Published online Jul 18, 2025. doi: 10.5312/wjo.v16.i7.106041
Revised: April 13, 2025
Accepted: June 13, 2025
Published online: July 18, 2025
Processing time: 152 Days and 18.4 Hours
Spinal tuberculosis, a destructive extrapulmonary form, often causes severe deformity and neurological deficits. Surgical intervention aims to debride lesions, reconstruct stability, and correct deformities. This study evaluates a combined posterior fixation and minimally invasive anterior approach for lumbar tuber
To evaluate the clinical outcomes and radiological parameters of posterior internal fixation combined with minimally invasive anterior lesion clearance and bone graft fusion for the treatment of lumbar tuberculosis.
Clinical data from 24 patients with lumbar tuberculosis who underwent posterior pedicle screw fixation combined with minimally invasive anterior lesion clearance were analyzed. The Cobb angle, visual analog scale (VAS) score, and Frankel classification were statistically assessed preoperatively and postoperatively. Complications and bone graft fusion were also recorded.
Wounds healed in the first stage in 22 patients; one patient developed a posterior incisional sinus tract, and one experienced postoperative tuberculosis recurrence. At the final follow-up, according to the Frankel classification, there were 1, 2, and 21 cases classified as grade C, grade D, and grade E, respectively. By the last follow-up, the Cobb angle, VAS score, and erythrocyte sedimentation rate had all decreased. Both X-ray and computed tomo
Posterior pedicle screw fixation combined with minimally invasive anterior lesion clearance is an effective and safe treatment for lumbar tuberculosis.
Core Tip: This study demonstrates that posterior pedicle screw fixation combined with minimally invasive anterior lesion clearance and bone graft fusion is an effective and safe treatment for lumbar tuberculosis. Clinical outcomes showed significant improvements in Cobb angle, pain relief (visual analog scale score), and neurological function (Frankel classification), with a high rate of first-stage wound healing (22/24 cases) and successful bone fusion (average: 5.2 months). While complications were rare (one case of incisional sinus tract and one recurrence), the combined approach offers minimally invasive advantages, including reduced soft tissue damage, faster recovery, and stable spinal reconstruction. These findings support its use as a viable surgical strategy for lumbar tuberculosis, balancing radical debridement, deformity correction, and functional restoration while minimizing morbidity. Further studies with larger cohorts are warranted to validate long-term efficacy.
- Citation: Pu FF, Peng XL, Zhou FZ, Zhao XL, Yang L, Cao JQ, Wei L, Feng J, Xia P. Treatment of lumbar tuberculosis with minimally invasive anterior lesion clearance combined with posterior fixation. World J Orthop 2025; 16(7): 106041
- URL: https://www.wjgnet.com/2218-5836/full/v16/i7/106041.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i7.106041
According to the Global Tuberculosis Report released by the World Health Organization, the number of newly diagnosed tuberculosis cases worldwide reached 10.8 million in 2023, continuing an upward trend compared to the previous year. Among these, cases in China accounted for approximately 6.8% of the global total, ranking among the top three world
This retrospective case series analyzed 24 patients with lumbar tuberculosis who underwent one-stage posterior individualized pedicle screw fixation combined with anterior small-incision lesion clearance in our department between January 2016 and June 2018. The study aimed to evaluate the clinical outcomes of this surgical approach.
The inclusion criteria were as follows: (1) Diagnosis of spinal tuberculosis confirmed by typical clinical manifestations, imaging studies, laboratory tests, postoperative histological examination, and pyogenic bacteria cultures; (2) Predominant involvement of the anterior spinal column, with evident abscess formation in the spinal canal, accompanied by significant pain and neurological symptoms; and (3) Patients with lumbar tuberculosis treated with posterior pedicle screw fixation combined with minimally invasive anterior lesion clearance.
The exclusion criteria were as follows: (1) Patients with active tuberculosis; (2) Patients with non-specific spinal infec
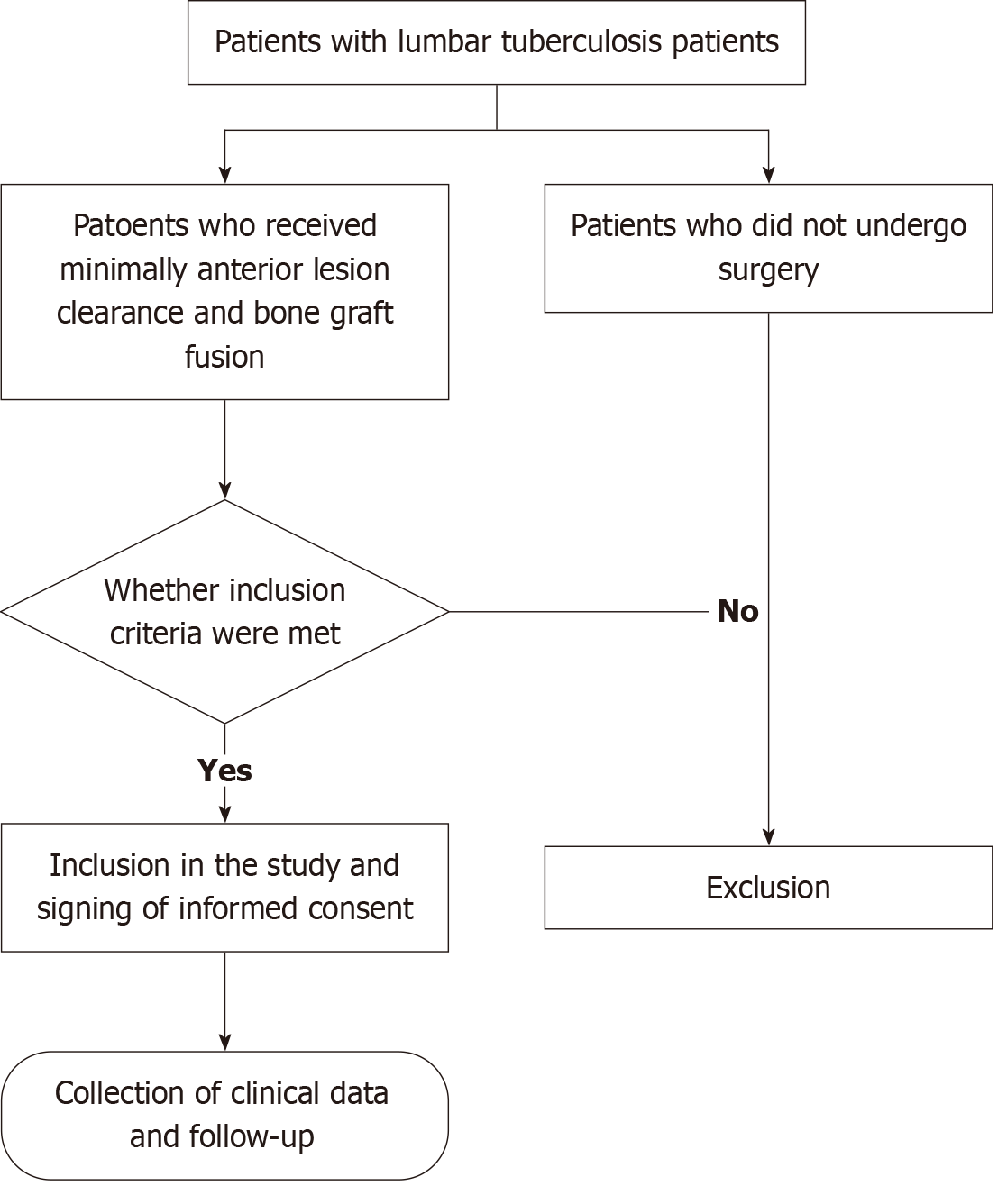
This retrospective study included 24 patients who underwent posterior internal fixation combined with minimally invasive anterior lesion clearance and bone graft fusion (Figure 1). The indications for surgery included: vertebral body destruction with necrotic bone, spinal instability, kyphotic deformity, neurological impairment, paravertebral abscess formation, severe low back pain or radicular pain, or failure of conservative treatment. The surgical approach for lesion removal was selected based on the extent of vertebral damage and the location of the abscess. The number of fixed segments and fixation strategy for the affected vertebrae were determined by lesion location, whether vertebral des
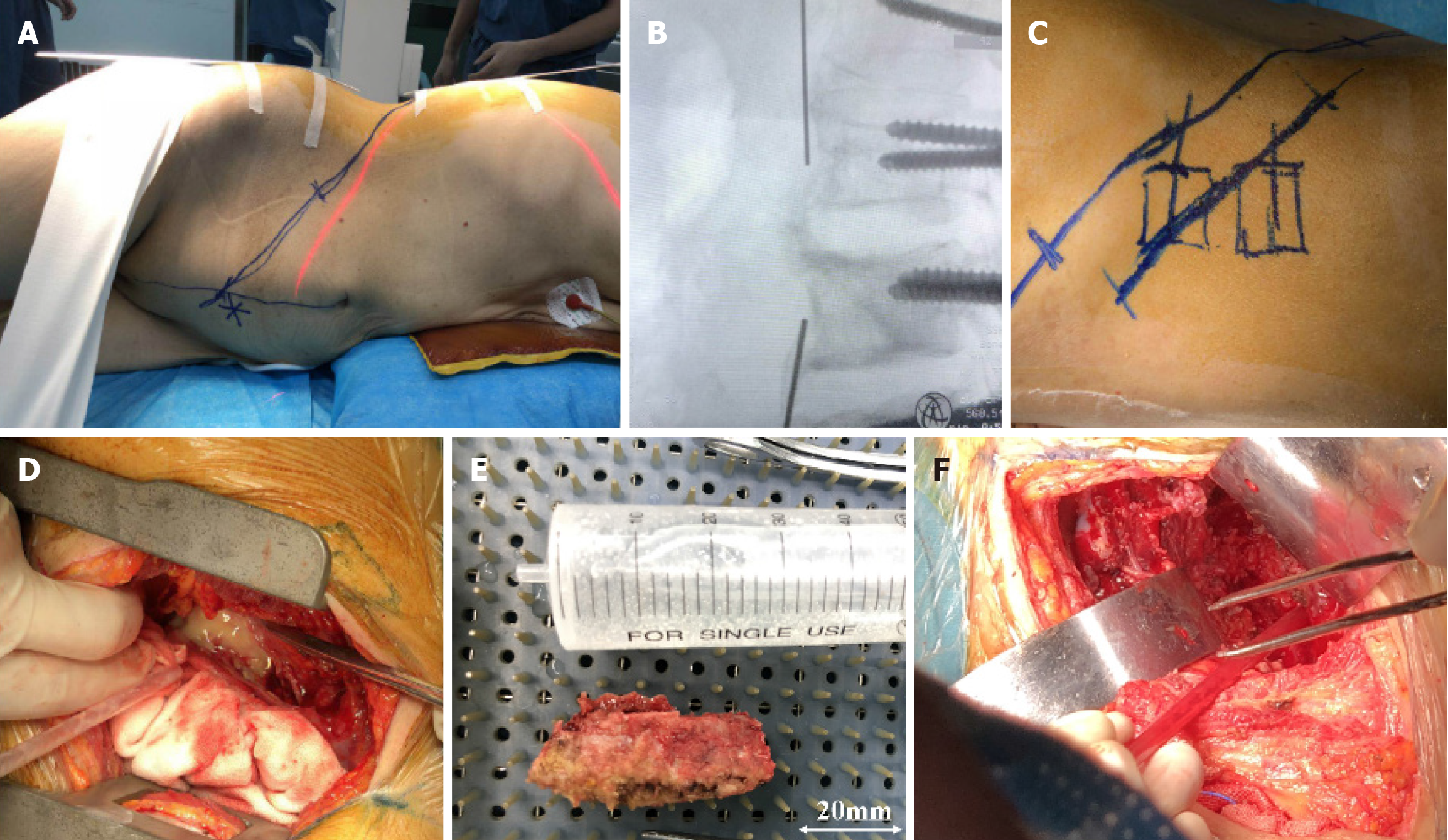
The patient was placed in a prone position, and a posterior midline incision was made, centered on the affected vertebra. The bilateral facet joints were exposed via a paravertebral muscle-splitting approach. Individual pedicle screws were inserted according to the degree of preoperative vertebral body destruction. The screw lengths ranged from 30 to 45 mm, and pedicle screws were implanted into one to two normal vertebral bodies above and below the lesion. Generally, in cases involving two vertebral bodies, two to three screws were inserted into the affected segments, and one normal vertebral body above and below received pedicle screws. For lesions involving three vertebral bodies, two to five screws were placed in the diseased segments, and one to two screws were implanted into the adjacent normal vertebrae. Kyphotic deformity was corrected using distraction and reduction through the internal fixation system. The patient was then rotated into a half-lateral position (Figure 2A). Centered on the diseased vertebra, an abdominal incision approximately 6-8 cm in length (Figure 2B and C) was made. Muscle fibers were separated bluntly, aligning the external oblique, internal oblique, and transversus abdominis muscles along the retroperitoneal space. The retroperitoneal margin was soaked in 0.9% sodium chloride solution to facilitate visualization of surrounding tissues. The abscessed tissue within the psoas major was debrided, followed by exposure of the affected vertebra. Necrotic intervertebral disc material, seque
Postoperatively, depending on the amount of fluid drained, the drainage tube was typically removed within 48-72 hours, and antibiotics were administered for 2-3 days. One week after surgery, patients were generally allowed to ambulate with the assistance of a thoracolumbar brace. During the first three months, patients were advised to minimize physical activity. Systemic nutritional support and anti-tuberculosis therapy were continued after the operation. Diagnostic evaluations-including complete blood count, erythrocyte sedimentation rate, and liver and kidney function tests-were repeated every two to four weeks during the entire course of anti-tuberculosis treatment. Routine urinalysis was per
All patients were followed up in the outpatient clinic. Frankel grading, visual analog scale (VAS) scores, and Cobb angles were recorded preoperatively, one week postoperatively, and at the final follow-up. To monitor neurological recovery and detect postoperative complications, X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) were performed every three months to assess lesion healing, bone graft fusion, and the integrity of pedicle screw fixation. The criteria for bone graft fusion proposed by Bridwell et al[7] were used to evaluate the fusion outcome. Grades I and II were considered indicative of successful bone graft fusion in this study.
Statistical analysis was performed using the SPSS version 20.0 software package. One-way analysis of variance (ANOVA) and repeated measures ANOVA were used to compare the data, and pairwise comparisons were conducted using the student-Newman-Keuls method. Categorical data were analyzed using non-parametric tests. A P value of < 0.05 was considered statistically significant.
This retrospective study included patients who underwent lumbar surgery at the Department of Spinal Surgery, Wuhan No. 1 Hospital; Wuhan Hospital of Integrated Traditional Chinese and Western Medicine; and Tongji Medical College, Huazhong University of Science and Technology, between January 2016 and June 2018. A total of 24 patients with lumbar tuberculosis-16 males and 8 females-were treated with posterior internal fixation combined with minimally invasive anterior lesion clearance and bone graft fusion. Patient ages ranged from 18 to 73 years (mean = 47.13, SD = 3.25), and the duration of disease ranged from 1 to 14 months (mean = 6.42, SD = 1.09). The clinical manifestations were as follows: all patients experienced varying degrees of lumbar pain, stiffness, flexion limitation, and restricted mobility. Seventeen patients (70.83%) presented with neurological symptoms of the lower limbs, such as numbness, weakness, diarrhea, or constipation. Seven patients (29.17%) exhibited typical tuberculosis-related symptoms, including low-grade fever, night sweats, and fatigue. Imaging studies revealed vertebral body and intervertebral disc destruction, along with paravertebral abscess formation, consistent with the diagnosis of lumbar tuberculosis. The average preoperative Cobb angle of kyphosis measured between the upper endplate of the superior vertebral body and the lower endplate of the inferior vertebral body was 15.21° ± 2.08° based on X-ray imaging. Laboratory examinations showed no significant abnormalities in hematologic indices or liver and kidney function tests. The average preoperative VAS score was 6.53 ± 1.14. Erythrocyte sedimentation rate ranged from 21 to 116 mm/h, with an average of 38.09 ± 1.17 mm/h (reference range: Adult males, 0-10 mm/h; adult females, 0-12 mm/h).
Anti-tuberculosis chemotherapy was administered with isoniazid (5-10 mg/kg/day), rifampicin (10 mg/kg/day), ethambutol (15 mg/kg/day), and pyrazinamide (25 mg/kg/day) for a duration of 2 to 4 weeks. For older patients with abnormal liver function or allergic reactions, individualized anti-tuberculosis regimens were formulated, and nutritional support was enhanced. Blood transfusion was provided to correct anemia when hemoglobin levels were below 10 g/L or serum albumin levels were below 30 g/L. The decision to proceed with surgery depended on tuberculosis symptomatology and erythrocyte sedimentation rate. The optimal timing for surgery was when symptoms were alleviated and body temperature was < 37.5 °C, hemoglobin was > 100 g/L, and erythrocyte sedimentation rate was < 60 mm/h.
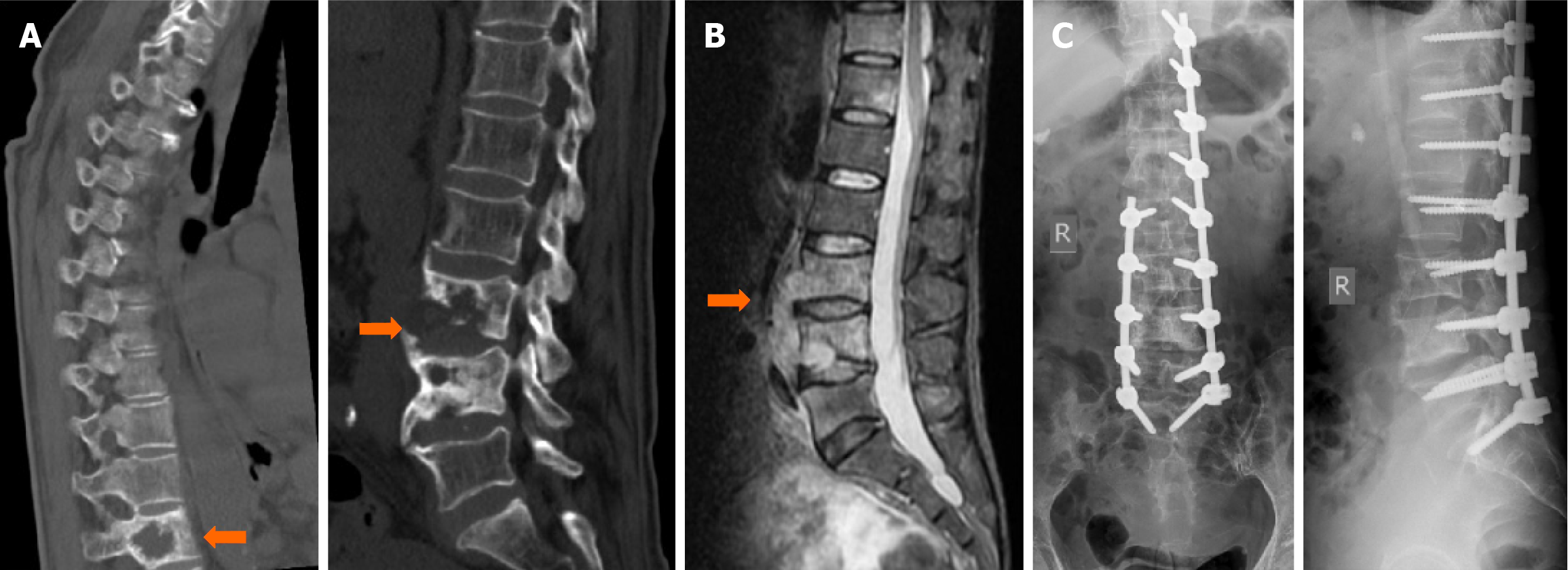
A total of 24 patients were included in the study. The operative time ranged from 1.7 to 3.4 hours, with an average of 2.2 ± 0.3 hours. Intraoperative blood loss ranged from 390 to 1180 mL, with an average of 580.0 ± 64.2 mL. There were 14 cases of single-segment fusion and 10 cases of double-segment fusion. All patients were followed postoperatively for 6 to 36 months, with an average follow-up duration of 19.25 ± 8.32 months. Primary wound healing occurred in 22 patients. One patient developed a posterior incisional sinus tract, and one experienced postoperative recurrence of tuberculosis. No cases of sinus formation, incisional hernia, cerebrospinal fluid leakage, or spinal tuberculosis recurrence were observed among the remaining patients. All systemic tuberculosis symptoms (e.g., fever, night sweats, and fatigue) resolved. At the final follow-up, Frankel classification results were as follows: 1 patient with grade C, 2 with grade D, and 21 with grade E. The mean preoperative Cobb angle of kyphosis (15.21° ± 2.08°) was significantly reduced to 4.17° ± 1.58° at the final follow-up (P < 0.05). The preoperative VAS score was 6.53 ± 1.14 and improved to 2.12 ± 0.68 at the final follow-up (P < 0.05). The erythrocyte sedimentation rate decreased from 38.09 ± 1.17 mm/h preoperatively to 9.96 ± 0.86 mm/h postoperatively (P < 0.05) (Table 1). Both X-ray and CT images confirmed bone healing. The fusion time ranged from 3 to 9 months, with a mean fusion duration of 5.2 months (Figure 3).
| Item | Cobb angle (°) | VAS score | ESR (mm/h) |
| Preoperative | 15.21 ± 2.08 | 6.53 ± 1.14 | 38.09 ± 1.17 |
| Final follow-up | 4.17 ± 1.58 | 2.12 ± 0.68 | 9.96 ± 0.86 |
| F value | 6.817 | 5.385 | 6.626 |
| P value | 0.016 | 0.030 | 0.017 |
The optimal surgical approach for lumbar tuberculosis remains a topic of ongoing debate, with various techniques offering distinct advantages and limitations[8]. The primary goals of surgical treatment are decompression of the spinal canal, thorough lesion removal, correction of spinal deformities, and reconstruction of spinal stability[9]. As the pathological damage caused by spinal tuberculosis primarily affects the vertebral body and intervertebral space, the anterior approach allows for direct visualization and complete lesion debridement, as well as anterior column support through bone grafting. When combined with posterior pedicle screw fixation, this technique may enhance the mechanical stability of the spine[10]. This, in turn, facilitates early postoperative mobilization and rehabilitation, which is why the combined approach is commonly applied in cases of lumbar tuberculosis. Patients with spinal tuberculosis often present with poor nutritional status and decreased vertebral bone mass. When anterior fixation is performed through the diseased vertebral bodies, the resulting mechanical strength is significantly lower than that achieved with posterior fixation and carries a higher risk of postoperative infection[11].
Multiple-level lumbar tuberculosis often requires long-segment fixation to maintain spinal stability. However, exce
Several studies have reported that posterior vertebral internal fixation for multi-segment spinal tuberculosis can effectively shorten the fixation length while achieving favorable clinical outcomes[17]. According to Wang et al[18], if more than 50% of normal tissue remains in the anterior and middle columns after lesion removal, pedicle screw fixation can be applied to the affected vertebra. They recommend selecting pedicle screws only when the bone in the lateral third of the medial and posterior columns of the diseased vertebra is intact. If one of the three spinal columns is compromised, internal fixation may not be appropriate. In the present study, two patients exhibited severe destruction of the vertebral middle column and were therefore unsuitable for pedicle screw fixation. The remaining patients successfully underwent screw implantation. While posterior fixation provides mechanical stability, it may be insufficient for managing anterior abscesses located in areas such as the iliac fossa, groin, or buttocks. In such cases, supplemental anterior debridement may be necessary[19]. We believe that thorough preoperative imaging evaluation can significantly reduce the incidence of screw exposure following lesion removal.
Endoscopic techniques have gained increasing attention due to advantages such as reduced blood loss and faster recovery. However, their application is limited by small correction angles and restricted operative fields[20]. An alter
Overall, the small anterior abdominal incision was associated with less damage to the affected vertebrae, adjacent structures, and vascular anatomy; reduced postoperative pain; and expedited recovery. However, this study had several limitations. First, the sample size was relatively small. Second, there was no comparative evaluation involving rando
This study demonstrates that individualized pedicle screw fixation, based on the degree of vertebral damage, combined with anterior small-incision lesion removal and bone grafting, is an effective and safe treatment for lumbar tuberculosis.
| 1. | Peng X, Pu F, Zhou F, Dai X, Xu F, Wang J, Feng J, Xia P. Has-miR-30c-1-3p inhibits macrophage autophagy and promotes Mycobacterium tuberculosis survival by targeting ATG4B and ATG9B. Sci Rep. 2025;15:10240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Qiu J, Peng Y, Qiu X, Gao W, Liang T, Zhu Y, Chen T, Hu W, Gao B, Deng Z, Liang A, Huang D. Comparison of anterior or posterior approach in surgical treatment of thoracic and lumbar tuberculosis: a retrospective case-control study. BMC Surg. 2022;22:161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Liao Y, Ye R, Tang Q, Tang C, Ma F, Luo N, Zhong D. Is It Necessary to Perform the Second Surgery Stage of Anterior Debridement in the Treatment of Spinal Tuberculosis? World Neurosurg. 2020;134:e956-e967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Liu Z, Li W, Xu Z, Wang X, Zeng H. One-stage posterior debridement, bone grafting fusion, and mono-segment vs. short-segment fixation for single-segment lumbar spinal tuberculosis: minimum 5-year follow-up outcomes. BMC Musculoskelet Disord. 2020;21:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Zhong Y, Yang K, Ye Y, Huang W, Liu W, Luo J. Single Posterior Approach versus Combined Anterior and Posterior Approach in the Treatment of Spinal Tuberculosis: A Meta-Analysis. World Neurosurg. 2021;147:115-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Liu Z, Zhang P, Li W, Xu Z, Wang X. Posterior-only vs. combined posterior-anterior approaches in treating lumbar and lumbosacral spinal tuberculosis: a retrospective study with minimum 7-year follow-up. J Orthop Surg Res. 2020;15:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976). 1995;20:1410-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 384] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 8. | Liu J, Wan L, Long X, Huang S, Dai M, Liu Z. Efficacy and Safety of Posterior Versus Combined Posterior and Anterior Approach for the Treatment of Spinal Tuberculosis: A Meta-Analysis. World Neurosurg. 2015;83:1157-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Bian Z, Gui Y, Feng F, Shen H, Lao L. Comparison of anterior, posterior, and anterior combined with posterior surgical treatment of thoracic and lumbar spinal tuberculosis: a systematic review. J Int Med Res. 2020;48:300060519830827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Ma S, Zhou Z, Yu H, Zhong J, Xiong J, Xu J, Deng W, Cao K. Posterior Approach With Osteotomized Debridement Versus Combined Anterior and Posterior Approach in Treating Thoracolumbar Tuberculosis: A Retrospective Cohort Study. Global Spine J. 2024;14:812-820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 11. | Ruparel S, Tanaka M, Mehta R, Yamauchi T, Oda Y, Sonawane S, Chaddha R. Surgical Management of Spinal Tuberculosis-The Past, Present, and Future. Diagnostics (Basel). 2022;12:1307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 12. | Xu Z, Wang X, Zhang Z, Jiang D, Jia R, Zhang Y. A comparison of three bone graft struts for interbody fusion using a posterior approach for lower lumbar spinal tuberculosis in adults: a midterm follow-up study. BMC Musculoskelet Disord. 2022;23:590. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Liu Z, Zhang P, Zeng H, Xu Z, Wang X. A comparative study of single-stage transpedicular debridement, fusion, and posterior long-segment versus short-segment fixation for the treatment of thoracolumbar spinal tuberculosis in adults: minimum five year follow-up outcomes. Int Orthop. 2018;42:1883-1890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Pu F, Feng J, Yang L, Zhang L, Xia P. Misdiagnosed and mismanaged atypical spinal tuberculosis: A case series report. Exp Ther Med. 2019;18:3723-3728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Kumaran SP, Thippeswamy PB, Reddy BN, Neelakantan S, Viswamitra S. An Institutional Review of Tuberculosis Spine Mimics on MR Imaging: Cases of Mistaken Identity. Neurol India. 2019;67:1408-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 16. | Wang W, Fan Z, Zhen J. MRI radiomics-based evaluation of tuberculous and brucella spondylitis. J Int Med Res. 2023;51:3000605231195156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 17. | Zhong Y, Huang Y, Chen Z, Liu Z, Liu W, Luo J, Ye Y. Structural Versus Nonstructural Bone Grafting Via the Posterior Approach in the Treatment of Thoracic and Lumbar Tuberculosis: A Systematic Review and Meta-Analysis. World Neurosurg. 2023;174:42-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Wang Z, Ge Z, Jin W, Qiao Y, Ding H, Zhao H, Lin Z, Chen J, Yang W. Treatment of spinal tuberculosis with ultrashort-course chemotherapy in conjunction with partial excision of pathologic vertebrae. Spine J. 2007;7:671-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Wu W, Li Z, Lin R, Wang S, Lin J. Single-stage posterior-only debridement, decompression and interbody fusion for the treatment of thoracolumbar spinal tuberculosis complicated with psoas abscesses. BMC Surg. 2021;21:84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Abudurexiti T, Haibier A, Yusufu A, Shoukeer K, Lin H. Retrospective Analysis of the Efficacy and Safety of Endoscopic Spinal Tuberculosis Focus Removal versus Posterior Pedicle Lesion Removal, Bone Grafting, and Internal Fixation Combined with Drug Chemotherapy for Thoracolumbar Tuberculosis. Infect Drug Resist. 2024;17:733-748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 21. | Ma J, Zhang Z, Lan J, Tian J, Chen F, Miao J. The treatment of tuberculosis in the upper thoracic spine using the small incision technique through the third rib. Front Surg. 2023;10:1236611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 22. | Srivastava SK, Aggarwal RA, Bhosale SK, Roy K, Nemade PS. The Versatile Approach: A Novel Single Incision Combined with Anterior and Posterior Approaches for Decompression and Instrumented Fusion to Treat Tuberculosis of the Thoracic Spine. Asian Spine J. 2017;11:294-304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |