Published online Apr 16, 2013. doi: 10.12998/wjcc.v1.i1.34
Revised: February 16, 2013
Accepted: March 6, 2013
Published online: April 16, 2013
Processing time: 124 Days and 16 Hours
The commonest type of simple vaginal cyst is the Mullerian cyst. These are typically lined by columnar epithelium and contain serous or mucinous fluid. If blood is found in the cyst, the source is usually due to the presence of endometrial elements in the cyst wall. The cyst is then termed an endometriotic cyst. In this case report, we have described a woman with a symptomatic 3 cm upper vaginal cyst who underwent surgical excision of the cyst. The cyst cavity was found to be full of old dark blood and mucous, however the wall contained no endometrial tissue and was lined by columnar epithelium which stained positive for mucous with mucicarmine. No cause for the intracystic hemorrhage was identified. We conclude that intracystic hemorrhage can occur in a simple Mullerian vaginal cyst in the absence of endometrial components.
Core tip: The commonest type of simple vaginal cyst is the Mullerian cyst. These are typically lined by columnar epithelium and contain serous or mucinous fluid. If the cyst contains blood it is thought to be due to the presence of endometrial elements in the cyst wall. It is then termed an endometrial cyst. We describe a simple Mullerian vaginal cyst containing blood in which no endometrial tissue was found. No cause for the intracystic hemorrhage was identified. We conclude that intracystic hemorrhage can occur in a simple Mullerian vaginal cyst in the absence of endometrial components.
- Citation: Rivlin ME, Meeks GR, Ghafar MA, Lewin JR. Intracystic hemorrhage in a non-endometriotic mullerian vaginal cyst. World J Clin Cases 2013; 1(1): 34-36
- URL: https://www.wjgnet.com/2307-8960/full/v1/i1/34.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i1.34
Vaginal cysts are relatively common and of these the commonest type found in the upper vagina is the Mullerian cyst arising from paramesonephric duct remnants[1]. Mullerian cysts are usually lined by columnar endocervical-like cells but may be lined by endometrial or fallopian type epithelium[2]. The cyst fluid has been described as serous, mucinous or purulent-like[3]. We have not found a reference to intracystic blood other than with the endometriotic cyst. We report a case of intracystic blood in a Mullerian cyst lacking any endometrial component.
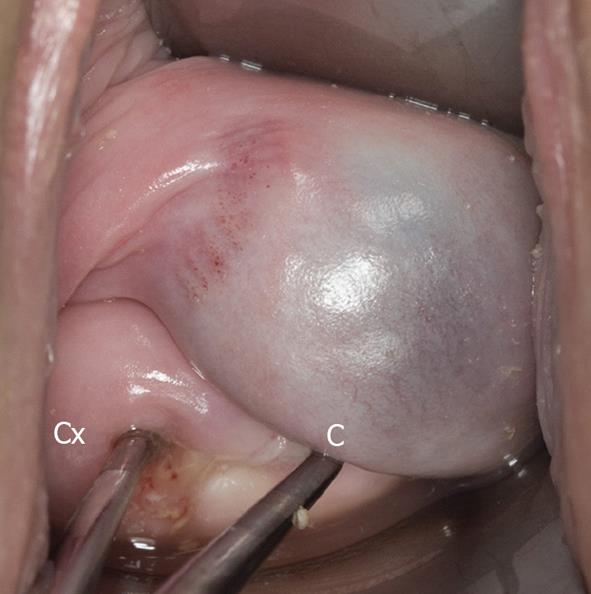
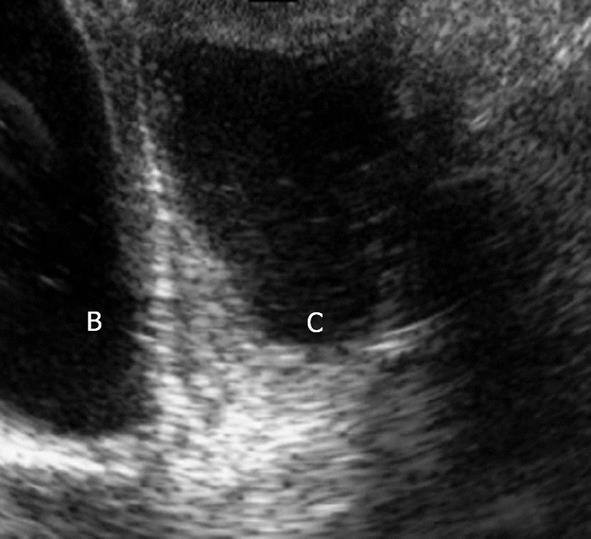
A 21-year-old nulliparous woman on oral contraceptives presented with a 3-year history of a vaginal cyst which was discovered on routine examination and was managed expectantly. Significant in her past history was a laparoscopy at age 19 for pelvic pain with essentially normal findings other than a 2 cm ovarian cyst which was biopsied and showed ovarian stroma. There was no evidence of endometriosis. She now felt that the cyst was causing discomfort with tampon use and intercourse sufficient for her to request its removal. A 3 cm cyst was seen on speculum examination in the left vaginal fornix at the 2-o’clock position antero-lateral to the cervix (Figure 1). The remainder of the pelvic examination was unremarkable. Pelvic sonogram noted a 3 cm. Echogenic fluid filled simple cyst anterior to the cervix with no connection to uterus or bladder (Figure 2). The pelvic organs were otherwise normal. Renal sonography showed normal urinary tracts. At surgery, on entry into the cyst cavity, 3 mL of dark old blood mixed with mucus was drained (Figure 3).
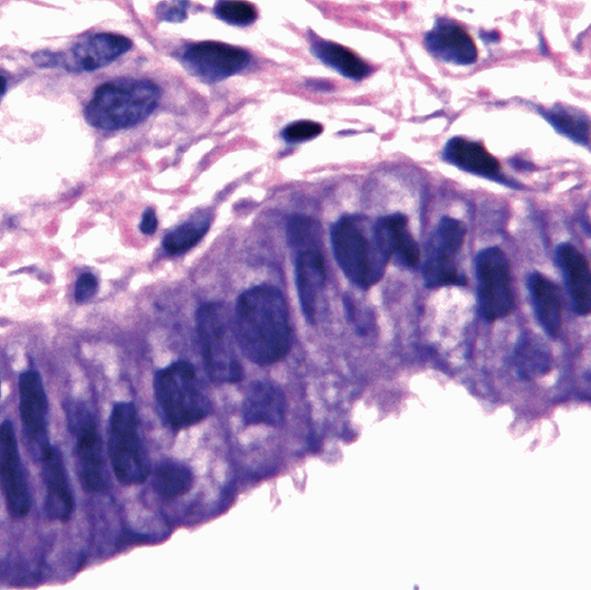
The cyst wall was excised and on microscopy found to be lined by columnar cells with intra-cytoplasmic mucus resembling endocervical epithelium (Figure 4).
Focal ciliated cells were also seen but no Bartholin gland tissue or vaginal adenosis was noted. Mucicarmine stain for mucus was positive. The pathologic findings were compatible with a diagnosis of a Mullerian cyst of endocervical type.
Vaginal cysts are usually asymptomatic and benign. They do not require excision unless they cause problems, pain and dyspareunia being the commonest complaints[2]. It is possible that the onset of symptomatology in our patient was related to the accumulation of blood in the cyst cavity. The finding of old blood in a vaginal cyst is highly suggestive of the presence of endometrial tissue in the cyst wall. Endometriotic cysts are uncommon. There were 6 in Evans series of 42 cases and 1 in Kondi-Pafitis series of 40 patients[1,3]. Endometriosis is defined as the ectopic implantation of endometrial glands and stroma. As regards the diagnosis of endometriosis in the vaginal area, 2 of the following 3 findings must be seen: endometrial glands, endometrial stroma and hemosiderin laden macrophages[2]. Distortion and destruction of the epithelium by hemorrhage is often present and there may be evidence of endometriosis elsewhere[1].
Another vaginal lesion that may contain glandular epithelium in the vagina is vaginal adenosis. This is attributed to incomplete replacement of vaginal columnar epithelium by squamous epithelium during embryogenesis. This lesion is often found in diethylstilbestrol exposed women and usually has a red grape-like mucosal appearance[2]. Another extremely rare condition, unilateral hematocolpos with ipsilateral renal agenesis was excluded by the negative laparoscopic pelvic examination and the sonographic demonstration of normal urinary tracts[4]. The absence of endometrial glands, stroma and hemosiderin laden macrophages in our patient excluded the diagnosis of endometriosis and the clinical appearance made the diagnosis of vaginal adenosis highly unlikely. Therefore the finding of hemorrhage in our patients’ imple Mullerian cyst is difficult to explain. Possibly local trauma may have been a factor, however the cyst was relatively avascular. It seems unlikely that endometrial tissue was destroyed by hemorrhage as there was no evidence of fibrosis or scarring in the cyst wall, furthermore laparoscopy 2 years prior, showed no evidence of pelvic endometriosis. We conclude that intracystic hemorrhage can occur in a simple Mullerian cyst in the absence of endometrial components.
P- Reviewer Mamishi S S- Editor Gou SX L- Editor A E- Editor Zheng XM
| 1. | Evans DM, Hughes H. Cysts of the vaginal wall. J Obstet Gynaecol Br Commonw. 1961;68:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Eilber KS, Raz S. Benign cystic lesions of the vagina: a literature review. J Urol. 2003;170:717-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 107] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 3. | Kondi-Pafiti A, Grapsa D, Papakonstantinou K, Kairi-Vassilatou E, Xasiakos D. Vaginal cysts: a common pathologic entity revisited. Clin Exp Obstet Gynecol. 2008;35:41-44. [PubMed] |
| 4. | Hollander MH, Verdonk PV, Trap K. Unilateral renal agenesis and associated Müllerian anomalies: a case report and recommendations for pre-adolescent screening. J Pediatr Adolesc Gynecol. 2008;21:151-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |