Published online Sep 19, 2025. doi: 10.5498/wjp.v15.i9.107924
Revised: May 22, 2025
Accepted: July 7, 2025
Published online: September 19, 2025
Processing time: 123 Days and 3.3 Hours
Phakic intraocular lens (IOL) implantation is a common treatment for high myopia. However, pre- and postoperative psychological changes, particularly anxiety and depression, are noteworthy concerns. Multiple studies have indicated a close relationship between ophthalmic diseases, including high myopia, glaucoma, anxiety, and depression.
To evaluate the impact of phakic IOL implantation on anxiety and depression in patients with high myopia.
Data from 136 patients with high myopia, who underwent phakic IOL implantation at the authors’ hospital between June 2024 and December 2024, were retrospectively analyzed. Clinical data were collected from the hospital’s electronic medical records system. Preoperative and one-month postoperative data were compared. Anxiety, depression, sleep quality, and quality of life were evaluated using the Hamilton anxiety scale, Hamilton depression scale, Pittsburgh Sleep Quality Index, and 36-item Short Form Health Survey, respectively.
Of 136 patients, 67.65% (n = 92) were female and 32.35% (n = 44) were male, with a mean ± SD age of 28.02 ± 5.72 years. The mean uncorrected visual acuity before and 1 month after treatment was 1.83 ± 0.24 log minimum angle of resolution (MAR) and 0.03 ± 0.07 log MAR, respectively. The mean best corrected visual acuity before and 1 month after treatment was 0.04 ± 0.07 log MAR and 0.01 ± 0.02 log MAR, respectively. All differences were statistically significant (P < 0.05). Compared with pretreatment, Hamilton anxiety scale and Hamilton depression scale scores significantly decreased 1 month post-treatment (P < 0.05). Furthermore, the Pittsburgh Sleep Quality Index score was significantly lower after than that before treatment (P < 0.05). The 36-item Short Form Health Survey quality of life score significantly improved after treatment (P < 0.05).
Phakic IOL implantation significantly reduces anxiety and depression and improves sleep quality and quality of life in patients with high myopia. This study provides new concepts for treating high myopia.
Core Tip: There is a well-documented association between ocular pathologies, particularly high myopia and glaucoma, and psychological comorbidities, such as anxiety and depression. The preoperative and postoperative psychological states of patients undergoing intraocular lens implantation surgery, including manifestations of anxiety and depression, represent significant clinical considerations. Evidence from this study demonstrates that intraocular lens implantation can effectively ameliorate anxiety and depressive symptoms in patients with high myopia, while concurrently yielding substantial improvement in both sleep quality and overall quality of life metrics.
- Citation: Chen XH, Dai XJ. Impact of phakic intraocular lens implantation on anxiety and depression in patients with high myopia. World J Psychiatry 2025; 15(9): 107924
- URL: https://www.wjgnet.com/2220-3206/full/v15/i9/107924.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i9.107924
High myopia is a common ophthalmological disease, defined as a refractive error exceeding -6.00 diopters or an axial length ≥ 26.5 mm, and is increasing in incidence globally[1,2]. The global prevalence of myopia is currently 22.9%, and projections suggest that, by 2050, nearly one-half of the global population will be myopic, with approximately 9.8% experiencing high myopia[3] and the highest prevalence in Asia[4]. Severe eye impairment, termed pathological myopia, may be caused by high myopia, according to previous reports[5]. In China, with changes in lifestyle and the widespread use of electronic devices, the incidence of myopia is increasing, and the prevalence of high myopia is trending toward younger ages: 27% of students have myopia, while the rate has increased to 81% among high-school students[4,6]. This proportion is even greater among those with higher education and those who are heavily reliant on electronic devices.
Notably, high myopia not only leads to decreased vision but also triggers a series of complications such as retinal detachment, macular degeneration, and glaucoma[7,8]. These complications further exacerbate visual burden and reduce quality of life, affecting not only physical health but also psychological well-being[9]. Studies have shown that individuals with high myopia often experience psychological problems such as anxiety and depression[10-12]. Multiple studies have indicated that limitations in the activities of daily living (such as driving, reading, and socializing) due to impaired vision can induce anxiety and depressive mood[13]. Furthermore, long-term reliance on thick corrective glasses or contact lenses may exacerbate self-image concerns, further increasing psychological stress levels. Therefore, understanding the psychological state of patients with high myopia and developing appropriate interventions is particularly important.
In recent years, phakic intraocular lens (IOL) implantation, a method for correcting myopia through minimally invasive surgery by implanting a specially designed artificial lens inside the eye, has emerged as a safe and effective treatment option[14]. Unlike traditional corneal surgery, phakic IOL technology does not require corneal ablation, but directly achieves refractive correction within the eye, similar to wearing a contact lens inside the eye[15,16]. It has become the mainstream correction method for high myopia and has witnessed significant technological progress in recent years. However, psychological changes before and after surgery, especially anxiety and depression, have not been fully addressed[17]. Therefore, an in-depth exploration of the impact of phakic IOL implantation on the psychological state of patients with high myopia is of significant clinical importance.
Accordingly, the present study aimed to evaluate the impact of phakic IOL implantation on anxiety and depression in patients with high myopia, with the hope of helping clinicians focus attention on the psychological health of patients during treatment, thereby improving treatment outcomes and patient quality of life.
This retrospective study included data from 136 patients diagnosed with high myopia, who underwent phakic IOL implantation at the authors’ hospital between June 2024 and December 2024. Patient clinical data were collected from the hospital’s electronic medical records system.
Structured interviews were conducted to gain a deeper understanding of patient psychological states. Interview content included the following: Preoperative expectations and anxieties regarding surgery; perceptions and understanding of vision improvement; subjective experiences of postoperative visual outcomes and discomfort; and perceived impact on life, study, and work. Interviews were conducted by professional psychological counselors or trained medical staff, using a semi-structured approach to ensure systematic and comprehensive content. The interview data supplemented the quantitative scale assessments with subjective feelings, providing richer qualitative information for analyzing psychological changes.
The inclusion criteria were as follows: Myopia > 8.00 D, cylinder < 2.00 D, and refractive stability in the previous 12 months; underwent phakic IOL implantation; and availability of comprehensive clinical information.
The exclusion criteria were as follows: Serious eye diseases, such as glaucoma, retinopathy, ocular inflammation, or other eye conditions that could impact surgical results; history of severe mental illness (e.g., major depression, bipolar disorder, schizophrenia, etc.); severe systemic diseases (e.g., heart disease, hepatic or renal insufficiency, etc.); history of other ophthalmic surgeries within 30 days before the procedure; and incomplete clinical data.
The present study was approved by the Institutional Ethics Committee of the authors’ hospital in accordance with the Declaration of Helsinki. Given the retrospective design of the study and the use of anonymized patient data, requirements for informed consent were waived by the Ethics Committee.
Initially, local anesthesia is administered intravenously accompanied by sedation under the supervision of an anesthesiologist. Subsequently, a corneal incision measuring 3.2 mm × 1.5 mm is created at the 12 o’clock position, facilitating the horizontal implantation of a foldable Artifex lens into the eye. Lens power is determined using the IOL Master 700 (Carl Zeiss Meditech AG, Jena, Germany) in conjunction with the phakic IOL implantation formula available in software version 7.1. A peripheral iridotomy is then performed at the 12 o’clock position with the incision rendered watertight, thereby obviating the need for suturing. Postoperative care involves the administration of levofloxacin eye drops for 5 days, alongside betamethasone eye drops, which were applied 4 times daily for 1 week. Subsequently, 0.1% fluoroethylene drops are administered on a gradually tapering schedule. Patients are scheduled for follow-up examination 1 month after the procedure.
Visual acuity (VA) was measured using a Snellen chart and reported as best-corrected VA (BCVA) and uncorrected VA (UCVA). Psychological assessment was performed using the Hamilton anxiety rating scale (HAM-A) and the Hamilton depression rating scale (HAM-D)[18]. The HAM-A consists of 14 items, each scored on a five-point scale ranging from 0 to 4, with higher scores indicating higher anxiety levels. The HAM-D includes 17 items, in which items 1, 2, 3, 7, 8, 9, 10, 11, 15, and 17 are rated on a 0-4 points scale, and items 4, 5, 6, 12, 13, 14, and 16 are rated on a 0-2 points scale. A higher total score indicates more severe depression.
Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI). The PSQI comprises seven dimensions: Sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, the use of hypnotic medications, and daytime functioning. Each dimension is scored on a scale of 0-3 points, with a total score ranging from 0 to 21 points. Higher scores indicate poorer sleep quality. Cronbach’s α coefficient for this scale is 0.710, indicating good reliability and validity[19]. Health status was assessed using the 36-item Short Form Health Survey (SF-36)[20], which includes 36 items, with a scoring range of 0-100 points, covering eight dimensions: Physical functioning, physical role functioning, bodily pain, general health, vitality, social functioning, emotional role functioning, and mental health.
Data processing and statistical analyses were performed using SPSS version 26.0 (IBM Corporation, Armonk, NY, United States). Continuous variables are expressed as mean ± SD using descriptive statistics, while categorical variables are expressed as numerical count and corresponding proportion (%). Differences with P < 0.05 were considered to be statistically significant.
Among 136 patients, 67.65% (n = 92) were female and 32.35% (n = 44) were male; the mean ± SD) age was 28.02 ± 5.72 years. The distribution of males and females is illustrated in Figure 1. The mean age of the participants was 28.02 ± 5.72 years, with a spherical degree of -9.52 ± 2.76 D, a cylindrical degree of -1.57 ± 0.63 D, an axis of 124.42 ± 72.13 degrees, an axial length of 27.25 ± 1.16 mm, a corneal thickness of 540.37 ± 34.28 μm, a corneal endothelial cell density of 2861.35 ± 217.16 cells/mm2, an intraocular pressure of 15.36 ± 2.93 mmHg, a mean duration of spectacle wear of 13.16 ± 5.25 years, and a mean duration of contact lens wear of 3.92 ± 4.26 years (Table 1).
| Variable | mean ± SD |
| Age (year) | 28.02 ± 5.72 |
| Sphere (diopters) | -9.52 ± 2.76 |
| Cylinder (diopters) | -1.57 ± 0.63 |
| Axis (degrees) | 124.42 ± 72.13 |
| Axial length (mm) | 27.25 ± 1.16 |
| Corneal thickness (μm) | 540.37 ± 34.28 |
| Corneal endothelium (cells/mm2) | 2861.35 ± 217.16 |
| Intraocular pressure (mmHg) | 15.36 ± 2.93 |
| Length of wearing spectacle (year) | 13.16 ± 5.25 |
| Length of wearing contact lens (year) | 3.92 ± 4.26 |
Patients’ mean pretreatment UCVA was 1.83 ± 0.24 Log minimum angle of resolution (MAR) and 0.03 ± 0.07 Log MAR one month after treatment. The mean pretreatment BCVA was 0.04 ± 0.07 Log MAR and 0.01 ± 0.02 Log MAR one month after treatment. All differences were statistically significant (P < 0.05) (Table 2).
| Variables | UCVA (log MAR) | BCVA (log MAR) | P value |
| Before treatment | 1.83 ± 0.24 | 0.04 ± 0.07 | < 0.001 |
| After treatment | 0.03 ± 0.05 | 0.01 ± 0.02 | 0.026 |
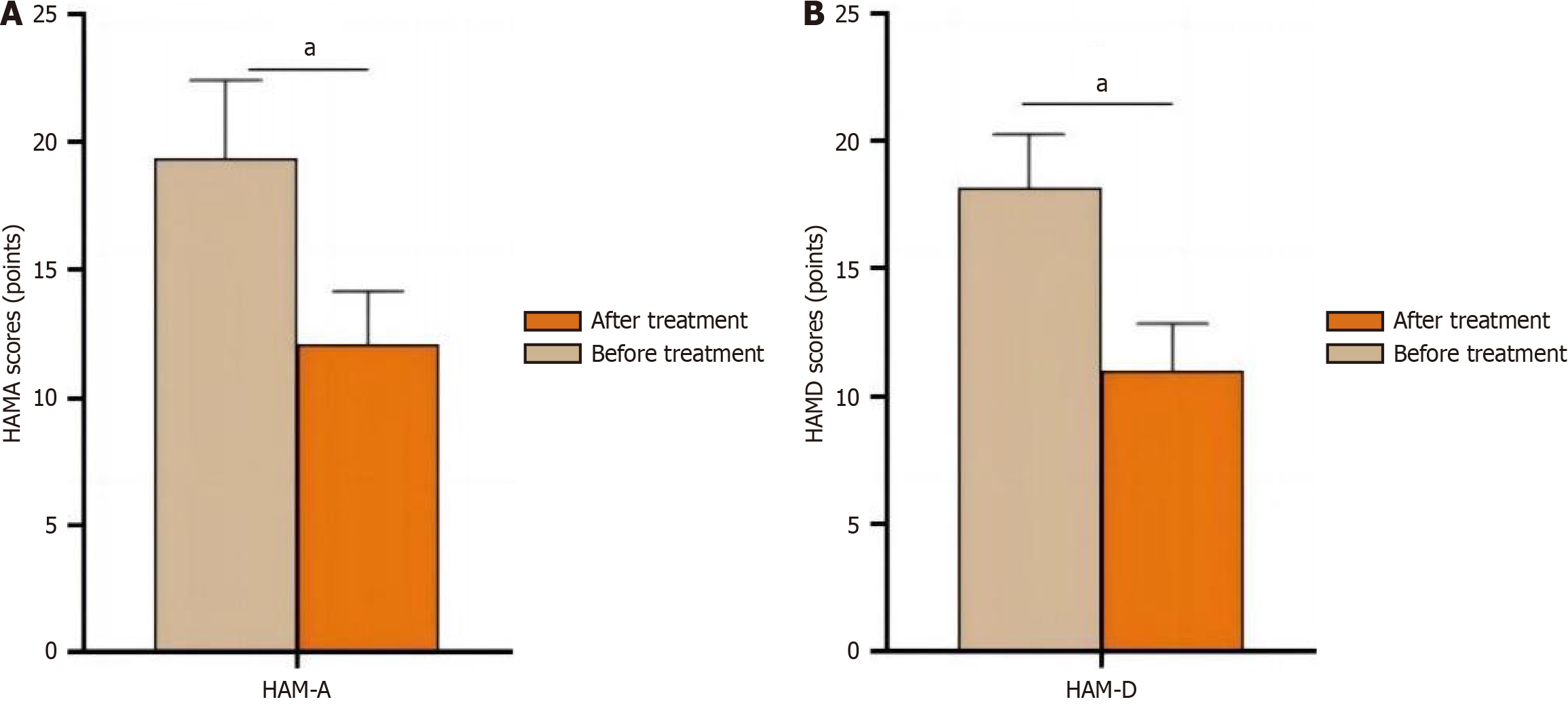
The mean pretreatment HAM-A score was 19.35 ± 3.09 and 12.12 ± 2.02 one month after surgery; the difference was statistically significant (P < 0.05) (Figure 2). The mean pretreatment HAM-D score was 18.15 ± 2.12 and 11.03 ± 1.86 one month after surgery; the difference was statistically significant (P < 0.05) (Figure 2).
The mean pretreatment PSQI total score was 18.89 ± 0.68, which decreased to 7.32 ± 0.56 after treatment, and all indicators exhibited significant improvement before and after treatment. All differences were statistically significant (P < 0.001) (Table 3).
| PSQI | Before treatment | After treatment | P value |
| Sleep efficiency | 2.82 ± 0.33 | 1.16 ± 0.52 | < 0.001 |
| Sleep quality | 2.77 ± 0.46 | 0.92 ± 0.45 | |
| Sleep disorder | 2.78 ± 0.37 | 0.87 ± 0.43 | |
| Sleep time | 2.89 ± 0.32 | 1.29 ± 0.58 | |
| hypnotic | 2.36 ± 0.48 | 0.87 ± 0.32 | |
| Sleep time | 2.64 ± 0.41 | 0.95 ± 0.35 | |
| Daytime dysfunction | 2.49 ± 0.38 | 0.71 ± 0.37 | |
| Total sores | 18.89 ± 0.68 | 7.32 ± 0.56 |
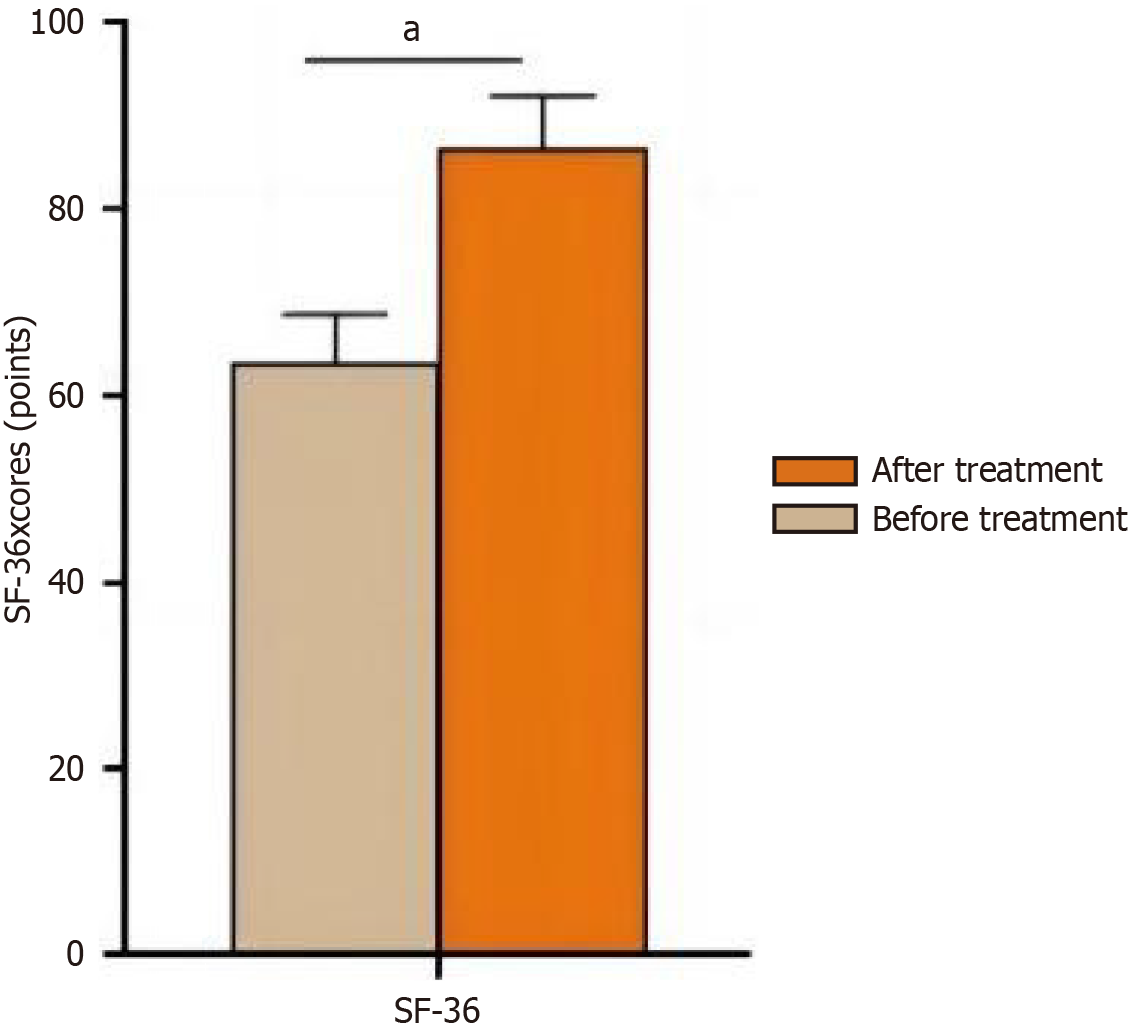
The mean pretreatment SF-36 score was 63.53 ± 5.12 and 86.72 ± 5.36 after treatment; the scores after treatment exhibited a statistically significant increase (P < 0.05) (Figure 3).
Results of the present study demonstrated that phakic IOL implantation significantly improved anxiety and depression in patients with high myopia. High myopia, generally defined as a refractive error of -6.00 diopters or greater, is not only associated with a higher risk for serious ocular complications, such as retinal detachment, glaucoma, and macular degeneration, but also has a profound impact on the activities of daily living and mental health. Limitations in visual function, concerns regarding potential vision loss, and social stigma related to high myopia can contribute to elevated levels of anxiety and depression in affected individuals. Understanding this background is crucial to interpret the significance of our findings. Before treatment, the patients’ mean HAM-A score was 19.35 ± 3.09, which decreased to 12.12 ± 2.02 one-month postoperatively. The HAM-D score decreased from 18.15 ± 2.12 to 11.03 ± 1.86, both of which were statistically significant (P < 0.05). This result is consistent with previous studies, indicating that ophthalmic surgery, especially for high myopia, can alleviate psychological burden[21-24]. In addition, the study revealed that phakic IOL implantation also significantly improved patient VA (UCVA improved from 1.83 ± 0.24 to 0.03 ± 0.07 Log MAR, and the mean BCVA was 0.04 ± 0.07 Log MAR, which improved to 0.01 ± 0.02 Log MAR one month after treatment). Given the detrimental effects of high myopia on mental health, the significant improvement in VA achieved through phakic IOL implantation likely addresses the root cause of psychological distress. By restoring clear vision and reducing the risk for vision-related complications, surgery effectively alleviates patient concerns regarding eye health, thereby reducing anxiety and depression scores. This not only highlights the therapeutic value of phakic IOL implantation for high myopia but also emphasizes the importance of considering the psychological well-being of patients with refractive disorders in clinical practice. A possible reason for this is that patients with high myopia often exhibit higher levels of anxiety and depression due to fear of vision loss. After surgery, the patients’ visual quality significantly improved, which effectively alleviated their psychological burden, thereby reducing their anxiety and depression scores. Furthermore, in this study, 67.65% of patients were female and 32.35% were male. Previous research has indicated that sex may contribute to differences in patients’ psychological responses and coping mechanisms, particularly when facing visual impairment and surgical risks. Women also exhibit higher levels of anxiety and psychological needs[25]. Future research should focus on sex differences and systematically analyze changes in preoperative and postoperative anxiety, depression, and quality of life in both males and females, with the aim of providing a theoretical basis for personalized interventions and improving the precision and effectiveness of treatment.
This study also found that patient PSQI scores significantly decreased after surgery, from 18.89 ± 0.68 to 7.32 ± 0.56, with a statistically significant difference (P < 0.001). Improvement in sleep quality is closely associated with the alleviation of anxiety and depression. Studies have shown that anxiety and depression can significantly affect sleep quality, and improvement in sleep quality may further promote mental health by regulating circadian rhythms and balance of neurotransmitters (such as serotonin)[26,27]. Therefore, phakic IOL implantation improves patient sleep quality by improving visual function, forming a virtuous cycle.
Furthermore, results of the present study also revealed that 1 month postoperatively, the SF-36 score significantly increased (from 63.53 ± 5.12 to 86.72 ± 5.36; P < 0.05), which further supports the positive impact of phakic IOL implantation on overall patient quality of life. The improvement in quality of life is not only reflected in the improvement of visual function but also includes the enhancement of mental health and social adaptability. Studies have shown that good visual function is closely associated with quality of life, especially among young(er) patients[28,29]. A possible explanation is that after surgery, patients can better participate in social activities, enhance their self-confidence and sense of happiness, thereby improving quality of life.
It should be noted that common complications, such as postoperative dry eye and glare, were not observed in the retrospective data of this study. However, considering the limitations of the study design and sample size (e.g., small number of cases, short follow-up period, and limitations in record-keeping), the occurrence of discomfort in some patients cannot be completely ruled out. In fact, postoperative discomfort, such as dry eye(s) and glare, may have a negative impact on patient psychological state, increasing the risk for anxiety and depression. Some preliminary studies have suggested that adverse visual experiences or discomfort after surgery may cause patients to worry about postoperative results, thereby affecting the speed and extent of psychological recovery. Therefore, future research with larger samples and longer follow-up periods is needed to systematically evaluate the incidence of these potential complications and their impact on mental health to more comprehensively understand the overall effect of refractive surgery on patient psychology.
The present study had several limitations, the first of which was its retrospective design. As such, it was not possible to completely eliminate the influence of confounding factors (such as the quality of postoperative care, level of family support, etc.), and may be subject to selection and information bias. Second, although this study included 136 patients, the sample size was relatively small. The mean age of the patients was 28 years, and elderly individuals or other groups were not included, resulting in insufficient sample representativeness. Moreover, the sample primarily consisted of a Chinese population, limiting the generalizability of the findings to elderly individuals or other ethnicities, and potentially limiting the universal applicability of the results. Third, this study only evaluated patients 1 month postoperatively, failing to reflect long-term effects. Fourth, the impact of different types of IOLs (e.g., monofocal, multifocal) on the psychological state was not analyzed. Future research should explore the influence of differences in visual quality associated with different IOL types on mental health. Furthermore, considering the variety of ophthalmic surgeries performed in clinical practice, future investigations should be prospective and multicenter in design, with extended follow-up periods and include control groups for other surgical types (e.g., photorefractive keratectomy and corneal refractive surgery). This would highlight the advantages of femtosecond laser-assisted corneal surgery, lens replacement, and other procedures compared with refractive surgery, thereby more clearly verifying the potential impact of postoperative discomfort, such as glare and dry eye, on psychological state and providing a more comprehensive basis for treatment strategies.
In summary, phakic IOL implantation has a significant effect on anxiety and depression in patients with high myopia, and significantly improves sleep quality and quality of life. These results provide important references for clinical practice. We recommended including psychological assessment in the routine follow-up program of phakic IOL implantation and providing psychological support and intervention when necessary to improve the overall treatment effect and quality of life.
| 1. | Wen K, Zhang L, Cai Y, Teng H, Liang J, Yue Y, Li Y, Huang Y, Liu M, Zhang Y, Wei R, Sun J. Identification and characterization of extrachromosomal circular DNA in patients with high myopia and cataract. Epigenetics. 2023;18:2192324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 2. | Wen K, Shao X, Li Y, Li Y, Li Y, Wang Q, Su R, Zhang L, Cai Y, Sun J, Zhang Y. The plasminogen protein is associated with high myopia as revealed by the iTRAQ-based proteomic analysis of the aqueous humor. Sci Rep. 2021;11:8789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Xiao H, Jiang D, Wang Y, Sun B, Li C, Lin Y, Liu L, Huang X, Vasudevan B, Chen Y. A comparative study of the prevalence of myopia and behavioral changes in primary school students. BMC Ophthalmol. 2022;22:370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Yang K, Li J, Zhang W, Liu Z, Song C, Zhao Y. Comparison of pre-chop technique using a reverse chopper and classic stop-and-chop technique in the treatment of high myopia associated with nuclear cataract. BMC Surg. 2022;22:206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Mori K, Kurihara T, Miyauchi M, Ishida A, Jiang X, Ikeda SI, Torii H, Tsubota K. Oral crocetin administration suppressed refractive shift and axial elongation in a murine model of lens-induced myopia. Sci Rep. 2019;9:295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Zhu Q, Tang Y, Guo L, Tighe S, Zhou Y, Zhang X, Zhang J, Zhu Y, Hu M. Efficacy and Safety of 1% Atropine on Retardation of Moderate Myopia Progression in Chinese School Children. Int J Med Sci. 2020;17:176-181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Shen EP, Chu HS, Cheng HC, Tsai TH. Center-for-Near Extended-Depth-of-Focus Soft Contact Lens for Myopia Control in Children: 1-Year Results of a Randomized Controlled Trial. Ophthalmol Ther. 2022;11:1577-1588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 8. | Zhang J, Li Z, Ren J, Wang W, Dai J, Li C, Huang X, Sun X, Liu L, Wang C. Prevalence of myopia: A large-scale population-based study among children and adolescents in weifang, china. Front Public Health. 2022;10:924566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 9. | Chen Y, Drobe B, Zhang C, Singh N, Spiegel DP, Chen H, Bao J, Lu F. Accommodation is unrelated to myopia progression in Chinese myopic children. Sci Rep. 2020;10:12056. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Peng W, Wang F, Sun S, Sun Y, Chen J, Wang M. Does multidimensional daily information predict the onset of myopia? A 1-year prospective cohort study. Biomed Eng Online. 2023;22:45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Pan F. Defocused Image Changes Signaling of Ganglion Cells in the Mouse Retina. Cells. 2019;8:640. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Guo LY, Sun H, Hu M, Jiang YH, Luo ZH. Mental health status of parents of young patients with high myopia. J Int Med Res. 2020;48:300060519873474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Lin Y, Luo S, Lu Q, Pan X. The Effects of Implantable Collamer Lens ICL Implantation in High Myopia Patients' Mental Health. Clin Ophthalmol. 2024;18:121-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Yang J, Zou Z, Wu M, He R, Nong Y, Li H, Zhou S. Development and validation of a new multivariable prediction model to estimate risk of abnormal vault. BMC Ophthalmol. 2023;23:203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 15. | Zheng LY, Zhu SQ, Su YF, Zou HY, Wang QM, Yu AY. Comparison between toric and spherical phakic intraocular lenses combined with astigmatic keratotomy for high myopic astigmatism. Eye Vis (Lond). 2017;4:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Demmin DL, Silverstein SM. Visual Impairment and Mental Health: Unmet Needs and Treatment Options. Clin Ophthalmol. 2020;14:4229-4251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 119] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 17. | Virgili G, Parravano M, Petri D, Maurutto E, Menchini F, Lanzetta P, Varano M, Mariotti SP, Cherubini A, Lucenteforte E. The Association between Vision Impairment and Depression: A Systematic Review of Population-Based Studies. J Clin Med. 2022;11:2412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 18. | Zheng JH, Sun WH, Ma JJ, Wang ZD, Chang QQ, Dong LR, Shi XX, Li MJ, Gu Q, Chen SY, Li DS. Differences in neuroanatomy and functional connectivity between motor subtypes of Parkinson's disease. Front Neurosci. 2022;16:905709. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 19. | Meabon JS, Cook DG, Yagi M, Terry GE, Cross DJ, Muzi M, Pagulayan KF, Logsdon AF, Schindler AG, Ghai V, Wang K, Fallen S, Zhou Y, Kim TK, Lee I, Banks WA, Carlson ES, Mayer C, Hendrickson RC, Raskind MA, Marshall DA, Perl DP, Keene CD, Peskind ER. Chronic elevation of plasma vascular endothelial growth factor-A (VEGF-A) is associated with a history of blast exposure. J Neurol Sci. 2020;417:117049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Shang Y, Zhang Y, Liu J, Chen L, Yang X, Zhu Z, Li D, Deng Y, Zhou Z, Lu B, Fu CG. Decreased E2F2 Expression Correlates with Poor Prognosis and Immune Infiltrates in Patients with Colorectal Cancer. J Cancer. 2022;13:653-668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 21. | Liu Z, Sun S, Sun X, Wu Y, Huang Y. Differences of Anxiety and Depression in Dry Eye Disease Patients According to Age Groups. Front Psychiatry. 2022;13:930714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Li Z, Wei J, Lu S, Wang F, Xia Y. Association between myopia and anxiety: a cross-sectional study based on Chinese university freshmen. Ann Transl Med. 2023;11:298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Parravano M, Petri D, Maurutto E, Lucenteforte E, Menchini F, Lanzetta P, Varano M, van Nispen RMA, Virgili G. Association Between Visual Impairment and Depression in Patients Attending Eye Clinics: A Meta-analysis. JAMA Ophthalmol. 2021;139:753-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 24. | van der Aa HP, Comijs HC, Penninx BW, van Rens GH, van Nispen RM. Major depressive and anxiety disorders in visually impaired older adults. Invest Ophthalmol Vis Sci. 2015;56:849-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 162] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 25. | Nandi M, Schreiber KL, Martel MO, Cornelius M, Campbell CM, Haythornthwaite JA, Smith MT Jr, Wright J, Aglio LS, Strichartz G, Edwards RR. Sex differences in negative affect and postoperative pain in patients undergoing total knee arthroplasty. Biol Sex Differ. 2019;10:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 26. | Guo H, Zhang Y, Wang Z, Shen H. Sleep Quality Partially Mediate the Relationship Between Depressive Symptoms and Cognitive Function in Older Chinese: A Longitudinal Study Across 10 Years. Psychol Res Behav Manag. 2022;15:785-799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 27. | Al-Ameri LT, Hameed EK, Maroof BS. Sleep quality in COVID-19 recovered patients. Sleep Sci. 2022;15:168-171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 28. | Omar R, Anan NS, Azri IA, Majumder C, Knight VF. Characteristics of eye injuries, medical cost and return-to-work status among industrial workers: a retrospective study. BMJ Open. 2022;12:e048965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Paletta Guedes RA, Paletta Guedes VM, Freitas SM, Chaoubah A. Utility values for glaucoma in Brazil and their correlation with visual function. Clin Ophthalmol. 2014;8:529-535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |