Published online Jun 18, 2025. doi: 10.5312/wjo.v16.i6.107753
Revised: April 10, 2025
Accepted: May 15, 2025
Published online: June 18, 2025
Processing time: 82 Days and 3 Hours
Thoracic ossification of the posterior longitudinal ligament (T-OPLL) is caused by the ossified posterior longitudinal ligament occupying space in the spinal canal, which causes compression of the thoracic spinal cord. Surgical treatment is di
A case of severe multi-segmental T-OPLL treated with thoracic anterior control
This case report suggests that TACAF is feasible for the treatment of long-segment T-OPLL, and has the advantages of low risk and reduced trauma. However, this operation still needs to be verified by clinical research with a larger sample size.
Core Tip: Thoracic ossification of the posterior longitudinal ligament, especially long-segment lesions, has always been a difficult problem in clinical work. The unique anatomical structure of thoracic vertebra leads to high risk and difficulty in surgical treatment. By loosening the intervertebral discs above and below the diseased segment, removing the lamina behind the diseased segment and pushing the diseased segment forward, a good therapeutic effect can be achieved and the surgical risk can be reduced.
- Citation: Jin XY, Wang HZ, Yang K, Bao Y, Wang Y, Ben XL, Sun HY. Thoracic anterior controllable antedisplacement fusion for thoracic ossification of the posterior longitudinal ligament: A case report. World J Orthop 2025; 16(6): 107753
- URL: https://www.wjgnet.com/2218-5836/full/v16/i6/107753.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i6.107753
Thoracic ossification of the posterior longitudinal ligament (T-OPLL) is an important cause of thoracic spinal stenosis and spinal cord compression injury. Although the incidence rate is not high, it is difficult to treat due to its anatomical characteristics, and the high risk of spinal cord injury and even paraplegia, and there are many complications, which has resulted in treatment difficulties at present[1,2]. Patients with T-OPLL may have no symptoms in the early stage. Fo
At present, the surgical treatment of T-OPLL is generally divided into posterior decompression and anterior de
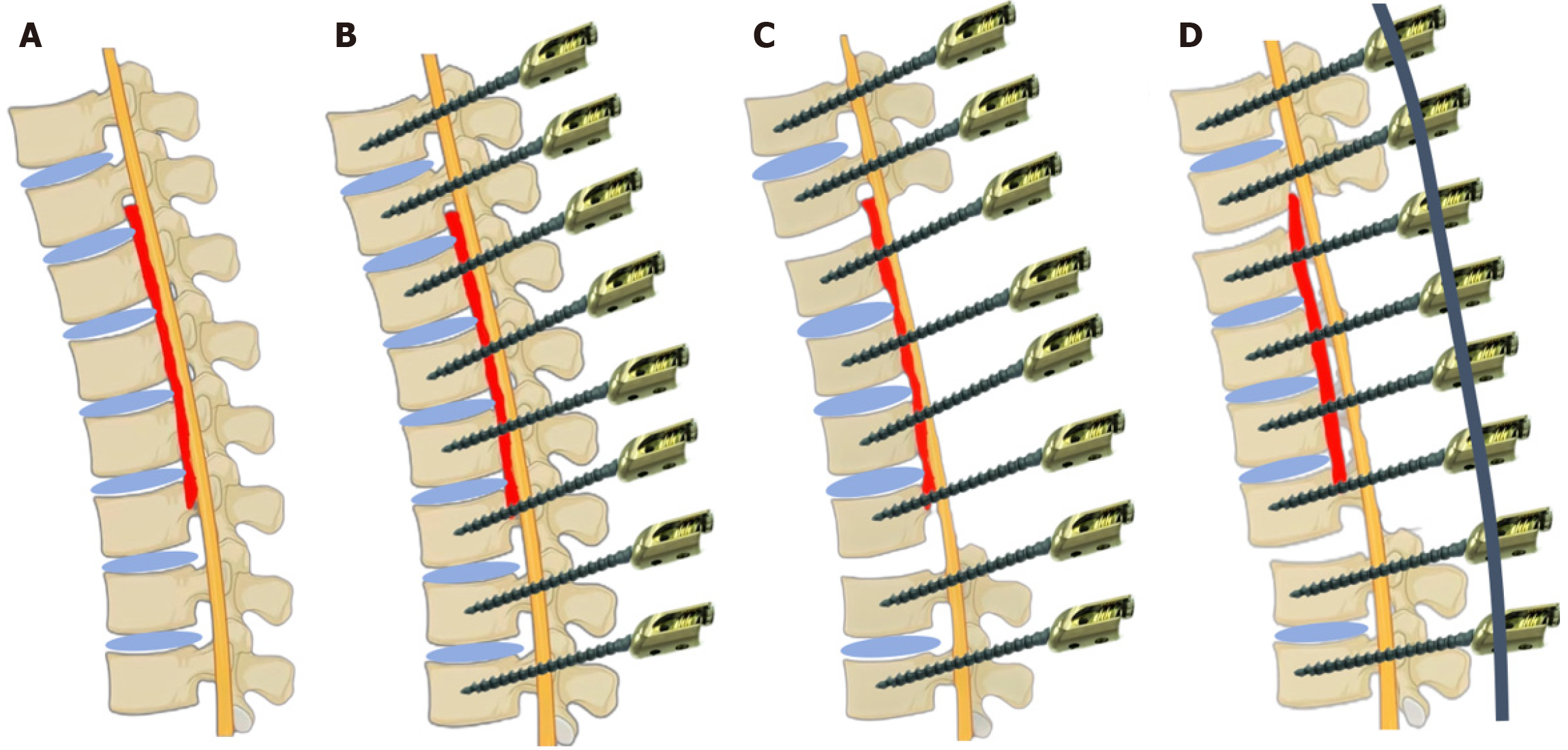
Recently, our team used TACAF to treat a case of severe T-OPLL by cutting off the thoracic vertebral lamina of the corresponding ossified segment, and removing the intervertebral disc between the cephalad and caudal normal/ossified segments. This was followed by cutting off all the ribs on both sides of the ossified segment, and using the nail and rod system to push forward several consecutive thoracic vertebral bodies together with the ossified posterior longitudinal ligament. This not only directly decompressed the spinal cord, but the huge risk of directly cutting off the ossified longitudinal ligament was avoided, which greatly reduced the difficulty of the operation and improved the safety.
A 45-year-old female was admitted to the hospital because of weakness of both lower limbs for one month, aggravated with numbness for 10 days.
The patient experienced lower limbs weakness one month ago, which became worse and accompanied by numbness 10 days later.
The patient was physically healthy.
The patient denied a family history of a similar disease.
The spine was centered and there was a physiological curvature. There was no pressure pain and percussion pain of cervical vertebra, the Spurling test and the bilateral Eaton test were negative, and bilateral Lasegue test was 70°. Muscle strength of both upper limbs was normal, tendon reflexes in both upper limbs were normal, and Hoffmann was negative in both hands. Muscle strength in both lower limbs decreased, deep and shallow skin sensations were present in both lower limbs, muscle tension in both lower limbs also increased, tendon reflexes in both lower limbs were hyperactive, the left side was severe, and bilateral ankle clonus was negative.
Not obviously special.
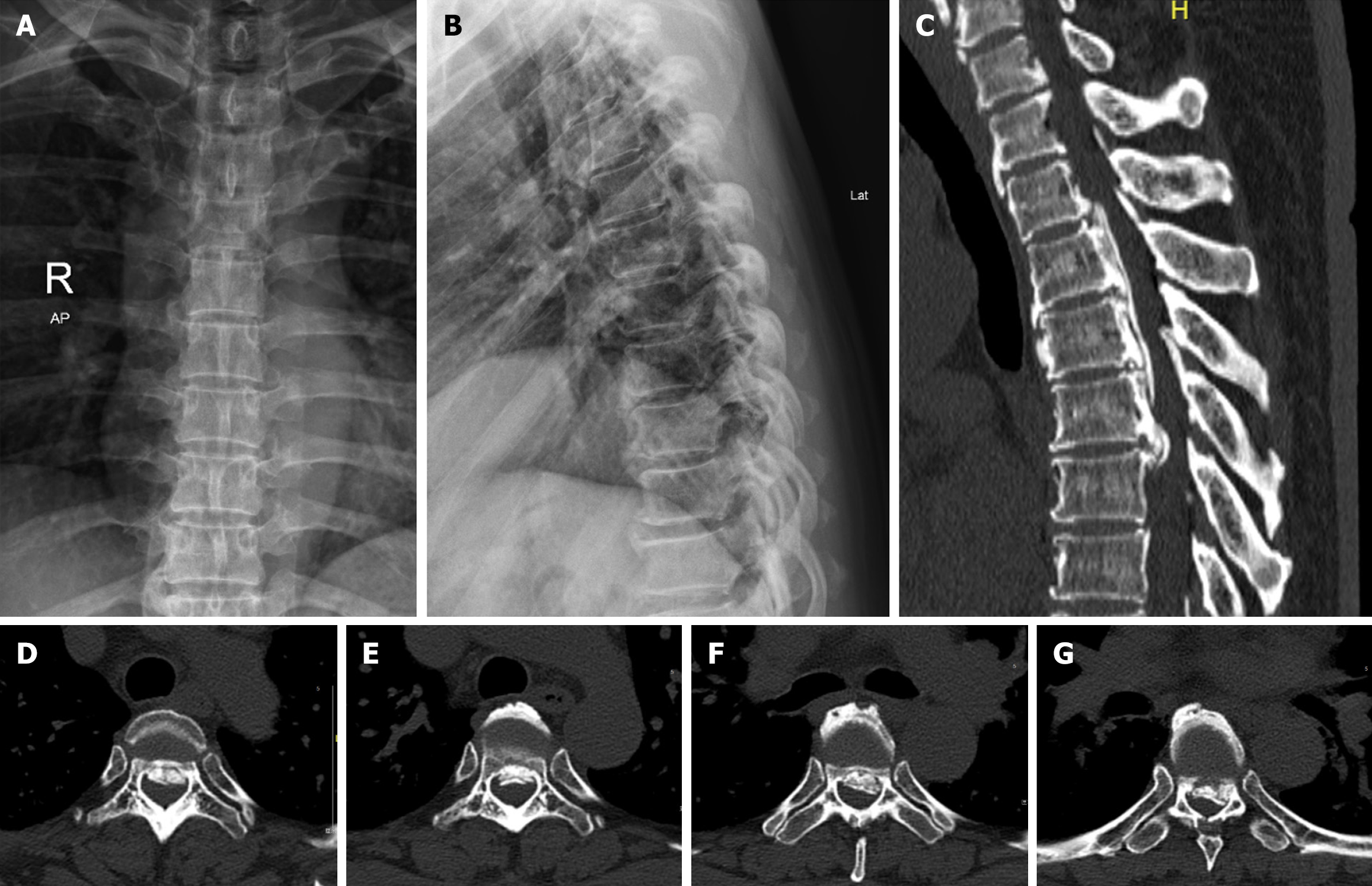
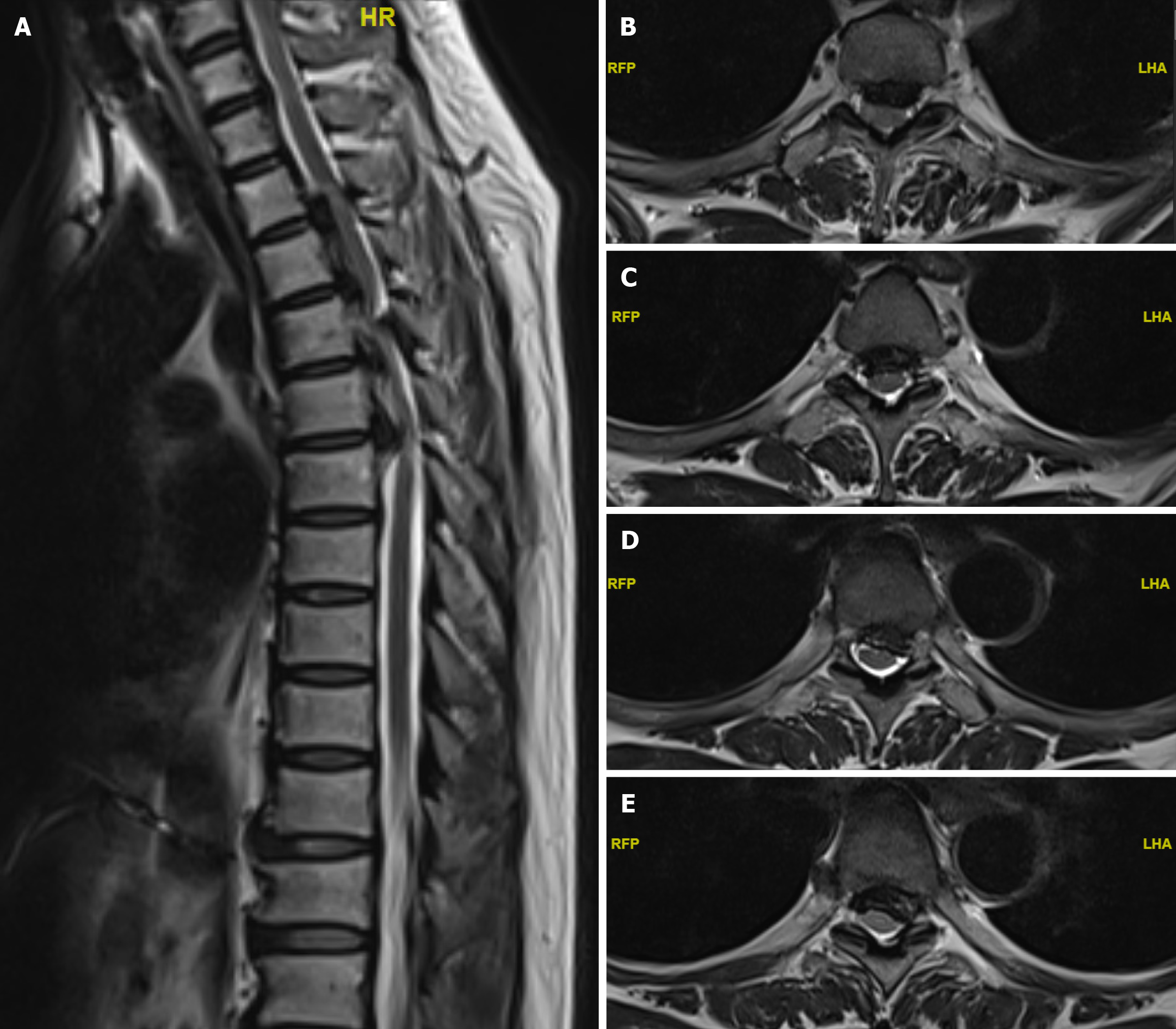
Computed tomography (CT) and magnetic resonance imaging (MRI) examination of the thoracic vertebra showed that the posterior longitudinal ligament of T2-6 vertebra was ossified, the area of spinal canal was decreased by 77.2%, the spinal canal was severely narrowed and the spinal cord was compressed. Blood tests, electrocardiography and color Doppler echocardiography showed no obvious abnormalities. Dual-energy X-ray absorptiometry showed no obvious osteoporosis. The preoperative modified-Japanese Orthopaedic Association score (m-JOA) was 4 points[15].
Thoracic ossification of the posterior longitudinal ligament.
Imaging examination included orthoposition and lateral position of the thoracic vertebra digital radiography, CT and 3D reconstruction of thoracic vertebra, and MRI of thoracic vertebra (Figures 1 and 2). According to the CT and three-dimensional reconstruction data of thoracic vertebra, the left and right diameter, anterior and posterior diameter and ossified segment range of the ossified posterior longitudinal ligament were measured to guide movement of the vertebral segment forward and the moving distance. In addition, the pedicle width was measured to predict the appropriate specifications of screws and guide pedicle screw implantation. The compression segment and degree of spinal cord were judged by thoracic vertebra MRI, and the surgical segment was further defined.
The patient was placed in the prone position after general anesthesia. The surgical steps were as follows: (1) Conventional disinfection towel laying; (2) Expose and place nails: After positioning with the C-arm machine, a longitudinal incision approximately 20 cm in length was made from T1 to T8, and the skin, subcutaneous tissue and deep fascia were cut, and the paraspinal muscles were stripped to the outside of the articular process along the spinous process to fully expose the vertebral lamina. Bipolar electrocoagulation and dry gauze were used to stop bleeding. The upper edge of the transverse process of T1-8 vertebral body and the outer edge of the vertebral plate were exposed, the surrounding soft tissues and ligaments were cleared, the area was located according to the "Dick" needle insertion method, the surrounding integrity was assessed, the depth was measured, drill holes were made and 16 pedicle screws were placed in T1-8, of which the screws on both sides of T3-6 were reserved with a height of approximately 5 mm and not screwed into the pedicle. The C-arm machine perspective showed that the screws were in good positions; (3) Excision of lamina: An ultrasonic osteotome was used to cut the laminae on both sides of T3-6 along the lateral edge of the laminae, the cut bone groove was enlarged, a nerve stripper was used to explore and peel the laminae and dura mater, a lamina rongeur was used to separate the overgrown bone and ligament around, and the laminae were gently prized open, and the nerve stripper was used to help peel the dura mater until the posterior laminae of T3-6 were completely removed, exposing the dura mater of the corresponding segment, which showed that the spinal cord floated well. The posterior fibrous ring of T2-3 and T6-7 segments were cut, and a small amount of nucleus pulposus tissue was taken out with nucleus pulposus forceps, and the intervertebral disc was released; (4) Free the ribs: An ultrasonic osteotome and sharp-nosed rongeur were used to cut the bilateral transverse costal joints of T3-T6 and the bilateral 3rd-6th ribs, and the intervertebral discs of T2-3 and T6-7 were carefully removed with curettage and nucleus pulposus forceps until the T3-6th segment lost its stability; (5) Moving the vertebral ossification complex forward: The connecting rod of appropriate length was placed, the nuts of the head and tail segments were synchronously and slowly tightened, and a titanium rod was used as the support point to push the ossified complex of T3-6 segment to the ventral side. The nut was tightened after pressurization until the whole T3-6 four-segment vertebral body moved forward by about 4 mm, and bleeding was fully stopped after washing. The sharp-nosed osteotome was used to bite off part of the single-layer cortical bone of the transverse process of the vertebral body to create a good bone grafting site, and the bitten autogenous bone was placed between the transverse processes on both sides for full bone grafting and fusion (Figure 3); and (6) Hemostasis and suture: Alternately bipolar electrocoagulation and a gelatin sponge were used to stop bleeding, a negative pressure drainage tube was left in the incision, the incision was sutured layer by layer and wrapped with a sterile dressing. Intraoperative bleeding was 800 mL and autologous blood transfusion was 656 mL. After the operation, the patient was safely returned to the ward.
After operation, the patients were given symptomatic treatment such as detumescence and analgesia, prevention of infection, anti-DVT of lower limbs and nutritional support. Wear thoracic brace for 3 months, ensure bone grafting and fusion, and exercise limb function at an early stage.
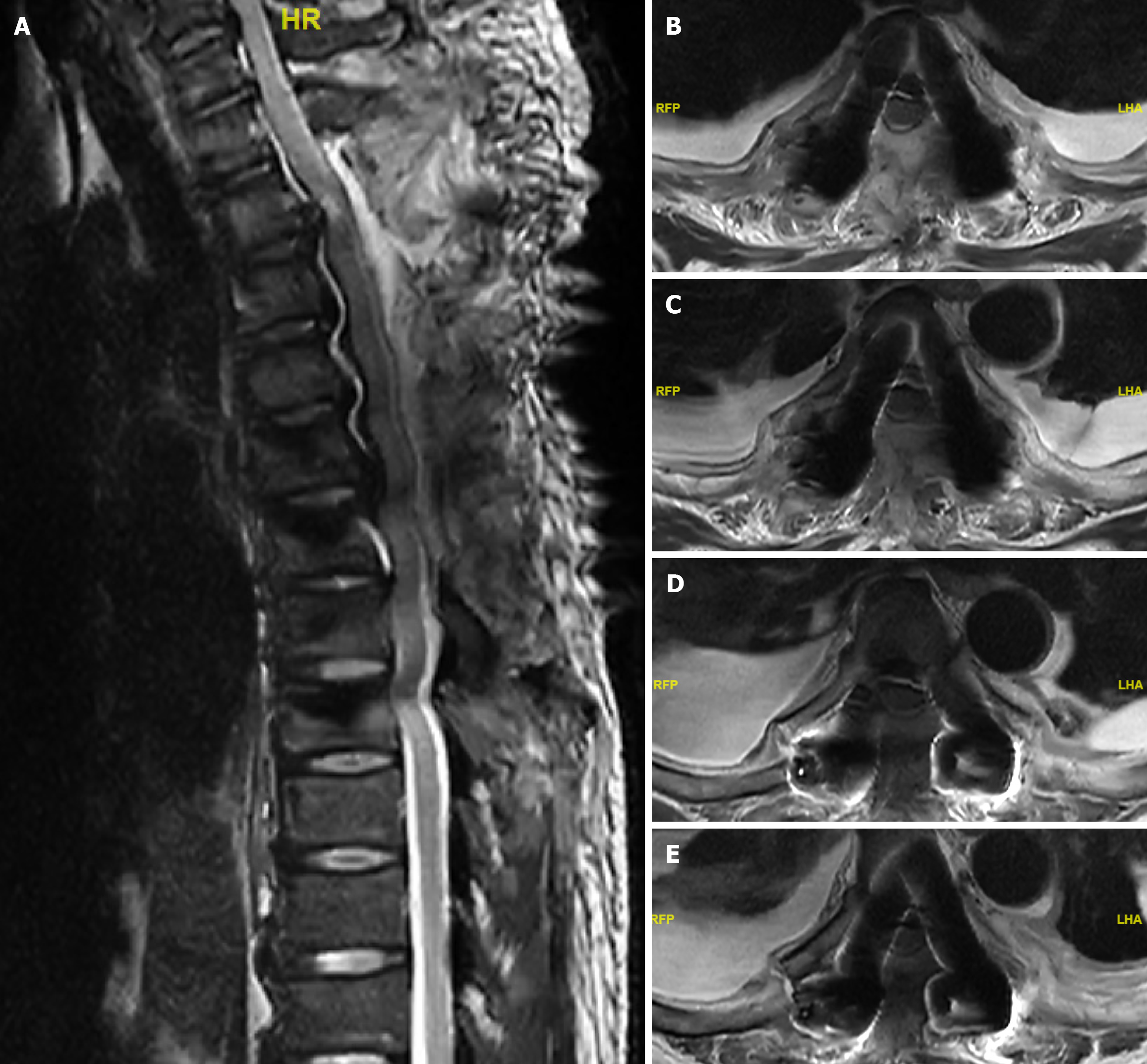
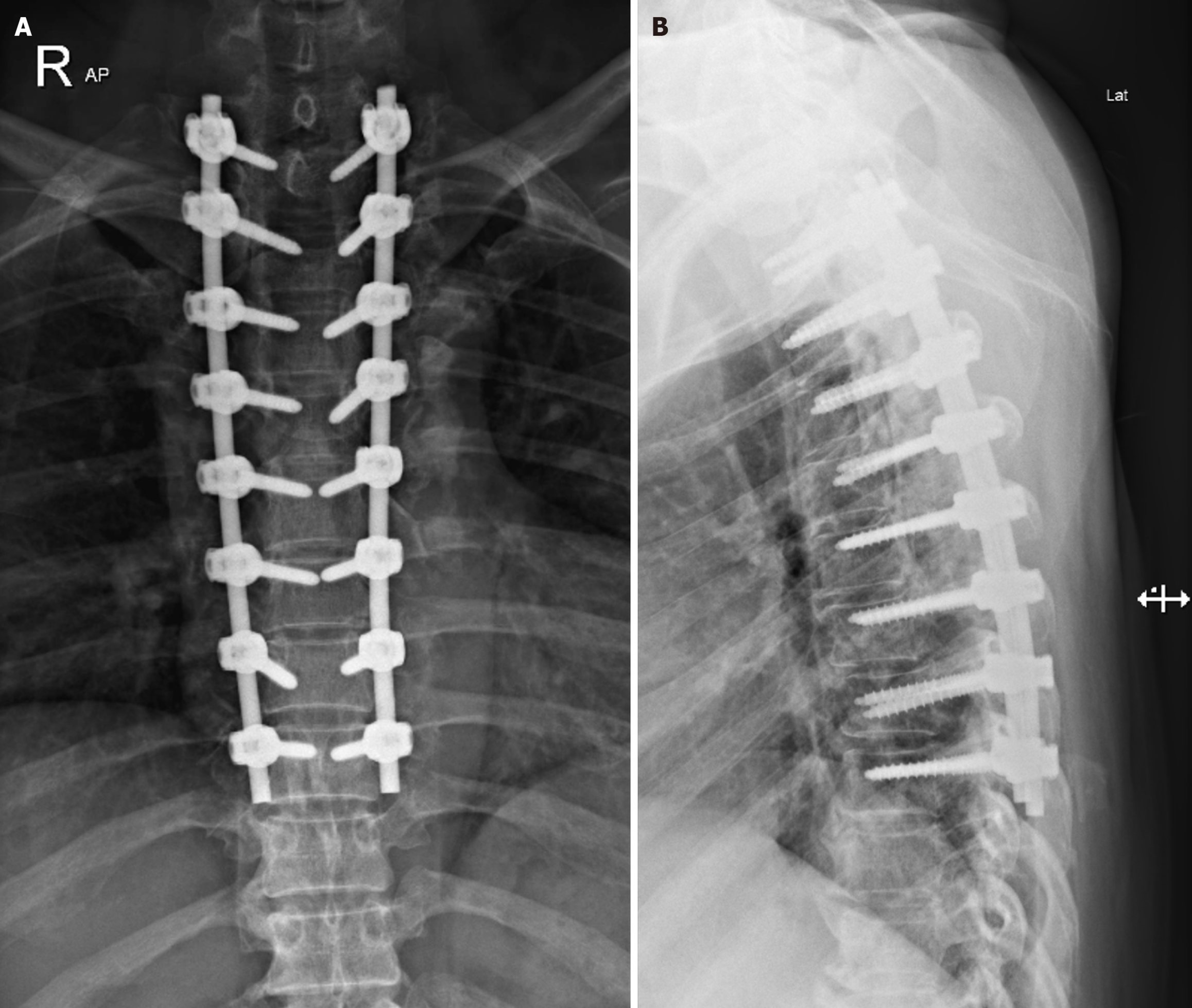
The operation lasted for 371 minutes, the blood loss was about 800 mL, and the autologous blood transfusion was about 656mL. After the operation, the numbness symptoms of both lower limbs were obviously relieved, and the activity was obviously restored, and the m-JOA score was raised to 9. X-ray examination showed that the internal fixation was good, CT scan showed that the physiological kyphosis of thoracic vertebra became straight, the vertebral body-ossification complex moved forward compared with Kyphosis-Line, and the vertebral body-ossification complex moved forward by about 4.4 mm; MRI examination showed that the compression of thoracic spinal cord was obviously improved and the spinal cord drifted backwards. After 3 months follow-up, bone healing can be seen at the rib osteotomy, and the imaging data are shown in Figures 4, 5, and 6.
T-OPLL, especially multi-segmental ossification, usually occupies space in the thoracic spinal canal. As the spinal canal of the thoracic vertebra is relatively narrow, and the ossified posterior longitudinal ligament easily causes spinal cord compression, the surgical risk is relatively high[16]. Moreover, when T-OPLL compresses the spinal cord, symptoms of nerve injury can occur, which cause gradual deterioration, and conservative treatment is not effective, therefore surgery is often necessary.
At present, the recovery rate of postoperative neurological function in commonly used clinical operations is less than 60%, and there are many complications, of which dural tear, deterioration of neurological function and cerebrospinal fluid leakage are frequent. In addition, surgical treatment is mainly suitable for ossification within 3 segments. With an increase in the number of diseased segments, the incidence of surgical complications and the incidence of postoperative neurological deterioration increased sharply[17,18].
However, this operation draws lessons from the concepts of "vertebral body-ossified complex" and "in-situ decompression of spinal cord" in the anterior cervical spine. During the operation, symmetrical vertical slots are made, and several consecutive thoracic vertebral bodies together with the ossified posterior longitudinal ligament are pushed forward to directly decompress the spinal cord, which can relieve spinal cord compression and greatly reduce the risk of spinal cord injury[19]. By moving the ossified section forward to enlarge the spinal canal, it is not necessary to directly remove the stressor and not touch the spinal cord, which reduces surgical complications caused by the operation around the dural sac and avoids the impact of the operation on nerves, which can not only relieve spinal cord compression, but also restore and maintain the anatomical position and nutritional state of the spinal cord. In addition, this operation is not limited by the number of ossified segments, and is especially suitable for the surgical treatment of T-OPLL with serious continuity in long segments. It can realize spinal cord decompression while avoiding ossified resection and osteotomy, and effectively reduce the risk of complications such as dural sac injury.
Determining the forward distance of the vertebral body-ossification complex is one of the key factors in this operation. The maximum anteroposterior diameter of the ossified section should be chosen as the forward movement distance may lead to excessive forward movement of the vertebral body. If there is adhesion between the ossified section and the dural sac and dural calcification, excessive forward movement will increase the risk of dural sac tearing and cerebrospinal fluid leakage. When this occurs, it is extremely difficult to repair the ventral dural sac, which will greatly increase the risk of secondary spinal cord injury. Therefore, it is very important to plan an appropriate anteversion distance before surgery. We suggest that the forward distance does not need to be based on the maximum anteroposterior diameter of ossification, but should be based on the fact that the physiological kyphosis of thoracic vertebra can be relieved and the spinal cord can float backwards. Comparing the Kyphosis-Line before and after surgery, it can be clearly seen that the physiological kyphosis of the thoracic vertebra was straight and the spinal cord drifted backwards in our patient.
Severing bilateral ribs is the key to free ossification of the vertebral body, but there is a risk of injury to intercostal nerves and blood vessels. However, in practice, the probability of such damage is relatively low. Firstly, in the osteotomy position, intercostal nerves and blood vessels are mainly in the middle of the intercostal space, and are not close to the rib bone surface. Secondly, the subperiosteal separation of ribs can reduce bleeding during osteotomy. Finally, the risk of injury to parietal pleura and important vascular structures can be reduced by retaining the anterior cortical bone and biting it with a gun clamp.
Opening the intervertebral foramen of the anterior vertebral body is disputed in this operation. We suggest that there is no need to deliberately open the intervertebral foramen in this technique. Firstly, if the intervertebral foramen is opened, this can easily cause damage to the nerve root during the operation. Secondly, during mature osteotomy and orthopedic surgery for kyphosis, which also changes the original biomechanics, the intervertebral foramen is not treated during the operation, and will not lead to complications without nerve root symptoms[20].
Although this operation has obvious advantages, there are still some drawbacks which require attention as follows: (1) During the operation of moving the vertebral body forward, after exposing and cutting the vertebral lamina of the moving forward segment, loosening the intervertebral disc at the head and tail end, and placing nails, the pedicle screws and nuts of the moving forward segment are locked first, and then a plurality of screw tighteners are synchronously and slowly screwed into the nuts of the non-moving forward segment. The screws are then pressed down by the titanium rod to complete the controllable moving forward of the vertebral ossification, and finally the nuts are locked; (2) There should be at least two pairs of screws at the head and tail ends of the ossified section in order to have enough force (the principle of reverse cantilever arm) to move the thoracic vertebral body and ossified section forward. With an increase in the number of vertebral bodies that need to be moved forward, more screws may be needed to fix them at the head and tail ends; (3) For the vertebral body that needs to be moved forward, the pedicle screws should be of a relatively long length, a part of the length of the tail end of the screw should be reserved to expose outside the pedicle. The specific length depends on the length of the spinal canal invaded by the ossified section in the sagittal direction; (4) T-OPLL patients with osteoporosis should be treated with bone cement screws during the operation or anti-osteoporosis treatment before the operation; and (5) The specific pathogenesis of ossification of the posterior longitudinal ligament of the spine remains to be clarified. Some scholars believe that fretting stress is an important factor for the growth of ossification[21]. Research shows that ossification in patients who have achieved firm fusion through anterior osteotomy had not progressed and even decreased during postoperative follow-up, while ossification in patients who have retained some mobility of the spine, such as in laminoplasty, has made some progress[22]. Therefore, intraoperative internal fixation should be firm and reliable, which has obvious significance for the prognosis of patients.
There are some limitations in this study. Only one patient was included for surgery and the postoperative follow-up time was short. The risk of intercostal nerve and artery injury, pleural injury, hemopneumothorax and so on may occur when the ribs are free during operation. In this case, there were few diseased vertebral segments, and further research on long segment T-OPLL needs to be carried out. Our patient was followed-up for a short time, and there are no long-term follow-up cases and postoperative revision cases to identify whether osteoporosis is due to age after surgery.
Controlled thoracic vertebroplasty is an effective treatment for T-OPLL, especially for long-segment lesions, with less bleeding, less trauma and low risk, which provides a new method for the treatment of T-OPLL but requires further investigation for verification in the future.
| 1. | Gao R, Yuan W, Yang L, Shi G, Jia L. Clinical features and surgical outcomes of patients with thoracic myelopathy caused by multilevel ossification of the ligamentum flavum. Spine J. 2013;13:1032-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Ushio S, Shindo S, Otani K, Kusano K, Miyake N, Yamada T, Nakai O, Okawa A. Predictors of good outcome after anterior decompression and fusion in patients with ossification of the posterior longitudinal ligament of the thoracic spine. J Orthop Sci. 2023;28:515-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Matsumoto M, Chiba K, Toyama Y, Takeshita K, Seichi A, Nakamura K, Arimizu J, Fujibayashi S, Hirabayashi S, Hirano T, Iwasaki M, Kaneoka K, Kawaguchi Y, Ijiri K, Maeda T, Matsuyama Y, Mikami Y, Murakami H, Nagashima H, Nagata K, Nakahara S, Nohara Y, Oka S, Sakamoto K, Saruhashi Y, Sasao Y, Shimizu K, Taguchi T, Takahashi M, Tanaka Y, Tani T, Tokuhashi Y, Uchida K, Yamamoto K, Yamazaki M, Yokoyama T, Yoshida M, Nishiwaki Y. Surgical results and related factors for ossification of posterior longitudinal ligament of the thoracic spine: a multi-institutional retrospective study. Spine (Phila Pa 1976). 2008;33:1034-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 109] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Xu ZW, Hu YC, Sun CG, Shang XP, Lun DX, Li F, Ji XB, Liu DY, Chen NW, Zhuang QS. Treatment for Thoracic Ossification of Posterior Longitudinal Ligament with Posterior Circumferential Decompression. Orthop Surg. 2017;9:206-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Hirabayashi S, Kitagawa T, Yamamoto I, Yamada K, Kawano H. Surgical Treatment for Ossification of the Posterior Longitudinal Ligament (OPLL) at the Thoracic Spine: Usefulness of the Posterior Approach. Spine Surg Relat Res. 2018;2:169-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Liu W, Hu L, Chou PH, Liu M, Kan W, Wang J. Comparison of anterior decompression and fusion versus laminoplasty in the treatment of multilevel cervical ossification of the posterior longitudinal ligament: a systematic review and meta-analysis. Ther Clin Risk Manag. 2016;12:675-685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Kanematsu R, Hanakita J, Takahashi T, Shimauchi-Ohtaki H, Miyasaka K, Minami M. Microsurgical Resection of Ossification of the Posterior Longitudinal Ligament in the Thoracic Spine via the Transthoracic Approach Without Spinal Fusion: 2-Dimensional Operative Video. World Neurosurg. 2021;145:454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Xu N, Yu M, Liu X, Sun C, Chen Z, Liu Z. A systematic review of complications in thoracic spine surgery for ossification of the posterior longitudinal ligament. Eur Spine J. 2017;26:1803-1809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Yang P, Ge R, Chen ZQ, Wen BT. Treatment of Thoracic Ossification of Posterior Longitudinal Ligament with One-Stage 360 Degree Circumferential Decompression Assisted by Piezosurgery. J Invest Surg. 2022;35:249-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Hu P, Yu M, Liu X, Liu Z, Jiang L. A circumferential decompression-based surgical strategy for multilevel ossification of thoracic posterior longitudinal ligament. Spine J. 2015;15:2484-2492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Saiwai H, Okada S, Hayashida M, Harimaya K, Matsumoto Y, Kawaguchi KI, Kobayakawa K, Maeda T, Ohta H, Shirasawa K, Tsuchiya K, Terada K, Kaji K, Arizono T, Saito T, Fujiwara M, Iwamoto Y, Nakashima Y. Surgery-related predictable risk factors influencing postoperative clinical outcomes for thoracic myelopathy caused by ossification of the posterior longitudinal ligament: a multicenter retrospective study. J Neurosurg Spine. 2020;32:703-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Kato S, Murakami H, Demura S, Yoshioka K, Yokogawa N, Takaki S, Oku N, Tsuchiya H. Indication for anterior spinal cord decompression via a posterolateral approach for the treatment of ossification of the posterior longitudinal ligament in the thoracic spine: a prospective cohort study. Eur Spine J. 2020;29:113-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Wang S, Sun K, Xu X, Sun J, Wang Y, Shi JG. A Novel "De-tension"-guided Anterior Decompression Strategy-Thoracic Anterior Controllable Antedisplacement Fusion (TACAF) for Multilevel Ossification of Posterior Longitudinal Ligament in Thoracic Spine: A Retrospective Study with at Least 2-Year Follow-Up. World Neurosurg. 2024;186:e639-e651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Yan C, Jia HC, Sun JC, Shi JG. Anterior controllable antidisplacement and fusion surgery for the treatment of extensive cervico-thoracic ossification of posterior longitudinal ligament with severe myelopathy: case report and literature review. Br J Neurosurg. 2023;37:364-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Ghogawala Z, Terrin N, Dunbar MR, Breeze JL, Freund KM, Kanter AS, Mummaneni PV, Bisson EF, Barker FG 2nd, Schwartz JS, Harrop JS, Magge SN, Heary RF, Fehlings MG, Albert TJ, Arnold PM, Riew KD, Steinmetz MP, Wang MC, Whitmore RG, Heller JG, Benzel EC. Effect of Ventral vs Dorsal Spinal Surgery on Patient-Reported Physical Functioning in Patients With Cervical Spondylotic Myelopathy: A Randomized Clinical Trial. JAMA. 2021;325:942-951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 140] [Cited by in RCA: 109] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 16. | Kasukawa Y, Miyakoshi N, Hongo M, Ishikawa Y, Kudo D, Kimura R, Ono Y, Iida J, Sato C, Shimada Y. Surgical Results of Patients with Myelopathy due to Ossification of the Ligamentum Flavum with Ossification of the Posterior Longitudinal Ligament or a Vertebral Fracture at the Same Level of the Thoracic Spine: A Retrospective Comparative Study. Asian Spine J. 2019;13:832-841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Imagama S, Ando K, Takeuchi K, Kato S, Murakami H, Aizawa T, Ozawa H, Hasegawa T, Matsuyama Y, Koda M, Yamazaki M, Chikuda H, Shindo S, Nakagawa Y, Kimura A, Takeshita K, Wada K, Katoh H, Watanabe M, Yamada K, Furuya T, Tsuji T, Fujibayashi S, Mori K, Kawaguchi Y, Watanabe K, Matsumoto M, Yoshii T, Okawa A. Perioperative Complications After Surgery for Thoracic Ossification of Posterior Longitudinal Ligament: A Nationwide Multicenter Prospective Study. Spine (Phila Pa 1976). 2018;43:E1389-E1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 18. | Onishi E, Yasuda T, Yamamoto H, Iwaki K, Ota S. Outcomes of Surgical Treatment for Thoracic Myelopathy: A Single-institutional Study of 73 Patients. Spine (Phila Pa 1976). 2016;41:E1356-E1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Yang H, Xu X, Shi J, Guo Y, Sun J, Shi G, Wang Y. Anterior Controllable Antedisplacement Fusion as a Choice for Ossification of Posterior Longitudinal Ligament and Degenerative Kyphosis and Stenosis: Postoperative Morphology of Dura Mater and Probability Analysis of Epidural Hematoma Based on 63 Patients. World Neurosurg. 2019;121:e954-e961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Miller DJ, Cahill PJ, Vitale MG, Shah SA. Posterior Correction Techniques for Adolescent Idiopathic Scoliosis. J Am Acad Orthop Surg. 2020;28:e363-e373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Chen Y, Chen D, Wang X, Yang H, Liu X, Miao J, Yu F. Significance of segmental instability in cervical ossification of the posterior longitudinal ligament and treated by a posterior hybrid technique. Arch Orthop Trauma Surg. 2013;133:171-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Lee DH, Nam WD, Kim NY, Park JW, Hong CG. Fate of Ossification of Posterior Longitudinal Ligament Following Anterior Cervical Fusion: Progression of Cervical Ossification of Posterior Longitudinal Ligament After Vertebral Body Sliding Osteotomy or Laminoplasty. World Neurosurg. 2021;146:e1270-e1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |