Published online Jun 18, 2025. doi: 10.5312/wjo.v16.i6.107292
Revised: April 17, 2025
Accepted: May 24, 2025
Published online: June 18, 2025
Processing time: 82 Days and 22.9 Hours
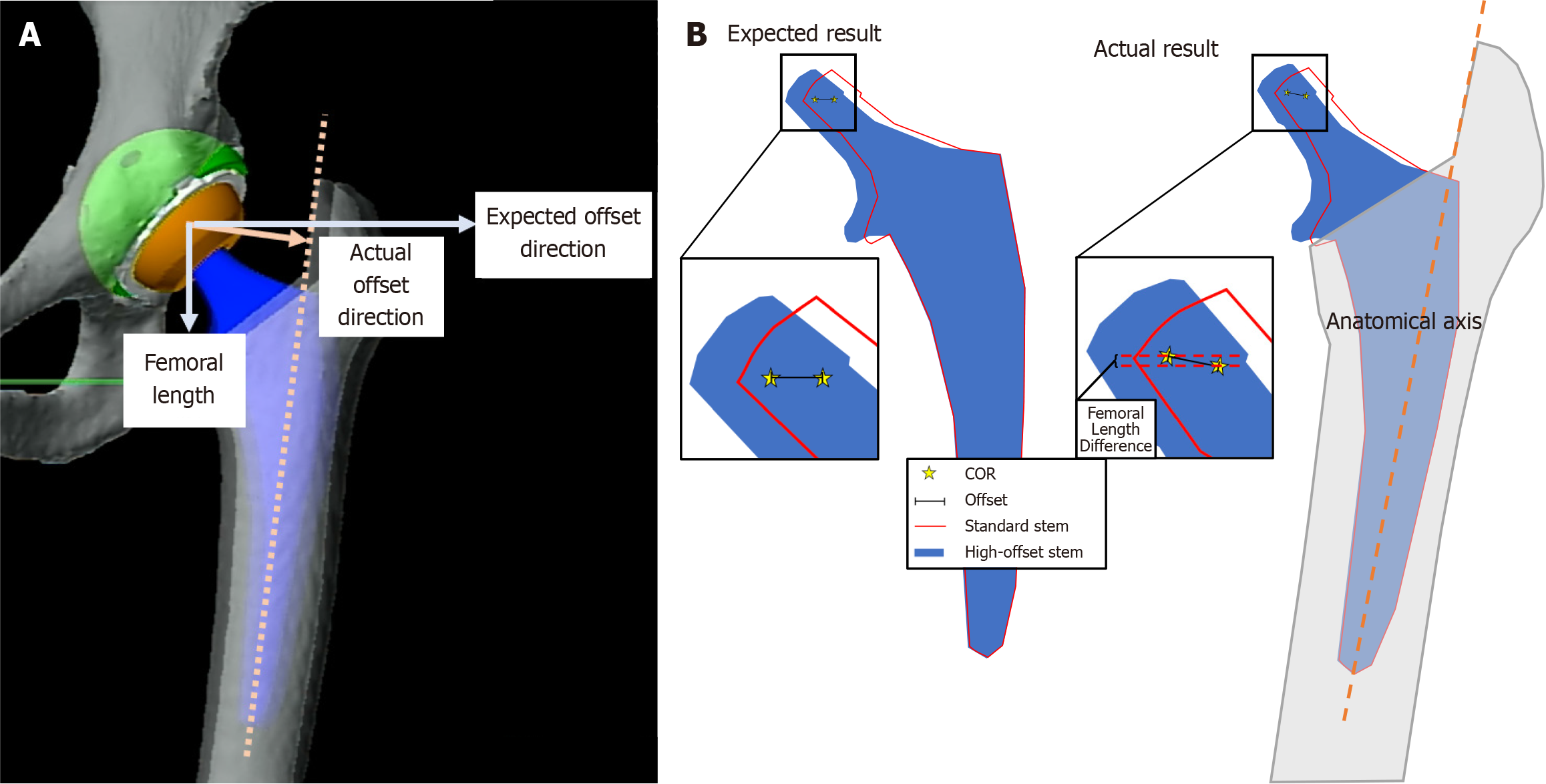
Certain implant combinations change leg length and offset in primary total hip arthroplasty (THA). Poor restoration of leg biomechanics is a frequently cited reason for patient dissatisfaction following primary THA. A pure high-offset stem should provide direct lateralization without affecting femoral length when compared to a standard stem. However, clinical experience with preoperative planning software based on computed tomography-based three-dimensional-models reveals that using pure high-offset stems in THA may cause a difference between expected (no change in femoral length) and actual (small increase) in postoperative femoral length.
To elucidate the causes of these femoral length discrepancies using preoperative planning software.
Preoperative templating for 43 robotic-assisted THAs, optimizing acetabular size and orientation, center of rotation, stem size and offset, and prosthetic head diameter were obtained. The preoperative planning software was used to calculate differences between preoperative and postoperative femoral length for standard and pure high-offset stems, unique to each patient.
Whilst the increase in femoral length between standard and high-offset stems was not significant (P = 0.93), 35 femurs (81.4%) experienced a 1-mm increase, and 3 (7.0%) experienced a 2-mm increase in femoral length while using high-offset stem compared to the standard stem. The incidence of femoral length increase was lower for patients with shorter femurs (18/22; 81.8%) compared to patients with longer femurs (20/21; 95.2%).
When pure high-offset stems were used in preoperative planning software, we demonstrated an unexpected increase in leg length between 1-2-mm in 88.4% of patients. This unexpected increase in femoral length is due to a function of the preoperative planning software’s planned stem alignment with the anatomical axis, and not an inherent fault in the stem design. With expanding accessibility of robotic-assisted THA platforms, all potential sources of postoperative leg length discrepancy should be identified during preoperative templating and necessary alterations to the surgical plan should be made to accommodate this unexpected difference when using a pure high-offset stem.
Core Tip: Discrepancies in leg length can result in patient dissatisfaction, complications, or even a need for revision. Surgeons should be aware of this unexpected increase in femoral length when using a pure high-offset stem in robotic-assisted total hip arthroplasty, especially for patients who may benefit from precise restoration of lower extremity biomechanics. With expanding accessibility of computer-navigated and robotic-assisted total hip arthroplasty platforms, any potential sources of postoperative leg length discrepancy should be identified during preoperative templating and necessary alterations to the surgical plan should be made to accommodate this unexpected difference when using a pure high-offset stem.
- Citation: Tung WS, Eslam Pour A, Sieberer J, Donnelley CA, Tommasini SM, Wiznia DH. Pure high-offset stems can cause an unexpected increase in femoral length in robotic-assisted primary total hip arthroplasty. World J Orthop 2025; 16(6): 107292
- URL: https://www.wjgnet.com/2218-5836/full/v16/i6/107292.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i6.107292
In primary total hip arthroplasty (THA), surgeons often choose implants based on familiarity, the implant’s effect on the center of rotation (COR), and the leg length and offset they wish to achieve through preoperative planning, intraoperative range of motion (ROM) tests, intraoperative computer navigation, and fluoroscopy[1]. Commonly, surgeons are concerned with hip ROM and impingement due to their contribution to postoperative subluxation and dislocation[2]. These factors can be improved by using larger femoral heads, high-offset stems, and plus (long) heads by increasing ROM and thus decreasing the risk of impingement, in addition to their positive effect on soft tissue tensioning and balancing, which can be protective against dislocation[3-6]. However, changing certain implant components to restore leg length, offset, and ROM may cause an iatrogenic change in leg length[6]. Restoration of leg length is critical as leg length discrepancy is a frequently cited reason for patient dissatisfaction following primary THA due to pain and patient perception of the difference[6-9].
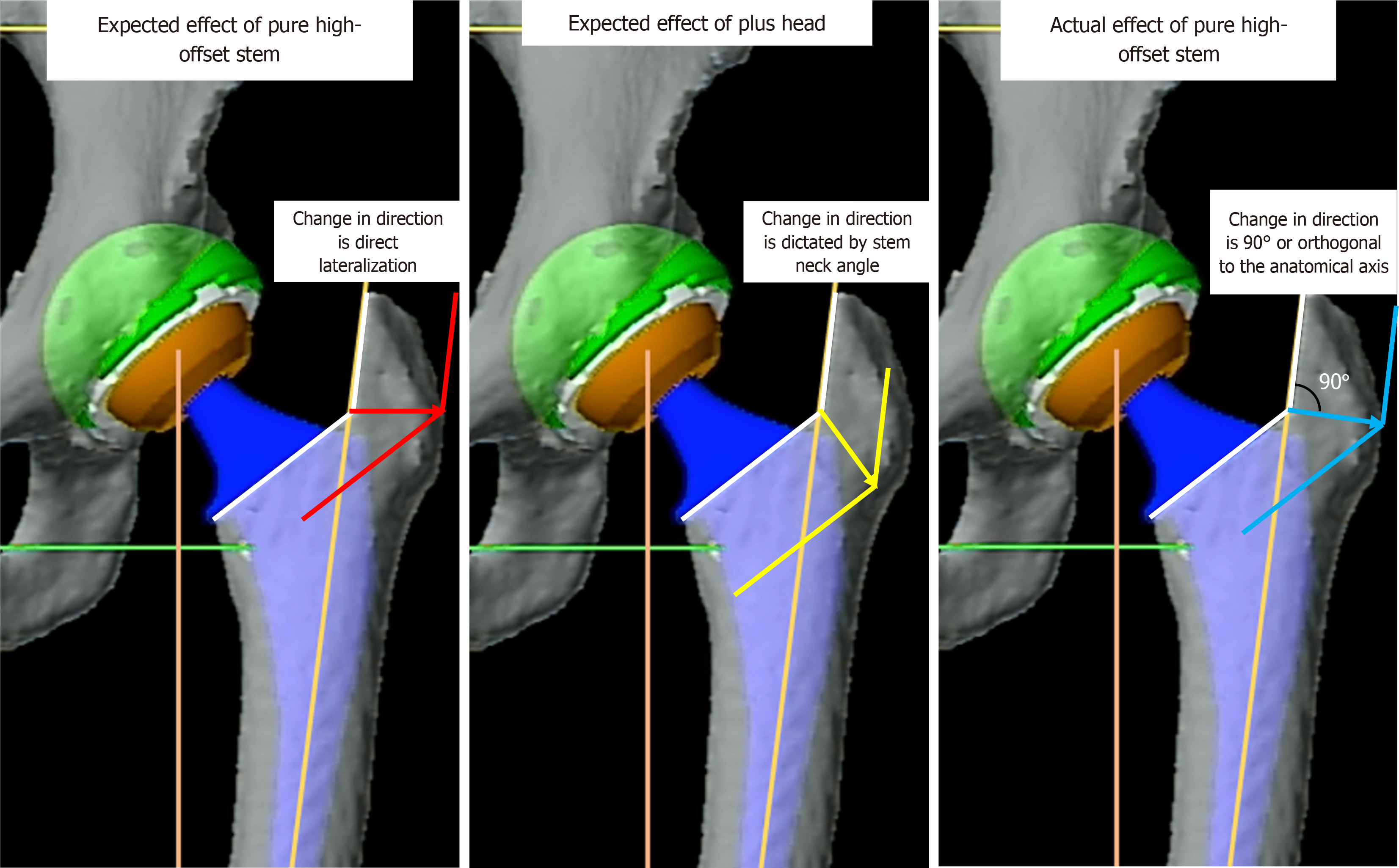
Precise restoration of femoral offset is another integral factor in ensuring the success of primary THA[6,10-13]. Offset can be optimized using a combination of surgical technique and implant design[1,3,6,14,15]. Reaming the acetabulum to a lesser degree and lateralizing the cup increases the offset, while reaming the acetabulum more and medializing the cup decreases the offset. For implant options, those that can increase offset include extended polyethylene liners, plus heads, and pure high-offset stem options that shift the neck component of the stem medially without changing the neck angle. Some stems also have different neck angle options. Stems with a lower neck angle can potentially increase horizontal offset, but they will decrease vertical offset. Plus (longer) heads will increase both horizontal and vertical offset, while minus (shorter) heads will decrease both horizontal and vertical offset.
Pure high-offset stems were introduced to surgeons with the guidance that a pure high-offset stem provides direct lateralization without affecting femoral length. However, it is the senior authors’ clinical experience with preoperative planning software and intraoperative testing verified with computer navigation that often reveals a minor increase between expected and actual postoperative femoral length when using a pure high-offset stem with a neutral head in the context of optimal stem and cup positioning and orientation. Therefore, the goal of this study is to: (1) Explore the rate of change in femoral length when using a pure high-offset stem with a neutral head on a preoperative planning platform; and (2) investigate the significance of this change in femoral length in patients with shorter or longer femurs. The secondary aim of this study is to compare the degree of femoral length increase between a standard stem with a neutral head, a pure high-offset stem with a neutral head, and a standard stem with a + 5 mm (plus) head. Consistent with extant literature, we hypothesize that the rate and magnitude of change in femoral length will be more accentuated in shorter patients due to the more prominent effect of femoral offset in this patient cohort[6].
This was a retrospective imaging and preoperative planning software analysis with data retrieved from the institution’s electronic medical records and preoperative planning for robotic-assisted primary THA software archives. Institutional Review Board exemption was obtained from Yale University, approval No. 2000032304.
A cohort of 42 patients who underwent primary THA via robotic-assisted surgery between February 1, 2021, and August 1, 2022, by a single surgeon at a single institution was identified. This study included patients aged 18-90 years who received primary THA for osteoarthritis, inflammatory arthritis, or avascular necrosis. As per the institution’s routine protocol, patients’ pelvic computed tomography (CT) scans and lateral lumbar radiographs in standing and relaxed sitting positions were obtained preoperatively. Our exclusion criteria were incomplete datasets, preoperative imaging, or three-dimensional (3D) modelling information. No patients were excluded, and our final sample included 42 patients (20 males and 22 females), with 1 patient receiving a staged bilateral primary THA for a total of 43 hips. The mean patient age was 58.1 years (range: 31.5-89).
After obtaining patient pelvic CT scans and lateral lumbar radiographs in standing and relaxed sitting positions, the imaging studies were imported to the preoperative planning software, MAKO™ Total Hip 4.1 preoperative planning was completed routinely for robotic-assisted THA to optimize acetabular implant size and orientation, COR, stem size and offset, and prosthetic head diameter. All surgeries were performed successfully, without any reported dislocations within the first postoperative year. Preoperative plans and data collected intraoperatively were used for simulation. The preoperative planning software provides the change between preoperative and postoperative leg length in rounded discrete millimeters for specific implant sizes, positioning, and orientation, unique to each patient’s anatomy.
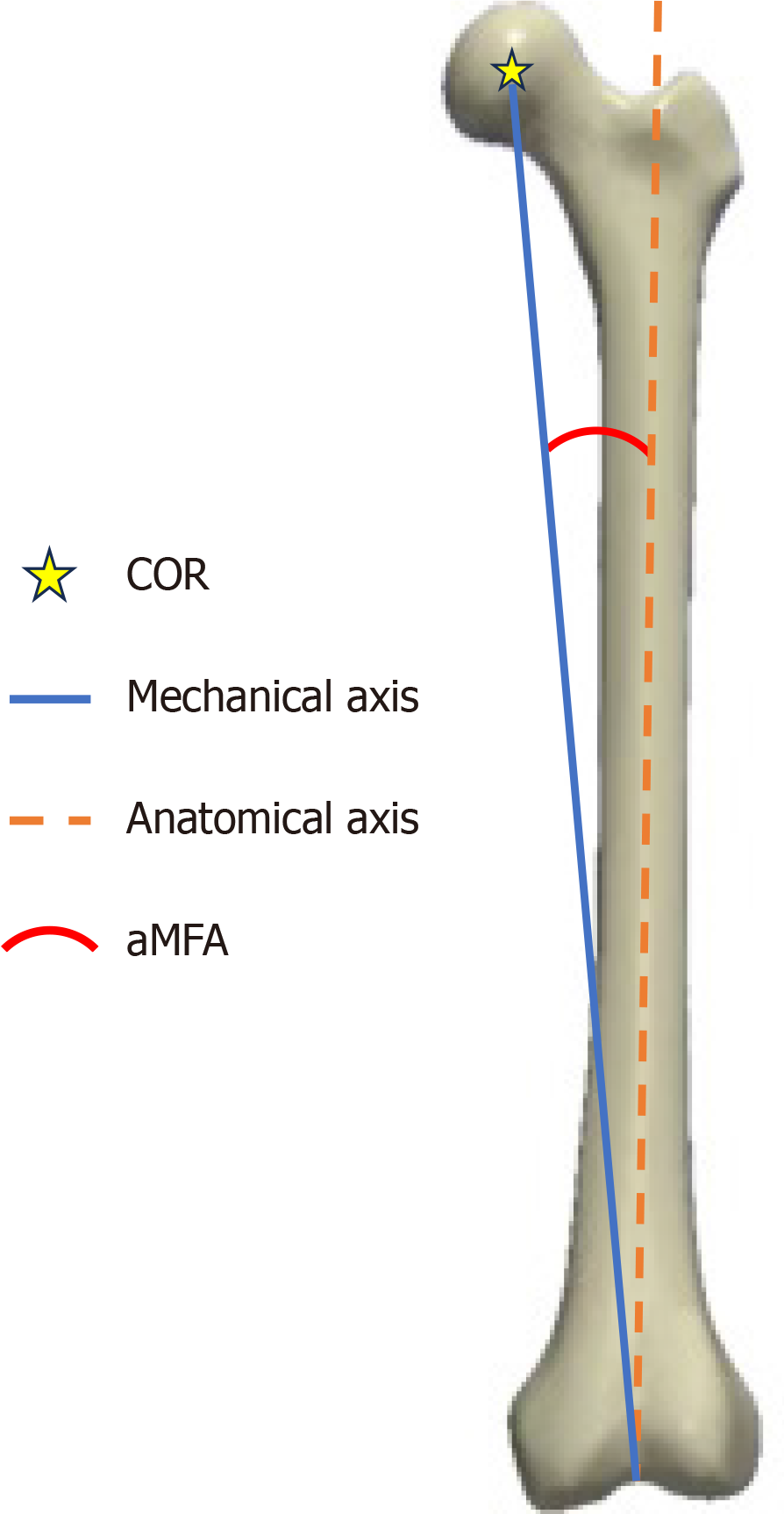
CT scans of patients undergoing primary robotic THA were downloaded and imported into Simpleware ScanIP (Synopsys, Mountain View, CA, United States) 3D segmentation software. Using the auto-segmentation function within the program, full 3D femur models of the operative laterality for each patient were recreated along with associated landmarks. The auto-segmentation tool identified the COR of the hip within the femoral head and the greater trochanter. For patients with severe hip deformity, the COR and greater trochanter were reidentified if necessary. The center of the intercondylar notch and any changes to the COR and greater trochanter were identified by a trained research fellow. Subsequently, the preoperative mechanical axis (distance between the COR and intercondylar notch), anatomical axis (distance between the greater trochanter and intercondylar notch), and angle between these two axes, or the anatomical mechanical femoral axis (aMFA), were measured (Figure 1). Femoral lengths of three different implant combinations: (1) Standard stem with a neutral head; (2) High-offset stem (5 mm lateralization) with a neutral head; and (3) Standard offset stem with a + 5 mm plus head, were measured for analysis. All simulations and measurements were obtained with 3D femur models using the Stryker Insignia® stem. Additionally, a subset of 10 femurs were selected and rated by another trained researcher for calculation of interrater reliability (IRR)[16].
Shapiro-Wilk normality tests were used to confirm that each series of measurements adhered to the Gaussian distribution. Linear regression models were used to elucidate the relationships between the native anatomical axis, as well as the native aMFA, and the increase in femoral length between the standard and high-offset stems with a neutral head. The native aMFA was chosen as a predictor as it provides a standardized value that demonstrates the relationship between the native anatomical axis and the femoral neck length. A Mann-Whitney U test was performed to determine any difference in central tendency of femoral length increase between the two groups stratified by the median length of the anatomical axis. Additionally, a Friedman Rank Sum test with post-hoc analysis was used to compare the difference in postoperative leg length of the three different implant combinations. IRR for the anatomical, mechanical axis, and aMFAs were calculated via two-way random, single measures, absolute agreement intraclass correlation coefficients in MATLAB 2023b and rated according to Koo and Li[16]. Additionally, the mean absolute disagreement between raters was calculated. Overall level of significance was set at a = 0.05 for all tests and individually adjusted by Bonferroni correction for each hypothesis to account for multiple hypothesis testing. 95% confidence intervals (CI) were reported where available. Post-hoc power analysis was not conducted as post-hoc power calculations are completely determined by the P value[17] Except IRR, all other data analyses were performed using R version 4.2.3 (The R Foundation for Statistical Computing, Vienna, Austria).
The mean anatomical axis length was 438 mm (SD: 29.5 mm), the median native mechanical axis length was 431 mm (SD: 29.0 mm), the median native femoral neck length was 48.4 mm (SD: 5.2 mm), and the median native aMFA was 6.3° (SD: 0.6°). More in-depth descriptive statistics are detailed in Table 1. Postoperative increase in femoral length between implant combinations ranged from 0-5 mm. The rate and specific ranges in femoral length increase, as well as their medians, between each combination are detailed in Table 2.
| Measure | Mean | SD | Median | IQR |
| Anatomical axis (mm) | 438 | 29.5 | 438 | 414-454 |
| Native mechanical axis (mm) | 431 | 29.0 | 427 | 407-450 |
| Native femoral neck length (mm) | 48.4 | 5.2 | 44.9 | 45.7-51.9 |
| Native aMFA (degrees) | 6.3 | 0.6 | 6.3 | 6.1-6.8 |
| Leg length difference in millimeters | Median (mm) | 0 | 1 | 2 | 3 | 4 | 5 |
| Standard vs high offset | 1 | 5 | 35 | 3 | - | - | - |
| High offset vs plus head | 2 | - | - | 29 | 13 | 1 | - |
| Standard vs plus head | 3 | - | - | - | 31 | 11 | 1 |
The Friedman Rank Sum test detected significant differences in the increase in femoral length between a standard stem with a neutral head, a standard stem with a + 5 mm head, and a high-offset stem with a neutral head (P < 0.0001). Post-hoc analysis with Bonferroni correction showed a significant difference in the increase in femoral length between a standard stem with neutral and + 5 mm head (P = 0.008). No other significant associations were found.
There was a strong positive relationship between the length of the anatomical axis and mechanical axis [coefficient: 0.961; CI: (0.900-1.022); P < 0.0001]. There was no association between native aMFA and the anatomical axis. Furthermore, linear regression models found no associations between the length of the native anatomical axis and an increase in femoral length (P = 0.97), nor the native aMFA and an increase in femoral length (P = 0.23).
Further analysis was conducted to compare the effects of standard and high-offset stems with a neutral head between patients with shorter (≤ 437 mm) and longer femurs (> 437 mm), based on the median length of the native anatomical axis. There was no significant difference found between an increase in femoral length for shorter and longer femurs (P = 0.48) using these two different implant constructs. However, four patients (18.2%) with shorter femurs had no increase in femoral length compared to 1 patient (4.8%) with a longer femur. As well, 2 patients (9.1%) with shorter femurs had an increase in femoral length of 2 mm compared to 1 patient (4.8%) with a longer femur. All other femurs in both groups had an increase in femoral length of 1 mm. IRR of the mechanical and anatomical axis measurement was excellent (both 95%CI: 0.99-1.00), with a mean absolute disagreement of 1.25 and 1.10 mm, respectively. IRR of aMFA was good to excellent with an intraclass correlation coefficients of 0.97 (95%CI: 0.82, 0.99), and a disagreement of 0.17 degrees.
Using a preoperative planning platform, the effect of a presumed pure high-offset stem on the rate and degree of increase in femoral length was demonstrated. Within our study cohort, 38 (88.4%) femurs experienced an increase in femoral length when a pure high-offset stem was used compared to a standard stem during preoperative templating. This increase has been confirmed to be a real difference, and this is not attributable to the implant design, but instead to how leg length is measured in the preoperative planning platform. The planned stem axis is aligned to the anatomical axis of the femur, or the expected trajectory of the femoral component of the prosthesis inside the femoral canal, and not directly aligned with the mechanical axis along which the length of the femur is measured relative to the ground (Figure 2). Hence, when a high-offset stem is used, the offset is added orthogonally to the anatomical axis of the femur, but not to the mechanical axis. Therefore, in this specific preoperative planning platform, a pure high-offset stem provides a lateral component and a small distal displacement component. Consequently, intraoperative placement of a pure high-offset stem translates the distal displacement of the femur observed during preoperative templating into a physical difference. The finding that a pure high-offset stem may increase leg length between 1-3 mm is contrary to commonly held understandings of the design and function of these implants.
Despite this finding, it is important to note that this combined displacement using a pure high-offset stem is not equivalent to the expected increase in offset and leg length when using a plus head. To demonstrate this, the effects of these two implants were represented visually (Figure 3) and the increase in femoral length between a high-offset stem with a neutral head and a standard stem with a + 5 mm head were calculated. If the effect on offset and leg length were equivalent between these two implant combinations, then no increase in femoral length would be expected. However, all femurs experienced an increase in femoral length to some degree, ranging from 2-4 mm (P < 0.0001). This increase in femoral length observed when a plus head is used is an expected consequence and is not attributed to how the stem axis is planned. Instead, when changing the length of the femoral head, the resultant position of the femur is completely dictated by the stem neck angle.
Post-hoc analysis with Bonferroni adjustment of the Friedman Rank Sum test found no significant difference in the increase in femoral length between standard and high-offset stems. While this analysis was not statistically significant, this increase between expected and actual femoral length can be observed clinically when using a computer-navigated or robotic-assisted THA platform. Most femurs in our cohort (35/43; 81.4%) experienced 1 mm (range: 0.50-1.49 mm) of femoral length increase, while 3 (7.0%) experienced 2 mm (range: 1.50-2.49 mm) of femoral length increase. Although many patients can often tolerate minor leg length discrepancy (LLD) of less than 10 mm, most can perceive a discrepancy of 5 mm or more[9,18]. If a surgeon can accept an overall LLD of 2 mm but does not realize that a high offset stem can also cause a change in the femoral length, then the cumulative effect has the potential to impact the patient. Irrespective of the objective difference in leg length, some may still find minute discrepancies a significant source of poor clinical outcomes and patient-reported outcome measures, as well as dissatisfaction[6,8,9,19,20].
It is also crucial to note that the overall discrepancy in leg length and its perception is multifactorial. While changes in anatomical femoral length are important, other factors such as knee alignment, deformities of the foot or spine, abductor muscle weakness, and pelvic obliquity can also cause patients to complain of suboptimal results. Therefore, the clinical impact of an increase in femoral length cannot be assessed as an independent factor[21]. Nonetheless, surgeons should be cognizant of even the most minute changes in femoral length, especially in patients where the precise restoration of biomechanics is critical in the context of moderate to severe preoperative deformity.
Consistent with extant literature, we hypothesized that the rate and degree of increase in femoral length would be more accentuated in shorter patients due to the more prominent effect of femoral offset in this patient cohort[6]. However, our 3D analysis found no significant difference when comparing the central tendency of femoral length increase between patients with shorter and longer femurs (P = 0.48). Additionally, the incidence of femoral length increase was also lower for patients with shorter femurs (81.8%) compared to patients with longer femurs (95.2%). Hence, this study shows that patients with shorter femurs may be less likely to be affected by the unexpected vertical displacement when using a pure high-offset stem, but both patient cohorts will inevitably benefit from closer inspection of the preoperative template to restore leg length optimally.
There are some limitations to this study. First, a sample of 43 hips was insufficient to detect a small effect of 1-2 mm of femoral length increase. Detecting a small effect size (Cohen’s d = 0.2) will require approximately 350 models. We do not currently have access to CT scans of that number, and do not have the engineering capacity to develop 3D models for such a large number of patients. Nonetheless, although femoral length increase may not have been statistically significant with our sample size, we believe that this study is sufficient to bring awareness of this unexpected increase in leg length in preoperative planning platforms that align the planned stem axis closer to the anatomical axis in situ, rather than the mechanical axis. Secondly, the results of this study were produced with only one stem design and robotic-assisted THA preoperative planning platform from one manufacturer. However, these results should still be applicable to other pure high-offset stems utilizing similar preoperative templating from other companies.
This study demonstrates a high incidence of unexpected increases in femoral length when using a pure high-offset stem during preoperative planning. This unexpected increase is due to a vector component of the high-offset stem projecting perpendicularly to the anatomical axis, inadvertently contributing to femoral lengthening. Discrepancies in leg length can result in patient dissatisfaction, complications, or even a need for revision. Surgeons should be aware of this unexpected result, especially for patients who may benefit from precise restoration of lower extremity biomechanics. Surgical teams using robotic-assisted systems should proactively inspect preoperative planning outputs cautiously for discrepancies and consider adjustments to mitigate unexpected lengthening. With expanding accessibility of computer-navigated and robotic-assisted THA platforms, any potential sources of postoperative LLD should be identified during preoperative templating, and necessary alterations to the surgical plan should be made to accommodate this unexpected difference when using a pure high-offset stem.
| 1. | Pour AE, Donnelley CA, Tung WS, Tommasini SM, Wiznia D. Some Offset Restoration Options Can Paradoxically Lead to Decreased Range of Motion in Primary Total Hip Arthroplasty: A 3-Dimensional Computer Simulation Study. J Arthroplasty. 2024;39:514-519.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Tung WS, Donnelley C, Eslam Pour A, Tommasini S, Wiznia D. Simulating movements of daily living in robot-assisted total hip arthroplasty with 3D modelling. Bone Jt Open. 2023;4:416-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Bourne RB, Rorabeck CH. Soft tissue balancing: the hip. J Arthroplasty. 2002;17:17-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 139] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Ogawa T, Takao M, Hamada H, Sakai T, Sugano N. Soft tissue tension is four times lower in the unstable primary total hip arthroplasty. Int Orthop. 2018;42:2059-2065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Lavigne M, Ganapathi M, Mottard S, Girard J, Vendittoli PA. Range of motion of large head total hip arthroplasty is greater than 28 mm total hip arthroplasty or hip resurfacing. Clin Biomech (Bristol). 2011;26:267-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Boe RA, Selemon NA, Eachempati KK, Paprosky WG, Sheth NP. Soft-Tissue Balancing in Total Hip Arthroplasty. JBJS Rev. 2021;9:e20.00116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Licini DJ, Burnikel DJ, Meneghini RM, Ochsner JL. Comparison of limb-length discrepancy after THA: with and without computer navigation. Orthopedics. 2013;36:e543-e547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Mahmood SS, Mukka SS, Crnalic S, Sayed-Noor AS. The Influence of Leg Length Discrepancy after Total Hip Arthroplasty on Function and Quality of Life: A Prospective Cohort Study. J Arthroplasty. 2015;30:1638-1642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Desai AS, Dramis A, Board TN. Leg length discrepancy after total hip arthroplasty: a review of literature. Curr Rev Musculoskelet Med. 2013;6:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 131] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 10. | Matsushita A, Nakashima Y, Jingushi S, Yamamoto T, Kuraoka A, Iwamoto Y. Effects of the femoral offset and the head size on the safe range of motion in total hip arthroplasty. J Arthroplasty. 2009;24:646-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 109] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Hayashi S, Nishiyama T, Fujishiro T, Hashimoto S, Kanzaki N, Nishida K, Kuroda R, Kurosaka M. Excessive femoral offset does not affect the range of motion after total hip arthroplasty. Int Orthop. 2013;37:1233-1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Forde B, Engeln K, Bedair H, Bene N, Talmo C, Nandi S. Restoring femoral offset is the most important technical factor in preventing total hip arthroplasty dislocation. J Orthop. 2018;15:131-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Snijders TE, van Erp JHJ, de Gast A. Restoring femoral offset and leg length; the potential of a short curved stem in total hip arthroplasty. J Orthop. 2019;16:396-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Charles MN, Bourne RB, Davey JR, Greenwald AS, Morrey BF, Rorabeck CH. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect. 2005;54:131-141. [PubMed] |
| 15. | Vigdorchik JM, Sharma AK, Madurawe CS, Elbuluk AM, Baré JV, Pierrepont JW. Does Prosthetic or Bony Impingement Occur More Often in Total Hip Arthroplasty: A Dynamic Preoperative Analysis. J Arthroplasty. 2020;35:2501-2506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 16. | Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15:155-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9979] [Cited by in RCA: 15924] [Article Influence: 1769.3] [Reference Citation Analysis (0)] |
| 17. | Althouse AD. Post Hoc Power: Not Empowering, Just Misleading. J Surg Res. 2021;259:A3-A6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 18. | Sykes A, Hill J, Orr J, Humphreys P, Rooney A, Morrow E, Beverland D. Patients' perception of leg length discrepancy post total hip arthroplasty. Hip Int. 2015;25:452-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 19. | Mahoney CR, Pellicci PM. Complications in primary total hip arthroplasty: avoidance and management of dislocations. Instr Course Lect. 2003;52:247-255. [PubMed] |
| 20. | Parvizi J, Sharkey PF, Bissett GA, Rothman RH, Hozack WJ. Surgical treatment of limb-length discrepancy following total hip arthroplasty. J Bone Joint Surg Am. 2003;85:2310-2317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 126] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 21. | Lazennec JY, Folinais D, Florequin C, Pour AE. Does Patients' Perception of Leg Length After Total Hip Arthroplasty Correlate With Anatomical Leg Length? J Arthroplasty. 2018;33:1562-1566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |