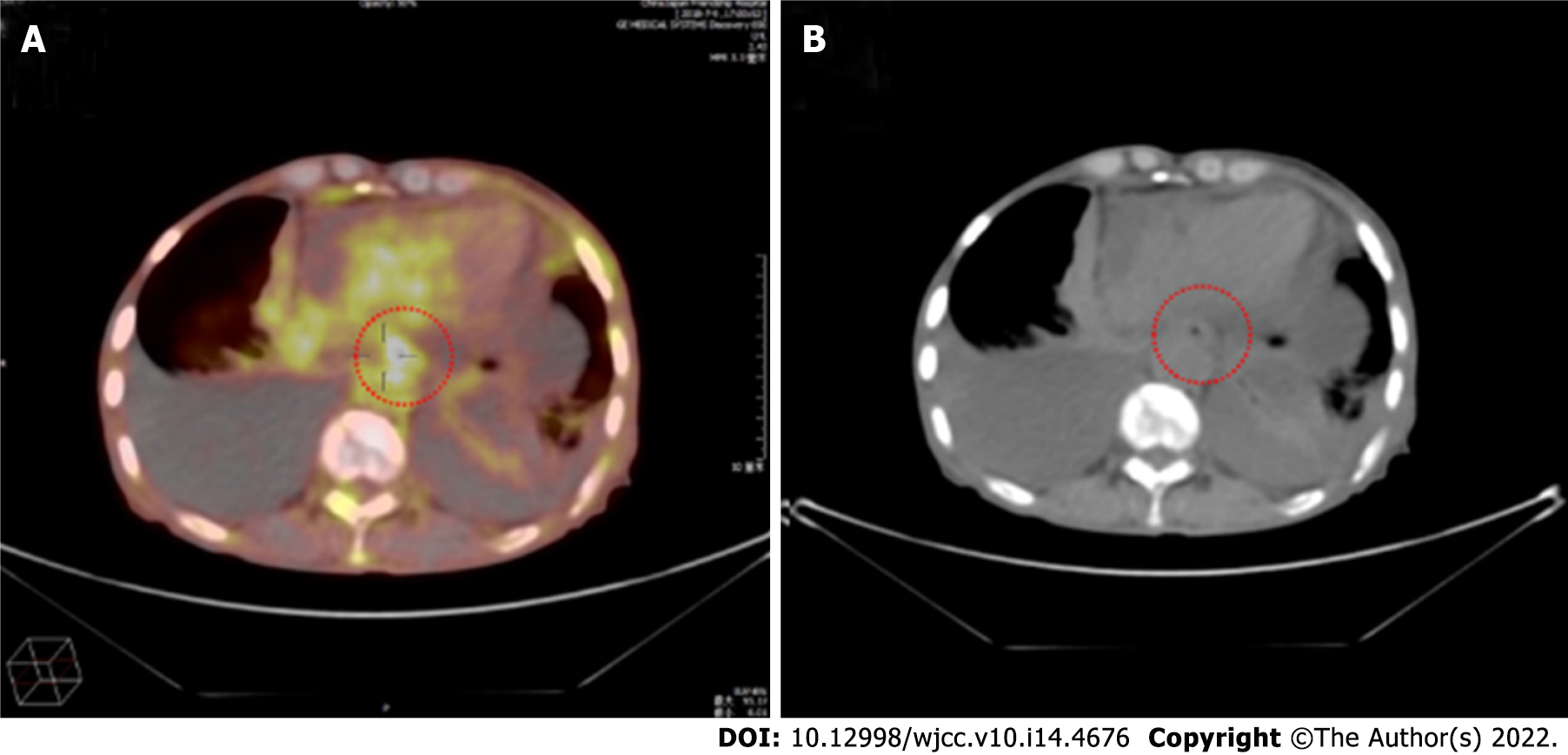
An 82-year-old male presented to our outpatient clinic and complained of difficulty in dysphagia and loss of appetite, accompanied by acid reflux without nausea and vomiting from May 2018. The positron emission tomography/computed tomography (CT) revealed diffuse thickening of the esophagus and stomach wall, with a maximum standard uptake value of 11.2 and bilateral pleural effusion rendering the tumor inoperable (Figure 1A and B). Because the cytology of the patient’s pleural fluid revealed pleural metastases, the tumor was staged as T4N3M1 (Stage IVB). The endoscopic study revealed a peripherally protruding neoplasm at 35 cm from the dental arch, which almost completely occluded the esophageal lumen. A biopsy was taken from the circumferential bulge. The pathological findings revealed poorly differentiated squamous cell carcinoma from the esophagus.
Subsequently, chemotherapy was performed: S-1 50 mg day 1-14, cisplatin 30 mg day 1, 21 d, one period, a total of four cycles (weight, 55 kg; height, 1.62 m; body surface area, 1.64 m2). After four cycles of chemotherapy, the patient’s symptoms were relieved, and the pleural effusion disappeared upon evaluation of the lesion, according to the Response Evaluation Criteria in Solid Tumors 1.1 criteria. Furthermore, after completing the four cycles of chemotherapy, the patient had a partial response (based on the medical records provided by the hospital where the patient previously visited). Afterward, the patient went home.
In early March 2019, the patient realized that the skin of the abdominal wall was hard and rough without pain, and the color became darker than the normal skin (Figure 2). The CT scan of the abdomen showed no obvious changes in skin and subcutaneous soft tissue (Figure 3). At the same time, we performed a fine needle biopsy of the skin of the changing part (Figure 2). Pathological results showed that the skin metastasis was derived from the poorly differentiated squamous cell carcinoma of the esophagus (Figure 4). Thus, the patient visited our hospital for a workup for his dysphagia and diffuse cutaneous metastasis. Based on the medical history and pathological findings, the skin metastasis was derived from the poorly differentiated squamous cell carcinoma of the esophagus (Figure 4).
The patient had a history of diabetes for 20 years and did not regulate the use of drugs. He denied the history of operation.
The patient had no history of smoking and occasionally drank alcohol. Furthermore, the patient quit drinking before admission to the hospital.
The patient’s vital signs were stable. The physical examination of the abdomen revealed that the skin of the abdominal wall was hard and rough without pain, and the color became darker than normal skin (Figure 2).
Blood tumor markers: total prostate specific antigen 6.92 ng/mL, serum CA72-4 61.32 U/mL, alpha-fetoprotein 3.65 ng/mL, carcinoembryonic antigen 915.10 ng/mL, serum CA125 90.91 U/mL, CA153 38.24 U/mL, gastrin-releasing peptide precursor 74.40 pg/mL, squamous cell carcinoma antigen 2.20 ug/L, neuron-specific enolase 11.00 ng/mL and serum CYFRA21-1 5.06 ng/mL.
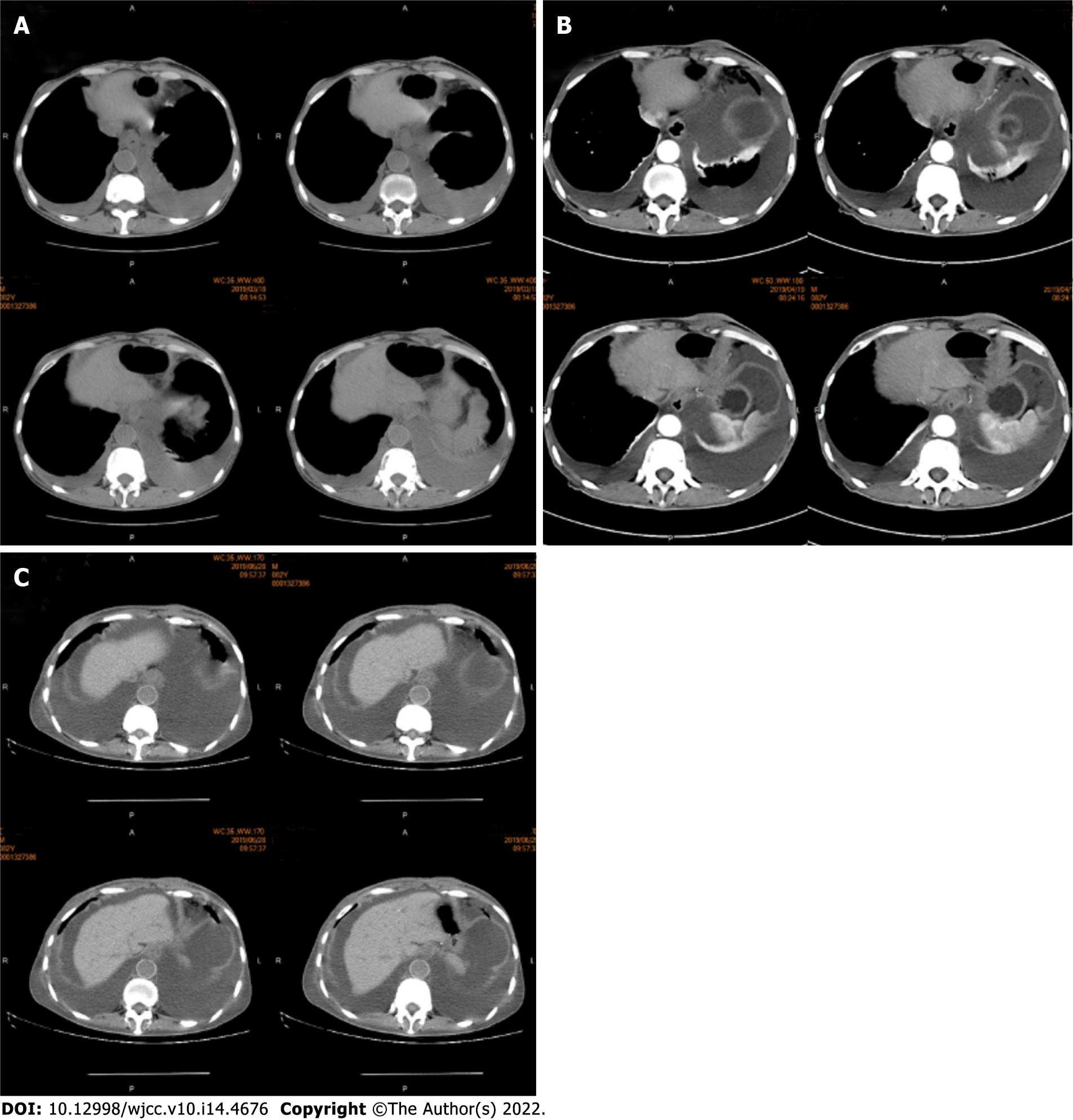
The abdominal CT revealed no obvious changes in the skin and subcutaneous soft tissue (Figure 3).
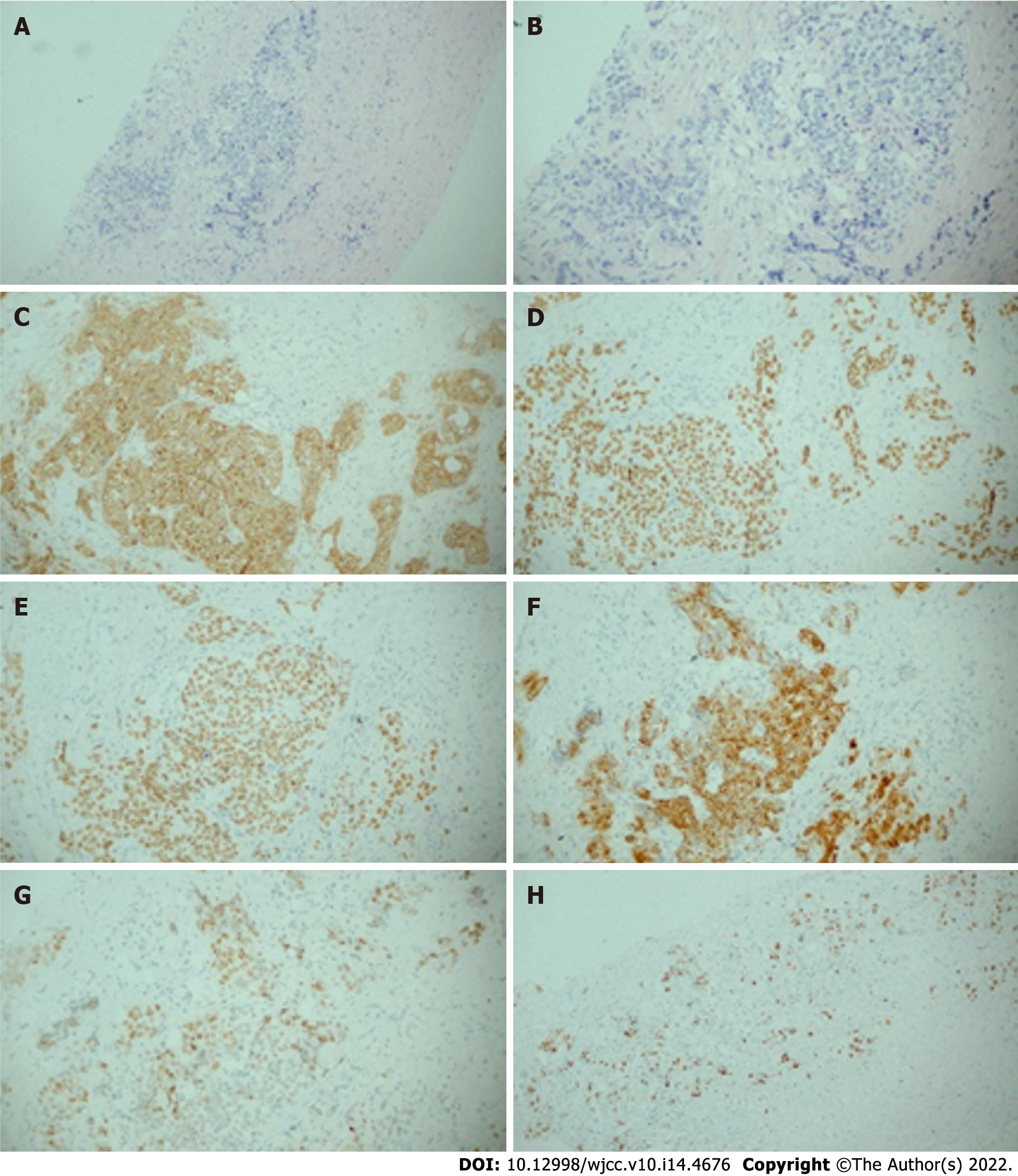
Infiltration of cancer cells was observed in the fibrous connective tissue by the puncture. The cancer cells were distributed in nests, with enlarged nuclei, hyperchromatic nuclei, heteromorphism, increased nucleoplasma ratio, and crowded arrangement (Figure 4A and B). Further immunohistochemical results showed that skin was positive for CK (Figure 4C), P40 (Figure 4D), P63 (Figure 4E), CK5/6 (Figure 4F), partially positive for P53 (Figure 4G), and about 20% positive for Ki67 (Figure 4H). The pathological results revealed that the skin metastasis was derived from the poorly differentiated squamous cell carcinoma of the esophagus (Figure 4).
The final diagnosis of the presented case was esophageal squamous cell carcinoma and relapse with cutaneous metastasis after first-line chemotherapy treatment.
The patient received systemic treatments, including second-line chemotherapy with apatinib and docetaxel.
After two cycles of chemotherapy, the patient’s abdominal wall cutaneous metastasis lesions significantly increased. Subsequently, nivolumab (120 mg, intravenous infusion on day 1) treatment was immediately applied. Unfortunately, after two cycles of nivolumab treatment, the patient’s condition did not alleviate, and the skin lesions increased. Eventually, the patient died of multiple organ failure.
In contrast to adenocarcinoma, squamous cell carcinoma is more likely to localize near the tracheal bifurcation, has a proclivity for earlier lymphatic spread and is associated with a poorer prognosis[6]. In Eastern Europe and Asia, squamous cell carcinoma is the most common histology, while adenocarcinoma is the most widespread in North America and West Europe[7].
The meta-analysis conducted by Strickley et al[8] indicated that the overall incidence of cutaneous metastasis is 5.3%. Melanoma and breast cancer is the most prone to metastasize to the skin and subcutaneous tissue[5,7]. However, other malignancies such as lung, colon, head and neck and hematologic diseases also have been described with a degree of frequency[8]. Furthermore, esophageal carcinoma cutaneous metastasis is rare, especially in esophageal squamous cell carcinoma, and the risk of skin metastasis is lower. However, esophageal adenocarcinoma more commonly metastasizes to the skin[4]. The manifestation of skin metastasis from esophageal cancer reported by most of the literature is scattered nodules that are rarely painful[9]. The retrospective analysis reported by Ferreira et al[10] revealed that similar to esophageal cancer, adenocarcinoma is the histological type of lung cancer most prone to skin metastasis. However, the most common clinical manifestation of skin metastasis of lung cancer is single nodules, and the most common site is the head[11]. Different from esophageal and lung cancer, typical ductal or lobular carcinoma tends to involve skin metastases to the thorax and abdomen, occasionally with hardened, erythematous plaques[12]. Nevertheless, the most common clinical presentation is single or multiple skin-toned or pink nodules[13].
Different from the literature, the present patient’s skin was mainly characterized by diffuse thickening and roughness. Cutaneous metastasis from esophageal carcinoma is rare and predominantly occurs in late tumor status. This suggested a rapid disease, as shown in Figure 3. The chest CT presented pleural effusion, suggesting that the disease recurred again (Figure 3A). The results suggested ascites effusion, lower esophagus dilation and esophageal wall thickening (Figure 3B). After two cycles of nivolumab treatment, the effusion increased, and the lower esophagus thickening became obvious (Figure 3C). The abdominal CT revealed that the abdominal wall skin was thicker than the other parts, but no subcutaneous nodules were observed. Imaging diagnosis can easily overlook the skin thickening progression and impending generalized metastatic spread[14]. Patients with esophageal cancer cutaneous metastasis have a poor prognosis. The average survival time after the development of cutaneous metastases is approximately only 4 mo[5].
Fine-needle aspiration cytology is a rapid and safe technique that can be used for the diagnosis of skin metastases. The critical evaluation of cytomorphological features, along with relevant clinical details, can help in the localization of unknown primary sites in some cases. Furthermore, the critical assessment of the morphological features of cells and the associated clinical details can help determine the source of the skin metastatic lesion[15].
Chemotherapy is the standard treatment for advanced esophageal cancer with distant metastases. Commonly used agents include 5-fluorouracil, platinum agents and taxanes. However, the objective response rate of platinum-containing dual-agent chemotherapy for esophageal squamous cell carcinoma is not high[16-18]. Immunotherapy with antibodies against PD-1 immunological checkpoints has exhibited optimistic results in the treatment of esophageal squamous cell carcinoma patients. A phase 2 clinical study, which included 64 patients, confirmed nivolumab monotherapy for advanced esophageal squamous cell carcinoma. The primary endpoint was the objective response rate, and the objective response rate was 17%. The conclusion suggests that nivolumab showed promising activity with a manageable safety profile in patients with esophageal advanced squamous cell carcinoma refractory or intolerant to standard therapies[19].
Therefore, investigators attempted to apply nivolumab for the treatment of esophageal cancer with skin metastases. In the present case, the patient was older (82-years-old), received third-line treatment, had a physical status score of 2 points and had multiple metastases with a heavier tumor burden. Hence, the treatment response at the immune checkpoint was poor[20]. Furthermore, the immune checkpoint inhibitor took a long time to achieve significant antitumor effects. After two cycles of immunological checkpoint inhibitor treatment, the tumor progressed, and the patient died. Therefore, based on the clinical trial data, it is recommended to apply the immune checkpoint inhibitor early.
In summary, extensive cutaneous metastasis of esophageal squamous cell carcinoma is extremely rare. Distributed skin metastases indicate that the tumor has advanced, and the prognosis is poor. The best treatment is timely systemic chemotherapy. For elderly patients with extensive skin metastases, immunotherapy after second-line or more than third-line treatment is less effective. This may be correlated to the low immunity of the patient, the lack of immune cell reserves and the inability to mobilize effective immune cells to clear the tumor. This hypothesis requires more experiments.
Diffuse cutaneous metastasis of esophageal squamous cell carcinoma is rare, and second-line chemotherapy and immunological checkpoint inhibitor treatment are not effective.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mitani S, Japan; Sugiyama Y, Japan S-Editor: Wang JL L-Editor: Filipodia P-Editor: Wang JL
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55843] [Article Influence: 7977.6] [Reference Citation Analysis (132)] |
| 2. | Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11444] [Cited by in RCA: 13214] [Article Influence: 1468.2] [Reference Citation Analysis (3)] |
| 3. | Torre LA, Siegel RL, Ward EM, Jemal A. Global Cancer Incidence and Mortality Rates and Trends--An Update. Cancer Epidemiol Biomarkers Prev. 2016;25:16-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2004] [Cited by in RCA: 2490] [Article Influence: 249.0] [Reference Citation Analysis (0)] |
| 4. | Quint LE, Hepburn LM, Francis IR, Whyte RI, Orringer MB. Incidence and distribution of distant metastases from newly diagnosed esophageal carcinoma. Cancer. 1995;76:1120-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 5. | Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol. 1993;29:228-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 554] [Cited by in RCA: 583] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 6. | Siewert JR, Ott K. Are squamous and adenocarcinomas of the esophagus the same disease? Semin Radiat Oncol. 2007;17:38-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 238] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 7. | Shaheen O, Ghibour A, Alsaid B. Esophageal Cancer Metastases to Unexpected Sites: A Systematic Review. Gastroenterol Res Pract. 2017;2017:1657310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Strickley JD, Jenson AB, Jung JY. Cutaneous Metastasis. Hematol Oncol Clin North Am. 2019;33:173-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Schwartz RA. Cutaneous metastatic disease. J Am Acad Dermatol. 1995;33:161-82; quiz 183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 296] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 10. | Ferreira L, Luís F, Cabral F. [Lung cancer and cutaneous metastasis]. Rev Port Pneumol. 2004;10:475-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Marcoval J, Penín RM, Llatjós R, Martínez-Ballarín I. Cutaneous metastasis from lung cancer: retrospective analysis of 30 patients. Australas J Dermatol. 2012;53:288-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Choate EA, Nobori A, Worswick S. Cutaneous Metastasis of Internal Tumors. Dermatol Clin. 2019;37:545-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Krathen RA, Orengo IF, Rosen T. Cutaneous metastasis: a meta-analysis of data. South Med J. 2003;96:164-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 281] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 14. | Shvili Y, Talmi YP, Gal R, Kessler E, Kolkov Z, Zohar Y. Basaloid-squamous carcinoma of larynx metastatic to the skin of the nasal tip. J Craniomaxillofac Surg. 1990;18:322-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Handa U, Kundu R, Dimri K. Cutaneous Metastasis: A Study of 138 Cases Diagnosed by Fine-Needle Aspiration Cytology. Acta Cytol. 2017;61:47-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Iizuka T, Kakegawa T, Ide H, Ando N, Watanabe H, Tanaka O, Takagi I, Isono K, Ishida K, Arimori M. Phase II evaluation of cisplatin and 5-fluorouracil in advanced squamous cell carcinoma of the esophagus: a Japanese Esophageal Oncology Group Trial. Jpn J Clin Oncol. 1992;22:172-176. [PubMed] |
| 17. | Kato K, Tahara M, Hironaka S, Muro K, Takiuchi H, Hamamoto Y, Imamoto H, Amano N, Seriu T. A phase II study of paclitaxel by weekly 1-h infusion for advanced or recurrent esophageal cancer in patients who had previously received platinum-based chemotherapy. Cancer Chemother Pharmacol. 2011;67:1265-1272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 18. | Muro K, Hamaguchi T, Ohtsu A, Boku N, Chin K, Hyodo I, Fujita H, Takiyama W, Ohtsu T. A phase II study of single-agent docetaxel in patients with metastatic esophageal cancer. Ann Oncol. 2004;15:955-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 181] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 19. | Kudo T, Hamamoto Y, Kato K, Ura T, Kojima T, Tsushima T, Hironaka S, Hara H, Satoh T, Iwasa S, Muro K, Yasui H, Minashi K, Yamaguchi K, Ohtsu A, Doki Y, Kitagawa Y. Nivolumab treatment for oesophageal squamous-cell carcinoma: an open-label, multicentre, phase 2 trial. Lancet Oncol. 2017;18:631-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 307] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 20. | Haratani K, Hayashi H, Chiba Y, Kudo K, Yonesaka K, Kato R, Kaneda H, Hasegawa Y, Tanaka K, Takeda M, Nakagawa K. Association of Immune-Related Adverse Events With Nivolumab Efficacy in Non-Small-Cell Lung Cancer. JAMA Oncol. 2018;4:374-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 531] [Cited by in RCA: 766] [Article Influence: 127.7] [Reference Citation Analysis (0)] |