Published online Sep 18, 2018. doi: 10.5312/wjo.v9.i9.149
Peer-review started: March 2, 2018
First decision: March 18, 2018
Revised: July 3, 2018
Accepted: July 14, 2018
Article in press: July 15, 2018
Published online: September 18, 2018
Processing time: 197 Days and 21.3 Hours
To compare clinical outcomes of patients with and without preoperative genu recurvatum (GR) following mobile bearing unicompartmental knee arthroplasty (UKA).
We prospectively followed 176 patients for at least 24 mo who had been treated by unilateral, minimally invasive, Oxford UKA. Patients with medial osteoarthritis (OA) knee and preoperative GR (Group I) accounted for 18% (n = 32) and patients without preoperative GR (Group II) accounted for the remaining 82% (n = 144). Knee score, pain scores, and functional scores were assessed for each patient and compared between the two groups. The incidence of postoperative GR and the postoperative hyperextension angles also were recorded and analyzed.
The pain score, knee score and functional score were not significantly different between the two groups. Similarly, the incidence of postoperative GR and the measured hyperextension angles were not significantly different between the two groups. The incidence of postoperative GR was 1/32 (3.12%) in Group I and 1/144 (0.69%) in Group II (P = 0.34). The mean postoperative hyperextension angles were 2.40° ± 2.19° (range: 1°-7°) for Group I and 1.57° ± 3.51° (range: 1°-6°) for Group II (P = 0.65).
Medial OA of the knee and concomitant GR is not a contraindication for the mobile bearing UKA.
Core tip: There is no previous study addressing the results of mobile bearing unicompartmental knee arthroplasty (UKA) in medial osteoarthritis (OA) knees with preexisting genu recurvatum (GR). This study determined the clinical outcomes and incidence of postoperative GR of medial OA knees with and without preexisting GR following mobile bearing UKA. Clinical outcomes, postoperative GR and hyperextension angle were evaluated at minimal 2 years of follow-up. Medial OA knees with and without GR showed no difference in clinical outcomes, incidence of postoperative GR or hyperextension angle. Therefore, medial OA knee with preoperative GR is not a contraindication for mobile bearing UKA.
- Citation: Pongcharoen B, Boontanapibul K. Outcomes of mobile bearing unicompartmental knee arthroplasty in medial osteoarthritis knee with and without preoperative genu recurvatum. World J Orthop 2018; 9(9): 149-155
- URL: https://www.wjgnet.com/2218-5836/full/v9/i9/149.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i9.149
The mobile bearing unicompartmental knee arthroplasty (UKA) has yielded excellent results in patients with medial osteoarthritis (OA) of the knees[1-6]. However, some patients who do not have neuromuscular disorders may develop medial OA of the knees and concomitant genu recurvatum (GR). Moreover, some patients have developed postoperative GR and shown poor clinical outcomes following fixed bearing UKA and total knee arthroplasty (TKA)[7-9]. The optimal prosthesis to use in patients with OA of the knees and GR remains controversial.
To the best of our knowledge, there have not been any studies reporting the clinical outcomes of mobile bearing UKA in medial OA knees with concomitant preoperative GR. The purpose of this study was, therefore, to determine the clinical outcome of the knee, as reflected by pain score, knee score and functional score, following the mobile bearing UKA and performing a comparison of the results between two groups of patients with medial OA knees, namely those with and without preoperative GR. The incidence of postoperative GR and the hyperextension angles were also compared.
We conducted a prospective cohort study of patients undergoing medial Oxford UKAs (Zimmer Biomet, Bridgend, United Kingdom), performed by a single surgeon, between January 2011 and November 2014 at the Thammasat University Hospital. The study was approved by the Human Research Ethics Committee of the Faculty of Medicine at Thammasat University. The clinical trial is registered at ClinicalTrials.gov (NCT02854189).
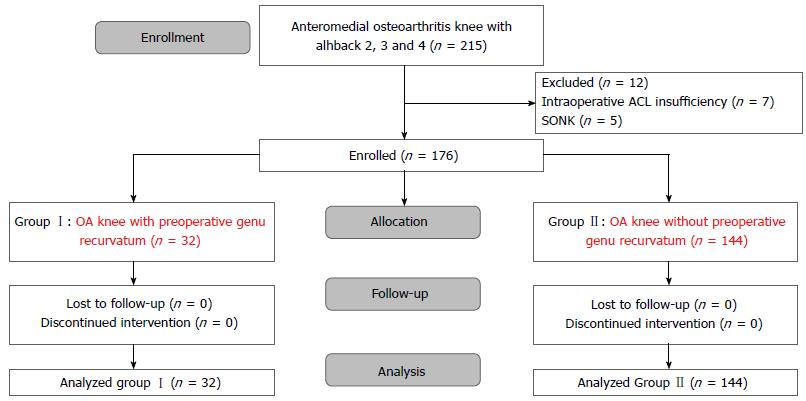
The patients were divided into two groups, with Group I consisting of 32 patients (32 knees) with preoperative GR and Group II consisting of 144 patients (144 knees) without preoperative GR. The Group I patients had hyperextension angle of more than 5°[7]. We enrolled patients with medial OA knees of moderate to severe Alhback class (grades 2, 3 and 4)[10]. The inclusion criteria were age older than 40 years, range of motion (ROM) greater than 90°, varus deformity less than 25°, and flexion contractures less than 20°. The exclusion criteria were diagnosis with spontaneous osteonecrosis of the knee (SONK), intraoperative anterior cruciate ligament insufficiency, posttraumatic arthritis, gouty arthritis, inflammatory joint disease, or history of a previous bilateral Oxford UKA. OA of the patellofemoral joint, young age and obesity were not considered contraindications for this procedure[1-3].
We recorded demographic data on a standard case record form, including age, sex, site, body mass index, preoperative ROM (measured with a long-arm goniometer), preoperative Knee Society Score© (KSS)[11], and preoperative tibiofemoral angle from standing anteroposterior knee radiograph (Table 1). The patients attended follow-up at 6 wk, 3 mo, 6 mo, 1 year, and annually thereafter. At each follow-up, a blinded research assistant recorded each patient’s KSS (pain score, knee score, and functional score). Incidence of postoperative GR and the hyperextension angles were also recorded. The patients were subjected to anteroposterior standing, lateral standing, skyline view and long-leg radiographs and the component alignment and tibiofemoral angles were recorded. Complications such as infection, component loosening, fractures and bearing dislocations were recorded.
| Variable | Group I (patients with preoperative genu recurvatum),n = 32 knees | Group II (patients without preoperative genu recurvatum),n = 144 knees | P-value |
| Age | 65.10 ± 8.02 (57-76) | 65.67 ± 7.40 (44-88) | 0.71 |
| Sex, male/female | 1/31 | 14/130 | 0.31 |
| Site, right/left | 16/17 | 70/74 | 0.91 |
| BMI | 26.76 ± 3.69 (20.81-33.21) | 26.26 ± 3.05 (20-42.22) | 0.47 |
| Knee score | 34.10 ± 2.47 (27-44) | 34.35 ± 2.62 (30-40) | 0.61 |
| Pain score | 11.52 ± 4.42 (0-20) | 11.75 ± 4.94 (0-20) | 0.23 |
| Functional score | 54.69 ± 9.75 (30-65) | 52.03 ± 10.13 (35-65) | 0.18 |
| ROM (°) | 122.58 ± 4.17 (110-125) | 119.37 ± 10.92 (90-130) | 0.10 |
| Tibiofemoral angle (°) | Varus 5.45 ± 3.86 (0-20) | Varus 5.68 ± 3.99 (0-15) | 0.77 |
The sample-size was calculated based on postoperative KSS, to ensure detection of a clinical relevant difference of 6 points using a standard deviation of 3.0[12]. It was determined that having 30 knees in Group I and 140 knees in Group II would allow for 80% power at the significance of 5%. Intergroup differences in age, knee score, pain score, functional score, body mass index, ROM, tibiofemoral angle, flexion contractures and GR were assessed using the Student’s t-test. Intergroup differences in incidence of GR, sex, ratio of sex and ratio of operative site were assessed using the chi-square or the Fisher’s exact test, as appropriate.
All patients were anesthetized via spinal block with morphine (0.1-0.2 mg). Prior to skin incision, all patients were fitted with a thigh tourniquet (inflated to 300 mmHg) and received 1 g cefazolin (intravenously). The size of the femoral component was chosen preoperatively using the X-ray template with a true lateral radiograph. For the Group I patients, there was an option of operation using a larger femoral component when the femoral component was between standard sizes or the hyperextension angle was between 10°-20°. Use of a larger femoral component will change the position at the superior part of the distal femoral condyle and tighten the extension gap, possibly preventing postoperative GR (Figure 1).
An anteromedial skin incision was made from the upper pole of the patella to the medial aspect of the tibial tubercle. A mini-midvastus approach was applied to all patients for prevention of patellar maltracking[13]. The patella was slightly subluxated laterally but was not everted. Minimally invasive instrumentation was used for all patients. The shaft of the tibial saw guide was parallel to the long axis of the tibia to create 7° tibial slope. The depth of the tibial bone cut was 2 mm below the deepest part of the medial tibial plateau and perpendicular to the mechanical axis. The posterior condyle of the femur was then cut using intramedullary femoral-guided instrumentation that connected the femoral drill guide with the intramedullary (IM) link.
The flexion gap was set at 100° of flexion, then the extension gap was set at 20° of flexion. The distal condyle of the femur was cut by the milling technique, to create equal flexion-extension gap. However, in Group I patients, the distal condyle of the femur were removed at 1 mm less length than that of the Group II patients, to tighten the extension gap. If patients in Group I showed slight flexion contracture (< 10°) intraoperatively after applying the trial prosthesis, the slight flexion contracture would have been accepted; however, if the knee showed flexion contracture more than 10°, the distal femur would have been recut to create equal gap.
All operations used the same instrumentation to finish the tibia and femur. Thirty millimeters of bupivacaine was injected prior to closing the incision, with one intraarticular drain (10-G) having been inserted before closing. The operative time, blood loss volume and occurrence of intraoperative fracture were recorded.
Medial OA knees with and without preoperative GR less than 19° have similar clinical outcome and incidence of postoperative GR. A total of 176 patients (15 males and 161 females) underwent unilateral mobile bearing UKAs, and the total 176 knees were evaluated for study entry (Trial profile, Figure 2). The patients’ ages ranged from 43-88 years (mean: 65.30 years). Thirty-two patients had preoperative GR and one hundred and forty-four patients did not have preoperative GR. All demographic and preoperative characteristics were similar between the two groups.
The mean hyperextension angle of Group I patients was 7.03° ± 3.19° (5°-19°). The mean hyperextension angle and flexion contracture of Group II patients were 0.02° ± 0.19° (1°-2°) and 6.99° ± 5.03° (1°-18°), respectively. Follow-up extended from 24 mo to 70 mo, for an overall mean of 37.66 mo; no patients were lost to follow-up. The pain scores, knee scores and functional scores were not significantly different between the two groups (Table 2). The mean KSS of patients in Group I improved from 34.10 ± 2.47 (27-44) to 97.97 ± 2.49 (94-100), and the KSS of patients in Group II improved from 34.35 ± 2.62 (30-40) to 96.91 ± 4.44 (81-100) (Tables 1 and 2). The incidence of postoperative GR was 3.13% in Group I compared to 0.7% in Group II (P = 0.34), and the mean postoperative hyperextension angle was 2.40° ± 2.19° (1°-7°) for Group I compared to 1.57° ± 3.51° (1-6) in Group II (P = 0.65) (Table 3). No patient in Group I showed flexion contracture.
| Variable | Group I (patients with preoperative genu recurvatum),n = 32 knees | Group II (patients without preoperative genu recurvatum),n = 144 knees | P-value |
| Knee score, points | 97.97 ± 2.49 (94-100) | 96.91 ± 4.44 (81-100) | 0.19 |
| Pain score, points | 48.94 ± 2.36 (45-50) | 48.71 ± 2.63 (40-50) | 0.64 |
| Functional score, points | 82.12 ± 4.85 (80-100) | 82.55 ± 5.10 (65-100) | 0.66 |
| Variable | Group I (patients with preoperative genu recurvatum),n = 32 knees | Group II (patients without preoperative genu recurvatum),n = 144 knees | P-value |
| Incidence of postoperative genu recurvatum (%) | 3.13 (1/32) | 0.69 (1/144) | 0.34 |
| Hyperextension angle (°) | 2.40 ± 2.19 (1-7)) | 1.57 ± 3.51 (1-6) | 0.65 |
The postoperative ROM, postoperative tibiofemoral angles, femoral component alignment, tibial component alignment, posterior slope of the tibial component, and operative times were not different between the two groups (Table 4). This study did not observe any postoperative complications, such as patellar crepitation, infections, mobile bearing dislocation or component loosening. However, one patient in Group II did suffer a medial tibial plateau fracture at 3 mo postoperatively and was excluded from the study; this patient underwent a revision TKA, with good result.
| Variable | Group I (patients with preoperative genu recurvatum),n = 32 knees | Group II (patients without preoperative genu recurvatum),n = 144 knees | P-value |
| Postoperative ROM (°) | 126.21 ± 5.30 (115-135) | 123.30 ± 9.88 (90-145) | 0.14 |
| Postoperative tibiofemoral angle (°) | 5.82 ± 1.55 (valgus 3-valgus 8) | 5.66 ± 1.77 (valgus 2-valgus 10) | 0.65 |
| Femoral component alignment (°) | 6.06 ± 1.43 (valgus 2-valgus 8) | 5.99 ± 1.56 (valgus 2-valgus 10) | 0.82 |
| Tibia component alignment (°) | Varus 0.97 ± 0.92 (varus 3-valgus 1) | Varus 0.77 ± 1.19 (varus 3-valgus 2) | 0.37 |
| Posterior slope of tibial component (°) | 6.73 ± 1.92 (4-10) | 6.31 ± 2.04 (2-10) | 0.28 |
| Operative time in min | 88.94 ± 10.59 (75-120) | 93.01 ± 13.64 (65-130) | 0.11 |
To the best of our knowledge, no previous study in the publicly available literature has addressed the clinical outcomes of the mobile bearing UKA in medial OA of the knees in patients with preexisting GR. In the study, the OA knees with and without preexisting GR showed good clinical outcome following mobile bearing UKA. The postoperative pain score, knee score and functional score were no different between the two groups (i.e., with and without preexisting GR). The incidence of postoperative GR and hyperextension angles were also essentially the same for the two groups.
Previous studies have found that patients who had preoperative GR tended to develop GR postoperatively, and showed poor clinical outcome following TKA and fixed bearing UKA applied using the standard surgical technique[7-9]. Only one study has determined the hyperextension angle of this group of patients following TKA and fixed bearing UKA[7]. In that study, the hyperextension angles decreased from 6° ± 2° to 2° ± 4° after TKA and 7° ± 2° to 1° ± 3° after fixed bearing UKA[7]. Therefore, Mullaji et al[14] set a slightly tight extension gap for medial OA knee with preoperative GR, with the aim of preventing recurrent hyperextension deformity following TKA. The patients with preexisting GR were reported to have good clinical results and no development of recurrent hyperextension deformity with the tight extension gap[14].
In the present study, the patients who had preoperative hyperextension angle up to 19° showed excellent clinical outcome and did not develop postoperative GR at 3 years of follow-up (Figure 3). The different results in our study compared to those from the previous studies may be due to several issues. First, the medial mobile bearing UKA has shown normal or nearly normal biomechanics and kinematics, with the knee joint stability, ligament tension and knee alignment returning to predisease stage levels[15-17]. Second, our study used a larger femoral component when between sizes. The extension gap was tight, even when knees were extended beyond full extension (Figure 1). It is important to note, however, that an abnormally large femoral component may also cause problems with the patellofemoral joint; nonetheless, our study showed no anterior knee pain, patellar crepitation or patellar dislocation in the Group I patients. Moreover, the phases I and II of the Oxford mobile bearing UKA used only a single size for the femoral component, being applied to all patients, and no patients to date have had to undergo surgical revision because of patellofemoral joint problems[1,18]. Third, our study set a tighter extension gap or slight flexion contracture in some of the patients in Group I, for prevention of GR. However, no patients have presented flexion contracture postoperatively, even after 2 years of follow-up. Moreover, no patients have developed overcorrection of the tibiofemoral joint. The tibiofemoral angle of Group I patients showed a greater valgus alignment than that of Group II patients, but this was within normal limits. Fourth, all patients were encouraged to perform quadricep exercises to improve quadricep muscle power before and after the operation. Meding et al[19] showed that weakness of the quadricep muscles can cause GR.
Our study has some limitations that should be considered when interpreting our findings. Firstly, the hyperextension angle may represent an underestimation. The pain may be uncomfortable for patients, resulting in some reduction of knee hyperextension. Therefore, both groups of patients might present higher hyperextension angles. Secondly, our study showed that the patients with preoperative GR of up to 19° have good clinical outcomes following mobile bearing UKA; patients with preoperative GR of more than 19° are now needed to compare the clinical outcome with primary TKA or constrained TKA. Thirdly, although the mean age of both groups was similar, the age range was different for the two groups (57-76 years for Group I patients and 44-88 years for Group II patients). Thus, the Group II patients may have presented better clinical outcome than the generally older Group I patients. However, the clinical outcome of the Group I patients was not different than that of the Group II patients. In conclusion, combined GR and medial OA of the knee is not a contraindication for mobile bearing UKA, and good outcomes may be expected.
Postoperative genu recurvatum (GR) has a tendency to develop in the medial osteoarthritis (OA) knee with preexisting GR following total knee arthroplasty (TKA) and unicompartmental knee arthroplasty (UKA). The prosthesis of choice for medial OA knee with preexisting GR is controversial. Constrained TKA has been chosen by some surgeons for prevention of postoperative GR, even though the patients could develop early loosening of the prosthesis, require early reoperation, and experience bone loss during revision TKA. The present study found that the medial OA knee with preoperative GR (< 19°) and without preoperative GR have similar clinical outcomes and determined the incidence of postoperative GR following mobile bearing UKA. Use of the normal biomechanic and kinematic parameters, while adjusting some steps of the surgical technique, including a tighter extension gap with and without application of larger femoral component, could prevent postoperative GR following mobile bearing UKA.
Medial OA knees with and without preexisting GR have shown good clinical outcomes and no difference in incidence of postoperative GR following mobile bearing UKA. However, the causes of OA knee with preexisting GR are unclear. Quadricep muscle weakness from spondylosis or abnormal ligament tension might underlie the occurrence of OA knee with preexisting GR. Therefore, the future research should focus on this yet unresolved issue.
The main objectives of this study were to determine the clinical outcomes and the incidence of postoperative GR in medial OA knees with and without preexisting GR.
In this prospective cohort study, we used pain score, functional score and knee score to compare patients having medial OA knees with and without preexisting GR. The occurrence of postoperative GR and hyperextension angle were also recorded. Follow-up extended from 24 mo to 70 mo, for a mean of 37.66 mo. No patients were lost to follow-up.
Medial OA knees with and without preexisting GR showed similar clinical outcomes and incidence of postoperative GR following mobile bearing UKA. The mean Knee Society Score© was 97.97 for patients with preexisting GR and 96.91 for patients without GR. The incidences of postoperative GR were 3.13% and 0.7% for patients with preexisting GR and patients without preexisting GR, respectively.
Medial OA knee with preoperative GR is not a contraindication for mobile bearing UKA.
Mobile bearing UKA with a little tight extension gap with and without use of a larger femoral component could prevent postoperative GR in the medial OA knee with preexisting GR. However, the causes of GR in OA knee patients without neuromuscular disorder remain unclear and should be identified by future studies.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Thailand
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Fernandez-Fairen M, Kuru T, Liu J S- Editor: Ji FF L- Editor: A E- Editor: Song H
| 1. | Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br. 1998;80:983-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 186] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 2. | Price AJ, Waite JC, Svard U. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2005;171-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 176] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 3. | Pongcharoen B, Reutiwarangkoon C. The comparison of anterior knee pain in severe and non severe arthritis of the lateral facet of the patella following a mobile bearing unicompartmental knee arthroplasty. Springerplus. 2016;5:202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Faour-Martín O, Valverde-García JA, Martín-Ferrero MA, Vega-Castrillo A, de la Red Gallego MA, Suárez de Puga CC, Amigo-Liñares L. Oxford phase 3 unicondylar knee arthroplasty through a minimally invasive approach: long-term results. Int Orthop. 2013;37:833-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Clarius M, Hauck C, Seeger JB, Pritsch M, Merle C, Aldinger PR. Correlation of positioning and clinical results in Oxford UKA. Int Orthop. 2010;34:1145-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Xue H, Tu Y, Ma T, Wen T, Yang T, Cai M. Up to twelve year follow-up of the Oxford phase three unicompartmental knee replacement in China: seven hundred and eight knees from an independent centre. Int Orthop. 2017;41:1571-1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Jiang L, Chen JY, Chong HC, Chia SL, Lo NN, Yeo SJ. Early Outcomes of Unicompartmental Knee Arthroplasty in Patients With Preoperative Genu Recurvatum of Non-neurological Origin. J Arthroplasty. 2016;31:1204-1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Siddiqui MM, Yeo SJ, Sivaiah P, Chia SL, Chin PL, Lo NN. Function and quality of life in patients with recurvatum deformity after primary total knee arthroplasty:s a review of our joint registry. J Arthroplasty. 2012;27:1106-1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Koo K, Silva A, Chong HC, Chin PL, Chia SL, Lo NN, Yeo SJ. Genu Recurvatum versus Fixed Flexion after Total Knee Arthroplasty. Clin Orthop Surg. 2016;8:249-253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968;Suppl 277: 7-72. [PubMed] |
| 11. | Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;13-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1602] [Cited by in RCA: 1613] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 12. | Lee WC, Kwan YH, Chong HC, Yeo SJ. The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2017;25:3354-3359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 195] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 13. | Pongcharoen B, Yakampor T, Charoencholvanish K. Patellar tracking and anterior knee pain are similar after medial parapatellar and midvastus approaches in minimally invasive TKA. Clin Orthop Relat Res. 2013;471:1654-1660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Mullaji A, Lingaraju AP, Shetty GM. Computer-assisted total knee replacement in patients with arthritis and a recurvatum deformity. J Bone Joint Surg Br. 2012;94:642-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Whittle MW, Jefferson RJ. Functional biomechanical assessment of the Oxford Meniscal Knee. J Arthroplasty. 1989;4:231-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Miller RK, Goodfellow JW, Murray DW, O’Connor JJ. In vitro measurement of patellofemoral force after three types of knee replacement. J Bone Joint Surg Br. 1998;80:900-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Price AJ, Rees JL, Beard DJ, Gill RH, Dodd CA, Murray DM. Sagittal plane kinematics of a mobile-bearing unicompartmental knee arthroplasty at 10 years: a comparative in vivo fluoroscopic analysis. J Arthroplasty. 2004;19:590-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 95] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Goodfellow JW, Kershaw CJ, Benson MK, O’Connor JJ. The Oxford Knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg Br. 1988;70:692-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 193] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Meding JB, Keating EM, Ritter MA, Faris PM, Berend ME. Total knee replacement in patients with genu recurvatum. Clin Orthop Relat Res. 2001;244-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |