Copyright
©The Author(s) 2020.
World J Clin Cases. Jan 26, 2020; 8(2): 425-435
Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.425
Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.425
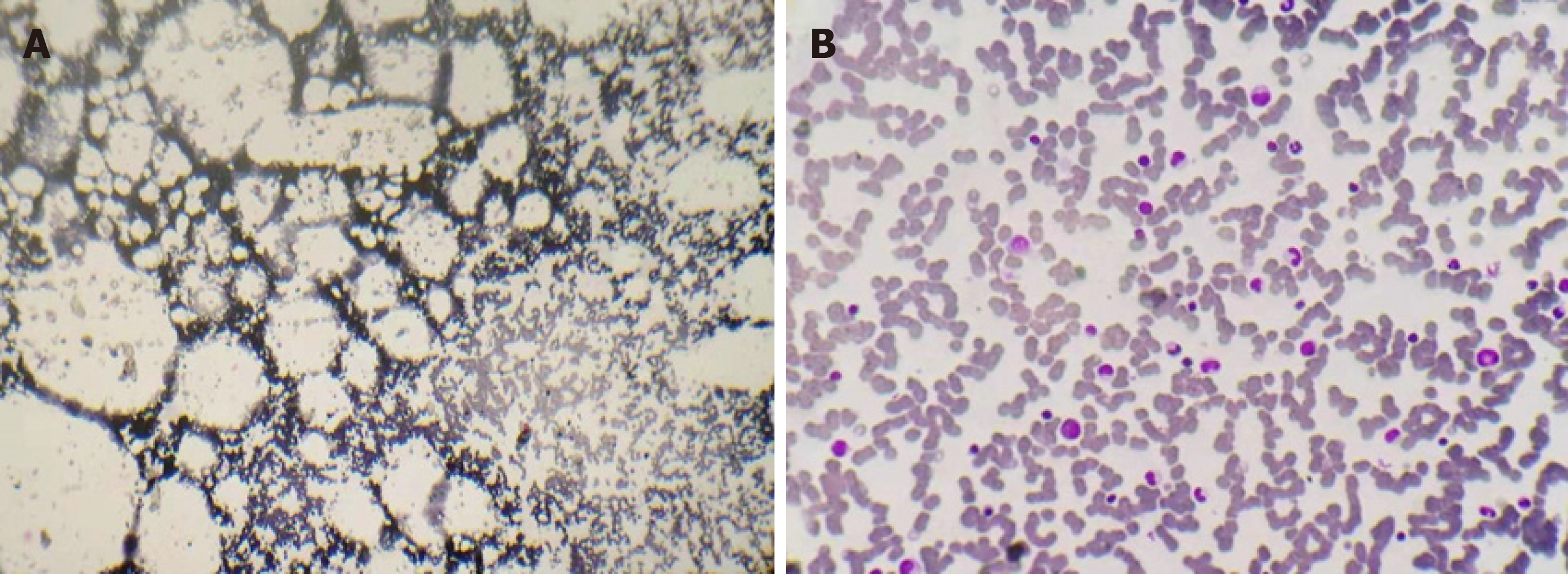
Figure 1 Bone marrow aspirate smears obtained from the posterior superior iliac spine of this refractory severe aplastic anemia patient.
A: A smear sampled 8 years ago when he was admitted to our center revealed severe hypocellularity with severe fatty replacement, predominantly lymphocytes, with few erythrocyte and myeloid precursors; B: A smear sampled on day 294 following mannitol and gentamycin treatment showed largely normal cellularity, with a normal proportion of myeloid precursors and lymphocytes as well as no atypical hematopoietic cells.
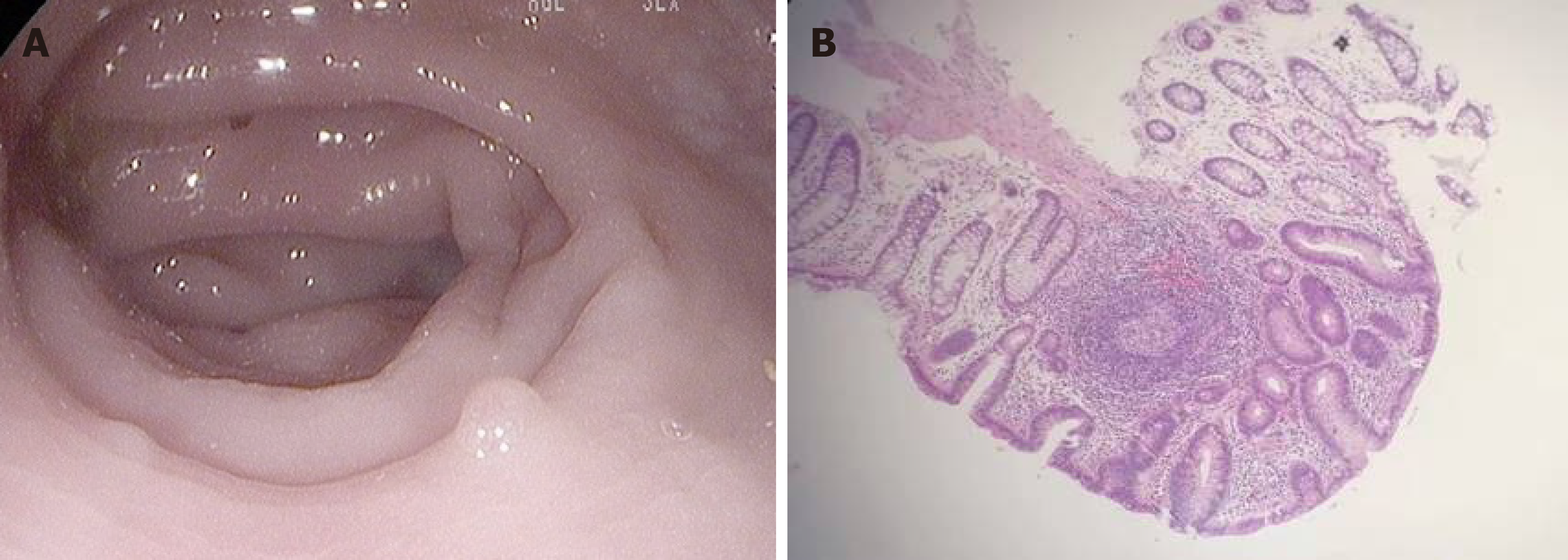
Figure 2 Gut inflammation verified by endoscopic examination.
A: Macroscopic examination of the large intestine showed that the mucous membrane was congested and swollen, the vascular lakes were absent, and there were several polyps in the sigmoid colon and rectum, confirming the presence of gut inflammation; B: Microscopic examination revealed that these polyps were enlarged lymphoid follicles which were structurally integrated, with the infiltration of a large amount of lymphocytes and plasma cells around the lymphoid follicles and underneath the mucous membrane, in accordance with inflammatory proliferation.
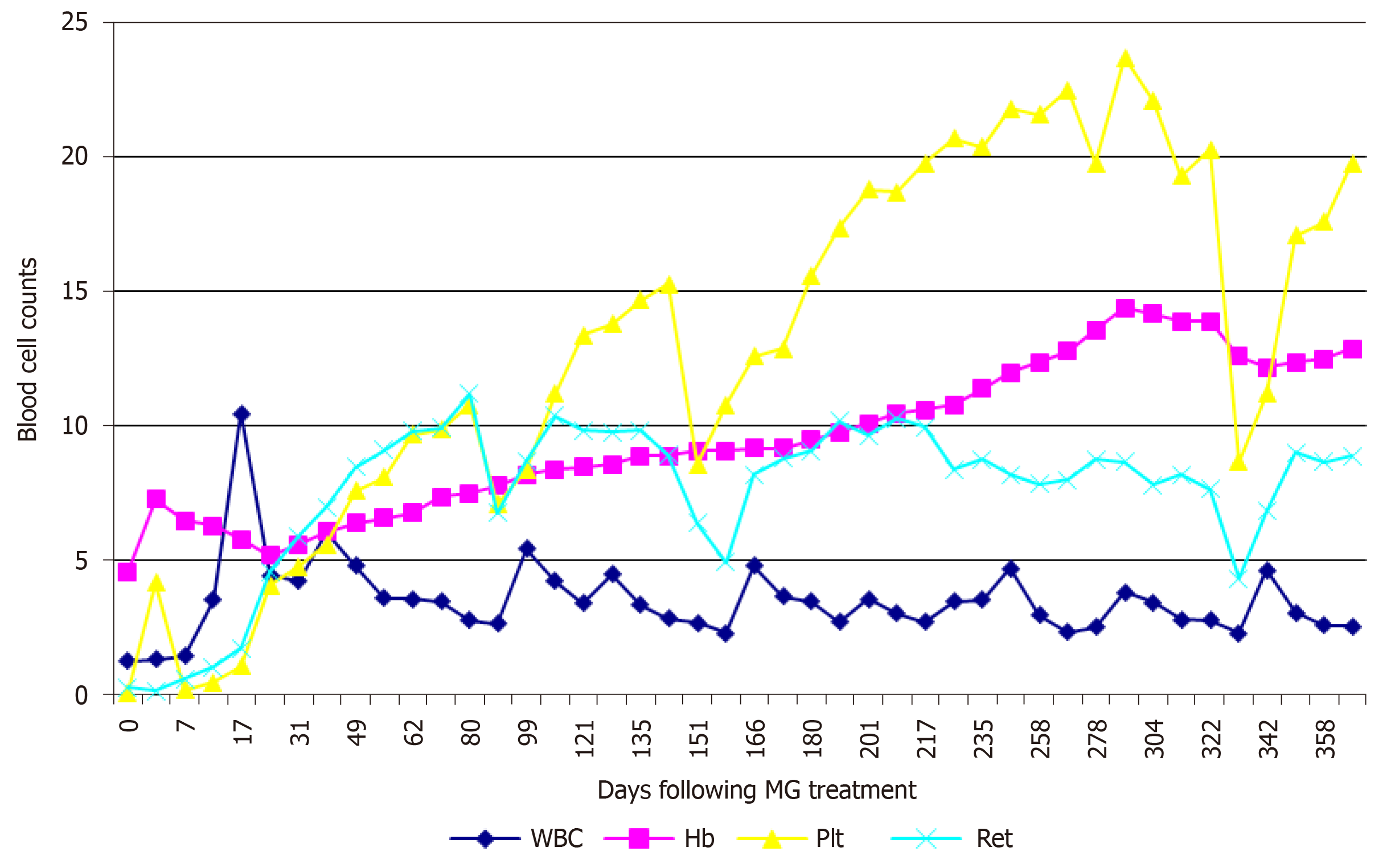
Figure 3 Excellent hematological response following mannitol-gentamycin or polyethylene-rifaximin treatments in the refractory severe aplastic anemia patient.
Mannitol-gentamycin treatments were performed on days 1, 31, and 92. Polyethylene-rifaximin (PR) treatments were performed on days 158, 189, 217, 248, 278, and 337. A transiently high responsiveness to recombinant human granulocyte colony stimulating factor was noted around day 17, and since then white blood cell counts (/µL) were maintained at relatively low levels. Plt (×10 /µL) and Ret (×10 /µL) levels increased rapidly, with each precipitous decrease occurring 7-8 wk after mannitol-gentamycin or PR treatments. Monthly administration of PR treatments was able to result in a stable hematopoietic response. Hb (g/dL) levels increased steadily.
- Citation: Zhao XC, Zhao L, Sun XY, Xu ZS, Ju B, Meng FJ, Zhao HG. Excellent response of severe aplastic anemia to treatment of gut inflammation: A case report and review of the literature. World J Clin Cases 2020; 8(2): 425-435
- URL: https://www.wjgnet.com/2307-8960/full/v8/i2/425.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i2.425