Published online Aug 18, 2025. doi: 10.5312/wjo.v16.i8.109885
Revised: June 11, 2025
Accepted: July 18, 2025
Published online: August 18, 2025
Processing time: 75 Days and 23.4 Hours
Leg length discrepancy (LLD) following total hip arthroplasty (THA) is a common complaint, leading to decreased patient satisfaction. However, the effect of LLD before THA on outcomes and complications is not well defined.
To assess the effect of prior LLD on rates of falls, implant-related complications, stay length, readmissions, and implant survival following THA.
A retrospective review of a nationwide insurance database was conducted from 2010 to 2021. All cases of THA and those with a prior diagnosis of LLD were identified. THA patients with LLD were matched to control patients 1:5 based on demographic and comorbidity profiles. Two-year fall rates and implant complications, lengths of stay, 90-day readmissions, and time to revision were compared between cohorts.
A total of 2038 patients with LLD were matched to 10165 control patients. The LLD group showed significantly greater rates of falls [odds ratio (OR) = 1.58; 95% confidence interval (95%CI): 1.24-2.01], dislocation (OR = 2.61; 95%CI: 2.10-3.24), mechanical loosening (OR = 4.58; 95%CI: 3.28-6.29), and periprosthetic fracture (OR = 2.70; 95%CI: 1.96-3.72) compared to the control group (all P < 0.001). Mean length of stay (LOS) was also significantly higher in the LLD group (3.1 days vs 2.8 days, P = 0.034). No significant difference in 90-day readmission rates (7.75% vs 7.02%, P = 0.244) was observed between the groups (P = 0.244). Time to revision was significantly less in the LLD group (225 days vs 544 days, P < 0.001).
LLD in patients having THA is related with significantly higher fall risk, rates of implant-related complications, LOS, and quicker time to revision. Identifying patients with LLD before their THA may help in identifying risks, better patient counselling, and more effective preoperative planning. However, the study have important limitations: Its design lacks information on the degree and cause of LLD, the time between diagnosis and surgery, and which leg with the discrepancy underwent the operation. Future well-designed studies should confirm the findings of this study.
Core Tip: Leg length discrepancy (LLD) after total hip arthroplasty (THA) is a routine complaint, resulting in decreased patient satisfaction. Yet, the consequence of LLD before THA on outcomes and complications is not well defined. Here, we assessed the effect of prior LLD on rates of falls, implant complications, length of stay, readmissions, and implant survival following THA. Patients undergoing THA with LLD exhibited markedly elevated rates of falls, increased odds of prosthetic complications, prolonged hospitalization, and earlier revision timelines. Considering these implications, assessing limb length before surgery becomes crucial to enhance surgical planning and perioperative management, thereby mitigating associated risks.
- Citation: Rodriguez HC, Mekkawy KL, Rust BD, Yergler TO, Corces A, Roche MW, Gupta A. Prior leg length discrepancy in total hip arthroplasty patients causes greater implant complications and faster time to revision. World J Orthop 2025; 16(8): 109885
- URL: https://www.wjgnet.com/2218-5836/full/v16/i8/109885.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i8.109885
Leg length discrepancy (LLD) is generally described as an asymmetry in the length of a limb, a condition that may arise congenitally or be acquired[1,2]. This incongruity is notably prevalent among individuals undergoing total hip arthroplasty (THA), presenting itself as a noteworthy concern both before and following the surgical intervention[3]. The clinical significance of LLD post-THA is underscored by its correlation with an elevated prevalence of aseptic loosening, post-operative dislocation, back pain, gait disturbances, a general sense of postoperative dissatisfaction and litigation[1,3,4]. Primary THA stands among the top five most frequently performed procedures across all surgical disciplines in the United States, with a projected continual increase in numbers through the year 2030[5,6]. Consequently, it is imperative to identify areas warranting enhancement in patient outcomes and satisfaction in this demographic.
Preoperative LLD is often overlooked, and its impact on outcomes following THA remains inadequately defined in current literature. LLD has the potential to unevenly stress joints from foot to spine in an upright posture, heightening internal joint load and diminishing articular cartilage contact area, thereby contributing to postoperative complications and osteoarthritis development[7]. Therefore, addressing preoperative LLD during THA planning is crucial for optimizing long-term joint function and reducing the risk of adverse outcomes.
This study aimed to investigate how pre-existing limb length discrepancy influences: (1) The risk of falls; (2) Prosthetic complications at 2 years follow-up; (3) Hospital stay duration, and rate of readmission within 90 days; and (4) The occurrence of revision hip arthroplasty and time to revision in individuals undergoing THA.
A comprehensive examination of the PearlDiver Database (PearlDiver Technologies, Colorado Springs, CO, United States) was conducted between January 2010 and October 2021. PearlDiver, a leading commercial database, serves as a comprehensive repository for extensive de-identified medical records sourced from private insurance claims analysis, conforming to Health Insurance Portability and Affordability Act regulations[8,9]. Given the de-identification of patients within the cohorts, this study is deemed exempt from the institutional review board. The identification of patients, diagnoses, procedures, and complications was facilitated through the application of the international classification of disease (ICD) codes, Ninth and Tenth Revisions, and current procedural terminology (CPT) codes. The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
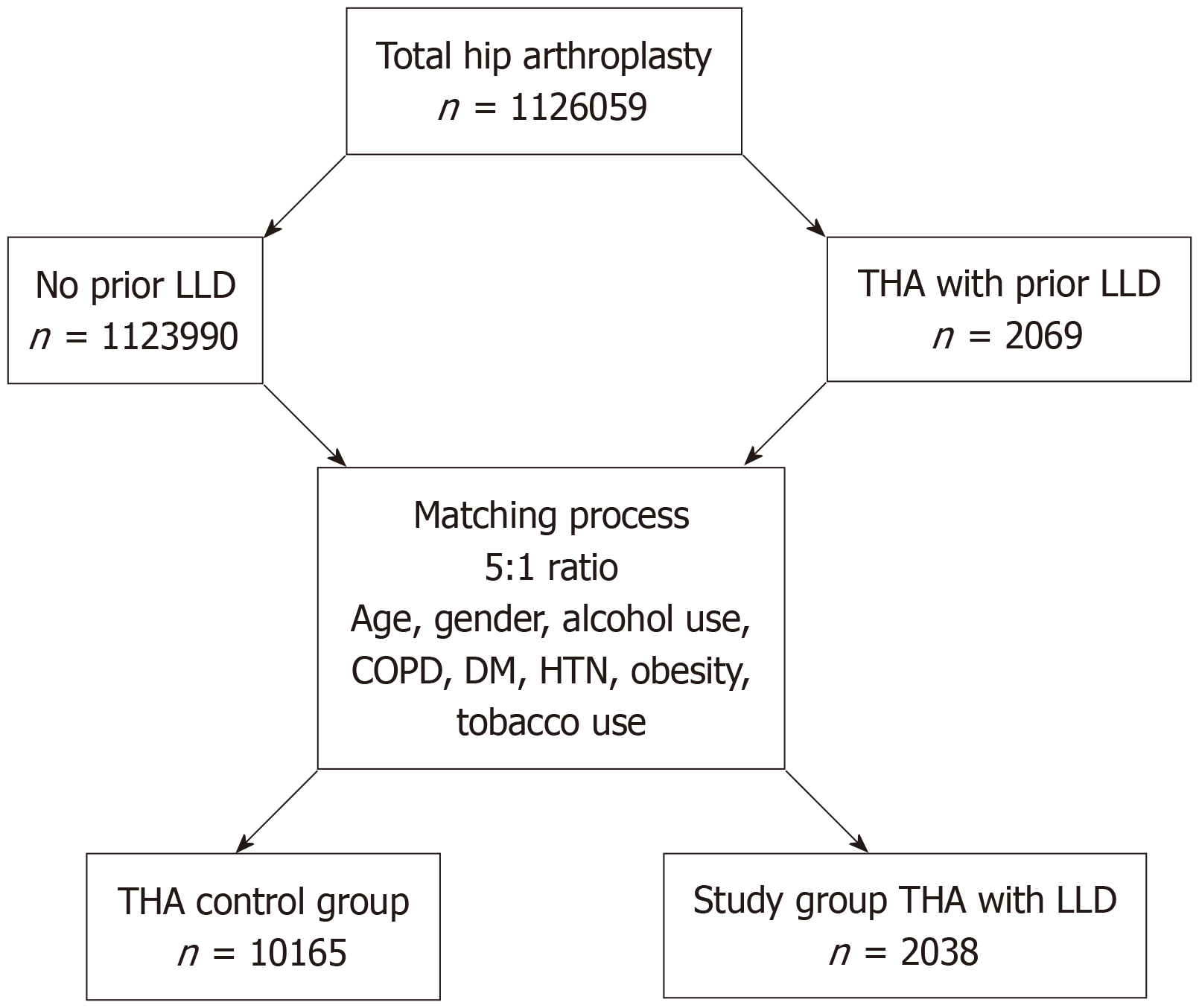
Patients with a pre-existing diagnosis of LLD were initially identified using ICD-10 codes M2175 through M21769. Those who underwent THA were identified through CPT codes CPT-27130, ICD-9 81.51, and relevant ICD-10 codes. A cohort was formed by selecting patients who had undergone THA and had a previous diagnosis of LLD. LLD patients undergoing THA were matched in a 1:5 ratio with THA patients without an LLD diagnosis based on demographic and comorbidity variables including age, gender, alcohol use, tobacco use, diabetes mellitus, chronic obstructive pulmonary disease, obesity, and hypertension. Following the inclusion and matching process, a total of 2038 patients with LLDs were successfully matched to 10165 control patients. The outcomes of this matching procedure demonstrated no statistically significant differences between the groups in terms of age, gender, and comorbidity burdens (Figure 1 and Table 1).
| Patient demographics | Leg length discrepancy, n = 2038 | Control, n = 10165 | P value |
| Age (mean ± SD) | 62.5 ± 13.0 | 62.6 ± 12.9 | 0.805 |
| Gender | 1 | ||
| Female | 1163 (57.1) | 5802 (57.1) | |
| Male | 875 (42.9) | 4363 (42.9) | |
| Comorbidity | |||
| Alcohol use | 203 (10.0) | 1009 (10.0) | 0.994 |
| COPD | 622 (30.5) | 3103 (30.5) | 1 |
| Diabetes mellitus | 700 (34.3) | 3494 (34.3) | 1 |
| Hypertension | 1546 (75.9) | 7724 (75.9) | 0.925 |
| Obesity | 929 (45.6) | 4633 (45.6) | 1 |
| Tobacco use | 901 (44.2) | 4499 (44.2) | 0.987 |
The primary outcomes included postoperative falls, 2-year prosthetic complications (dislocation, mechanical loosening, periprosthetic fracture, and fibrosis), length of hospital stay, 90-day readmission rates, and time from baseline procedure to revision THA.
Continuous variables were expressed as means ± SD, while categorical variables were presented as frequencies and percentages, as applicable. Patient age differences were evaluated using Student's t-test, and discrepancies in length of stay (LOS) and time to revision were assessed using Welch's t-tests. χ2 tests were employed to examine variations in patient gender and comorbidities. A logistic regression model was constructed to determine odds ratios (ORs) and 95% confidence intervals (95%CIs) for the influence of prior LLD diagnosis on fall rates, readmission rates, and implant-related complications. All statistical analyses were conducted using R, version 4.2.1 software (R Foundation for Statistical Computation, Vienna, Austria). Statistical significance was established at an alpha level below 0.05.
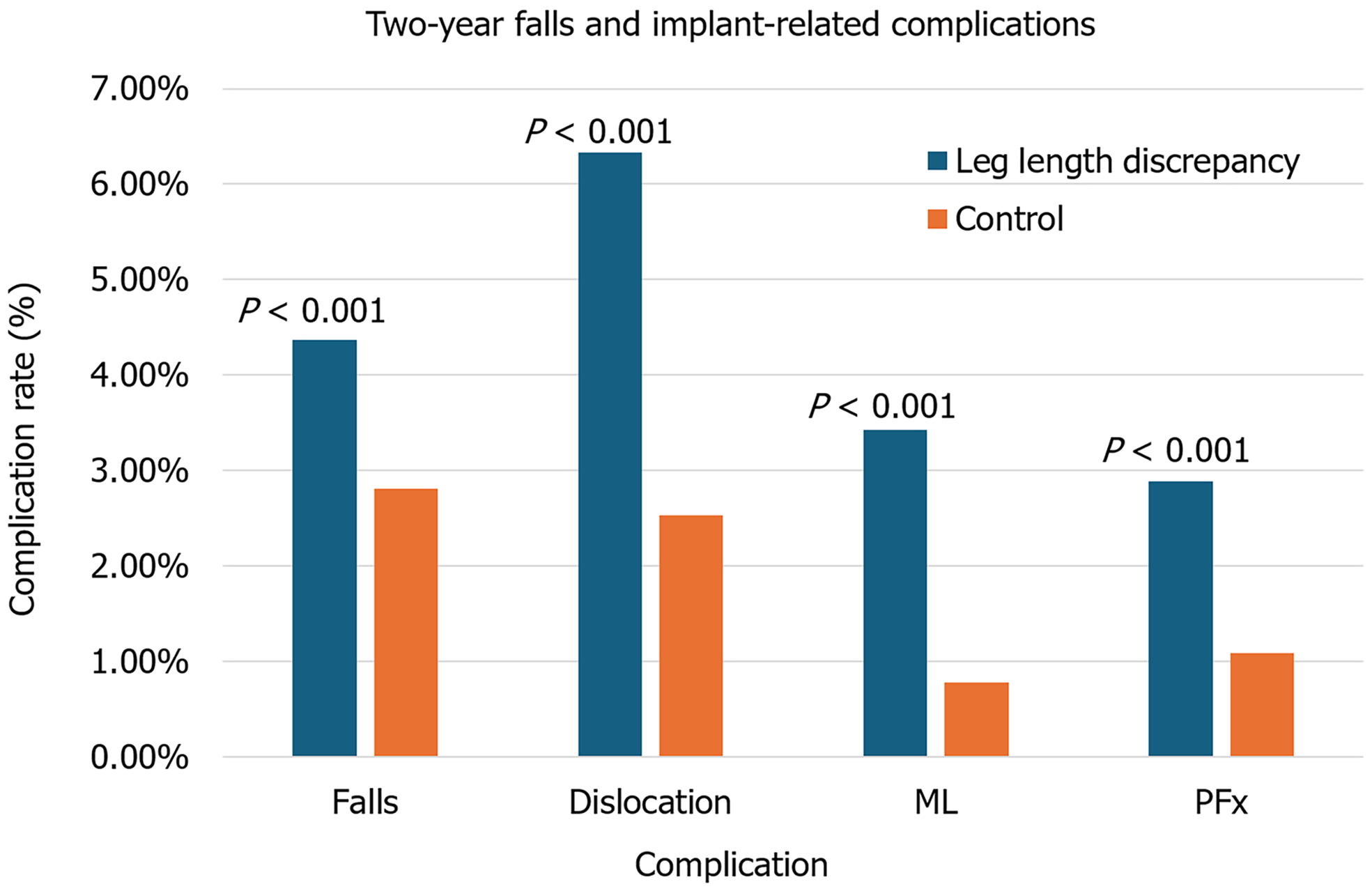
Fall rates within 2 years postoperatively were significantly higher in the LLD group compared to the control group (OR = 1.58; 95%CI: 1.24-2.01; P < 0.001). The odds of each 2-year implant-related complication evaluated were more in the LLD group. The highest increase in odds was with mechanical loosening (OR = 4.58; 95%CI: 3.28-6.29; P < 0.001), followed by periprosthetic fracture (OR = 2.70; 95%CI: 1.96-3.72; P < 0.001), and dislocation (OR = 2.61; 95%CI: 2.10-3.24; P < 0.001; Table 2 and Figure 2).
| Complication | Leg length discrepancy (%) | Control (%) | OR | 95%CI | P value |
| Falls | 4.37 | 2.81 | 1.58 | 1.24-2.01 | < 0.001 |
| DL | 6.33 | 2.53 | 2.61 | 2.10-3.24 | < 0.001 |
| ML | 3.43 | 0.78 | 4.54 | 3.28-6.29 | < 0.001 |
| PFx | 2.89 | 1.09 | 2.70 | 1.96-3.72 | < 0.001 |
There was no notable variance in hospital readmissions within the 90-day postoperative period between the cohorts under investigation (7.75% vs 7.02%, P = 0.244). Additionally, the in-hospital LOS was significantly higher in the LLD group compared to the control group (3.1 days vs 2.8 days, P = 0.034; Table 3). The prevalence of revision THA was 6.72% in the LLD group, and 3.48% in the matched-control group. The mean time from baseline procedure to revision surgery was significantly decreased in the LLD group (225 ± 309 days) when compared to the control group (544 ± 758 days; P < 0.001; Table 4).
| Utilization | Leg length discrepancy | Control | OR | 95%CI | P value |
| Readmission (%) | 7.75 | 7.02 | 1.11 | 0.93-1.33 | 0.244 |
| Length of stay (day) | 3.1 ± 3.4 | 2.8 ± 2.6 | 0.034 |
| Utilization | Leg length discrepancy | Control | P value |
| Time to revision (day) | 225 ± 309 | 544 ± 758 | < 0.001 |
In this study, patients undergoing THA with prior LLD demonstrated significantly higher rates of falls at the 2-year postoperative mark, increased odds of implant complications, extended LOS, and markedly earlier revision times compared to the patients without a prior LLD diagnosis. The documented rise in fall incidences among this patient cohort is likely multifactorial in nature. Specifically, individuals with leg length asymmetry tend to exhibit asymmetrical postural control and diminished stability during weight-bearing activities such as standing and walking[10,11]. This phenomenon can be elucidated by a variety of compensatory mechanisms that induce alterations in hip, pelvis, and trunk angulation, resulting in biomechanical stress[12]. These biomechanical changes cascade to provoke muscle weakness and asymmetry, which in turn exacerbates instability, thereby increasing the propensity for falls[13]. Moreover, alterations in proprioceptive feedback from the leg and hip further contribute to this instability. Following THA and adequate correction of LLD, there may be a potential period of proprioceptive adjustment to the evenly lengthened limb, leading to an increased risk of falls[14].
Patients with LLD before THA had notably higher odds of experiencing implant-related complications within two years post-surgery. Achieving optimal alignment and stability is paramount, yet it presents challenges in this particular patient group. Insufficient limb length assessment before THA can leave LLD unaddressed, contributing to biomechanical failures like instability, dislocation, premature wear, and component loosening[14,15]. Additionally, individuals with LLD commonly experience soft tissue imbalances, leading to laxity in the surrounding tissues due to leg shortening. This condition increases the likelihood of hip dislocation and reduces the longevity of implants[16]. In addition, it is possible that performing a THA with LLD can increase surgical times and result in increased postoperative pain.
The rise in hospital LOS may stem from the heightened complexity of the surgical procedure, necessitating additional steps for achieving precise leg length alignment. Extra procedural measures could result in increased blood loss and insufficient bone regeneration[2,14]. Additionally, deep tissue infection is a complication that can arise, further contributing to the extended length of hospital stay[17]. Patients with LLD post-THA, depending on severity, can require more intensive and specialized rehabilitation. This includes prolonged care to address gait abnormalities, restore balance, and regain muscular strength to adapt to the new leg length[2,13,18].
Finally, patients with diagnosed LLD who underwent THA had a significantly reduced timeframe for revision surgery. Descamps et al[19] similarly reported this finding, identifying LLD as a primary cause for revision THA. This could result from the compounded factors of heightened fall risk and increased implant complications, as previously discussed. Revision surgery leads to higher 30-day mortality, postoperative complications, and increased procedural cost[14,19]. Consequently, the implications of these findings underscore the critical importance of addressing LLD preoperatively to mitigate these adverse outcomes.
This study sheds light on the impact of pre-existing LLD on various outcomes following THA, however, several limitations must be considered. Primarily, a retrospective study is limited to statements of causality between LLD and the observed outcomes. Secondly, the PearlDiver Database is reliant upon proper coding to obtain diagnoses and procedures. Any errors in coding introduce a potential collection bias of the sample[18]. Additionally, the study design lacks information on the degree and cause of LLD, the time between diagnosis and surgery, and which leg with the discrepancy underwent the operation. However, this study’s strength lies in querying over 157 million patient files via PearlDiver, granting it substantial statistical power. To our knowledge, it’s the inaugural study examining how preoperative LLD impacts outcomes and complications post-THA.
Patients undergoing THA with LLD exhibit markedly elevated rates of falls, increased odds of prosthetic complications, prolonged hospitalization, and earlier revision timelines. Considering these implications, assessing limb length before surgery becomes crucial to enhance surgical planning and perioperative management, thereby mitigating associated risks. These results underscore the necessity for forthcoming prospective studies of higher caliber aimed at a deeper comprehension of the impact of limb length discrepancy preceding THA.
| 1. | Tipton SC, Sutherland JK, Schwarzkopf R. The Assessment of Limb Length Discrepancy Before Total Hip Arthroplasty. J Arthroplasty. 2016;31:888-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Vogt B, Gosheger G, Wirth T, Horn J, Rödl R. Leg Length Discrepancy- Treatment Indications and Strategies. Dtsch Arztebl Int. 2020;117:405-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | Hardwick-Morris M, Wigmore E, Twiggs J, Miles B, Jones CW, Yates PJ. Leg length discrepancy assessment in total hip arthroplasty: is a pelvic radiograph sufficient? Bone Jt Open. 2022;3:960-968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 4. | Sato R, Hamada H, Uemura K, Takashima K, Ando W, Takao M, Saito M, Sugano N. Leg length discrepancy should be assessed based on the whole length of the lower limb in patients with osteoarthritis secondary to developmental dysplasia of the hip. Bone Jt Open. 2024;5:79-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Schwartz AM, Farley KX, Guild GN, Bradbury TL Jr. Projections and Epidemiology of Revision Hip and Knee Arthroplasty in the United States to 2030. J Arthroplasty. 2020;35:S79-S85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 489] [Article Influence: 97.8] [Reference Citation Analysis (0)] |
| 6. | Mekkawy KL, Rodriguez HC, Gosthe RG, Corces A, Roche MW. Immediate Postoperative Zolpidem Use Increases Risk of Falls and Implant Complication Rates Following Total Hip Arthroplasty: A Retrospective Case-Control Analysis. J Arthroplasty. 2024;39:169-173.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Murray KJ, Azari MF. Leg length discrepancy and osteoarthritis in the knee, hip and lumbar spine. J Can Chiropr Assoc. 2015;59:226-237. [PubMed] |
| 8. | Alluri RK, Leland H, Heckmann N. Surgical research using national databases. Ann Transl Med. 2016;4:393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 213] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 9. | Passias PG, Williamson TK, Kummer NA, Pellisé F, Lafage V, Lafage R, Serra-Burriel M, Smith JS, Line B, Vira S, Gum JL, Haddad S, Sánchez Pérez-Grueso FJ, Schoenfeld AJ, Daniels AH, Chou D, Klineberg EO, Gupta MC, Kebaish KM, Kelly MP, Hart RA, Burton DC, Kleinstück F, Obeid I, Shaffrey CI, Alanay A, Ames CP, Schwab FJ, Hostin RA Jr, Bess S; International Spine Study Group. Cost Benefit of Implementation of Risk Stratification Models for Adult Spinal Deformity Surgery. Global Spine J. 2025;15:818-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Azizan NA, Basaruddin KS, Salleh AF, Sulaiman AR, Safar MJA, Rusli WMR. Leg Length Discrepancy: Dynamic Balance Response during Gait. J Healthc Eng. 2018;2018:7815451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Eliks M, Ostiak-Tomaszewska W, Lisiński P, Koczewski P. Does structural leg-length discrepancy affect postural control? Preliminary study. BMC Musculoskelet Disord. 2017;18:346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Gordon JE, Davis LE. Leg Length Discrepancy: The Natural History (And What Do We Really Know). J Pediatr Orthop. 2019;39:S10-S13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 13. | Miyagi I, Ohta M, Tamari M. Effect of Leg Length Discrepancy on Dynamic Gait Stability. Prog Rehabil Med. 2023;8:20230013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 14. | Mekkawy KL, Davis T, Sakalian PA, Pino AE, Corces A, Roche MW. Leg length discrepancy before total knee arthroplasty is associated with increased complications and earlier time to revision. Arthroplasty. 2024;6:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Dargel J, Oppermann J, Brüggemann GP, Eysel P. Dislocation following total hip replacement. Dtsch Arztebl Int. 2014;111:884-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 16. | Röder C, Vogel R, Burri L, Dietrich D, Staub LP. Total hip arthroplasty: leg length inequality impairs functional outcomes and patient satisfaction. BMC Musculoskelet Disord. 2012;13:95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Kariksiz M, Karakoyun O. Limb lengthening with one Precice nail over its capacity. Saudi Med J. 2019;40:1058-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 18. | Mekkawy KL, Saha P, Rodriguez HC, Stafford JA, Roche MW, Corces A, Gosthe RG. Planovalgus Foot Deformity in Patients Undergoing Total Hip Arthroplasty Is Associated With Increased Risk of Falls, Implant-Related Complications, and Revisions: A Case-Control Analysis. J Arthroplasty. 2024;39:2820-2823.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Descamps J, Teissier V, Graff W, Mouton A, Bouché PA, Marmor S. Managing early complications in total hip arthroplasty: the safety of immediate revision. J Orthop Traumatol. 2023;24:38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |