Copyright
©The Author(s) 2015.
World J Dermatol. Nov 2, 2015; 4(4): 135-144
Published online Nov 2, 2015. doi: 10.5314/wjd.v4.i4.135
Published online Nov 2, 2015. doi: 10.5314/wjd.v4.i4.135
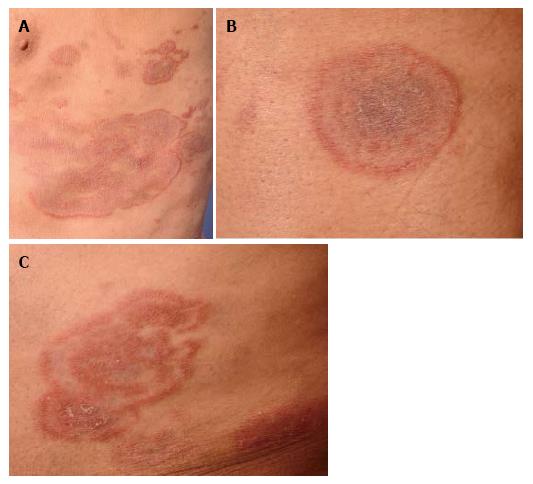
Figure 1 Mycosis fungoides presenting with annular lesions.
Clinical photographs of an 80-year-old male patient (case 1) with slowly progressive annular, cockadiform and arcuate lesions resembling tinea corporis (A), erythema exsudativum multiforme (B), and granuloma annulare (C), respectively.
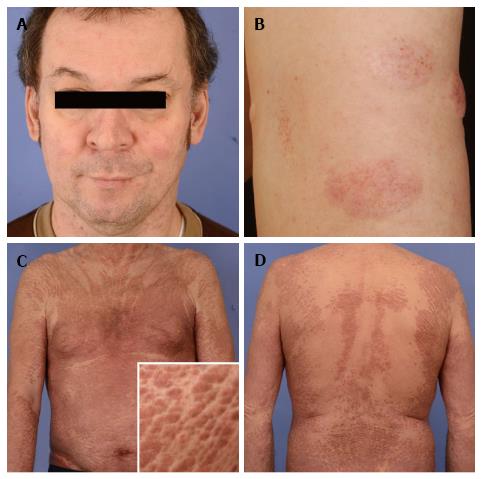
Figure 2 Mycosis fungoides resembling rosaea and Sézary-syndrome mimicking Ofuji´s papuloerythroderma.
A: Clinical images of a 46-year-old patient with granulomatous mycosis fungoides imitating rosacea and at the same time exhibiting clinical features of dermal elastolysis due to granulomatous slack skin syndrome (B) (case 9); C and D: Clinical images of a 71-year old patient with mycosis fungoides/Sézary-syndrome masquerading as Ofuji´s papuloerythroderma (case 2).
Figure 3 Mycosis fungoides as imitator of benign inflammatory dermatoses.
Clinical photomicrographs of skin lesions of mycosis fungoides mimicking urticaria pigmentosa (A) (case 5), plantar eczema (B) (case 7) and vitiligo/pityriasis alba (C) (case 6).
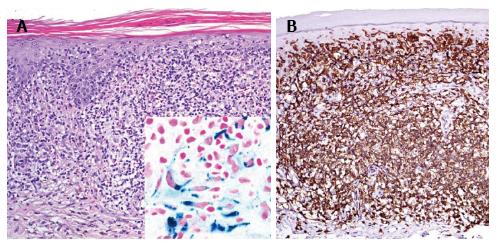
Figure 4 Histological findings.
A: Case 5 exhibitis extensive purpuric changes, pigment incontinence, interface dermatitis (HE staining, magnification 400 ×. Inlet iron staining); B: CD8+ cytotoxic epidermotropic infiltrate is depicted (CD8 immunohistochemical staining).
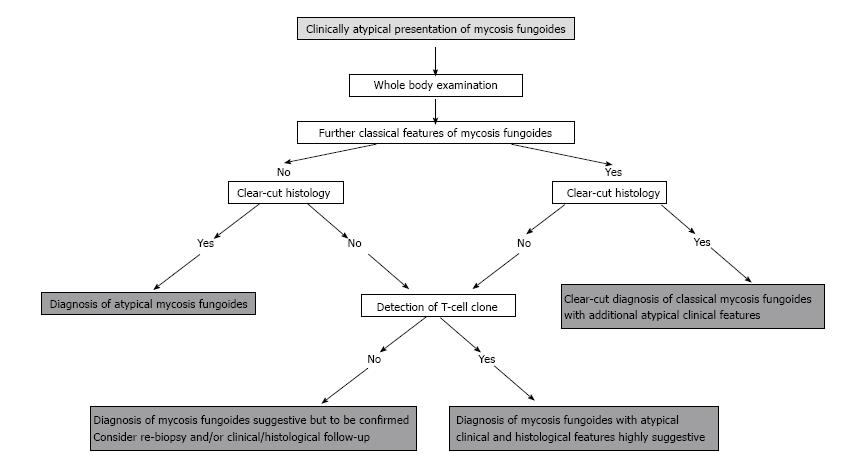
Figure 5 Schematic diagnostic algorithms for the clinical and histopathological work-up of “mimicking” cases of mycosis fungoides.
- Citation: Wobser M, Geissinger E, Rosenwald A, Goebeler M. Mycosis fungoides: A mimicker of benign dermatoses. World J Dermatol 2015; 4(4): 135-144
- URL: https://www.wjgnet.com/2218-6190/full/v4/i4/135.htm
- DOI: https://dx.doi.org/10.5314/wjd.v4.i4.135