Published online Jul 18, 2017. doi: 10.5312/wjo.v8.i7.561
Peer-review started: January 16, 2017
First decision: March 28, 2017
Revised: April 10, 2017
Accepted: May 3, 2017
Article in press: May 5, 2017
Published online: July 18, 2017
Processing time: 180 Days and 18 Hours
To investigate non-ossifying fibromas (NOFs) common fibrous bone lesions in children that occur in bones of the lower extremities.
We analyzed 44 cases of NOF including 47 lesions, which were referred with a working diagnosis of neoplastic lesions. Lesions were located in the upper extremities (1 proximal humerus, 1 distal radius) and the lower extremities (25 distal femurs, 12 proximal and 4 distal tibias, and 4 proximal fibulas).
Three cases had NOFs in multiple anatomical locations (femur and fibula in 1 case, femur and tibia in 2 cases). Overall, larger lesions > 4 cm and lesion expansion at the cortex were seen in 21% and 32% of cases, respectively. Multiple lesions with bilateral symmetry in the lower extremities suggest that these NOFs were developmental bone defects. Two patients suffered from fracture and were treated without surgery, one in the radius and one in the femur. Lesions in the upper extremities (i.e., humerus of a 4-year-old female and radius of a 9-year-old male) expanded at the cortex and lesion size increased with slow ossification.
NOFs in the lower extremity had fewer clinical problems, regardless of their size and expansiveness. In these two upper extremity cases, the NOFs had aggressive biological features. It seems that there is a site specific difference, especially between the upper extremity and the lower extremity. Furthermore, NOFs in the radius are predisposed to fracture because of the slender structure of the radius and the susceptibility to stress.
Core tip: Non-ossifying fibromas (NOFs) are common lesions in the lower extremities of children. We analyzed 44 cases of NOF including 47 lesions comprising 2 upper extremity cases and 45 lower extremity cases. Larger lesions > 4 cm and lesion expansion at the cortex were seen in 21% and 32% of cases, respectively. Lesions in the upper extremities in the humerus and the radius expanded at the cortical bone, and lesion size increased with slow ossification, suggestive of aggressive biological features. Furthermore, NOFs in the radius are predisposed to fracture because of the slender structure of the radius and the susceptibility to stress.
- Citation: Sakamoto A, Arai R, Okamoto T, Matsuda S. Non-ossifying fibromas: Case series, including in uncommon upper extremity sites. World J Orthop 2017; 8(7): 561-566
- URL: https://www.wjgnet.com/2218-5836/full/v8/i7/561.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i7.561
Non-ossifying fibromas (NOFs) are a common type of benign fibrous lesion that tend to occur in the metaphysis of the long bones in the lower extremities[1,2]. NOF can be diagnosed based on its presentation on plain radiographs[3,4] where it typically appears as a small, cortical osteolytic lesion. Approximately 30% of young patients in their first or second decade of life can have a NOF[2]. Typically, NOFs are asymptomatic and lesions are found incidentally. A lesion is usually self-limiting and disappears by the age of 20 to 25 years in most cases[3]. Therefore, lesions are considered to be a developmental bone defect rather than a true neoplasm[1,2]. Histologically, NOFs are composed of spindle-shaped fibroblasts, multinucleated giant cells, and foamy histiocytes, which are identical to a benign fibrous histiocytoma (BFH), which is a neoplastic lesion[2]. BFHs occur predominantly in adults, and a BFH is considered to have more aggressive biological features compared with a NOF. Interestingly, the current case series includes some patients with NOFs in less common sites such as the humerus, radius, and fibula. Herein we discuss upper and lower extremity NOFs and emphasize the anatomical differences between them.
A clinical summary of the 44 cases of NOF is shown in Table 1. A total of 47 lesions were referred to our institution with a working diagnosis of neoplastic lesions. A diagnosis of NOF was made based on plain radiographic findings. NOF appears as a cortically based osteolytic lesion with an osteosclerotic rim. In cases with atypically large lesions, a magnetic resonance image (MRI) examination was added in order to exclude aggressive bone tumors, such as osteosarcomas. The NOF cases we analyzed were in 26 males and 18 females. The average age at the first visit was 10.5 (range, 4 to 16) years. The NOFs were located in a humerus (n = 1), radius (n = 1), femurs (n = 25), tibias (n = 16), and fibulas (n = 4). Among these cases, lesions occurred in multiple locations in 3 cases with femur involvement, in 2 cases with tibia involvement and in 1 case with femur and fibula involvement. Bilateral lesions, in which the size and the location were almost symmetrical such that we counted them as a single lesion, were seen in 3 cases with femur involvement. The location of each lesion was also classified as anterior, medial, lateral, posterior, or inter-medullary. Findings of expansion at the cortices adjacent to lesions were assessed. A lesion > 4 cm in size was defined as large.
| Bone site | NOFs, n | M:F | Mean age, yr | R/L/B extremities, n | Lesion > 4 cm, n (%) | Ant/med/lat/post/intramed location, n | Expansion, n (%) | Fracture, n (%) |
| Humerus | 1 | |||||||
| Proximal | 1 | 0:1 | 4.0 | 1/0/0 | 1 (100) | 1/0/0/0/0 | 1 (100) | 0 |
| Radius | 1 | |||||||
| Distal | 1 | 1:0 | 7.0 | 0/1/0 | 0 | 0/0/0/0/1 | 1 (100) | 1 (100) |
| Femur | 25 | |||||||
| Distal | 25 | 15:10 | 9.2 | 9/9/7 | 5 (20) | 0/5/0/20/0 | 5 (20) | 1 (4) |
| Tibia | 16 | |||||||
| Proximal | 12 | 8:4 | 14.5 | 6/6/0 | 2 (17) | 0/4/1/7/0 | 3 (25) | 0 |
| Distal | 4 | 2:2 | 13.5 | 3/1/0 | 2 (50) | 0/0/4/0/0 | 2 (50) | 0 |
| Fibula | 4 | |||||||
| Proximal | 4 | 2:2 | 12.5 | 2/2/0 | 0 | 0/0/1/3/0 | 3 (75) | 0 |
| Total lesions1 | 47 | 26:18 | 10.5 | 21/19/7 | 10 (21) | 1/9/6/30/1 | 15 (32) | 2 (4) |
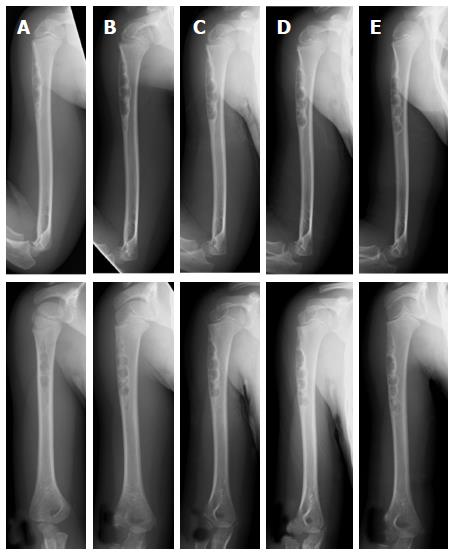
Among the NOF cases, a lesion size > 4 cm was seen in 10 out of 47 (21%) cases. Cortical expansions were seen in 15 out of 47 (32%) cases. The cases of upper extremity NOFs involved 1 humerus and 1 radius. A 4-year-old female had a NOF on the proximal side of her humerus. Plain radiographs revealed a multinodular osteolytic lesion in the cortex on the anterior aspect of the humerus. Thinning and expansion of the adjacent cortex was observed. During a 7-mo follow-up, it was noted that the size of the lesion had increased. Ossification was seen, but the earlier osteolytic finding was still prominent on a follow-up radiograph taken 31 mo later (Figure 1). A 9-year-old male had a NOF on the distal diaphysis of his radius. The lesion was discovered when he sustained a pathological fracture at the site of the lesion. Upon initial assessment, the plain radiographs revealed an irregularity of the adjacent cortex, suggesting a fracture. An osteolytic lesion with marginal sclerosis was seen. The size of the lesion was observed to increase at a 2 years and 5 mo follow-up because the patient had refractured his radius at the lesion site. Although ossification was evident on the proximal aspect of the lesion, an osteolytic lesion was also prominent at the 3-year follow-up (Figure 2).
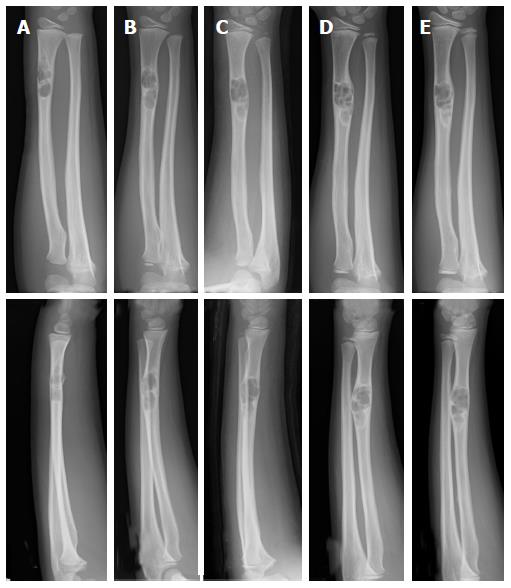
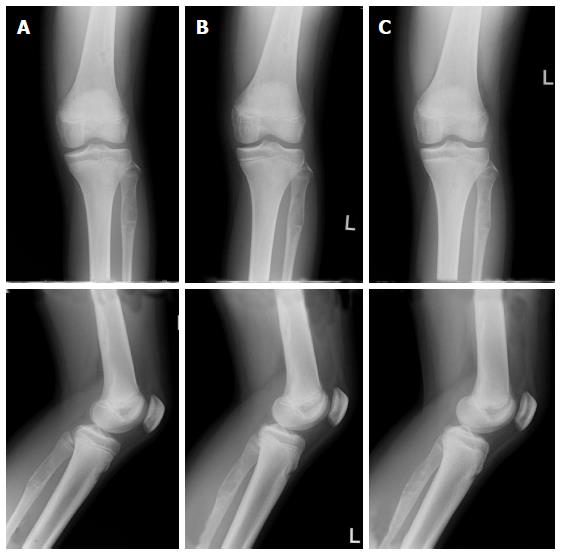
The cases of lower extremity NOFs involved femurs, tibias, and fibulas. All femoral lesions were at distal locations. Both large-sized lesions with expansion at the cortex were seen in 20% of cases with femoral involvement. One case of NOF in the femur was diagnosed with a concurrent fracture based on an MRI finding of a high signal intensity at the cortex adjacent to the lesion (Figure 3). Of the 16 cases with tibia involvement, 12 lesions were in a proximal location and 4 were distal. Large-sized lesions occurred in 2 out of 12 (17%) cases in the proximal tibia and in 2 out of 4 (50%) cases in the distal tibia. Extension at the cortex was seen in 3 out of 12 (25%) cases in the proximal tibia and in 2 out of 4 (50%) cases in the distal tibia. These femoral and tibial lesions were in either the medial, lateral, or posterior locations, in contrast to the anterior location in the case of humerus involvement. All 4 cases of NOFs in fibulas presented with lesions in proximal locations. NOF cases with cortical expansion were seen in 3 out of 4 (75%) cases with fibula involvement. One fibular case had multiple lesions that included the femur (Figure 4).
NOF predominantly occurs in the lower extremities, especially around the knee[1,2]. In the current series, the frequency of a distal location in the femur was rather low, because all the referred cases were considered as potential neoplastic lesions, and when small more typical NOFs in the distal femur were identified, the patients were not referred. NOFs are not considered to be true neoplasms, but rather a developmental bone defect[1-3]. Cases with multiple affected locations, such as the femur and fibula or the femur and tibia, support the notion of a natural developmental defect.
Findings of lesion size increases with expansion at the cortex suggest NOFs can be more aggressive in nature. Cytological abnormalities of translocation (1;4)(p31;q34) and del(4)(p14) supplied evidence for some NOFs with neoplastic characteristics[5,6]. It is possible that NOFs could have a neoplastic nature because histologically they are indistinguishable from the neoplastic lesions of BFH, which are more aggressive in nature than those of NOFs[7]. Using image analysis techniques to differentiate between BFHs and NOFs, BFHs appear more likely to have less distinct borders that are central rather than eccentric[7,8]. BFHs tend to occur in adults, while the vast majority of cases of NOF occur in children. However, it has been proposed that BFHs may be underestimated among patients less than 20 years of age, and the diagnosis of BFH should be considered when NOF-like pathology is accompanied by pain or rapid lesion growth[7]. In the current series, NOFs in the lower extremities ossified, even in cases with large lesions that increased in size, but none was diagnosed as BFH.
NOFs located in the humerus and radius were included in this study although the upper extremities are an uncommon site for these lesions. Both lesions had extended at the cortex and lesion size increased over time; however, ossification was observed despite osteolytic findings still being prominent at 3 years of follow up. Although the number of upper extremity NOF cases was small, they can have an aggressive nature with BFH-like features when compared with the NOFs in the lower extremities. The NOF located in the radius resulted in a complication when the patient sustained repeated fractures. NOF lesions that occupy more than 50% of the transverse diameter of the involved bone are more likely to lead to a fracture[2,9]. The slender anatomical structure of the radius would also have contributed to the risk of a pathological fracture at the location of the NOF in this case.
In conclusion, NOFs in lower extremities have the non-neoplastic characteristics of a developmental bone defect. In contrast, NOFs in the humerus and the radius tended to have more aggressive biological characteristics similar in nature to those of BFHs with expansion at the cortex, an increase in size, and slow ossification. It seems that there is a site specific difference between the upper and lower extremities. In addition, NOFs in the radius are potentially prone to fracture because of the slender structure of the affected bone.
Non-ossifying fibromas (NOFs) are a common type of benign fibrous lesion that tend to occur in the metaphysis of the long bones in the lower extremities. The upper extremity is less common for NOFs. NOFs are considered to be a developmental bone defect rather than a true neoplasm. However, the histology of NOFs is identical to that of benign fibrous histiocytoma, which is a neoplastic lesion.
Small NOFs have no clinical significance. The neoplastic characterization of NOFs was difficult. Therefore, the authors collected NOF cases that were referred with a working diagnosis of neoplastic lesions. Consequently, large NOFs with possible aggressive characteristics, as well as NOFs in rare locations, were collected.
The authors analyzed 44 cases of NOFs including 47 lesions comprising two upper extremity cases and 45 lower extremity cases. Clinical information and plain radiographs were collected. The findings associated with possible aggressiveness were further analyzed, such as incidence of fracture and radiographic observations of size and expansiveness. It seems that there is a site specific difference between the upper and lower extremities. NOFs in the lower extremity are considered to be a developmental bone defect rather than a true neoplasm, even though NOFs can be large and have expansion at the cortex. Lesions in the humerus and the radius were expanded at the cortex and lesion size increased with slow ossification. Furthermore, NOFs in the radius are predisposed to fracture because of the slender structure of the radius and its susceptibility to stress.
The results are useful for clinicians in the making a diagnosis of NOF and following up the patients.
NOF: Non-ossifying fibroma; BFH: Benign fibrous histiocytoma; MRI: Magnetic resonance image.
This is a well-designed paper about a rarely seen clinical condition.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Demiroz SM S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Hetts SW, Hilchey SD, Wilson R, Franc B. Case 110: Nonossifying fibroma. Radiology. 2007;243:288-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Dorfman HD, Czerniak B. Bone tumors. St Louis, MO, Mosby, 1998. Hum Pathol. 1999;30:1269. |
| 3. | Betsy M, Kupersmith LM, Springfield DS. Metaphyseal fibrous defects. J Am Acad Orthop Surg. 2004;12:89-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Hod N, Levi Y, Fire G, Cohen I, Ayash D, Somekh M, Horne T. Scintigraphic characteristics of non-ossifying fibroma in military recruits undergoing bone scintigraphy for suspected stress fractures and lower limb pains. Nucl Med Commun. 2007;28:25-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Nelson M, Perry D, Ginsburg G, Sanger WG, Neff JR, Bridge JA. Translocation (1; 4)(p31; q34) in nonossifying fibroma. Cancer Genet Cytogenet. 2003;142:142-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Tarkkanen M, Kaipainen A, Karaharju E, Böhling T, Szymanska J, Heliö H, Kivioja A, Elomaa I, Knuutila S. Cytogenetic study of 249 consecutive patients examined for a bone tumor. Cancer Genet Cytogenet. 1993;68:1-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Ceroni D, Dayer R, De Coulon G, Kaelin A. Benign fibrous histiocytoma of bone in a paediatric population: a report of 6 cases. Musculoskelet Surg. 2011;95:107-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Al-Jamali J, Gerlach UV, Zajonc H. Benign fibrous histocytoma of the distal radius: a report of a case and a review of the literature. Hand Surg. 2010;15:127-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Easley ME, Kneisl JS. Pathologic fractures through nonossifying fibromas: is prophylactic treatment warranted? J Pediatr Orthop. 1997;17:808-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |