Published online Aug 19, 2025. doi: 10.5498/wjp.v15.i8.106025
Revised: April 7, 2025
Accepted: June 18, 2025
Published online: August 19, 2025
Processing time: 176 Days and 3.1 Hours
Depression is a prevalent mental health disorder characterized by high relapse rates, highlighting the need for effective preventive interventions. This paper reviews the potential of reinforcement learning (RL) in preventing depression relapse. RL, a subset of artificial intelligence, utilizes machine learning algorithms to analyze behavioral data, enabling early detection of relapse risk and optimi
Core Tip: Reinforcement learning (RL) holds significant promise in preventing depression relapse by enabling personalized and adaptive mental health interventions. By leveraging advanced machine learning algorithms, RL can analyze behavioral data for early relapse risk detection and optimize treatment strategies tailored to individual needs. This study reviews the existing literature, highlighting RL’s potential to transform mental health care through personalized learning and data-driven decision-making. However, challenges such as algorithmic complexity and ethical considerations must be addressed. Future research should focus on larger-scale studies and interdisciplinary collaboration to establish RL as a viable tool for effective depression management and relapse prevention.
- Citation: Byeon H. Can reinforcement learning effectively prevent depression relapse? World J Psychiatry 2025; 15(8): 106025
- URL: https://www.wjgnet.com/2220-3206/full/v15/i8/106025.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i8.106025
Depression remains a formidable challenge in contemporary society, characterized by its pervasive nature and high relapse rates. The urgent need for effective preventive strategies grows as depression’s global burden increases. Recent advancements in artificial intelligence have introduced novel approaches to mental health care, with reinforcement learning (RL) emerging as a promising field of interest[1-3]. This study aims to comprehensively review the current landscape of research on the application of RL for preventing depression relapse, elucidating its potential and limitations. By systematically examining the existing literature, this study seeks to provide valuable insights into the viability of RL as a tool for reducing the burden of depression relapse, ultimately contributing to the development of more effective mental health strategies.
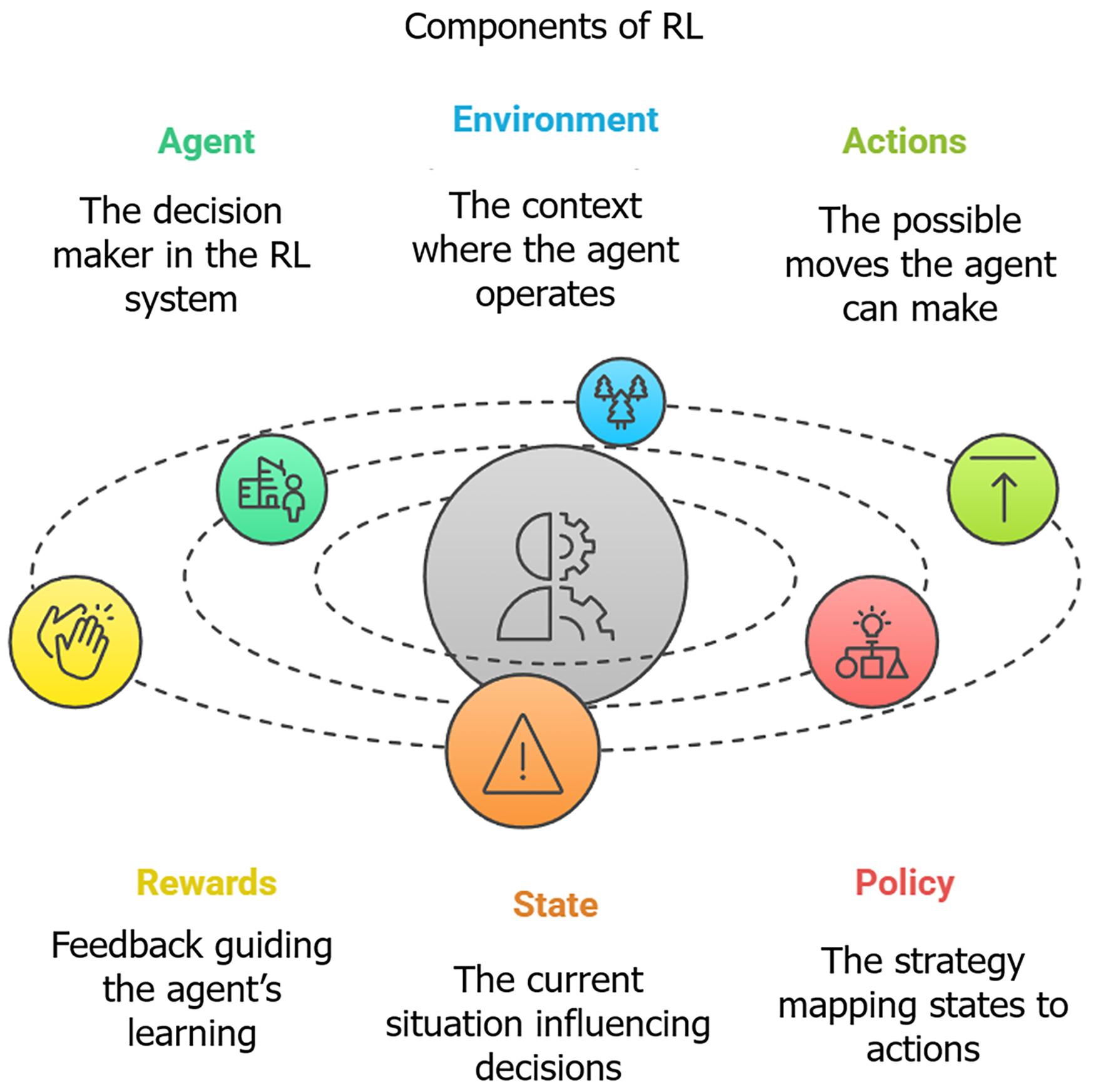
RL, a subfield of machine learning, empowers an ‘agent’ - typically the algorithmic core of a digital therapeutic system - to learn optimal decision-making by interacting with an ‘environment’, which in the clinical context represents the patient and their dynamic situation. Inspired by behavioral psychology, the agent learns through trial and error. Central to RL are its core components (Figure 1), which require careful definition within the clinical setting. The 'state' encapsulates the patient’s current condition, potentially defined by a combination of factors such as self-reported mood scores (e.g., daily ratings, Patient Health Questionnaire 9), behavioral data captured via sensors (e.g., activity levels, sleep patterns), engagement with the therapeutic platform, or even physiological markers. Based on this state, the agent selects an 'action' from a predefined set, such as suggesting a specific cognitive behavioral exercise, prompting for journaling, recom
The application of machine learning to mental health, particularly for depression relapse prevention, is a rapidly evolving field. While various paradigms like supervised learning can effectively predict relapse risk based on historical data patterns, they often fall short in dynamically optimizing sequences of personalized interventions over time. Traditional therapeutic approaches similarly rely on standardized protocols, potentially lacking the flexibility needed for the highly dynamic and individual nature of relapse trajectories. In this context, RL is gaining considerable attention as it offers distinct advantages. Unlike supervised methods that primarily focus on prediction from static datasets, RL excels at learning optimal policies for sequential decision-making through direct interaction with the environment - in this case, the patient’s evolving state. This allows for the development of personalized treatment strategies that adapt in real time to an individual’s condition and responses, aiming to maximize long-term well-being and minimize relapse. This inherent capacity for real-time, adaptive intervention planning provides a strong rationale for prioritizing RL in the development of next-generation depression relapse prevention tools.
A key advantage of RL in treating depression lies in its capacity for personalized learning. Depression manifests differently in each individual, influenced by a complex interplay of biological, psychological, and social factors. RL algorithms can analyze vast amounts of data to identify individual patterns and optimize interventions accordingly. This personalization is crucial in mental health, where it can significantly improve treatment effectiveness and patient adherence.
Several recent studies have explored the use of RL in creating personalized mental health treatment protocols. Gönül et al[4] emphasized the effectiveness of a clustering-based RL approach for tailoring e-Health interventions to individual patient needs. This personalized approach ensures that interventions are not only relevant to the patient’s unique circumstances but also delivered at optimal times, maximizing their impact. Furthermore, Boukhechba et al[5] highlight the potential of integrating mobile sensing with machine learning to develop dynamically adaptive mental health systems. These systems can adjust treatments based on continuous patient data monitoring, enabling proactive interventions that can potentially prevent depressive episodes. Such sophisticated technologies can allow mental health practitioners to provide more tailored and effective care, potentially leading to improved patient outcomes and reduced relapse rates. RL has also proven effective in promoting behavioral change, a critical aspect of depression treatment. By framing therapeutic goals in terms of rewards and penalties, RL can motivate patients to engage in healthier behaviors and adhere to treatment plans. RL-based interventions can encourage participation in mood-enhancing activities or medication adherence, providing positive reinforcement for compliance. Research has also explored the use of RL to gain mechanistic insights into depression. Brown et al[6] investigated how RL algorithms could map therapeutic components to specific symptoms of major depression, revealing potential behavioral and learning-based interventions. Similarly, Lauffenburger et al[7] studied the REINFORCE trial, which used RL to personalize communication strategies for improving medication adherence. Their findings demonstrated how carefully designed RL systems can adapt to individual behavioral patterns and enhance adherence by tailoring interactions to individual needs.
The potential of RL to improve treatment adherence is particularly important in managing chronic conditions, where consistent engagement with treatment protocols is crucial. For example, Queirazza et al[8] demonstrated how RL could be used to classify and predict responses to cognitive-behavioral therapy for depression, utilizing neural correlates of reward prediction errors to personalize patient care. These advancements in RL applications offer valuable insights into developing health interventions that maintain patient engagement and promote sustained behavioral change.
In the context of objective, data-driven decision-making, RL stands out for its ability to leverage data to inform treatment strategies. With the increasing availability of digital health data, including mobile health applications and wearable devices, RL algorithms can be employed to make informed decisions that are based on real-time data. This approach not only enhances the precision of treatment but also ensures that interventions are grounded in objective evidence rather than subjective judgment alone.
RL has introduced innovative avenues in the treatment of depression across multiple technological channels. In mobile app-based behavioral therapies, RL algorithms enable the delivery of interactive, personalized therapy sessions that are responsive to user performance, thereby maintaining engagement and effectiveness. Virtual reality (VR) enhances exposure therapy by allowing precise adjustment of anxiety-provoking stimuli through RL algorithms, leading to gradual desensitization and therapeutic benefit. Rahman et al[9] in 2023 demonstrated that RL-enhanced VR therapy can optimize exposure parameters to maximize therapeutic outcomes while ensuring patient comfort, suggesting a robust potential for treating various anxiety disorders, including those co-morbid with depression. Furthermore, in brain-computer interfaces (BCIs), the fusion of RL with neurofeedback offers adaptive training protocols that guide patients to modulate brain activity toward desired neural patterns. Huang et al[10] in 2021 highlighted the efficacy of such RL-BCI systems in enhancing emotion regulation and cognitive functioning, which are crucial for alleviating depressive symptoms. This study implies a transformative impact of RL-driven BCIs, presenting a powerful tool for personalizing mental health care[10].
In summary, the integration of RL paradigms within depression treatment regimens presents a promising avenue for advancing mental healthcare delivery. This approach offers the potential for personalized and adaptive interventions, leveraging data-driven insights to optimize treatment efficacy. By employing RL principles, clinicians can develop innovative therapeutic strategies that not only address the core symptoms of depression but also actively engage patients as collaborative partners in their recovery journey. Continued research is crucial to fully explore the potential of RL in improving mental health outcomes, mitigating the risk of depressive episodes, and ultimately enhancing the overall well-being of individuals affected by this prevalent condition.
The design and methodology of studies investigating RL for depression relapse prevention are vital for interpreting findings and clinical implications[11-16]. Study design intricacies like computational modeling and task-specific frameworks can significantly affect outcomes[17]. Participant selection criteria vary widely across studies regarding demographics, depression severity, and comorbidities[12]. Many studies target individuals with multiple depressive episodes due to their elevated relapse risk[13]. Intervention programs utilizing RL show diversity in form and intensity, often using digital platforms like mobile applications and online portals with gamification to enhance engagement[14]. Some studies explore VR environments with RL algorithms dynamically adjusting exposure levels[15]. Additionally, neurofeedback through BCIs leverages RL to help patients modulate brain activity[16]. Evaluating RL-based depression interventions requires a dynamic approach assessing symptom reduction (using Hamilton Depression Rating Scale, Beck Depression Inventory), quality of life improvements (via patient-reported outcomes), and relapse risk mitigation. RL paradigms facilitate explicit predictions of symptom trajectories[17]. RL mechanisms offer significant potential for relapse prevention through continuous monitoring of individual risk factors[18,19] (Table 1).
| Ref. | Algorithm/model | Target subjects | Intervention program | Main results |
| Lindqvist et al[11] | RL | Psychiatric disorders patients | Not specified | Examines underlying mechanisms linking mental illness with cellular aging through reinforcement learning |
| Pike and Robinson[12] | RL in mood disorders | Patients with mood/anxiety disorders | Meta-analysis | Identifies differences in RL patterns between mood disorders and control individuals |
| Crawley[13] | Computation and RL framework | Patients with depression | Behavioral activation | Highlights the role of RL in understanding changes in psychological therapy for depression |
| Weimann and Gißke[14] | Digital therapeutics with RL | General healthcare consumers | Personalizing behavioral transformations through digital platforms | Reviews potential of RL in personalizing therapy with gamified engagement tools |
| Petrescu et al[15] | RL in VR environments | Anxiety disorder patients | VR with biosignals integration | Uses VR environments with RL algorithms for anxiety detection and management |
| Guan et al[16] | Affective BCI | Adolescents | Neurofeedback and RL | Implements RL with BCIs to modulate brain activity and detect depression in adolescence |
| Kunisato et al[17] | Probabilistic RL | Patients with depression | Reward-based decision-making tasks | Analyzes effects of depression on reward-based decisions and action variability |
| Yoon et al[18] | Tree-based RL | Patients with hand deformity | Personalized treatment decisions | Applies RL to determine optimal personalized treatments in rheumatoid arthritis |
Contemporary research strongly supports the potential of RL methodologies in mitigating depressive symptoms and reducing relapse rates[20]. RL algorithms can significantly decrease the severity and frequency of depressive episodes by modeling cognitive responses and adjusting behavioral therapies[20]. Petre et al[21] in 2024 found substantial reductions in anxiety and depression symptoms, along with enhanced relapse prevention, particularly in RL-driven aftercare and mobile interventions. RL-based interventions also contribute to significant improvements in overall quality of life[22]. Zhang et al[22] emphasized RL’s potential in developing adaptive intervention plans addressing individual stressors and depressive symptoms. The potential of RL to prevent relapse warrants particular attention, with a growing body of research showing a significant reduction in recurrence likelihood among individuals in RL-based treatment programs. This is mainly due to RL’s personalization and adaptive nature, allowing tailored interventions and sustained behavioral changes[23]. Oyebode et al[23] in 2023 illustrated how RL’s capacity for personalization and real-time adaptation precisely targets treatment strategies, effectively mitigating stress and preventing relapse across mental health conditions. Deliu et al[24] in 2024 emphasized RL’s utility in constructing optimal adaptive interventions that dynamically adjust to individual patient progress and preferences. Ma et al[25] described how continuously monitoring patient progress and dynamically adjusting treatment strategies in real-time enhances the overall efficacy of mental health treatments.
Although the results are promising, there are several limitations that impact the generalizability and applicability of current research. One significant issue is the small sample sizes in many studies, which limit the statistical power and generalizability of the findings. Additionally, the short duration of most interventions makes it difficult to assess the long-term sustainability of treatment effects, particularly in terms of preventing relapse.
Another limitation is the potential for selection bias, as studies often include participants who are already inclined to engage in new interventions. This could skew the results, as these individuals might naturally have a higher likelihood of positive outcomes. Furthermore, the complexity of RL algorithms and the need for technological infrastructure can impede implementation in real-world clinical settings, especially in underserved areas with limited resources.
Finally, controlling confounding variables remains a challenge in studying RL-based interventions for depression. The multifaceted nature of depression, influenced by biological, psychological, and social factors, requires rigorous control of extraneous variables to isolate the effects of RL interventions. While current research provides promising initial evidence, the full potential of RL in preventing depression relapse is yet to be fully explored. To strengthen the evidence base and guide future clinical applications, larger-scale studies with rigorous methodologies are necessary. By addressing limitations such as sample size, intervention duration, and methodological rigor, researchers can establish RL as a viable and valuable addition to the clinical toolkit for managing depression.
One of the foremost advantages of RL is its capacity for personalized learning experiences. RL algorithms can dynamically adjust interventions to align with each individual’s unique needs and preferences, thereby improving therapeutic outcomes. By continuously analyzing patient data and updating treatment plans in real time, RL facilitates a highly personalized approach to mental health care. This degree of customization is particularly beneficial in addressing depression, where the variability in symptoms and individual responses to therapy necessitates a flexible and adaptive intervention strategy.
RL leverages vast amounts of data to inform decision-making, thereby enhancing the objectivity and precision of treatment plans. This data-driven approach allows for the identification of patterns and trends that may not be evident through traditional therapeutic methods. By utilizing real-time data from various sources, such as wearable devices and mobile applications, RL can provide timely insights and recommendations, ensuring that interventions remain relevant and effective.
The incorporation of RL into mental health interventions can significantly enhance patient motivation and engagement. By framing therapeutic activities as a series of rewards and challenges, RL can encourage patients to actively participate in their treatment journey. The use of gamification elements and adaptive feedback mechanisms further reinforces positive behaviors, helping patients to maintain engagement and adherence over time. This sustained motivation is crucial for achieving long-term therapeutic success and preventing relapse.
RL-based interventions can be delivered through digital platforms, such as mobile apps and online programs, making them highly accessible to a broad audience. This digital delivery model overcomes geographical and logistical barriers, enabling individuals in remote or underserved areas to access effective mental health care. Furthermore, the scalability of RL interventions allows for widespread implementation, potentially reaching large populations with minimal additional resources.
One of the primary challenges associated with RL is the complexity of its algorithms. The development and implementation of RL models require specialized knowledge and expertise, which can be a barrier for mental health practitioners and organizations lacking technical resources. Additionally, the intricate nature of these algorithms can complicate the interpretation and application of their outputs, necessitating robust training and support systems for effective use.
The use of RL in mental health raises several ethical concerns, particularly regarding data privacy and algorithmic bias. The reliance on extensive personal data to inform RL models necessitates stringent measures to protect patient confidentiality and secure sensitive information. Furthermore, the potential for bias in RL algorithms, stemming from skewed data inputs or flawed model design, poses a risk of perpetuating inequalities in treatment outcomes. Addressing these ethical issues is essential to ensure the responsible and equitable use of RL in mental health care.
Translating RL-based interventions from research settings to real-world clinical environments presents significant challenges. The integration of RL into existing therapeutic frameworks requires careful consideration of workflow, infrastructure, and resource allocation. Moreover, the variability in individual responses to RL interventions necessitates ongoing evaluation and adaptation, which can be resource-intensive and complex to manage in practice.
In summary, while RL offers substantial promise for enhancing depression treatment and relapse prevention, it is imperative to navigate its associated challenges carefully. By addressing the complexity of algorithms, ethical considerations, and clinical implementation hurdles, mental health professionals can leverage RL’s strengths to develop innovative, effective, and equitable interventions. As the field continues to evolve, ongoing research and collaboration will be key to realizing the full potential of RL in mental health care.
The future of RL in mental health care, particularly in the prevention of depression relapse, holds tremendous promise. As technological advancements continue to accelerate, RL is poised to play an increasingly integral role in developing sophisticated, personalized, and effective therapeutic interventions. This section explores the potential future directions for RL in mental health, as well as key recommendations to address current challenges and optimize its application.
The ongoing advancement of machine learning techniques is expected to yield more sophisticated RL algorithms capable of handling complex, multifaceted mental health scenarios. These algorithms will likely incorporate elements of deep learning and neural networks to enhance their predictive accuracy and adaptability. By processing and integrating diverse data sources, including behavioral, physiological, and environmental inputs, future RL models will offer increasingly nuanced and individualized treatment strategies.
The integration of RL with advanced sensor technologies presents an exciting frontier for mental health care. Wearable devices, smart home systems, and mobile technologies can provide continuous, real-time data streams to RL algorithms, facilitating more accurate assessments and timely interventions. This seamless integration will enable the creation of adaptive, context-aware therapeutic environments that respond dynamically to the patient’s needs and conditions.
Future RL applications are likely to feature more sophisticated human-machine interaction interfaces, fostering collaborative therapeutic relationships. By utilizing natural language processing and conversational agents, RL systems can engage patients in meaningful dialogue, providing support and guidance in a user-friendly and accessible manner. This interaction will not only improve patient engagement but also empower individuals to take an active role in their mental health management.
To facilitate the clinical implementation of RL-based interventions, the development of standardized evaluation tools is essential. These tools should be designed to assess the effectiveness, safety, and user experience of RL applications in various mental health contexts. By establishing clear benchmarks and guidelines, practitioners can more confidently integrate RL into existing therapeutic frameworks and monitor its impact over time.
Validating the long-term effectiveness of RL interventions is critical to ensuring their viability as sustainable mental health solutions. Future research should prioritize longitudinal studies that track patient outcomes over extended periods, providing insights into the durability of treatment effects and the potential for relapse prevention. This evidence will be crucial for gaining acceptance among clinicians and stakeholders and for informing best practices in RL application.
As RL becomes more prevalent in mental health care, addressing ethical and privacy concerns will be paramount. Strategies to mitigate algorithmic bias, ensure data security, and protect patient confidentiality must be rigorously developed and implemented. Engaging with ethicists, legal experts, and patient advocacy groups will be essential in establishing ethical guidelines and fostering public trust in RL technologies.
While RL has shown promise in the context of depression, its potential applications extend to a wide range of mental health disorders. Future research should explore RL-based interventions for conditions such as anxiety, posttraumatic stress disorder, bipolar disorder, and substance use disorders. By expanding the scope of RL applications, researchers can contribute to a more comprehensive understanding of its capabilities and limitations across different clinical scenarios.
The future of RL in mental health care will benefit from collaborative models that integrate the strengths of artificial intelligence and human expertise. By fostering partnerships between technologists, clinicians, and researchers, the field can develop hybrid approaches that leverage the unique insights and skills of each domain. Such collaboration will enhance the development of RL interventions that are both technologically advanced and clinically relevant.
In conclusion, the future of RL in mental health care is bright, with vast potential to transform depression treatment and relapse prevention. By embracing technological advancements, addressing clinical and ethical challenges, and fostering interdisciplinary collaboration, the mental health field can harness the full potential of RL to improve patient outcomes and advance the quality of care.
In conclusion, the integration of RL methodologies within mental healthcare presents a transformative paradigm for the management of depression and the prevention of relapse. By leveraging the capabilities of personalized learning, data-driven decision-making, and enhanced patient engagement, RL offers a promising avenue for the development of adaptive and efficacious therapeutic interventions. Despite the challenges associated with algorithmic complexity, ethical considerations, and the practicalities of clinical implementation, the potential benefits of RL in improving patient outcomes are substantial. Continued research focused on overcoming these hurdles is crucial.
However, this study did not conduct a systematic review according to PRISMA guidelines due to the limited number of prior studies specifically applying RL to depression. Future systematic reviews adhering to these guidelines are necessary as the field matures to provide a comprehensive understanding. Moving forward, realizing the potential of RL requires concrete interdisciplinary collaboration between artificial intelligence experts, clinicians, researchers, and importantly, patients. Essential pathways to foster this collaboration include establishing joint funding initiatives and grant proposals specifically targeting artificial intelligence in mental health, creating secure platforms and protocols for sharing diverse, ethically sourced, and anonymized datasets crucial for robust model training and validation, and forming interdisciplinary working groups to develop shared best practices, ethical guidelines, and standardized evaluation metrics. These collaborative structures are vital for refining RL applications and ensuring their safe, ethical, and responsible deployment within clinical contexts. Future research, facilitated by such partnerships, must prioritize the development of robust evaluation frameworks, validation across diverse populations, and methodologies that effectively bridge computational techniques with clinical insights and patient needs. Furthermore, significant effort should be directed towards exploring practical strategies for seamlessly integrating RL-driven tools into routine clinical workflows while ensuring stringent data privacy and security measures, thereby enhancing their real-world utility and safeguarding patient information.
| 1. | Khadija Singh K, Jabeen U, Bezzateev S. Artificial Intelligence Applications in Depression Management. In: Artificial Intelligence in Healthcare. Boca Raton: Taylor & Francis, 2024. |
| 2. | Rocha A, Camacho R, Ruwaard J, Riper H. Using multi-relational data mining to discriminate blended therapy efficiency on patients based on log data. Internet Interv. 2018;12:176-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Yasin S, Othmani A, Raza I, Hussain SA. Machine learning based approaches for clinical and non-clinical depression recognition and depression relapse prediction using audiovisual and EEG modalities: A comprehensive review. Comput Biol Med. 2023;159:106741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 4. | Gönül S, Namlı T, Coşar A, Toroslu İH. A reinforcement learning based algorithm for personalization of digital, just-in-time, adaptive interventions. Artif Intell Med. 2021;115:102062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Boukhechba M, Baglione AN, Barnes LE. Leveraging Mobile Sensing and Machine Learning for Personalized Mental Health Care. Ergonom Des. 2020;28:18-23. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Brown VM, Zhu L, Solway A, Wang JM, McCurry KL, King-Casas B, Chiu PH. Reinforcement Learning Disruptions in Individuals With Depression and Sensitivity to Symptom Change Following Cognitive Behavioral Therapy. JAMA Psychiatry. 2021;78:1113-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 59] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 7. | Lauffenburger JC, Yom-Tov E, Keller PA, McDonnell ME, Crum KL, Bhatkhande G, Sears ES, Hanken K, Bessette LG, Fontanet CP, Haff N, Vine S, Choudhry NK. The impact of using reinforcement learning to personalize communication on medication adherence: findings from the REINFORCE trial. NPJ Digit Med. 2024;7:39. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Queirazza F, Fouragnan E, Steele JD, Cavanagh J, Philiastides MG. Neural correlates of weighted reward prediction error during reinforcement learning classify response to cognitive behavioral therapy in depression. Sci Adv. 2019;5:eaav4962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 9. | Rahman MA, Brown DJ, Mahmud M, Harris M, Shopland N, Heym N, Sumich A, Turabee ZB, Standen B, Downes D, Xing Y, Thomas C, Haddick S, Premkumar P, Nastase S, Burton A, Lewis J. Enhancing biofeedback-driven self-guided virtual reality exposure therapy through arousal detection from multimodal data using machine learning. Brain Inform. 2023;10:14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 10. | Huang W, Wu W, Lucas MV, Huang H, Wen Z, Li Y. Neurofeedback training with an electroencephalogram-based brain-computer interface enhances emotion regulation. IEEE Trans Affective Comput. 2021;14:998-1011. [DOI] [Full Text] |
| 11. | Lindqvist D, Epel ES, Mellon SH, Penninx BW, Révész D, Verhoeven JE, Reus VI, Lin J, Mahan L, Hough CM, Rosser R, Bersani FS, Blackburn EH, Wolkowitz OM. Psychiatric disorders and leukocyte telomere length: Underlying mechanisms linking mental illness with cellular aging. Neurosci Biobehav Rev. 2015;55:333-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 235] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 12. | Pike AC, Robinson OJ. Reinforcement Learning in Patients With Mood and Anxiety Disorders vs Control Individuals: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2022;79:313-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 68] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 13. | Crawley DV. Using computation to understand change in psychological therapy: A reinforcement learning framework of behavioural activation for depression. [cited 15 January 2025]. Available from: https://discovery.ucl.ac.uk/id/eprint/10179646/. |
| 14. | Weimann T, Gißke C. Unleashing the Potential of Reinforcement Learning for Personalizing Behavioral Transformations with Digital Therapeutics: A Systematic Literature Review. Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies; 2024 Feb 21-23; Rome, Italy. Portugal: SciTePress Digital Library, 2024: 230-245. |
| 15. | Petrescu L, Petrescu C, Mitruț O, Moise G, Moldoveanu A, Moldoveanu F, Leordeanu M. Integrating Biosignals Measurement in Virtual Reality Environments for Anxiety Detection. Sensors (Basel). 2020;20:7088. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Guan Z, Zhang X, Huang W, Li K, Chen D, Li W, Sun J, Chen L, Mao Y, Sun H, Tang X, Cao L, Li Y. A Method for Detecting Depression in Adolescence Based on an Affective Brain-Computer Interface and Resting-State Electroencephalogram Signals. Neurosci Bull. 2025;41:434-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Kunisato Y, Okamoto Y, Ueda K, Onoda K, Okada G, Yoshimura S, Suzuki S, Samejima K, Yamawaki S. Effects of depression on reward-based decision making and variability of action in probabilistic learning. J Behav Ther Exp Psychiatry. 2012;43:1088-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 78] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 18. | Yoon AP, Song Y, Lin IF, Wang L, Chung KC. Tree-Based Reinforcement Learning for Identifying Optimal Personalized Treatment Decisions for Hand Deformity in Rheumatoid Arthritis. Plast Reconstr Surg. 2024;154:1259-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Liebenow B, Jones R, DiMarco E, Trattner JD, Humphries J, Sands LP, Spry KP, Johnson CK, Farkas EB, Jiang A, Kishida KT. Computational reinforcement learning, reward (and punishment), and dopamine in psychiatric disorders. Front Psychiatry. 2022;13:886297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Gregory S, Long JD, Klöppel S, Razi A, Scheller E, Minkova L, Papoutsi M, Mills JA, Durr A, Leavitt BR, Roos RAC, Stout JC, Scahill RI, Langbehn DR, Tabrizi SJ, Rees G. Operationalizing compensation over time in neurodegenerative disease. Brain. 2017;140:1158-1165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 21. | Petre LM, Piepiora PA, Gemescu M, Gheorghe DA. Internet- and mobile-based aftercare and relapse prevention interventions for anxiety and depressive disorders: a systematic review. Front Psychol. 2024;15:1474016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Zhang Y, Liu G, Huang H, Xiong R, Zhang H. Dual-stream collaborative tracking algorithm combined with reliable memory based update. Neurocomputing. 2022;480:39-60. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 23. | Oyebode O, Fowles J, Steeves D, Orji R. Machine Learning Techniques in Adaptive and Personalized Systems for Health and Wellness. Int J Hum-Comput Int. 2023;39:1938-1962. [DOI] [Full Text] |
| 24. | Deliu N, Williams JJ, Chakraborty B. Reinforcement Learning in Modern Biostatistics: Constructing Optimal Adaptive Interventions. Int Stat Rev. 2024. [DOI] [Full Text] |
| 25. | Ma X, Zhang Y, Huang J. Reachable set estimation and synthesis for semi-Markov jump systems. Inf Sci. 2022;609:376-386. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |