Published online Apr 19, 2020. doi: 10.5498/wjp.v10.i4.59
Peer-review started: November 4, 2019
First decision: December 26, 2019
Revised: February 26, 2020
Accepted: March 12, 2020
Article in press: March 12, 2020
Published online: April 19, 2020
Processing time: 164 Days and 19.5 Hours
The prevalence of depression in patients with chronic obstructive pulmonary disease (COPD) ranges from 10% to 42%, but the diagnosis of depression in patients with COPD is often unrecognized and untreated. Unrecognized depression has major implications for compliance with medical treatment, prolonged lengths of stay, increased frequency of hospital admissions, and increased consultations with primary care physicians. Many studies have attempted to identify risk factors for progression, prognosis and response to therapy in patients with depression. However, few studies have examined the risk factors for depression in patients with COPD, and some results remain controversial.
To identify the potential risk factors to define patients with COPD who are at “high risk” of depression.
The clinical data of 293 patients with COPD were reviewed from January 2017 to December 2018. The correlations between demographics, clinical characteristics and depression were analyzed. The risk factors for depression in patients with COPD were identified by multivariate logistic regression analysis. The cutoff value, sensitivity and specificity of the independent correlation factors were calculated with a receiver operating characteristic curve.
Of the 293 patients included, 65 (22.18%) individuals were identified to have depression. Significant differences were detected between patients with and without depression in terms of body mass index (BMI), forced expiratory volume in 1 s (FEV1), and COPD assessment test (CAT) score (all P < 0.05). Low BMI, low FEV1, and high CAT were independent risk factors for depression in patients with COPD and the cutoff values of BMI, FEV1, and CAT scores were 21.373 kg/m2, 0.855 L and 12.5, respectively.
Low BMI, low FEV1, and high CAT score were identified as independent risk factors for depression in patients with COPD.
Core tip: The prevalence of depression in patients with chronic obstructive pulmonary disease (COPD) ranges from 10% to 42%. However, the risk factors for depression in patients with COPD have been examined in few studies, and some results remain controversial. The purpose of the current study is to investigate the correlation between clinical parameters and the symptoms of depression, and to identify independent risk factors to define patients with COPD who are at “high risk” of depression. Low body mass index, low forced expiratory volume in 1 s and high chronic obstructive pulmonary disease assessment test score were identified as independent risk factors for depression in patients with COPD.
- Citation: Yao HM, Xiao RS, Cao PL, Wang XL, Zuo W, Zhang W. Risk factors for depression in patients with chronic obstructive pulmonary disease. World J Psychiatr 2020; 10(4): 59-70
- URL: https://www.wjgnet.com/2220-3206/full/v10/i4/59.htm
- DOI: https://dx.doi.org/10.5498/wjp.v10.i4.59
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity with an economic and social burden that is both substantial and increasing[1,2]. COPD is currently the fourth-leading cause of death and is expected to surpass stroke within the next decade to become the third leading cause of death[3]. Because medical treatments have made limited inroads, patients with COPD experience recurring acute exacerbations, frequent hospital admissions, poor survival, and impaired physical functioning and quality of life[4-6]. The reported prevalence of depression in patients with COPD ranges from 10% to 42%, a proportion much higher than that in the general population[7,8]. Although evidence suggests that certain interventions such as antidepressants, pulmonary rehabilitation, and counseling may improve health outcomes, the diagnosis of depression in patients with COPD is often unrecognized and untreated in primary and specialty care[9,10]. Unrecognized depression has major implications for compliance with medical treatment, prolonged lengths of stay, increased frequency of hospital admissions, and increased consultations with primary care physicians, all of which could decrease quality of life in patients[11,12]. The Hospital Anxiety and Depression Rating Scale (HADS) is one of the most commonly used instruments for depression in the literature[13]. The HADS is subjective and is intended for anxiety and depression screening of patients in general hospitals. It is a 14-item self-report questionnaire comprising two subscales: HADS-anxiety subscale (HADS-A) and HADS-depression subscale (HADS-D), which are scored from 0 to 21 to detect the presence of symptoms of anxiety and depression. The scale is designed for use in patients with physical illness; therefore, none of the items include somatic symptoms of depression or anxiety. Although the screening tool is widely available, it cannot provide enough information for early diagnosis.
Many studies have attempted to identify risk factors for progression, prognosis and response to therapy in patients with depression[10,14]. However, few studies have examined the risk factors for depression in patients with COPD, and some results remain controversial[14]. Thus, further research is needed to detect depression in patients with COPD for early diagnosis and treatment. The purpose of the current study is to investigate the correlation between clinical parameters and the symptoms of depression, and to identify independent risk factors to define patients with COPD at “high risk” of depression.
This was a retrospective study with no involvement in clinical or animal research. The requirement for ethical permission was waived according to the statements regarding the application of ethical permission by the Ethical Committee of the First Affiliated Hospital of Nanchang University. A retrospective study was conducted and a series of consecutive patients newly diagnosed with COPD between January 2017 and December 2018 were included in this study. COPD diagnosis was made according to the Global Initiative for Chronic Obstructive Lung Disease[15]. We studied the files of the patients carefully to ensure that all factors that might affect the outcome of the assessment were considered when the patients were included in this study. Standard treatment was given to each patient. The diagnosis of depression mainly relied on the HADS-D, and the HADS scale was carried out by an experienced psychiatrist when the patients were stable. A review and meta-analysis of studies reported that a cutoff of 8 or more on the HADS-D produced a sensitivity of 0.82 (95%CI: 0.73–80) and a specificity of 0.74 (95%CI: 0.60–0.84) for depressive disorders[16]. Therefore, we used a cutoff of 8 or more on the HADS-D to dichotomize the HADS-D scores for the purposes of the regression analyses. All the patients were inpatients and were recruited from medical hospital wards.
Patients presenting with confounders of comorbidity or other conditions that could potentially affect the evaluation of risk factors, such as dependent care living situations, life expectancy of less than six months, trouble with eye-sight, and diagnosis of dementia or Alzheimer's disease, were excluded from this study. For patients already diagnosed with depressive disorder or history of such disorder, only those with depression associated with COPD were included in this study and the judgments were made by an experienced psychiatrist. Patients receiving antidepressants, anxiolytics or other psychiatric medication were excluded in order to avoid introducing bias as treatment options might have a potential impact on HADS scores.
The demographics and clinical characteristics of the patients in this retrospective study included age, gender, marital status, household income, smoking status, duration of respiratory symptoms, number of acute exacerbations in the previous year, body mass index (BMI, kg/m2), forced expiratory volume in 1 s (FEV1, L), and Modified British Medical Research Council Questionnaire (mMRC) and Chronic Obstructive Pulmonary Disease assessment test (CAT) scores at the time of the primary diagnosis of COPD. The correlation between clinical parameters and depression was analyzed, and the risk factors for depression in patients with COPD were identified.
All analyses were performed using IBM SPSS Version 22 (SPSS Inc. Chicago IL, USA). Qualitative variables were expressed as numbers and percentages, and were assessed by the χ2 test or Fisher’s exact test. Continuous variables were reported as the mean ± SD and were compared with independent samples t-tests or univariate analysis. Independent risk factors related to depression were analyzed using a multivariate logistic regression analysis model. A receiver operating characteristic (ROC) curve was used to assess the predictive value of risk factors in patients with depression. Statistical significance was set as a P value less than 0.05.
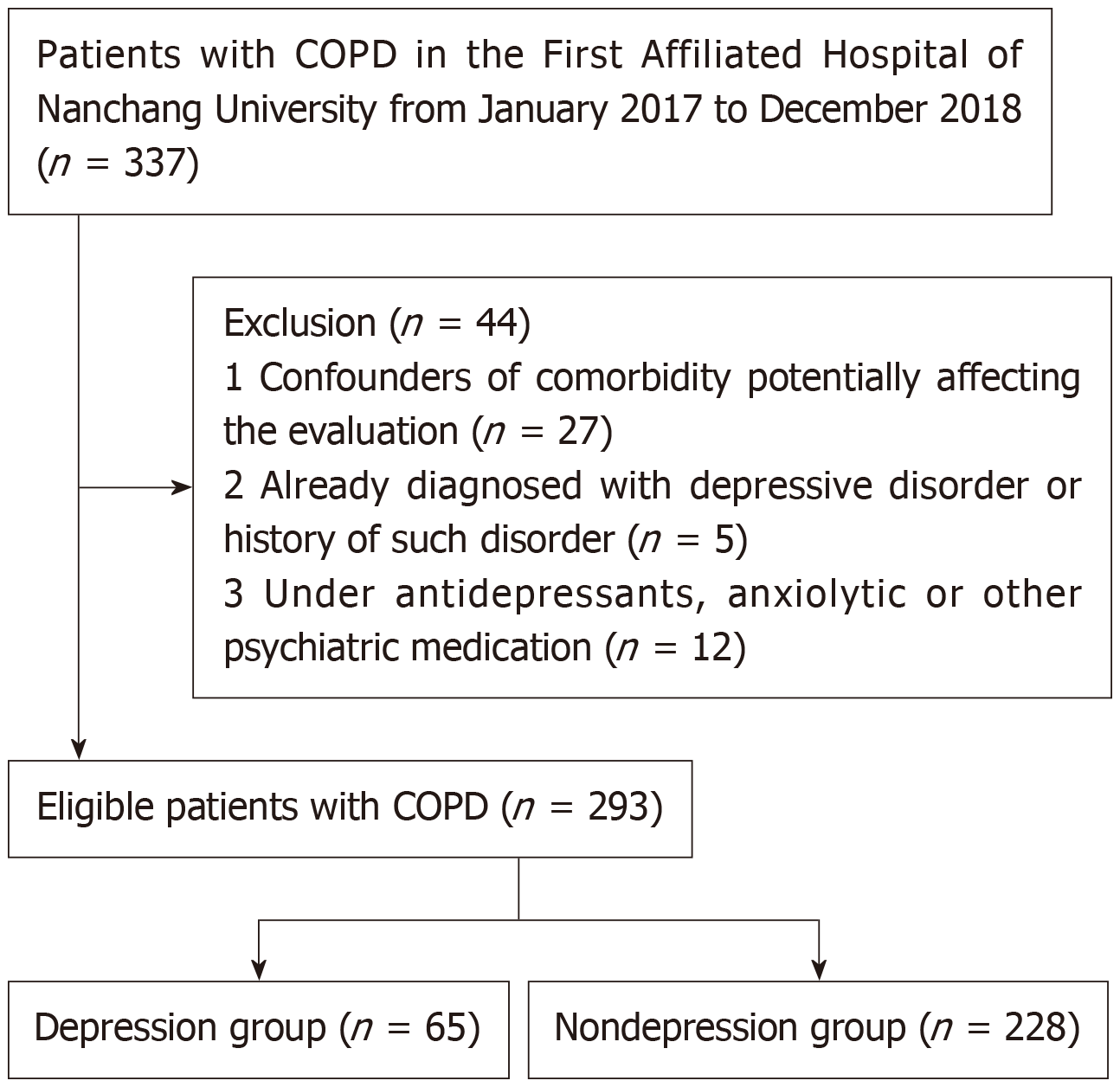
A total of 293 patients with COPD were included in this study (Figure 1). Patients’ demographics are shown in Table 1. Of the 293 patients who were eligible for inclusion, 65 individuals were identified to have depression. The overall incidence of depression in this study was 22.18% (65/293). Most of the patients were male (240 patients, 81.91%), with an average age of 65.62 ± 7.31 years. Among these patients, 38.91% were past smokers, and 33.79% were current smokers. The household income type of most patients was low income (149 patients, 50.85%) or medium income (105 patients, 35.84%).
| Patient characteristics | Number of patients |
| Age at diagnosis (mean ± SD, yr) | 65.62 ± 7.31 |
| Gender | |
| Female | 53 (18.09) |
| Male | 240 (81.91) |
| Smoking history | |
| Never smoker | 80 (27.30) |
| Past smoker | 114 (38.91) |
| Current smoker | 99 (33.79) |
| Household income | |
| Low income | 149 (50.85) |
| Medium income | 105 (35.84) |
| High income | 39 (13.31) |
| Patients with depression | 65 (22.18) |
| HADS-D score | 5.09 ± 2.73 |
The differences between clinical parameters and depression were investigated and the results are presented in Table 2. The results revealed that depression in patients with COPD was associated with the duration of respiratory symptoms, the number of exacerbations per year, BMI, FEV1, and the mMRC dyspnea scale and CAT scores as significant differences were found between patients with and without depression for these factors (all P < 0.05). These results indicated that the duration of respiratory symptoms, the number of exacerbations per year, BMI, FEV1, and the mMRC dyspnea scale and CAT scores were potentially related to depression in patients with COPD. No statistically significant differences in age, gender, marital status, household income and smoking history were observed between the 2 groups (P > 0.05).
| Factors | Depression | No depression | P value |
| Age at diagnosis (mean ± SD, yr) | 65.12 ± 7.62 | 65.76 ± 7.23 | NS |
| Gender | 65 | 228 | NS |
| Female | 9 | 44 | |
| Male | 56 | 184 | |
| Marital status | 65 | 228 | NS |
| Married or partner | 52 | 194 | |
| Single, divorced, separated or widowed | 13 | 34 | |
| Household income | 65 | 228 | NS |
| High income | 12 | 27 | |
| Medium income | 20 | 82 | |
| Low income | 33 | 119 | |
| Smoking history | 65 | 228 | NS |
| Never smoker | 15 | 49 | |
| Past smoker | 24 | 96 | |
| Current smoker | 26 | 83 | |
| Duration of respiratory symptoms (mo) | 111.28 ± 41.92 | 79.51 ± 112.47 | 0.026 |
| Exacerbation rate (prior yr) | 2.09 ± 1.28 | 1.58 ± 0.94 | 0.004 |
| BMI (kg/m2) | 18.51 ± 3.34 | 20.75 ± 4.09 | 0.000 |
| FEV1 (L) | 0.82 ± 0.30 | 1.11 ± 0.44 | 0.000 |
| mMRC dyspnea scale | 1.86 ± 0.75 | 1.67 ± 0.69 | NS |
| CAT score | 13.08 ± 3.71 | 10.30 ± 4.20 | 0.002 |
| HADS score | 9.18 ± 1.27 | 3.93 ± 1.72 | 0.000 |
Multivariate logistic regression analysis was carried out to identify the potential risk factors for depression in patients with COPD. Low BMI (OR = 0.893, P < 0.05), low FEV1 (OR = 0.325, P < 0.05), and high CAT score (OR = 1.111, P < 0.05) were independent risk factors for depression. No significant differences were found for the duration of respiratory symptoms or the number of exacerbations per year between COPD patients with and without depression (P > 0.05) (Table 3).
| Factors | β | OR | 95%CI | P value |
| Duration of respiratory symptoms | 0.002 | 1.002 | 0.999-1.004 | NS |
| Exacerbation rate (prior yr) | 0.13 | 1.139 | 0.854-1.518 | NS |
| BMI (kg/m2) | -0.113 | 0.893 | 0.830-0.962 | 0.003 |
| FEV1 (L) | -1.124 | 0.325 | 0.132-0.803 | 0.002 |
| CAT score | 0.105 | 1.111 | 1.021-1.209 | 0.004 |
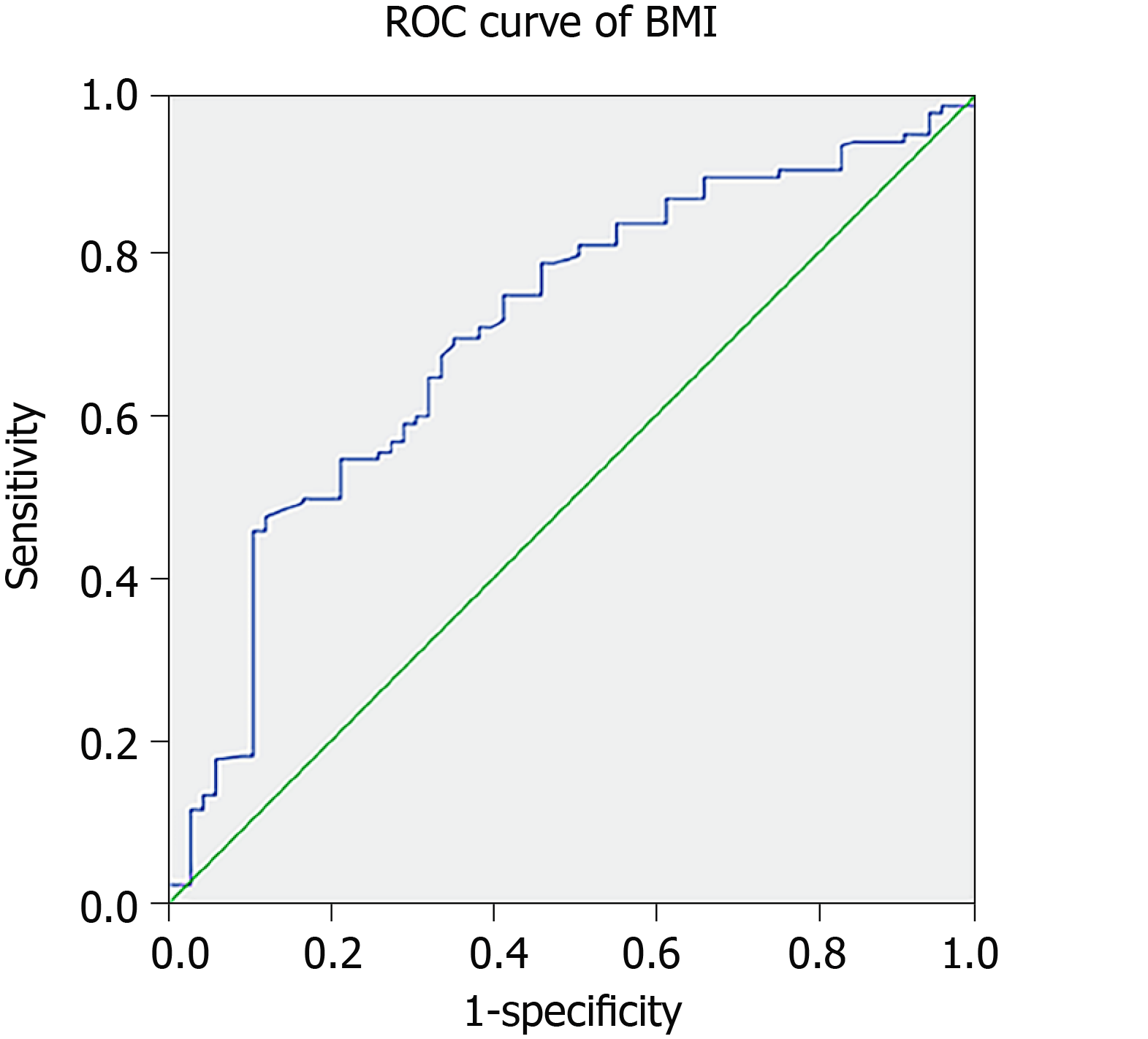
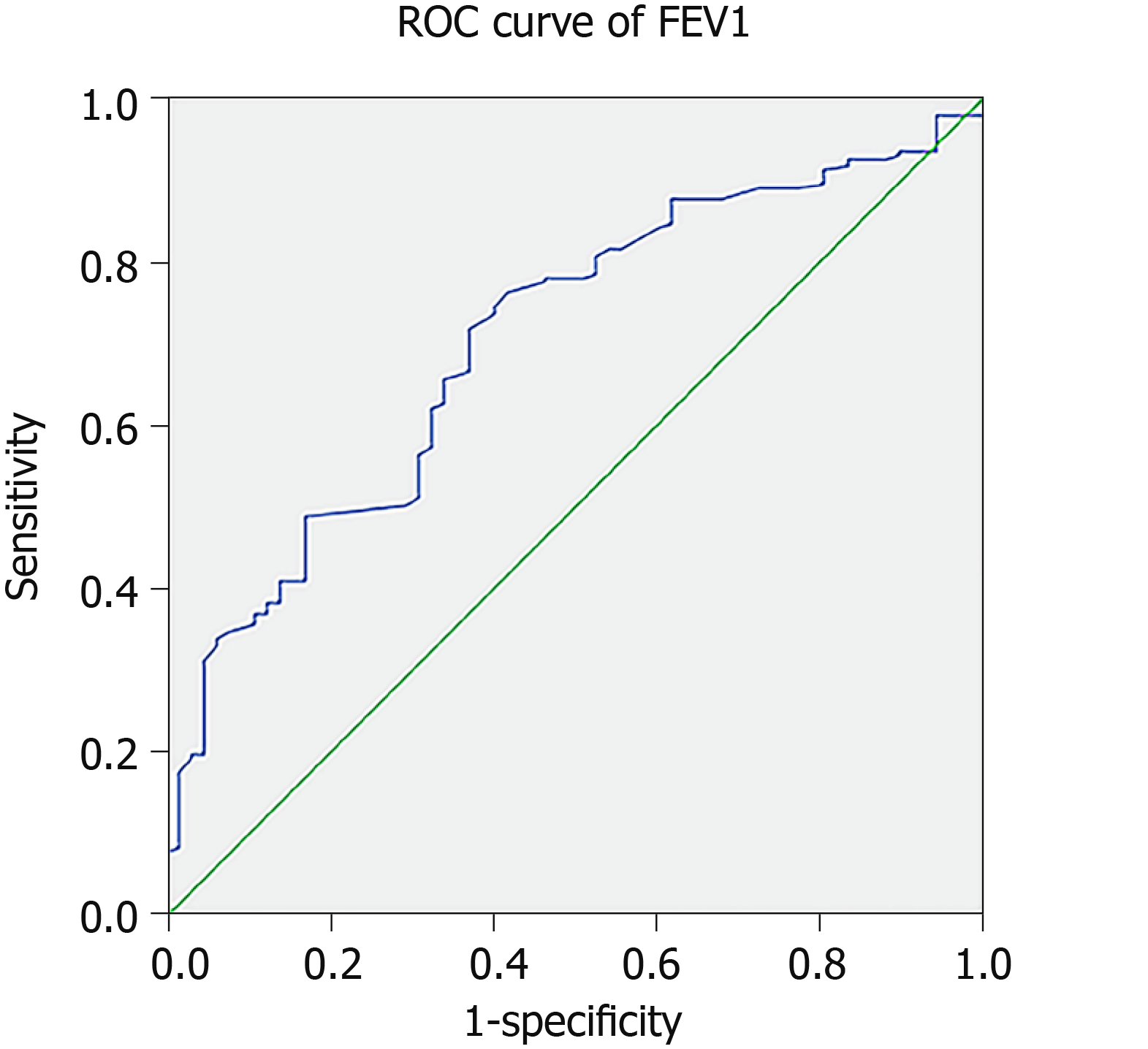
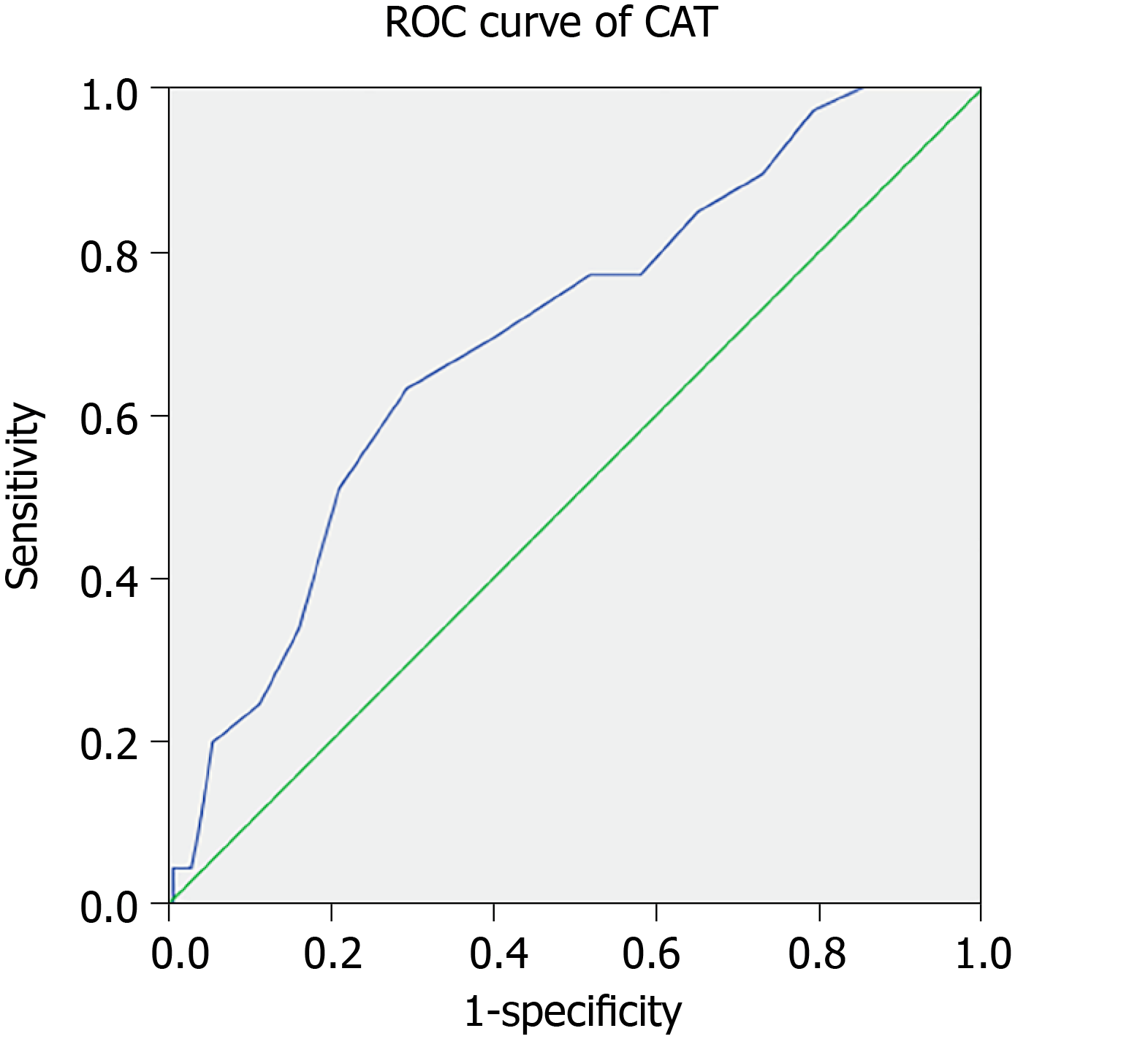
Figure 2, Figure 3 and Figure 4 show the ROC curves of BMI, FEV1, and CAT score for predicting the risk of depression; these factors had comparable accuracy in predicting depression in COPD patients (the AUC of these factors were 0.705, 0.702 and 0.694, respectively). The cutoff values of these factors were 21.375 kg/m2, 0.855 L and 12.5, respectively. BMI had the highest diagnostic accuracy for predicting the risk of depression (AUC = 0.705, P < 0.05), with a sensitivity and specificity of 49.6% and 83.1%, respectively. Additionally, combined BMI and FEV1 with CAT score had a higher AUC (BMI + FEV1: 74.5%; BMI + CAT: 73.5%; FEV1 + CAT: 73.0%; BMI + FEV1 + CAT: 76.6%) than that of one single factor (Table 4).
| Factors | Cutoff value | Sensitivity (%) | Specificity (%) | AUC | 95%CI | P value |
| BMI (kg/m2) | 21.375 | 49.6 | 83.1 | 0.705 | 0.633-0.776 | 0.001 |
| FEV1 (L) | 0.855 | 71.5 | 63.1 | 0.702 | 0.634-0.770 | 0.003 |
| CAT score | 12.5 | 63.1 | 70.6 | 0.694 | 0.624-0.765 | 0.001 |
| BMI+FEV1 | 76.9 | 66.7 | 0.745 | 0.684-0.807 | 0.000 | |
| BMI+CAT | 72.3 | 67.1 | 0.735 | 0.669-0.802 | 0.000 | |
| FEV1+CAT | 76.9 | 60.5 | 0.730 | 0.667-0.794 | 0.000 | |
| BMI+FEV1+CAT | 72.3 | 75.0 | 0.766 | 0.705-0.827 | 0.000 |
COPD is a major respiratory noncommunicable disease and is currently the third leading cause of death worldwide[17]. Depression occurs in up to 42% of persons with COPD[11], almost twice as often as in those without COPD[18]. In line with previous studies, the incidence of depression in our study was 22.18%, based on a population of 293 patients. Depression in patients with COPD is associated with physical impairment[19], readmission[20], increased dyspnea[21,22], and mortality[23]. Due to the considerable overlap between the physical symptoms of depression and the symptoms of COPD, patients with COPD may not be able to recognize this mental illness, and diagnosis is easily missed by doctors compared with that in patients with other comorbidities or depression alone[24]. Due to these factors, depression may reduce patient compliance with COPD treatment, thus leading to deterioration related to COPD. Therefore, identifying valuable predictive factors that are readily available could meaningfully benefit timely intervention to cure depression. In this retrospective study, we evaluated the association between clinical factors and depression in patients with COPD. Previous studies reported that depression in patients with COPD was associated with multiple factors, including age, gender, marital status, smoking history and social performance[25-27]. However, in this study, a correlation between the above-mentioned factors and depression was not found. The reason for this result may be that these studies were performed primarily in patients with severe COPD, and few of them focused on risk factors in patients with mild COPD.
BMI had been widely used to measure obesity, and there is growing evidence that BMI is an independent predictor of mental disorders[28]. A previous study reported that the average depression score in an obesity group was higher than that in a normal BMI group[28]. Zhao et al[29] revealed that obese individuals (≥ 25.0 kg/m2) were 38% more likely to experience depression, and were 40% more likely to have lifetime depression after fully adjusting for several factors, such as obesity-related comorbidities, demographics, and psychosocial factors. Lee et al[30] indicated that adjusted odds ratios for depression formed a U-shaped relationship with BMI categories (underweight group: 1.31, overweight group: 0.94, obese group: 1.01, severely obese group: 1.28). The BMI level with the lowest likelihood of depression was 18.5-25 kg/m2 in women and 23-25 kg/m2 in men[30]. However, few studies have analyzed the relationship between BMI and depression in patients with COPD. In the current study, we identified BMI as an independent risk factor correlated with depression. The cutoff value was 21.375 kg/m2. This finding suggested that BMI levels < 21.375 kg/m2 could help to distinguish populations of patients with COPD at a higher risk of depression.
Previous data highlighted the association between FEV1 and depression. A study reported that among 100 dairy farmers with COPD, as defined by a postbronchodilator FEV1/forced vital capacity ratio < 0.7, depression in patients was associated with lower FEV1, as well as with certain COPD-related characteristics (current smoking, dyspnea severity, and poorer quality of life)[31]. Von Siemens et al[32] demonstrated that FEV1 was significantly (P < 0.05) related to the Patient Health Questionnaire 9 score, which is one of the screening tools for depression. Significant differences were found for FEV1 levels, reflecting COPD severity, between patients with and without depression[33]. This result could help patients with depression avoid being untreated or undertreated[34]. Consistent with previous studies, our study indicated that FEV1 was an independent risk factor for depression in patients with COPD. The cut-off value was 0.855 L, and the sensitivity and specificity were 71.5% and 63.1%, respectively.
The CAT score was developed in 2009 as a patient-administered, short questionnaire to test health-related quality of life in patients with COPD[35]. Lower scores indicated less severe symptoms. There was a significant difference in CAT scores between patients with depression and without depression[35]. The analyses by von Siemens et al[32] revealed, with a cut-off CAT score of 20, an AUC of 0.81. Based on the close relationship between the tests, the CAT score and depression were also omitted from further analysis. Interestingly, this value was similar to the critical value of 18, which had been proposed to be better than the conventional threshold of 10 in terms of the classification of COPD severity. Lee et al[36] indicated that the CAT score and symptoms were correlated with the formation of depression in patients with COPD. In line with previous studies, the results of our study showed significant differences in CAT scores between patients with and without depression, and we identified that the CAT score was an independent risk factor correlated with depression. The cutoff value was 12.5. This finding indicated that a CAT score > 12.5 was a risk factor for depression in patients with COPD.
To identify the predictive accuracy of combined risk factors for predicting depression in patients with COPD, we analyzed the combined risk factors for depression in the present study. Compared to BMI, FEV1 or CAT score alone, we found that combining FEV1 and CAT score with BMI had higher predictive value for predicting depression in patients with COPD. This finding indicated that the combination of risk factors appeared to be more useful for predicting depression.
To our knowledge, we have been successful in identifying low BMI, low FEV1 and high CAT score as independent depression associated risk factors in patients with COPD. Although the results are interesting, limitations to our study still exist. First, this was a retrospective study with a relatively small sample, which may have resulted in bias during analysis of the results. Second, we only collected variables from patients with COPD at the time of diagnosis, and some variables, such as the time to depression and follow up, were not reported. Third, patient variables were from a single medical institution and the results of our study for predicting depression were not satisfactory. Thus, a multicenter study with more patients is needed to verify our results. Fourth, some studies indicated that the HADS was saturated by the presence of a common distressing factor, in part because it was intended to focus on lack of pleasure and autonomous arousal, leading to the difficulty in distinguishing depression from anxiety. This explained the result that the HADS anxiety scale and depression scale served the same purpose as a screening tool for depression[37]. For research purposes, the use of a summed HADS total score was recommended and appeared to provide an adequate estimate. In clinical practice, HADS is not recommended when it is necessary to distinguish between anxiety and depression. Due to its poor trait coverage and narrow focus, short tools covering broad anxiety and depression symptoms may be more appropriate[38,39]. COPD patients have greater disease burden than other populations. In addition to the widespread symptoms of depression, our results also identified several risk factors for depression including low BMI, low FEV1, and high CAT score. However, barriers to recognition exist at the provider and system levels. At the provider level, lack of ambitions and stereotypes can be obstacles. At the system level, poor integration of mental health services with primary health care is another obstacle.
In conclusion, based on this analysis, we established that approximately one-fifth of patients with COPD developed depression. Additionally, we identified low BMI, low FEV1, and high CAT score as risk factors for depression in COPD patients. Combining these factors predicted the highest risk of developing depression. However, a prospective study with a large sample size and multicenter analysis is needed to prove the conclusions of our study.
The reported prevalence of depression in patients with chronic obstructive pulmonary disease (COPD) ranges from 10% to 42%, a proportion much higher than that in the general population. Certain interventions such as antidepressants, pulmonary rehabilitation, and counseling may improve health outcomes, but the diagnosis of depression in patients with COPD is often unrecognized and untreated in primary and specialty care. Unrecognized depression has major implications for compliance with medical treatment, prolonged lengths of stay, increased frequency of hospital admissions, and increased consultations with primary care physicians, all of which could decrease quality of life in patients.
Many studies have attempted to identify risk factors for progression, prognosis and response to therapy in patients with depression. However, few studies have examined the risk factors for depression in patients with COPD, and some results remain controversial.
The main objective of the current study is to investigate the correlation between clinical parameters and the symptoms of depression, and to identify independent risk factors to define patients with COPD at “high risk” of depression.
The Hospital Anxiety and Depression Rating Scale (HADS) is one of the most commonly used instruments for depression in the literature. A series of consecutive patients newly diagnosed with COPD were included in this study. The diagnosis of depression mainly relied on the HADS, and the HADS scale was carried out by an experienced psychiatrist when the patients were stable. We used a cutoff of 8 or more on the HADS to dichotomize the HADS scores for the purposes of the regression analyses. The correlation between clinical parameters and depression was analyzed, and the risk factors for depression in patients with COPD were identified.
Multivariate logistic regression analysis was carried out to identify the potential risk factors for depression in patients with COPD. Low body mass index (BMI), low forced expiratory volume in 1 s (FEV1), and high COPD assessment test (CAT) score were independent risk factors for depression. BMI had the highest diagnostic accuracy for predicting the risk of depression. Additionally, combined BMI and FEV1 with CAT score had a higher area under curve than that of one single factor.
Approximately one-fifth of patients with COPD developed depression. Additionally, we identified low BMI, low FEV1, and high CAT score as risk factors for depression in COPD patients. Combining these factors predicted the highest risk of developing depression.
Some variables, such as the time to depression and follow up, were not reported, which may have resulted in bias during analysis of the results. A prospective study with a large sample size and multicenter analysis is needed to prove the conclusions of our study.
Manuscript source: Unsolicited Manuscript
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Kotzalidis GD, Tung TH, Hosak L, Barik R, Dimopoulos N S-Editor: Wang YQ L-Editor: Webster JR E-Editor: Liu MY
| 1. | Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O'Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095-2128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9500] [Cited by in RCA: 9579] [Article Influence: 736.8] [Reference Citation Analysis (0)] |
| 2. | Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fèvre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gosselin R, Grainger R, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Ma J, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O'Donnell M, O'Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leòn FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163-2196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5305] [Cited by in RCA: 5774] [Article Influence: 444.2] [Reference Citation Analysis (0)] |
| 3. | Jemal A, Ward E, Hao Y, Thun M. Trends in the leading causes of death in the United States, 1970-2002. JAMA. 2005;294:1255-1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 666] [Cited by in RCA: 650] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 4. | Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. 2002;121:121S-126S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 373] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 5. | Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157:1418-1422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1292] [Cited by in RCA: 1485] [Article Influence: 55.0] [Reference Citation Analysis (0)] |
| 6. | Connors AF Jr, Dawson NV, Thomas C, Harrell FE, Desbiens N, Fulkerson WJ, Kussin P, Bellamy P, Goldman L, Knaus WA. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments). Am J Respir Crit Care Med. 1996;154:959-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 868] [Cited by in RCA: 912] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 7. | Dowson C, Laing R, Barraclough R, Town I, Mulder R, Norris K, Drennan C. The use of the Hospital Anxiety and Depression Scale (HADS) in patients with chronic obstructive pulmonary disease: a pilot study. N Z Med J. 2001;114:447-449. [PubMed] |
| 8. | Yohannes AM, Baldwin RC, Connolly MJ. Prevalence of sub-threshold depression in elderly patients with chronic obstructive pulmonary disease. Int J Geriatr Psychiatry. 2003;18:412-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 66] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Peveler R, Carson A, Rodin G. Depression in medical patients. BMJ. 2002;325:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 96] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Maurer J, Rebbapragada V, Borson S, Goldstein R, Kunik ME, Yohannes AM, Hanania NA, ACCP Workshop Panel on Anxiety and Depression in COPD. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008;134:43S-56S. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 528] [Cited by in RCA: 485] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 11. | Kunik ME, Roundy K, Veazey C, Souchek J, Richardson P, Wray NP, Stanley MA. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127:1205-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 268] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 12. | Jones PW, Baveystock CM, Littlejohns P. Relationships between general health measured with the sickness impact profile and respiratory symptoms, physiological measures, and mood in patients with chronic airflow limitation. Am Rev Respir Dis. 1989;140:1538-1543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 136] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Bock K, Bendstrup E, Hilberg O, Løkke A. Screening tools for evaluation of depression in Chronic Obstructive Pulmonary Disease (COPD). A systematic review. Eur Clin Respir J. 2017;4:1332931. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Xu W, Collet JP, Shapiro S, Lin Y, Yang T, Platt RW, Wang C, Bourbeau J. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med. 2008;178:913-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 230] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 15. | Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ, Nishimura M, Stockley RA, Sin DD, Rodriguez-Roisin R. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3156] [Cited by in RCA: 3721] [Article Influence: 310.1] [Reference Citation Analysis (0)] |
| 16. | Brennan C, Worrall-Davies A, McMillan D, Gilbody S, House A. The Hospital Anxiety and Depression Scale: a diagnostic meta-analysis of case-finding ability. J Psychosom Res. 2010;69:371-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 265] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 17. | Bousquet J, Anto JM, Sterk PJ, Adcock IM, Chung KF, Roca J, Agusti A, Brightling C, Cambon-Thomsen A, Cesario A, Abdelhak S, Antonarakis SE, Avignon A, Ballabio A, Baraldi E, Baranov A, Bieber T, Bockaert J, Brahmachari S, Brambilla C, Bringer J, Dauzat M, Ernberg I, Fabbri L, Froguel P, Galas D, Gojobori T, Hunter P, Jorgensen C, Kauffmann F, Kourilsky P, Kowalski ML, Lancet D, Pen CL, Mallet J, Mayosi B, Mercier J, Metspalu A, Nadeau JH, Ninot G, Noble D, Oztürk M, Palkonen S, Préfaut C, Rabe K, Renard E, Roberts RG, Samolinski B, Schünemann HJ, Simon HU, Soares MB, Superti-Furga G, Tegner J, Verjovski-Almeida S, Wellstead P, Wolkenhauer O, Wouters E, Balling R, Brookes AJ, Charron D, Pison C, Chen Z, Hood L, Auffray C. Systems medicine and integrated care to combat chronic noncommunicable diseases. Genome Med. 2011;3:43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 134] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 18. | Liu H, Song M, Zhai ZH, Shi RJ, Zhou XL. Group singing improves depression and life quality in patients with stable COPD: a randomized community-based trial in China. Qual Life Res. 2019;28:725-735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Hu J, Meek P. Health-related quality of life in individuals with chronic obstructive pulmonary disease. Heart Lung. 2005;34:415-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Osman IM, Godden DJ, Friend JA, Legge JS, Douglas JG. Quality of life and hospital re-admission in patients with chronic obstructive pulmonary disease. Thorax. 1997;52:67-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 218] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 21. | Carrasco Garrido P, de Miguel Díez J, Rejas Gutiérrez J, Centeno AM, Gobartt Vázquez E, Gil de Miguel A, García Carballo M, Jiménez García R. Negative impact of chronic obstructive pulmonary disease on the health-related quality of life of patients. Results of the EPIDEPOC study. Health Qual Life Outcomes. 2006;4:31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 115] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 22. | Hajiro T, Nishimura K, Tsukino M, Ikeda A, Oga T, Izumi T. A comparison of the level of dyspnea vs disease severity in indicating the health-related quality of life of patients with COPD. Chest. 1999;116:1632-1637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 144] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 23. | Domingo-Salvany A, Lamarca R, Ferrer M, Garcia-Aymerich J, Alonso J, Félez M, Khalaf A, Marrades RM, Monsó E, Serra-Batlles J, Antó JM. Health-related quality of life and mortality in male patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166:680-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 269] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 24. | Stage KB, Middelboe T, Stage TB, Sørensen CH. Depression in COPD--management and quality of life considerations. Int J Chron Obstruct Pulmon Dis. 2006;1:315-320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Cleland JA, Lee AJ, Hall S. Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Fam Pract. 2007;24:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 26. | Gudmundsson G, Gislason T, Janson C, Lindberg E, Suppli Ulrik C, Brøndum E, Nieminen MM, Aine T, Hallin R, Bakke P. Depression, anxiety and health status after hospitalisation for COPD: a multicentre study in the Nordic countries. Respir Med. 2006;100:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 152] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 27. | Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007;167:60-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 419] [Cited by in RCA: 454] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 28. | Lee HS, Park E. Association of serum ferritin level and depression with respect to the body mass index in Korean male adults. Nutr Res Pract. 2019;13:263-267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Zhao G, Ford ES, Dhingra S, Li C, Strine TW, Mokdad AH. Depression and anxiety among US adults: associations with body mass index. Int J Obes (Lond). 2009;33:257-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 272] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 30. | Lee JH, Park SK, Ryoo JH, Oh CM, Choi JM, McIntyre RS, Mansur RB, Kim H, Hales S, Jung JY. U-shaped relationship between depression and body mass index in the Korean adults. Eur Psychiatry. 2017;45:72-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 31. | Guillien A, Laurent L, Soumagne T, Puyraveau M, Laplante JJ, Andujar P, Annesi-Maesano I, Roche N, Degano B, Dalphin JC. Anxiety and depression among dairy farmers: the impact of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 32. | von Siemens SM, Jörres RA, Behr J, Alter P, Lutter J, Lucke T, Söhler S, Welte T, Watz H, Vogelmeier CF, Trudzinski F, Rief W, Herbig B, Kahnert K; COSYCONET study group. Effect of COPD severity and comorbidities on the result of the PHQ-9 tool for the diagnosis of depression: results from the COSYCONET cohort study. Respir Res. 2019;20:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 33. | Löwe B, Schenkel I, Carney-Doebbeling C, Göbel C. Responsiveness of the PHQ-9 to Psychopharmacological Depression Treatment. Psychosomatics. 2006;47:62-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 86] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 34. | Matte DL, Pizzichini MM, Hoepers AT, Diaz AP, Karloh M, Dias M, Pizzichini E. Prevalence of depression in COPD: A systematic review and meta-analysis of controlled studies. Respir Med. 2016;117:154-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 125] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 35. | Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1525] [Cited by in RCA: 2190] [Article Influence: 146.0] [Reference Citation Analysis (0)] |
| 36. | Lee YS, Park S, Oh YM, Lee SD, Park SW, Kim YS, In KH, Jung BH, Lee KH, Ra SW, Hwang YI, Park YB, Jung KS; Korean COPD Study Group. Chronic obstructive pulmonary disease assessment test can predict depression: a prospective multi-center study. J Korean Med Sci. 2013;28:1048-1054. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 37. | Mitchell AJ, Meader N, Symonds P. Diagnostic validity of the Hospital Anxiety and Depression Scale (HADS) in cancer and palliative settings: a meta-analysis. J Affect Disord. 2010;126:335-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 258] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 38. | Norton S, Cosco T, Doyle F, Done J, Sacker A. The Hospital Anxiety and Depression Scale: a meta confirmatory factor analysis. J Psychosom Res. 2013;74:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 290] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 39. | Burns A, Höfer S, Curry P, Sexton E, Doyle F. Revisiting the dimensionality of the Hospital Anxiety and Depression Scale in an international sample of patients with ischaemic heart disease. J Psychosom Res. 2014;77:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |