Copyright
©The Author(s) 2022.
World J Clin Cases. Jan 21, 2022; 10(3): 1000-1007
Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.1000
Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.1000
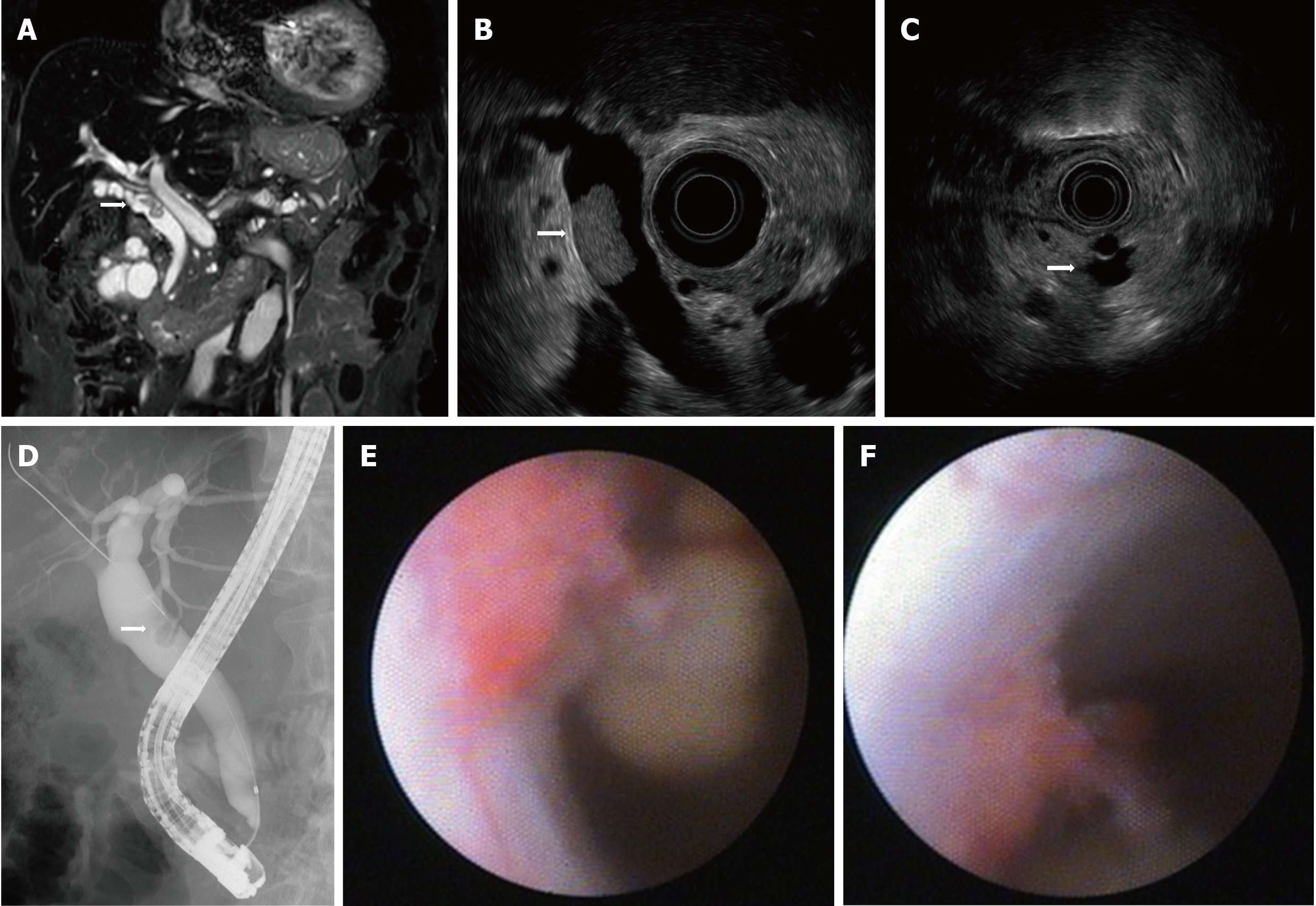
Figure 1 Imaging results upon referral.
A: Magnetic resonance cholangiopancreatography showing a filling defect in the common bile duct (CBD); B: Endoscopic ultrasound (EUS) showing a papillary tumor in the CBD; C: EUS showing intraductal papillary mucinous neoplasm with a mural nodule; D: ERC showing a filling defect of contrast agent in the CBD; E: Peroral cholangioscopy showing a papillary tumor in the CBD; F: Tumor spontaneously detached during examination.
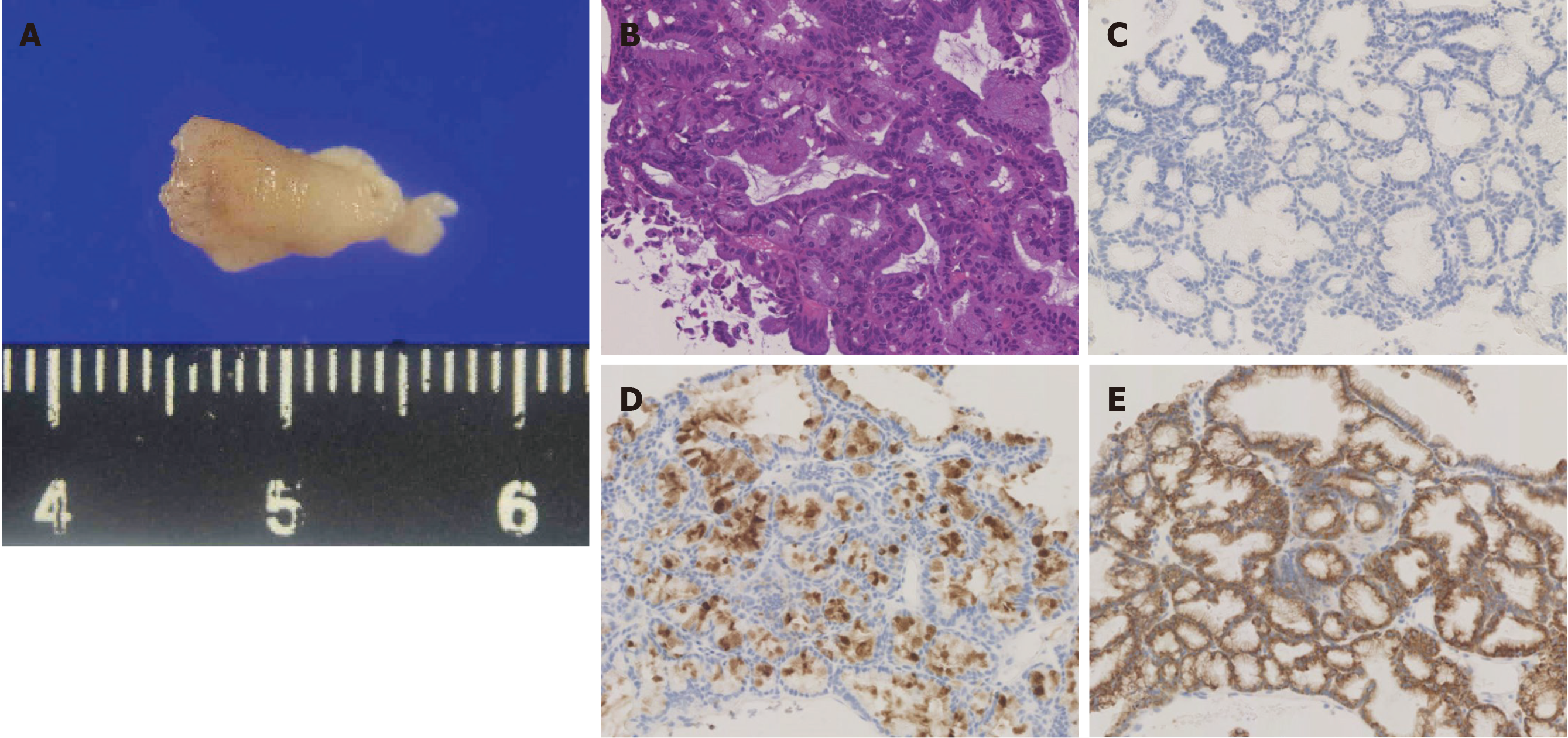
Figure 2 Pathological findings.
A: Pathological specimen obtained using peroral cholangioscopy (approximately 12 mm diameter); B: Hematoxylin and eosin stains showing intermediate nuclear atypia; C-E: Immunohistochemical analysis of MUC2 (undetectable) (C), MUC5AC (positive) (D), and MUC6 (positive) (E).
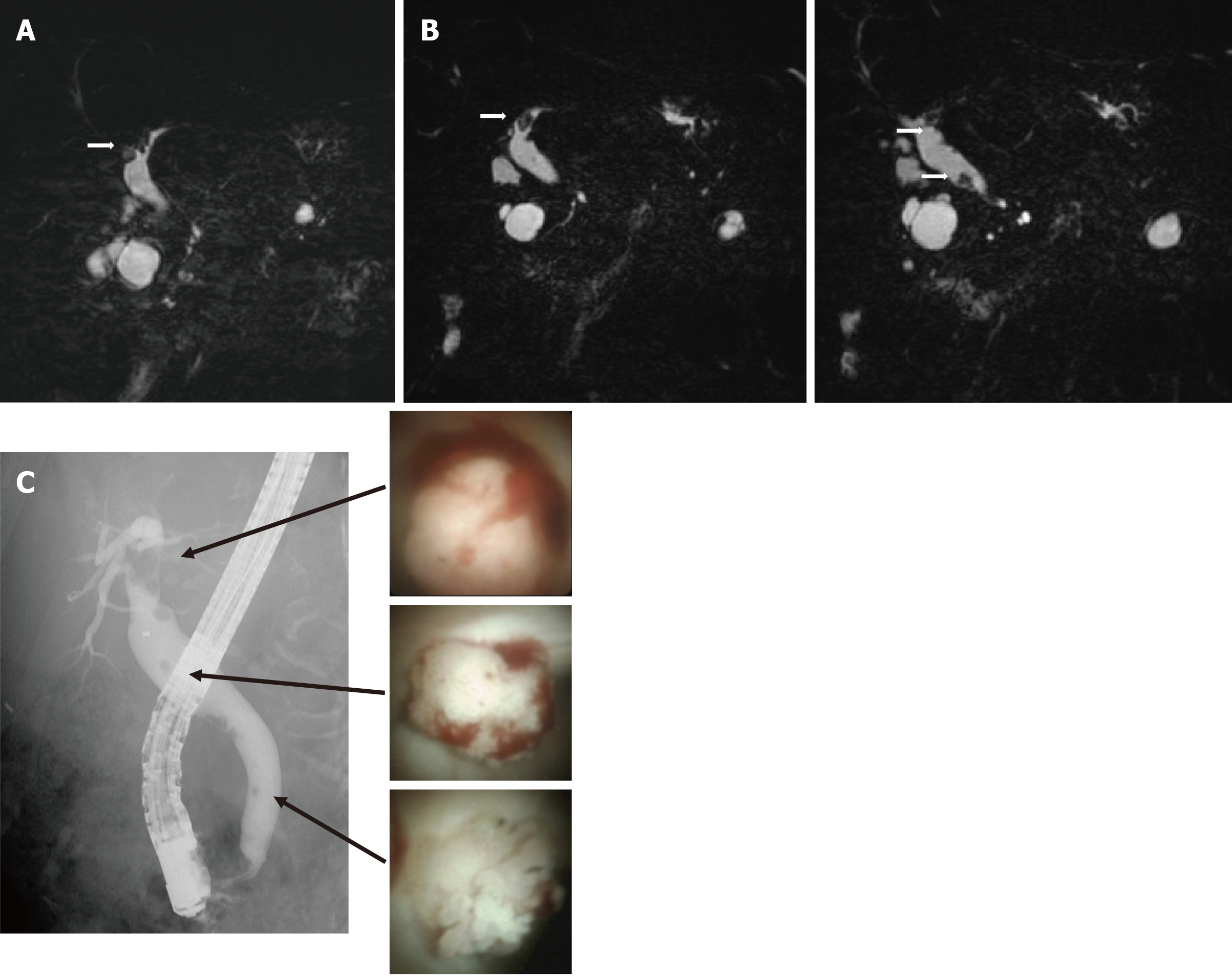
Figure 3 Follow-up imaging after diagnosis.
A: Six months after magnetic resonance cholangiopancreatography (MRCP) showing a defect of the left intrahepatic duct. B: One year after MRCP showing a defect in the left intrahepatic duct and multiple defects in the extrahepatic duct. C: Endoscopic retrograde cholangiography showing multiple filling defects of contrast agent in the extrahepatic and intrahepatic ducts. Peroral cholangioscopy showing papillary tumors in the intrahepatic and extrahepatic ducts.
- Citation: Fukuya H, Kuwano A, Nagasawa S, Morita Y, Tanaka K, Yada M, Masumoto A, Motomura K. Multicentric recurrence of intraductal papillary neoplasm of bile duct after spontaneous detachment of primary tumor: A case report. World J Clin Cases 2022; 10(3): 1000-1007
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/1000.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.1000