Published online May 19, 2023. doi: 10.5498/wjp.v13.i5.131
Peer-review started: January 21, 2023
First decision: January 31, 2023
Revised: February 2, 2023
Accepted: April 17, 2023
Article in press: April 17, 2023
Published online: May 19, 2023
Processing time: 117 Days and 20.4 Hours
In the beginning of the 1900s, the prevalence of catatonia in inpatient samples was reported to be between 19.5% and 50%. From the mid-1900s, most clinicians thought that catatonia was disappearing. Advances in medical sciences, particularly in the field of neurology, may have reduced the incidence of neurological diseases that present with catatonic features or mitigated their severity. More active pharmacological and psychosocial treatment methods may have either eliminated or moderated catatonic phenomena. Moreover, the relatively narrow descriptive features in modern classifications compared with classical texts and ascribing catatonic signs and symptoms to antipsychotic-induced motor symptoms may have contributed to an apparent decline in the incidence of catatonia. The application of catatonia rating scales introduced in the 1990s revealed significantly more symptoms than routine clinical interviews, and within a few years, the notion of the disappearance of catatonia gave way to its un-expected resurgence. Several systematic investigations have found that, on average, 10% of acute psychotic patients present with catatonic features. In this editorial, the changes in the incidence of catatonia and the possible underlying causes are reviewed.
Core Tip: Although the prevalence of catatonia was reported to be between 19.5% and 50% in the early 1900s, most clinicians thought that catatonia was disappearing by mid-century, However, more recent systematic investigations have found that catatonia continues to be a common clinical disorder with an average prevalence of 10%. The apparent historical changes in the prevalence of catatonia reflects shifts in the socio-cultural context of psychiatry, the type of service, diagnostic criteria, research methods, and advances in treatment and clinical practice. We propose the establishment of an international society and journal dedicated to the study of catatonia to facilitate understanding and research.
- Citation: Ungvari GS, Caroff SN, Csihi L, Gazdag G. Catatonia: “Fluctuat nec mergitur”. World J Psychiatry 2023; 13(5): 131-137
- URL: https://www.wjgnet.com/2220-3206/full/v13/i5/131.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i5.131
During most of the last century, in line with the prevailing Kraepelinian tradition, catatonia essentially was used to refer to catatonic schizophrenia, although a careful reading of Kraepelin’s textbook shows a more sophisticated view of catatonia[1-4]. In the two authoritative classical textbooks, the prevalence of catatonia in inpatient samples is reported to be between 19.5%[1] and 50%[5], whereas it was 35.4% according to the Wernicke–Kleist–Leonhard school[6]. However, from the mid-1900s, there was a growing consensus among clinicians that catatonia was becoming nearly extinct, as Mahendra[7] famously asked, “Where have all the catatonics gone?”. Such clinical impressions were supported by a few, although not all[8,9], epidemiological studies that attempted the nearly impossible task of determining the changes in the real prevalence of catatonia across several years or decades against the background of shifts in the socio-cultural context of psychiatry, the type of service (inpatient, outpatient, and community), diagnostic criteria, research methods, and advances in treatment and clinical practice in general.
Relatively comparable, albeit not necessarily reliable, rough estimates of the changes in the frequency of catatonia can be made by focusing on single sites when comparing two time periods. For example, between 1850 and 1950, the rate of first admissions for catatonia decreased from 6% to 0.5% in the Bethlem royal hospital, a leading hospital and academic center in London, United Kingdom[10]. Another example from Finland showed a decline in the frequency of admissions for catatonic schizophrenia from 40.1% to 11% over just 20 years from 1933–1935 to 1953-1955[11]. In two Polish hospitals, where catatonia was diagnosed very conservatively, the frequency of catatonic schizophrenia diagnoses decreased 190-fold from 1924–1929 to 1994–1999 and 36-fold from 1958–1963 to 1994–1999[12]. From 1964 to 1984, catatonic schizophrenia nearly disappeared entirely in a university hospital in Santiago, Chile[13]. In a Belgian academic center, based on a chart review of 19309 admissions, the diagnosis of catatonic schizophrenia decreased from 7.8% to 1.3% in the two consecutive decades of 1980–1989 and 1990–2000[14].
Several plausible reasons have been proposed for the decline in the rate of catatonia observed in the second part of the last century. Advances in medical sciences, particularly in the field of neurology, may have reduced the incidence of neurological diseases that present with catatonic features or mitigated their severity[7]. More active pharmacological and psychosocial treatment methods may have either eliminated or moderated catatonic phenomena. Moreover, the relatively narrow descriptive features in modern classifications compared with classical texts and ascribing catatonic signs and symptoms to antipsychotic-induced motor symptoms may have contributed to the reduced incidence of catatonia[15,16]. The application of catatonia rating scales introduced in the 1990s[17] revealed significantly more symptoms than routine clinical interview, suggesting that insufficient diagnostic practices were responsible for the under-recognition of catatonia[14].
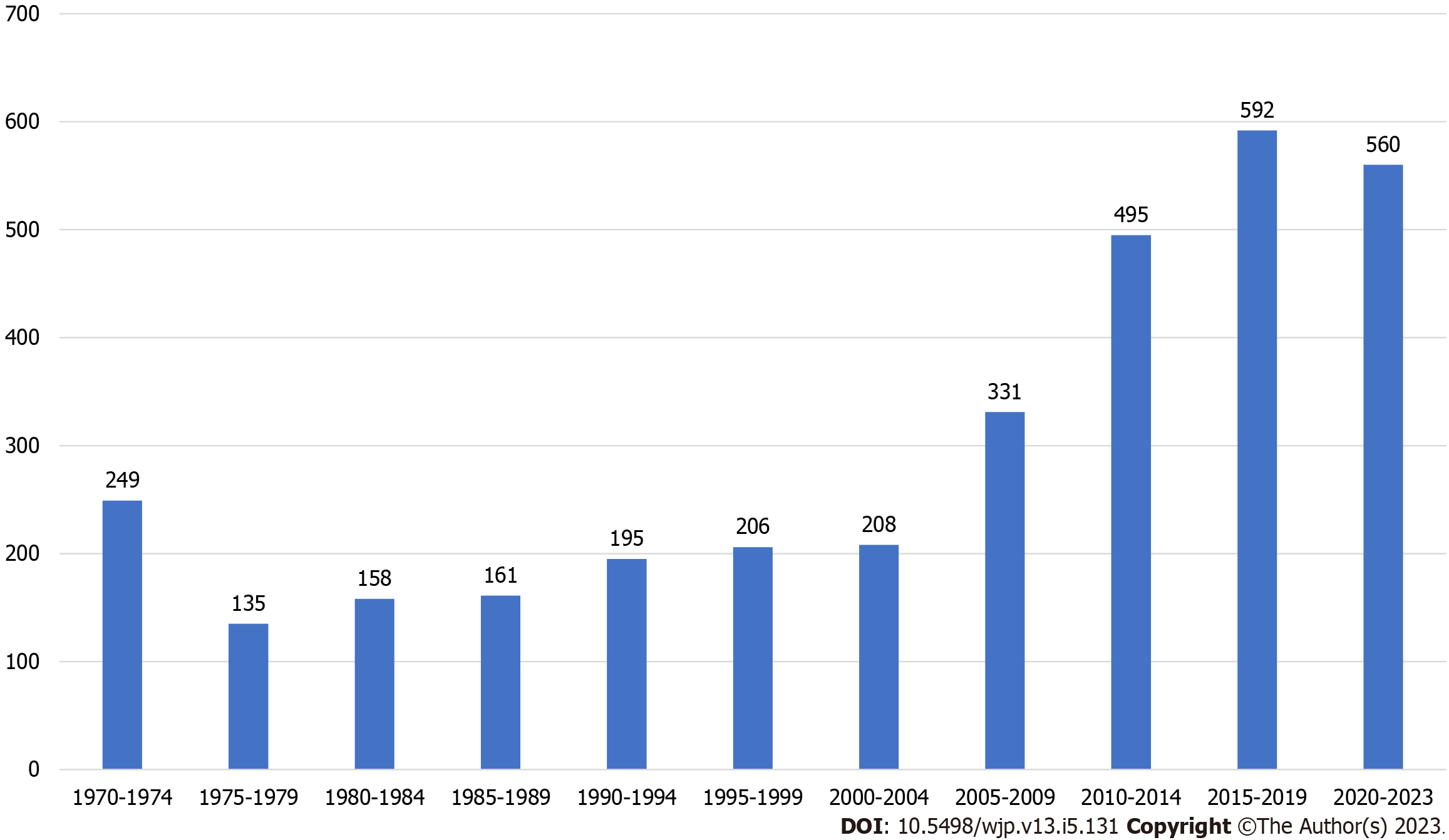
From the 1990s, the situation changed, and within a few years, the notion of the disappearance of catatonia gave way to its unexpected resurgence[18,19] (Figure 1). Several systematic investigations have found that, on average, 10% of acute psychotic patients present with catatonic features[20], with a wide range of frequencies from 1% in Nigeria[21], 3.7% in Mexico[22] to 38% in Greece[23], 50% in Belgium[24] and 68% in the United States[25]. The corresponding figures reached 20% for depression[26], 31% for mania[27], and almost 100% for the chronically hospitalized psychotic population[28]. Awareness has also broadened to encompass catatonia occurring in the context of general medical conditions[16,18]. Since the 1990s, interest in the epidemiological[16], clinical[29,30] and neurobiological[31,32] aspects of catatonia has continued unabated, stimulated by its semi-independent place in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition[33,34] and in addition to secondary catatonia occurring in the context a wide range of psychiatric and medical conditions also appeared as an independent diagnostic category in the International Classification of Diseases, 11th revision[35].
The apparent disappearance of catatonia from psychiatric practice and research for decades and its recent re-discovery raises serious questions. The intriguing fact is that a well-known and easily observable motor phenomena, which has been reported in such a high proportion in acute psychiatric admissions over the past two decades, was declared to be essentially extinct for approximately four decades in the second part of the last century. The logical argument is that, if catatonia had temporarily become extinct, there must have been a very significant environmental and/or neurobiological change responsible for this, which went unnoticed for a while and then stopped. However, there has been no suggestion that such panoramic environmental or biological changes affecting motor symptoms in psychiatric patients have occurred. However, if catatonia did not actually disappear, which is the likely scenario, the question remains how mainstream psychiatry missed an important aspect of mental disorders for decades. A possible answer to this puzzling question may provide important information about the nature of catatonia and psychiatric diagnostic practice. However, this is a complex issue and reaching a firm conclusion is unlikely as the available studies on catatonia are fraught with major methodological flaws that make it difficult to make comparisons between studies across time[16].
We posit that catatonia may have been modified in its manifestations and may have lessened in intensity and frequency due to advances in treatment of schizophrenia and mood disorders, but never disappeared entirely[15]. Rather, it was not given adequate attention by clinicians, particularly in the internationally dominant Anglo-American psychiatry with pockets of exceptions in Europe, such as at the Wernicke–Kleist-Leonhard school of psychiatry[6,36]. There are also indications that catatonia never disappeared in developing countries[37], but has occurred at a similar or even higher frequency and severity to those in Western settings[38] albeit possibly with a different symptom profile[39]. Over the past three decades, several Indian studies examined the phenomenology[40,41] and the frequency of catatonia in acute inpatient admissions that ranged from 4.8%[40] to 10.3%[41], 16.3%[42] and 37.2%[43].
In the following section, we outline some of the factors that support our view that the disappearance of catatonia was apparent, but not real. From a broader perspective, the temporary disappearance of catatonia in psychiatric research and practice during the middle decades of the 20th century is the logical consequence of the development of psychiatry in the last century.
In the second part of the 20th century, the whole fabric of psychiatric practice moved away from traditional stand-alone institutions that existed at the fringes of society to a more community and office-based model focused on outpatient therapy. From the 1920s, psychodynamic psychiatry, based on psychoanalysis and its versions, had an increasingly large impact on mainstream psychiatry, mainly in the United States and to a lesser degree in other Western countries, although isolated examples of biologically-oriented descriptive psychiatry, such as the Wernicke–Kleist–Leonhard school or French neuropsychiatry[44] never ceased to exist in continental Europe. As psychodynamic psychiatry focuses on the inner psychic life of the patients and not the observation of patients’ manifest behavior or motor symptoms, catatonia lost its significance in English-language psychiatry, and its signs and symptoms were glossed over in diagnostic practice.
Diagnostic practices have also undergone profound changes from the 1960s with the introduction of objective rating scales[45] and then operationalized diagnostic criteria in the 1970s[46]. The original psychopathological descriptions, including those for catatonia, were made by psychiatrists who had the opportunity to observe their patients every day in different situations over several weeks, months, or years. Many of these psychiatrists actually lived in the institutions and had fewer commitments outside of their clinical work than their modern counterparts. The democratization and decentralization of psychiatric practice, coupled with the widespread introduction of simplified cross-sectional diagnosis, as in the Diagnostic and Statistical Manual of Mental Disorders third edition[47], greatly altered the relationship between patients and psychiatrists and the diagnostic process.
In the developed world, this situation emerged starting in the 1960s with the arrival of de-institutionalization; the establishment of short-term acute psychiatric wards in general hospitals; community outpatient psychiatry evolving to brief 15-min “med checks”; and the collaborative role of allied mental health professionals providing psychiatric services, just to mention a few important factors. As a result, psychiatrists began spending less and less time in direct contact with their patients in the modern era, which may have reduced the likelihood of detecting catatonic symptoms. For instance, restructuring a regional psychiatric service in the United Kingdom resulted in psychiatrists having access to “less than 20% of the total case-load”[48].
Another aspect of contemporary psychiatric practice that may have hindered the easy detection of catatonia is exemplified by a landmark study conducted at the Institute of Psychiatry in London, one of the leading academic psychiatric centers in the world that have provided the scientific foundation to sanction diagnostic practices in the modern era[49]. In a series of diagnostic exercises, 28 psychiatrists with at least 4 years of clinical experience were asked to diagnose patients during the same 5-min diagnostic interviews based on either a video of the patients during the interview, a soundtrack recording of the interview, or only written transcripts. Surprisingly, the diagnostic accuracy measured against the final hospital discharge diagnoses was essentially identical in these three different diagnostic situations. Kendell came to the important conclusion that observing the patients’ behavior did not improve diagnostic accuracy, indicating that behavioral or motor symptoms had no, or negligible, currency in the diagnostic process although this academic center stressed the importance of behavioral symptoms and careful observations. Kendell also found that diagnostic accuracy did not increase after 4 years spent in psychiatric practice, thereby questioning the value of accumulated experience and the power of observation developed during this experience in making a diagnosis. Furthermore, based on the diagnostic accuracy of 70% reached after 5 min in each rating situation, the author suggested significantly shortening the standard 1-hour diagnostic interview. The implications of these findings on the under-recognition of catatonia are obvious.
It is well known from classical textbooks that the frequency and intensity of catatonic episodes fluctuate over time[1,5,6] and that they may not manifest at the time of cross-sectional assessment, which is how modern catatonia rating scales are conducted, resulting in a potential failure to detect the whole scope of catatonic symptomatology, particularly in chronically ill patients. For example, the Bush–Francis Catatonia Rating Scale (BFCRS)[17], the most widely used rating instrument, requires only 5–10 min to complete, although raters are encouraged to consult their medical notes covering the previous 24-h period, albeit only for the items of “withdrawal” and “autonomic abnormality.” The BFCRS has been shown to be adequate for assessing acute catatonic episodes[17], but it may not be entirely sufficient for persistent or periodic catatonia in patients with chronic illness[50], as previously suggested[51]. A study comparing the number and severity of catatonic signs and symptoms covered by the BFCRS, rated by skilled clinicians, with the “gold standard” of extended, unobtrusive observations by an experienced clinician found that the latter method yielded significantly higher ratings[52]. Signs and symptoms that were most frequently missed by cross-sectional assessment, but captured by longitudinal clinical observations were mannerisms, stereotypy, grimacing, perseveration, and apparently purposeless impulsivity[52].
Following the widespread introduction of antipsychotic drugs in psychiatric practice in the mid-1950s, it took about a decade to recognize the full spectrum and significance of drug-induced motor symptoms and syndromes referred to as extrapyramidal side effects (EPS). The importance of EPS in psychiatry may have overshadowed catatonic and other illness-related motor symptoms in clinical practice. Catatonic signs and symptoms may have been obscured by and ascribed to drug-induced EPS[15]. EPS-like motor symptoms have been consistently reported in drug-naïve patients since the 1990s, raising the possibility that, in many instances, catatonia may have been indeed misdiagnosed as EPS[53]. Even if this were not the case, the recognition of motor symptoms in drug-naïve patients helped refocus attention to catatonia.
We believe that the growing number of publications on catatonia and the number of clinicians and researchers displaying a keen interest in this subject have reached the level that warrants the establishment of an international society and a journal dedicated to the study of catatonia, to bring together interested parties, promote and coordinate research, and disseminate relevant knowledge to the broader mental health community. This may be one the avenues to further facilitate a greater understanding of catatonia, thereby improving the lives of patients with catatonia.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: European Association of Psychosomatic Medicine; European Forum for ECT; Hungarian Psychiatric Association.
Specialty type: Psychiatry
Country/Territory of origin: Hungary
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jaimes-Albornoz W, Spain; Kar SK, India; Sahoo S, India S-Editor: Li L L-Editor: A P-Editor: Zhao S
| 1. | Kraepelin E. Dementia Praecox and Paraphrenia. Edinburgh: Livingstone, 1908/1919. [DOI] [Full Text] |
| 2. | Ungvari GS, Caroff SN, Gerevich J. The catatonia conundrum: evidence of psychomotor phenomena as a symptom dimension in psychotic disorders. Schizophr Bull. 2010;36:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 89] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | Kendler KS. The development of Kraepelin's mature diagnostic concept of catatonic dementia praecox: a close reading of relevant texts. Schizophr Bull. 2020;46:471-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Hirjak D, Foucher JR, Ams M, Jeanjean LC, Kubera KM, Wolf RC, Northoff G. The origins of catatonia - Systematic review of historical texts between 1800 and 1900. Schizophr Res. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 5. | Bleuler E. Dementia Praecox or the Group of Schizophrenias. New York, NY: International Universities Press, 1950. |
| 6. | Leonhard K. Die Aufteilung der endogenen Psychosen. Berlin: Akademie Verlag, 1957. |
| 7. | Mahendra B. Where have all the catatonics gone? Psychol Med. 1981;11:669-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 66] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Guggenheim FG, Babigian HM. Diagnostic consistency in catatonic schizophrenia. Schizophr Bull. 1974;103-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Ciompi L, Müller C. [Lifestyle and age of schizophrenics. A catamnestic long-term study into old age]. Monogr Gesamtgeb Psychiatr Psychiatry Ser. 1976;12:1-242. [PubMed] |
| 10. | Leff J. Psychiatry Around the Globe: A Transcultural View. New York, NY: Marcel Dekker Inc., 1981.. |
| 11. | Achte KA. [The course of schizophrenic and schizophreni-form psychoses. A comparative study of changes in disease pictures, prognoses and the patient-physician relationship during the years 1933-1935 and 1953-1955]. Acta Psychiatr Scand Suppl. 1961;36:1-273. [PubMed] |
| 12. | Wlazło A, Kleszczyński J, Błaszczyk A, Tyfel P, Jakubczyc A, Morasiewicz J. [The frequency of diagnosis of catatonic schizophrenia in hospitals in Lubliniec (1894-1932, 1934-1936, 1970-1999) and Boleslawiec (1958-1999)]. Psychiatr Pol. 2003;37:695-701. [PubMed] |
| 13. | Silva H, Jerez S, Catenacci M, Mascaro J. [Decrease of catatonic schizophrenia in patients hospitalized in 1984 in comparison to 1964]. Acta Psiquiatr Psicol Am Lat. 1989;35:132-138. [PubMed] |
| 14. | van der Heijden FM, Tuinier S, Arts NJ, Hoogendoorn ML, Kahn RS, Verhoeven WM. Catatonia: disappeared or under-diagnosed? Psychopathology. 2005;38:3-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 108] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Stompe T, Ortwein-Swoboda G, Ritter K, Schanda H, Friedmann A. Are we witnessing the disappearance of catatonic schizophrenia? Compr Psychiatry. 2002;43:167-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Caroff SN, Mann SC, Campbell EC, Sullivan KA. Epidemiology. In: Caroff SN, Mann SC, Francis A, Fricchione GL, Editors. Catatonia. Washington DC: American Psychiatric Publishing Inc., 2004: 15-32. |
| 17. | Bush G, Fink M, Petrides G, Dowling F, Francis A. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93:129-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 588] [Cited by in RCA: 678] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 18. | Fink M, Taylor MA. Catatonia. A Clinician's Guide to Diagnosis and Treatment. Cambridge, United Kingdom: Cambridge University Press, 2003. [DOI] [Full Text] |
| 19. | Shorter E, Fink M. The Madness of Fear. A History of Catatonia. New York, NY: Oxford University Press, 2018. [DOI] [Full Text] |
| 20. | Rosebush PI, Hildebrand AM, Furlong BG, Mazurek MF. Catatonic syndrome in a general psychiatric inpatient population: frequency, clinical presentation, and response to lorazepam. J Clin Psychiatry. 1990;51:357-362. [PubMed] |
| 21. | Usman DM, Olubunmi OA, Taiwo O, Taiwo A, Rahman L, Oladipo A. Comparison of catatonia presentation in patients with schizophrenia and mood disorders in lagos, Nigeria. Iran J Psychiatry. 2011;6:7-11. [PubMed] |
| 22. | Espinola-Nadurille M, Ramirez-Bermudez J, Fricchione GL, Ojeda-Lopez MC, Perez-González AF, Aguilar-Venegas LC. Catatonia in Neurologic and Psychiatric Patients at a Tertiary Neurological Center. J Neuropsychiatry Clin Neurosci. 2016;28:124-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Oulis P, Lykouras L. Prevalence and diagnostic correlates of DSM-IV catatonic features among psychiatric inpatients. J Nerv Ment Dis. 1996;184:378-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Stuivenga M, Morrens M. Prevalence of the catatonic syndrome in an acute inpatient sample. Front Psychiatry. 2014;5:174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 25. | Wilson JE, Niu K, Nicolson SE, Levine SZ, Heckers S. The diagnostic criteria and structure of catatonia. Schizophr Res. 2015;164:256-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 97] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 26. | Starkstein SE, Petracca G, Tesón A, Chemerinski E, Merello M, Migliorelli R, Leiguarda R. Catatonia in depression: prevalence, clinical correlates, and validation of a scale. J Neurol Neurosurg Psychiatry. 1996;60:326-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 86] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Bräunig P, Krüger S, Shugar G. Prevalence and clinical significance of catatonic symptoms in mania. Compr Psychiatry. 1998;39:35-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Rogers D. The motor disorders of severe psychiatric illness: a conflict of paradigms. Br J Psychiatry. 1985;147:221-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 107] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 29. | Sienaert P, Rooseleer J, De Fruyt J. Measuring catatonia: a systematic review of rating scales. J Affect Disord. 2011;135:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 118] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 30. | Jaimes-Albornoz W, Ruiz de Pellon-Santamaria A, Nizama-Vía A, Isetta M, Albajar I, Serra-Mestres J. Catatonia in older adults: A systematic review. World J Psychiatry. 2022;12:348-367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (3)] |
| 31. | Walther S, Nadesalingam N, Nuoffer M, Kyrou A, Wüthrich F, Lefebvre S. Structural alterations of the motor cortex and higher order cortical areas suggest early neurodevelopmental origin of catatonia in schizophrenia. Schizophr Res. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 32. | Northoff G, Hirjak D. Spatiotemporal psychopathology - an integrated brain-mind approach and catatonia. Schizophr Res. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 33. | Francis A, Fink M, Appiani F, Bertelsen A, Bolwig TG, Bräunig P, Caroff SN, Carroll BT, Cavanna AE, Cohen D, Cottencin O, Cuesta MJ, Daniels J, Dhossche D, Fricchione GL, Gazdag G, Ghaziuddin N, Healy D, Klein D, Krüger S, Lee JW, Mann SC, Mazurek M, McCall WV, McDaniel WW, Northoff G, Peralta V, Petrides G, Rosebush P, Rummans TA, Shorter E, Suzuki K, Thomas P, Vaiva G, Wachtel L. Catatonia in Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. J ECT. 2010;26:246-247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 34. | American Psychiatric Association; DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders: DSM-5™. 5th ed. Washington, DC: American Psychiatric Publishing, Inc., 2013. [RCA] [DOI] [Full Text] [Cited by in Crossref: 66101] [Cited by in RCA: 58201] [Article Influence: 3637.6] [Reference Citation Analysis (4)] |
| 35. | World Health Organization. International Classification of Diseases 11th Revision. [cited 3 April 2023]. Available from: https://icd.who.int/en. |
| 36. | Kleist K. Schizophrenic symptoms and cerebral pathology. J Ment Sci. 1960;106:246-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 37. | World Health Organization. Report of the International Pilot Study of Schizophrenia. WHO: Geneva, 1973:1. [cited 3 April 2023]. Available from: https://apps.who.int/iris/bitstream/handle/10665/39405/WHO_OFFSET_2_%28chp1-chp8%29.pdf?sequence=1&isAllowed=y. |
| 38. | Chandrasena R. Catatonic schizophrenia: an international comparative study. Can J Psychiatry. 1986;31:249-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 39. | Chalasani P, Healy D, Morriss R. Presentation and frequency of catatonia in new admissions to two acute psychiatric admission units in India and Wales. Psychol Med. 2005;35:1667-1675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 40. | Dutt A, Grover S, Chakrabarti S, Avasthi A, Kumar S. Phenomenology and treatment of Catatonia: A descriptive study from north India. Indian J Psychiatry. 2011;53:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 41. | Sarkar S, Sakey S, Mathan K, Bharadwaj B, Kattimani S, Rajkumar RP. Assessing catatonia using four different instruments: Inter-rater reliability and prevalence in inpatient clinical population. Asian J Psychiatr. 2016;23:27-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Subramaniyam BA, Muliyala KP, Hari Hara S, Kumar Reddi VS. Prevalence of catatonic signs and symptoms in an acute psychiatric unit from a tertiary psychiatric center in India. Asian J Psychiatr. 2019;44:13-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Banerjee A, Sharma LN. Catatonia incidence in acute psychiatric admissions. Indian J Psychiatry. 1995;37:35-39. [PubMed] |
| 44. | Baruk H. Pathogenie du syndrome catatonique et catatonie experimentale. Paris, France: Gaston Doin, 1932. |
| 45. | Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21041] [Cited by in RCA: 22863] [Article Influence: 351.7] [Reference Citation Analysis (0)] |
| 46. | Feighner JP, Robins E, Guze SB, Woodruff RA Jr, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry. 1972;26:57-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3829] [Cited by in RCA: 3009] [Article Influence: 56.8] [Reference Citation Analysis (0)] |
| 47. | American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 3rd Ed. Washington, DC. 1980. |
| 48. | Freeman H. Evaluation in mental health care. Br J Psychiatry. 1992;161:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 49. | Kendell RE. Psychiatric diagnoses: a study of how they are made. Br J Psychiatry. 1973;122:437-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 49] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 50. | Wong E, Ungvari GS, Leung SK, Tang WK. Rating catatonia in patients with chronic schizophrenia: Rasch analysis of the Bush-Francis Catatonia Rating Scale. Int J Methods Psychiatr Res. 2007;16:161-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 51. | Bush G, Petrides G, Francis A. Catatonia and other motor syndromes in a chronically hospitalized psychiatric population. Schizophr Res. 1997;27:83-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 52. | Ungvari GS, Chow LY, Leung HCM, Lau BST. Rating chronic catatonia: discrepancy between cross-sectional and longitudinal assessment. Rev Psiquiatr Clín. 26:56-61. |
| 53. | Solmi M, Pigato GG, Roiter B, Guaglianone A, Martini L, Fornaro M, Monaco F, Carvalho AF, Stubbs B, Veronese N, Correll CU. Prevalence of Catatonia and Its Moderators in Clinical Samples: Results from a Meta-analysis and Meta-regression Analysis. Schizophr Bull. 2018;44:1133-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 111] [Article Influence: 15.9] [Reference Citation Analysis (0)] |