Published online Jun 18, 2025. doi: 10.5312/wjo.v16.i6.107422
Revised: April 17, 2025
Accepted: May 23, 2025
Published online: June 18, 2025
Processing time: 87 Days and 5.1 Hours
Phantom limb pain (PLP) is not only a physical pain experience but also poses a significant challenge to mental health and quality of life. Currently, the mecha
Core Tip: Phantom limb pain (PLP) is one of the most common complications of amputation. Extended reality (XR) has advantages of being a noninvasive, nonpharmacological treatment. We review the application of XR in treating PLP. We explore the potential of virtual reality, augmented reality, and mixed reality in alleviating pain and improving psychological status and quality of life of patients with PLP. We highlight the latest advances and future research directions, providing a theoretical basis for developing more effective treatment strategies.
- Citation: Gan D, Wang SY, Liu K, Zhang SY, Huang H, Xing JH, Qin CH, Wang KY, Wang T. Innovative exploration of phantom limb pain treatment based on extended reality technology. World J Orthop 2025; 16(6): 107422
- URL: https://www.wjgnet.com/2218-5836/full/v16/i6/107422.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i6.107422
Phantom limb pain (PLP) is one of the most common complications of amputation. Approximately 57.7 million patients worldwide have undergone amputation as a result of trauma[1]. In China, there were approximately 2 million amputees. In the United States, there were approximately 1.7 million amputees, and the annual number of new amputations was approximately 215000[2]. The primary causes of amputation include peripheral vascular disease, severe trauma, infection, and tumors, and the incidence of PLP does not significantly differ among these various causes[3]. About 65% of amputees develop PLP within 1 month after amputation, 82% within 1 year and 87% throughout their lifetime[4]. The sensation of PLP can be likened to throbbing, stabbing, drilling, squeezing, burning, twisting, and in some patients, there may also be other bodily pain symptoms such as headaches and back pain[5]. The precise mechanism underlying PLP remains unclear, but likely involve a complex interplay of peripheral, central and psychological factors[6]. Currently, there are > 25 treatment methods for PLP in clinical practice[7]. Mirror therapy (MT) has become an important choice due to its low cost, noninvasiveness and effectiveness that is not significantly inferior to that of other methods[8-11]. However, MT is not without its limitations. Specifically, it imposes constraints on the patient's posture and restricts the range of limb movement. Additionally, the size of the mirror itself is limited. These limitations can easily cause the mirrored limb to break the illusion, thereby providing patients with a suboptimal experience. With the advancement of computer te
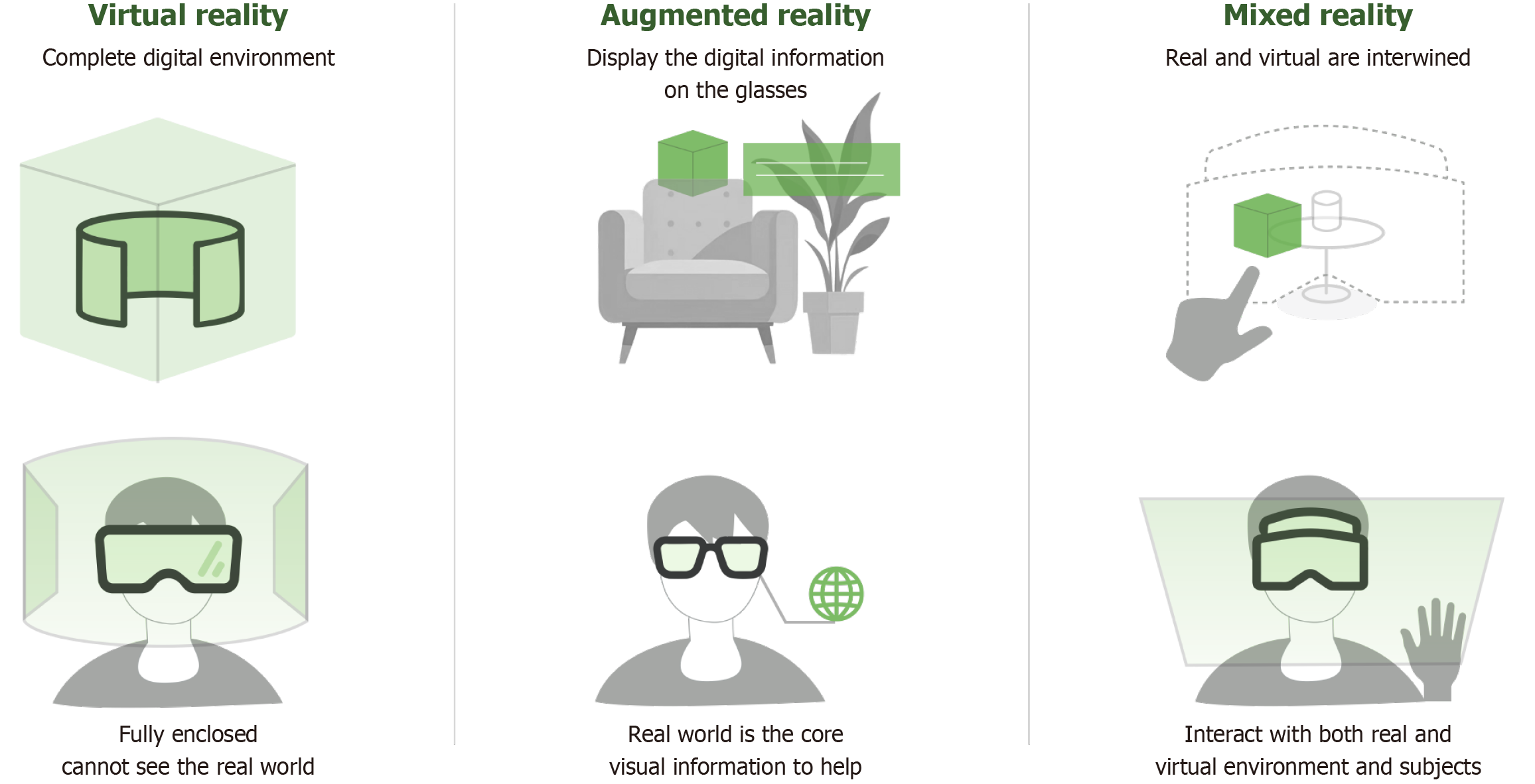
XR technology refers to the use of computer technology and wearable devices to create a human–computer interactive environment, which is the general term for VR, AR, mixed reality (MR) and other emerging immersive technologies[12]. VR provides a fully virtual environment where users can interact with computer-generated imagery and audio, completely immersing them without the need to perceive the real world. AR overlays virtual objects onto the real environment, enabling users to simultaneously experience both reality and virtual content. MR integrates the advantages of both VR and AR, allowing users to interact with virtual objects in real time within the real world. This makes virtual content responsive to changes in the real environment and enables users to adjust visual and auditory stimuli in a multisensory setting. The main features of XR technology are compared in Table 1, and the visual difference is showed in Figure 1.
| Virtual reality | Augmented reality | Mixed reality | |
| Need a device | Yes | Yes | Yes |
| Virtual environment | Totally | None | Fusion |
| Virtual subjects | Totally | Interactive boxes | On demand |
| Real environment | None | Totally | Fusion |
| Real subjects | None | Totally | Totally |
| Difficulty of the development | Moderate | Difficult | Hardest |
The application of XR technology within the medical field has garnered increasing attention. Its uses are expanding in surgical simulation, case presentation, rehabilitation training, medical education, and other areas. At present, there are 69 medical devices involving AR/VR approved in the United States[13]. XR technology has the potential to create immersive, interactive and realistic environments that can promote learning through feedback, reflection and practice while reducing the risks and costs associated with real-life scenarios[14]. In 2021, a VR treatment system (EaseVRx) was approved by the United States Food and Drug Administration (FDA) for the auxiliary treatment of chronic pain[15]. The VR program utilized its fully immersive characteristics to apply behavioral therapies, such as deep relaxation and attention diversion, to alleviate pain. The integrated application of XR technology fosters the development of multidisciplinary collaboration and offers a new theoretical and technical foundation for future pain management strategies.
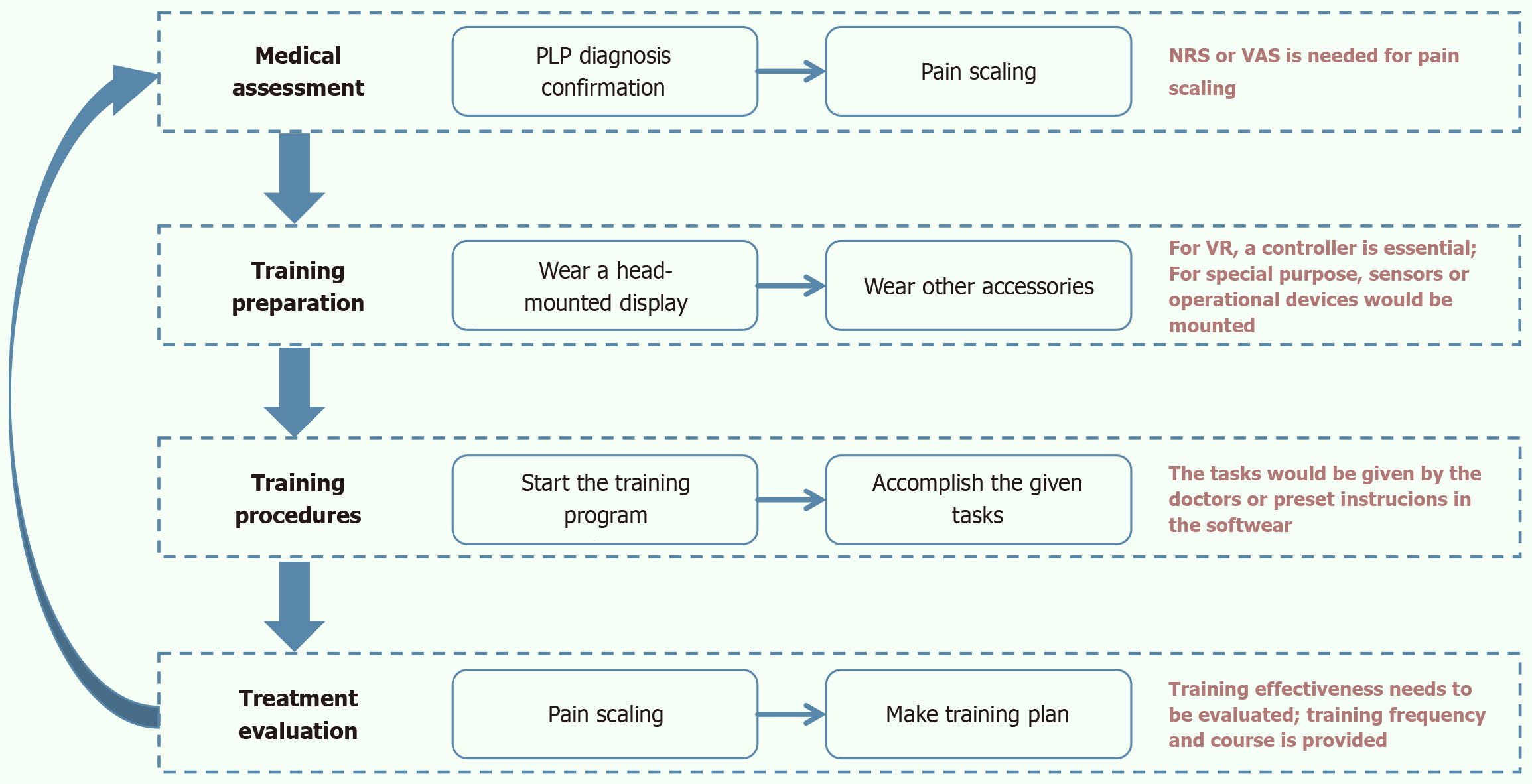
When XR is applied to PLP patients, a head-mounted display must be worn. Depending on the type of XR device and the specific treatment approach, patients may need to wear handheld controllers, sensors or other interactive devices. Using the head-mounted display, patients can visualize a computer-generated representation of their amputated limb. Guided by the physician's instructions or voice prompts from the training software, they then use this virtual limb to perform a series of tasks outlined in the program, thereby completing the full treatment process. The general procedures are showed in Figure 2. Given the distinct features and developmental stages of XR technologies, VR, AR and MR methods are discussed separately. Some of the key studies are listed in Table 2[16-27].
| Ref. | Type of study design | VR/AR/MR | Intervention | Treatment duration | No. of sessions | Pain assessment | Pretreatment | Post-treatment | Treatment efficiency |
| Ortiz-Catalan et al[20], 2016 | Single-group clinical trial | AR/VR | Machine learning-based myoelectric control of virtual limb in AR/VR environments, including gaming tasks (e.g., racing car, target matching) | 2 hours/session | 12 | NRS, PRI | NRS: 5.2 ± 1.6, PRI: 19.2 ± 10.5 | NRS: 3.5 ± 2.1, PRI: 9.6 ± 8.1 | 50% of patients reduced medication intake; 71% reported ≥ 50% pain reduction at 6 months follow-up |
| Osumi et al[17], 2017 | Clinical trial | VR | VR system using head-mounted display to show mirror-reversed computer graphic image of intact arm, simulating phantom limb movement | 10 minutes (single session) | 1 | NRS, SF-MPQ | NRS: 5.2 ± 2.4, SF-MPQ: 8.3 ± 7.6 | NRS: 3.0 ± 2.1, SF-MPQ: 2.5 ± 3.2 | 39.1% reduction in NRS; 61.5% reduction in SF-MPQ |
| Lendaro et al[19], 2017 | Case study | VR | Phantom motor execution with myoelectric pattern recognition and virtual reality for lower-limb amputee | Approximately 2 hours/session | 23 | NRS, PRI | NRS: 4, PRI: 32 | NRS: 2, PRI: 10 | 50% reduction in NRS; 68% reduction in PRI |
| Perry et al[22], 2018 | Clinical trial | VR | Virtual integration environment using electromyography to control virtual avatar limb movements | 30 minutes/session | Average 18 | VAS, SF-MPQ | VAS: Curve in figure, SF-MPQ: Curve in figure | VAS: Curve in figure, SF-MPQ: A curve in figure | 88% of participants reported pain reduction; 29% sustained relief at 6 months |
| Rothgangel et al[23], 2018 (n = 75) | Single-blind RCT | AR | Group A: MT (4 weeks) + AR (6 weeks); group B: MT (4 weeks) + self-delivered MT (6 weeks); group C: Sensomotor exercises of intact limb (10 weeks) | 10 weeks (4 weeks initial + 6 weeks follow-up) | 10 individual sessions (first 4 weeks) | NRS | NRS: Mean 5.7 | Group A: 4.6 (10 weeks), 4.1 (6 months); group B: 3.6 (10 weeks), 2.7 (6 months); group C: 4.1 (10 weeks), 4.5 (6 months) | No significant between-group differences in NRS; 3 patients in group B showed complete recovery of PLP at 6 months |
| Rutledge et al[18], 2019 | Feasibility study | VR | VR MT with bicycle pedaler and motion sensor to synchronize real/virtual limb motion | Single session (feasibility testing) | 1 | Phantom Limb Pain Questionnaire | 57.1% (8/14) participants reported PLP; 93% (13/14) reported one or more unpleasant phantom sensations | 28.6% (4/14) continued to report PLP symptoms and 28.6% (4/14) reported phantom sensations | Participants rated the treatment highly (75%) on the dimensions of helpfulness, immersion, realism, and satisfaction |
| Kulkarni et al[24], 2020 | Pilot study | VR | Immersive VR with virtual limb visualization and interactive tasks | 55 minutes/session/months | 3 sessions (3 month) | NRS | NRS: Mean 6.11 | Mean NRS: 3.56 | Reduction in NRS with no significant difference |
| Thøgersen et al[21], 2020 | Case series | AR | Customized AR training with virtual limb visualization matched to individual phantom perception, controlled via myoelectric signals; 3 tasks (pick-and-place, imitation, sorting), functional magnetic resonance imaging before and after intervention | 45 minutes/session, over 2 weeks | 8 | SF-MPQ, NRS | NRS: Mean 2.26 (for responding patients) | SF-MPQ: Mean change = | 52% reduction in SF-MPQ; 41% reduction in NRS; cortical reorganization correlated with pain relief |
| Tong et al[25], 2020 | Case series | VR | Immersive VR where intact limb movements control a virtual avatar, providing mirrored visual feedback | 4–6 weeks | 3–10 | VAS, SF-MPQ | VAS: Mean 7.6, SF-MPQ: Mean 16.4 | VAS: Mean 6.15, SF-MPQ: Mean 7.06 | 19.04% reduction in VAS; 56.96% reduction in SF-MPQ; all participants showed pain reduction; improvements in anxiety and depression |
| Ambron et al[16], 2021 | Clinical trial | VR | Custom VR games controlling avatar legs via motion-tracking sensors on intact/residual limbs | 55 minutes/session | 5–7 distractor sessions + 10–12 targeted sessions | VAS | VAS: 6.1 ± 2.1 | VAS: 3.1 ± 2.1 | 28% reduction after distractor sessions; 39.6% reduction after targeted sessions |
| Annaswamy et al[27], 2022 | Pilot study | MR | Home-based use of Mr. MAPP system (mixed reality MT with exergames: Bubble Burst, Pedal, Piano games) | 1 month | Daily sessions | NRS, SF-MPQ, Patient-Specific Functional Scale | No clear baseline pain intensity reported | No clear trends in pain scores | Not statistically significant due to small sample size; 1/4 participants reported functional improvement |
| Lendaro et al[26], 2024 | RCT | XR (VR/AR) | Phantom motor execution using myoelectric pattern recognition to control XR environment vs PMI with guided mental rehearsal | Variable (28–40 weeks total) | 15 | PRI from SF-MPQ, NRS | Phantom motor execution: NRS: 4.48 ± 2.77, PRI: 14.5 ± 8.78, PMI: NRS: 4.04 ± 2.87, PRI: 14.71 ± 7.28 | Phantom motor execution: NRS change = 1.97 ± 0.11, PRI change = 9.35 ± 0.22 PMI: NRS change = 1.25 ± 0.18, PRI change = 10.03 ± 0.45 | 64.5% (phantom motor execution) and 68.2% (PMI) reduction in PRI; 71% (phantom motor execution) and 68% (PMI) experienced ≥ 50% pain reduction |
VR technology has shown promise by providing a sense of realism during training, thereby promoting skill acquisition and retention, and inducing functional recovery in area of neurorehabilitation[28]. The reduction and cure of PLP is achieved through activated the cortical representation of the phantom[29]. This indicates that PLP is also a task for neurorehabilitation, so VR technology should be equally effective in alleviating PLP. In terms of technical application, constructing a virtual environment provides participants with immersive visual VR experiences. By engaging multiple senses, it diverts attention from PLP and guides the reshaping of brain neurons, thereby achieving pain relief[16].
First of all, VR can completely substitute MT. There are several methods to achieve the reproduction of residual limbs. The first method is to display the image of the healthy side in reverse, which is a direct copy of MT. Osumi et al[17,30] had the patient wear a display that presented an inverted image of their entire arm (virtual phantom limb), inducing the patient to perceive the autonomous execution of the phantom limb during residual limb movement. They utilized the Short-form McGill Pain Questionnaire to assess the characteristics of PLP in 19 patients, achieving a pain relief rate (or PLP alleviation rate) of 52.1% ± 38.2% from a single session of VR mirror visual feedback therapy. Compared to MT, this method increases the range of motion; however, if the patient has bilateral amputations, the mirror effect is absent. The second method involves a fully virtual limb, similar to those in a VR game, where the patient controls the movement of the virtual limb using a joystick[31]. Rutledge et al[18] developed a VR environment for cycling and designed a specialized device for patients with prosthetic limbs. This device allows the movement of the prosthetic limb to be reflected in the VR environment and displayed in the imaging system of the helmet, enabling patients to see the feedback of their phantom limb movements within the virtual setting. A meta-analysis[32] showed that both MT and VR were equally effective in alleviating PLP, with neither demonstrating superior efficacy. Nonetheless, larger randomized controlled trials are still needed.
VR technology achieves its intervention effect by cheating the brain, but patients often harbor higher expectations for such technology. The interaction between patients and their limbs in the virtual world is achieved through simple movements, yet it lacks the patients' own perception. Ichinose et al[33] had participants to use VR devices for neurorehabilitation exercises. During this process, participants operated the virtual limbs to touch their cheeks, while real tactile stimuli were provided through motors. The results showed that the median pain reduction rate in the cheek intervention group (33.3% ± 24.4%) was significantly higher than that in the intact hand control group (16.7% ± 12.3%) and the no-stimulation control group (12.5% ± 13.5%, P < 0.05). This indicates that applying sensory feedback to the patient's cheeks can significantly enhance the analgesic effect of visual feedback during phantom limb movement. This suggests that a treatment approach combining VR with tactile and visual multisensory feedback is of great significance for pain relief in patients.
In addition to using VR alone, combining it with electromyographic control techniques offers new perspectives for treating PLP. Using VR technology, an immersive environment can be created that diverts patients' attention from pain, while electromyographic control captures and analyzes muscle activity in real time and regulates limb movements with external devices. This not only enhances the interactive effects of treatment but also helps patients reshape their perception of their limbs. Chau et al[34] utilized immersive VR MT, and equipped patients with armband electro
In addition to relieving PLP, VR technology has also been shown to improve depression and mental health in amputees[35]. VR has shown unique advantages in the treatment of PLP, which deserves further application and research.
AR technology integrates the virtual subjects generated by computers with the user's real-world surroundings. This is achieved through photoelectric display technology, interactive technology, multiple sensor technology, and computer graphics and multimedia technology. It enhances the interaction between users, digital content and the real world, allowing for the display of virtual images while maintaining transparency[36]. Compared to VR, AR has a greater degree of integration with the real environment, enabling patients to receive virtual auxiliary content related to treatment within the familiar real-world setting, thereby reducing the sense of isolation that pure virtual scenes can bring.
By overlaying a virtual hand model onto the residual limb using AR glasses and controlling it with electromyography (EMG) signals from the residual limb, patients are encouraged to practice using the virtual hand through games[37]. Ortiz-Catalan et al[20] combined machine learning, AR, VR and serious games for PLP intervention, and the treatment process selectively repeated each step according to its difficulty level. To the end, this approach reduced pain distribution by 47%, decreased Numerical Rating Scale (NRS) scores by 32%, and lowered Visual Analog Scale scores by 51%. This treatment method also reduced the impact of pain on daily life and sleep quality, and significantly decreased the use of analgesics. Studies are now required to examine the magnitude of effects compared with alternative treatments, or placebo, to determine whether this treatment warrants the investment in resources and training that would be required to deliver this therapy in practice[38]. A virtual arm visualization, aligned with the individual's phantom limb perception, was integrated into an AR intervention. Seven participants with PLP and telescoped phantom limbs underwent eight supervised, home-based AR training sessions (each lasting 45 minutes) over a period of 2 weeks. The virtual arm was superimposed onto the participants' residual limbs using EMG for control. The AR training sessions comprised three tasks designed to re-engage neural circuits associated with the lost limb. Measures of agency (using the Rubber Hand Illusion questionnaire) and telescoping (through proprioceptive drift and felt telescoping assessments) were monitored following each training session. Functional magnetic resonance imaging during lip pursing was conducted before and after the intervention. The pain rating index scores decreased by 52%, while the NRS scores for PLP severity (ranging from 0 to 6) in patients benefiting from the intervention were reduced by 41%[21].
Keesom et al[39] utilized AR devices for PME treatment. Most participants who had undergone limb amputation and experienced chronic PLP described the PME treatment as a valuable addition to their strategies for alleviating PLP. The PME treatment transformed passive pain management into an active strategy, with positive effects on quality of life, sleep and energy levels. Learning to control the phantom limb and normalizing its perceived size were found to contribute to successful treatment outcomes.
MR technology is a combination of VR and AR in three-dimensional (3D) applications. A core feature of MR technology is to introduce and integrate 3D hologram into the real world seen by users, and establishes interactive feedback loop between the virtual world and the real world to enhance the sense of reality and space of user experience. Compared to AR and VR, MR not only anchors virtual objects into the physical world, enabling the user to interact with both virtual and real objects, but also allows the user to experience depth and perspective, which significantly improves 3D visua
MR technology is often used for surgical navigation and medical education rather than entertainment[14,41,42]. MR technology seamlessly integrates virtual limbs and scenes with the real environment, allowing patients to perceive both the real world and virtual therapeutic elements simultaneously. This approach enables treatment to occur in familiar, real-world settings. The research on MR for PLP has been conducted by the same team since 2017. Over 7 years, the team has progressed from initially using the system to verify its therapeutic effects to more recent studies that apply it to various scenarios, such as the home environment, thus achieving deeper and broader applications. In 2017, Bahirat et al[43] introduced a new MR system called Mr. MAPP, aiming to improve the treatment outcomes for patients with PLP. The system utilized an RGB-D camera to capture real-time 3D models of the patient and generates skeletal structures of the missing limb using computer vision and graphics technology, enabling natural interaction with virtual objects. Research findings indicated that Mr. MAPP had significant value in alleviating PLP and received positive feedback from users, marking a crucial breakthrough in MR technology in this field. In 2022, researchers conducted clinical feasibility studies, confirming the practicality of Mr. MAPP and demonstrating its potential to improve pain and function in patients with PLP[27]. By 2023, researchers released their latest findings, exploring the application of the Mr. MAPP system in home environments to evaluate its effectiveness for patients with PLP. The study required PLP patients to use the system at home and record their daily pain intensity to analyze its impact on pain perception and daily function. The results demonstrated that this method was indeed effective. Researchers noted that using MR technology can avoid issues such as skin color and clothing misalignment that often occur with VR due to over-reliance on virtual limb models, but its immersion is slightly less than that of VR[44].
Although research on MR for PLP is still in an early stage, it has made considerable progress by merging with the real world through virtual representations of real objects and human–computer interaction. This method overcomes the limitations of VR being isolated from the real environment and AR lacking human–computer synchronization. Treatment outcomes and patient satisfaction could be enhanced by applying MR to personalized treatment, where real-time monitoring of patient responses can assist in adjusting intervention strategies.
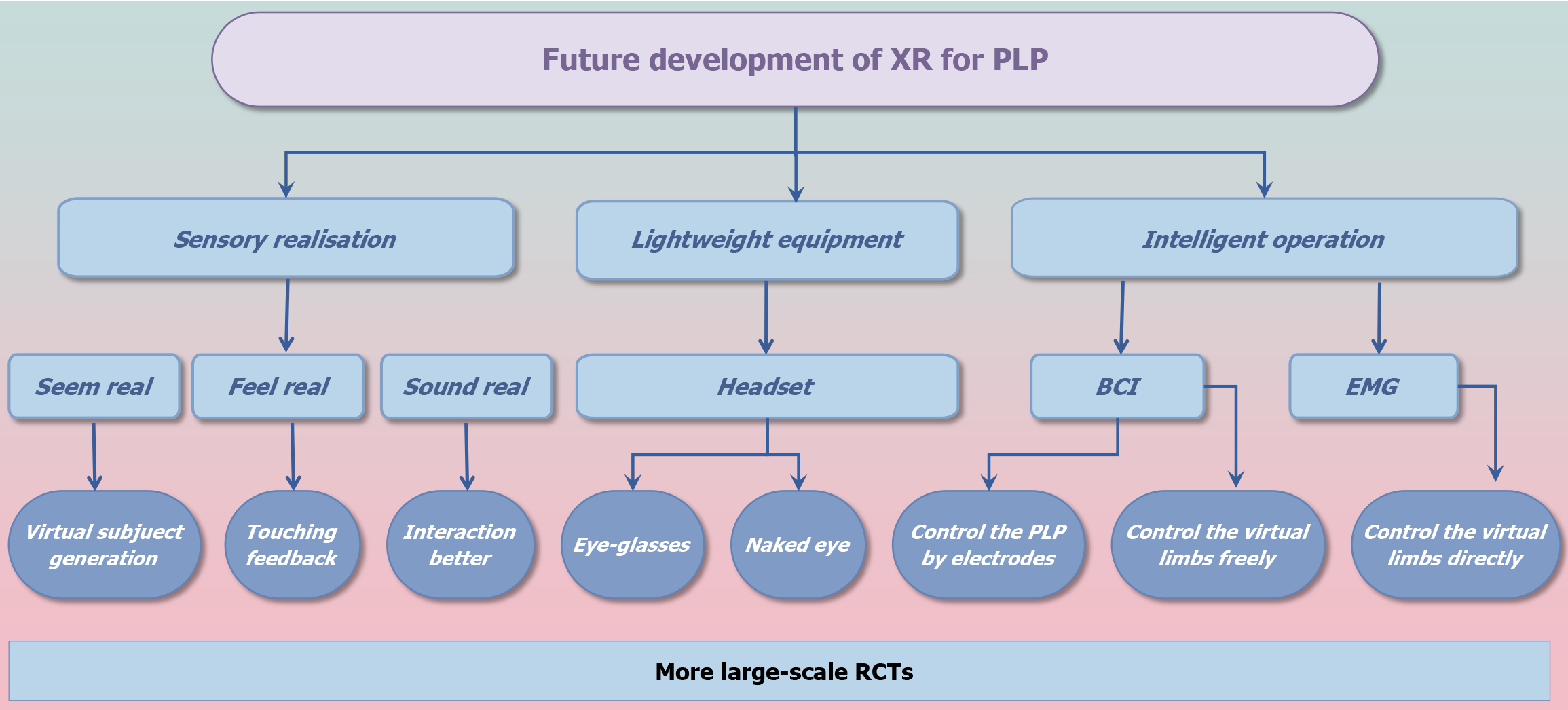
In recent years, the rapid development of XR technology has gradually drawn attention to its potential applications in the medical field, profoundly transforming human production and lifestyle. XR technology has expanded beyond gaming and commercial sectors into emerging areas such as healthcare, education and manufacturing, with industry penetration rates continuously on the rise. Many digital therapies based on XR technology have been approved by the United States FDA[13]. In addition, XR technology has been used to treat a variety of diseases, such as insomnia[45], post-traumatic stress disorder[46], stroke[47] and anxiety disorder[48], and the scope is expanding. It is believed that, in the near future, XR technology will help more diseases (Figure 3)[49].
XR technology offers a new approach by providing an immersive therapeutic environment and a multisensory experience for PLP patients. However, relying solely on XR technology may not fully address PLP. Therefore, it is advisable to combine XR with other treatments, such as physical therapy and electromyographic control. During physical therapy (including massage and physiotherapy), XR technology can be utilized to control virtual limbs for simulated movements. This involves overlaying virtual motion guidance information onto the patient's residual limb, allowing for a more intuitive understanding of whether their movements meet the necessary requirements. Additionally, EMG signals can offer real-time feedback on muscle activity, enabling patients to adjust their muscle states in real-time based on this feedback, thereby enhancing the rehabilitation outcomes for patients with PLP. In the future, brain–computer interface technology could be integrated to collect and decode the EEG signals generated when patients control virtual limbs, providing a more intuitive reflection of the sensory status of the affected limb and transmitting it back to XR devices to adjust treatment plans in real time, achieving personalized and dynamic therapeutic feedback.
The number of studies using VR/AR/MR technology to treat PLP is gradually increasing. However, due to common issues such as small sample sizes and less rigorous experimental design, although many positive results suggest that XR technology may become a potential nonpharmacological treatment for PLP, more long-term research and large-scale clinical trials are still required to verify the long-term effectiveness and safety of XR technologies.
| 1. | McDonald CL, Westcott-McCoy S, Weaver MR, Haagsma J, Kartin D. Global prevalence of traumatic non-fatal limb amputation. Prosthet Orthot Int. 2021;45:105-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 97] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 2. | Culp CJ, Abdi S. Current Understanding of Phantom Pain and its Treatment. Pain Physician. 2022;25:E941-E957. [PubMed] |
| 3. | Nees TA, Matt C, Deisenhofer J, Block J, Wolf SI, Renkawitz T, Lehner B, Alimusaj M. Pain After Lower Limb Amputations: Insights from the Heidelberg Amputation Registry. Medicina (Kaunas). 2024;60:1887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Stankevicius A, Wallwork SB, Summers SJ, Hordacre B, Stanton TR. Prevalence and incidence of phantom limb pain, phantom limb sensations and telescoping in amputees: A systematic rapid review. Eur J Pain. 2021;25:23-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 5. | Kooijman CM, Dijkstra PU, Geertzen JHB, Elzinga A, van der Schans CP. Phantom pain and phantom sensations in upper limb amputees: an epidemiological study. Pain. 2000;87:33-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 311] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 6. | Flor H. Phantom-limb pain: characteristics, causes, and treatment. Lancet Neurol. 2002;1:182-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 420] [Cited by in RCA: 363] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 7. | Aternali A, Katz J. Recent advances in understanding and managing phantom limb pain. F1000Res. 2019;8:F1000 Faculty Rev-F1000 Faculty1167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 8. | Jiang ZB, Yue K, He RL, Xu SR, Zhou ZH, Feng Y, Xiao H, Ma K, Li SQ, Yang LQ, Wang Y, Sun T, Fan XC, Xue ZX, Feng PJ, Zhang DY, Fan BF. [Consensus of Chinese painology experts on diagnosis and treatment of phantom limb pain (2024 edition)]. Zhonghua Tengtongxue Zazhi. 2024;20:164-178. [DOI] [Full Text] |
| 9. | Andrews C, Southworth MK, Silva JNA, Silva JR. Extended Reality in Medical Practice. Curr Treat Options Cardiovasc Med. 2019;21:18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 10. | The US Food and Drug Administration. Augmented Reality and Virtual Reality in Medical Devices. 2024. Available from: https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices#what. |
| 11. | Asoodar M, Janesarvatan F, Yu H, de Jong N. Theoretical foundations and implications of augmented reality, virtual reality, and mixed reality for immersive learning in health professions education. Adv Simul (Lond). 2024;9:36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 12. | The US Food and Drug Administration. FDA Authorizes Marketing of Virtual Reality System for Chronic Pain Reduction. 2021. Available from: https://www.fda.gov/news-events/press-announcements/fda-authorizes-marketing-virtual-reality-system-chronic-pain-reduction. |
| 13. | Campo-Prieto P, Rodríguez-Fuentes G. Effectiveness of mirror therapy in phantom limb pain: a literature review. Neurologia (Engl Ed). 2022;37:668-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Purushothaman S, Kundra P, Senthilnathan M, Sistla SC, Kumar S. Assessment of efficiency of mirror therapy in preventing phantom limb pain in patients undergoing below-knee amputation surgery-a randomized clinical trial. J Anesth. 2023;37:387-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 15. | Limakatso K, Parker R. Treatment Recommendations for Phantom Limb Pain in People with Amputations: An Expert Consensus Delphi Study. PM R. 2021;13:1216-1226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 16. | Ambron E, Buxbaum LJ, Miller A, Stoll H, Kuchenbecker KJ, Coslett HB. Virtual Reality Treatment Displaying the Missing Leg Improves Phantom Limb Pain: A Small Clinical Trial. Neurorehabil Neural Repair. 2021;35:1100-1111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 17. | Osumi M, Ichinose A, Sumitani M, Wake N, Sano Y, Yozu A, Kumagaya S, Kuniyoshi Y, Morioka S. Restoring movement representation and alleviating phantom limb pain through short-term neurorehabilitation with a virtual reality system. Eur J Pain. 2017;21:140-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | Rutledge T, Velez D, Depp C, McQuaid JR, Wong G, Jones RCW, Atkinson JH, Giap B, Quan A, Giap H. A Virtual Reality Intervention for the Treatment of Phantom Limb Pain: Development and Feasibility Results. Pain Med. 2019;20:2051-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 19. | Lendaro E, Mastinu E, Håkansson B, Ortiz-Catalan M. Real-time Classification of Non-Weight Bearing Lower-Limb Movements Using EMG to Facilitate Phantom Motor Execution: Engineering and Case Study Application on Phantom Limb Pain. Front Neurol. 2017;8:470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Ortiz-Catalan M, Guðmundsdóttir RA, Kristoffersen MB, Zepeda-Echavarria A, Caine-Winterberger K, Kulbacka-Ortiz K, Widehammar C, Eriksson K, Stockselius A, Ragnö C, Pihlar Z, Burger H, Hermansson L. Phantom motor execution facilitated by machine learning and augmented reality as treatment for phantom limb pain: a single group, clinical trial in patients with chronic intractable phantom limb pain. Lancet. 2016;388:2885-2894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 133] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 21. | Thøgersen M, Andoh J, Milde C, Graven-Nielsen T, Flor H, Petrini L. Individualized Augmented Reality Training Reduces Phantom Pain and Cortical Reorganization in Amputees: A Proof of Concept Study. J Pain. 2020;21:1257-1269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Perry BN, Armiger RS, Wolde M, McFarland KA, Alphonso AL, Monson BT, Pasquina PF, Tsao JW. Clinical Trial of the Virtual Integration Environment to Treat Phantom Limb Pain With Upper Extremity Amputation. Front Neurol. 2018;9:770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Rothgangel A, Braun S, Winkens B, Beurskens A, Smeets R. Traditional and augmented reality mirror therapy for patients with chronic phantom limb pain (PACT study): results of a three-group, multicentre single-blind randomized controlled trial. Clin Rehabil. 2018;32:1591-1608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 24. | Kulkarni J, Pettifer S, Turner S, Richardson C. An investigation into the effects of a virtual reality system on phantom limb pain: a pilot study. Br J Pain. 2020;14:92-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Tong X, Wang X, Cai Y, Gromala D, Williamson O, Fan B, Wei K. "I Dreamed of My Hands and Arms Moving Again": A Case Series Investigating the Effect of Immersive Virtual Reality on Phantom Limb Pain Alleviation. Front Neurol. 2020;11:876. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Lendaro E, Van der Sluis CK, Hermansson L, Bunketorp-Käll L, Burger H, Keesom E, Widehammar C, Munoz-Novoa M, McGuire BE, O'Reilly P, Earley EJ, Iqbal S, Kristoffersen MB, Stockselius A, Gudmundson L, Hill W, Diers M, Turner KL, Weiss T, Ortiz-Catalan M. Extended reality used in the treatment of phantom limb pain: a multicenter, double-blind, randomized controlled trial. Pain. 2025;166:571-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Annaswamy TM, Bahirat K, Raval G, Chung YY, Pham T, Prabhakaran B. Clinical feasibility and preliminary outcomes of a novel mixed reality system to manage phantom pain: a pilot study. Pilot Feasibility Stud. 2022;8:232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 28. | Teo WP, Muthalib M, Yamin S, Hendy AM, Bramstedt K, Kotsopoulos E, Perrey S, Ayaz H. Does a Combination of Virtual Reality, Neuromodulation and Neuroimaging Provide a Comprehensive Platform for Neurorehabilitation? - A Narrative Review of the Literature. Front Hum Neurosci. 2016;10:284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 102] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 29. | Makin TR, Flor H. Brain (re)organisation following amputation: Implications for phantom limb pain. Neuroimage. 2020;218:116943. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 30. | Osumi M, Inomata K, Inoue Y, Otake Y, Morioka S, Sumitani M. Characteristics of Phantom Limb Pain Alleviated with Virtual Reality Rehabilitation. Pain Med. 2019;20:1038-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 31. | Yoshimura M, Kurumadani H, Hirata J, Senoo K, Hanayama K, Sunagawa T, Uchida K, Gofuku A, Sato K. Case Report: Virtual reality training for phantom limb pain after amputation. Front Hum Neurosci. 2023;17:1246865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Rajendram C, Ken-Dror G, Han T, Sharma P. Efficacy of mirror therapy and virtual reality therapy in alleviating phantom limb pain: a meta-analysis and systematic review. BMJ Mil Health. 2022;168:173-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 33. | Ichinose A, Sano Y, Osumi M, Sumitani M, Kumagaya SI, Kuniyoshi Y. Somatosensory Feedback to the Cheek During Virtual Visual Feedback Therapy Enhances Pain Alleviation for Phantom Arms. Neurorehabil Neural Repair. 2017;31:717-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 34. | Chau B, Phelan I, Ta P, Humbert S, Hata J, Tran D. Immersive Virtual Reality Therapy with Myoelectric Control for Treatment-resistant Phantom Limb Pain: Case Report. Innov Clin Neurosci. 2017;14:3-7. [PubMed] |
| 35. | Abbas RL, Cooreman D, Sultan HA, Nayal ME, Saab IM, Khatib AE, Kawam AE, Melhat AME. Effect of Adding Virtual Reality Training to Traditional Exercise Program on Pain, Mental Status and Psychological Status in Unilateral Traumatic Lower Limb Amputees: A Randomized Controlled Trial. Games Health J. 2024;13:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 36. | Xiong J, Hsiang EL, He Z, Zhan T, Wu ST. Augmented reality and virtual reality displays: emerging technologies and future perspectives. Light Sci Appl. 2021;10:216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 232] [Article Influence: 58.0] [Reference Citation Analysis (0)] |
| 37. | Prahm C, Eckstein K, Bressler M, Wang Z, Li X, Suzuki T, Daigeler A, Kolbenschlag J, Kuzuoka H. PhantomAR: gamified mixed reality system for alleviating phantom limb pain in upper limb amputees-design, implementation, and clinical usability evaluation. J Neuroeng Rehabil. 2025;22:21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 38. | Giummarra M. Augmented reality for treatment of phantom limb pain-are we there yet? Lancet. 2016;388:2844-2845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 39. | Keesom E, Lidström-Holmqvist K, Ortiz-Catalan M, Pilch M, Lendaro E, Hermansson L, van der Sluis CK. Reducing phantom limb pain using phantom motor execution enabled by augmented and virtual reality: participants' perspectives on an innovative treatment. Disabil Rehabil. 2024;1-10. [PubMed] [DOI] [Full Text] |
| 40. | Lu L, Wang H, Liu P, Liu R, Zhang J, Xie Y, Liu S, Huo T, Xie M, Wu X, Ye Z. Applications of Mixed Reality Technology in Orthopedics Surgery: A Pilot Study. Front Bioeng Biotechnol. 2022;10:740507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 33] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 41. | Nazzal EM, Zsidai B, Hiemstra LA, Lustig S, Samuelsson K, Musahl V. Applications of Extended Reality in Orthopaedic Surgery. J Bone Joint Surg Am. 2023;105:1721-1729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Freschi C, Parrini S, Dinelli N, Ferrari M, Ferrari V. Hybrid simulation using mixed reality for interventional ultrasound imaging training. Int J Comput Assist Radiol Surg. 2015;10:1109-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 43. | Bahirat K, Annaswamy T, Prabhakaran B. Mr.MAPP: Mixed Reality for MAnaging Phantom Pain. Proceedings of the 25th ACM international conference on Multimedia, 2017. [DOI] [Full Text] |
| 44. | Annapureddy D, Annaswamy TM, Raval G, Chung YY, Prabhakaran B. A novel mixed reality system to manage phantom pain in-home: results of a pilot clinical trial. Front Pain Res (Lausanne). 2023;4:1183954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 45. | Wan Y, Gao H, Zhou K, Zhang X, Xue R, Zhang N. Virtual reality improves sleep quality and associated symptoms in patients with chronic insomnia. Sleep Med. 2024;122:230-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 46. | van 't Wout-Frank M, Arulpragasam AR, Faucher C, Aiken E, Shea MT, Jones RN, Greenberg BD, Philip NS. Virtual Reality and Transcranial Direct Current Stimulation for Posttraumatic Stress Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2024;81:437-446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 47. | Laver KE, Lange B, George S, Deutsch JE, Saposnik G, Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017;11:CD008349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 470] [Cited by in RCA: 426] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 48. | Drop DLQ, Vlake JH, Wils EJ, Van Bommel J, Jung C, Hilling DE, Bienvenu OJ, Korevaar TIM, Schut AFC, van Mol MMC, Gommers D, van Genderen ME. Effect of an intensive care unit virtual reality intervention on relatives´ mental health distress: a multicenter, randomized controlled trial. Crit Care. 2025;29:62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 49. | Ansari SA, Agrawal AP, Wajid MA, Wajid MS, Zafar A. MetaV: A Pioneer in feature Augmented Meta-Learning Based Vision Transformer for Medical Image Classification. Interdiscip Sci. 2024;16:469-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |