Published online Jun 18, 2025. doi: 10.5312/wjo.v16.i6.106871
Revised: April 8, 2025
Accepted: May 24, 2025
Published online: June 18, 2025
Processing time: 100 Days and 21 Hours
Radial head fractures constitute approximately one-third of all elbow fractures, significantly impacting the young and active population. While open reduction and internal fixation is the preferred treatment for displaced fractures, its high complication rate in comminuted fractures has led to the increasing use of radial head arthroplasty (RHA). RHA provides improved functional outcomes with fewer complications, yet its long-term efficacy remains a topic of debate.
To evaluate the functional outcomes of patients undergoing RHA with a modular metallic prosthesis for comminuted Mason type III and IV radial head fractures.
A prospective and retrospective hospital-based study was conducted at Dayanand Medical College and Hospital, Ludhiana over 32 months (January 2021-August 2023). A total of 26 patients with Mason type III and IV fractures were included, with six retrospective and 20 prospective cases. Functional outcomes were assessed using the Mayo Elbow Performance Score (MEPS), elbow range of motion, pain via Visual Analog Scale, and activities of daily living at immediate postoperative, three-month, and six-month follow-ups.
MEPS at 6 months follow up for 4 cases (15.38%) had good scores, and 22 cases (84.62%) had excellent scores, with a mean ± SD of 97.31 ± 6.67. Comparisons showed significant improvement from immediate post-operative to 3 months (P < 0.0001), from immediate post-operative to 6 months (P < 0.0001), and between 3 months and 6 months (P < 0.0001). None of the patients had elbow instability after radial head replacement and 22 cases (84.62%) had no complications, while 3 cases (11.54%) had a stiff elbow, and 1 case (3.85%) had heterotopic ossification.
RHA is an effective treatment for comminuted radial head fractures, providing stable elbow function with minimal complications.
Core Tip: Radial head arthroplasty is an effective treatment modality to restore the stability and congruency of elbows with comminuted radial head fractures (Mason type III and IV). In our study there was a significant improvement in the range of motion involving flexion, extension deficit, supination and pronation during the follow up period with minimal compli
- Citation: Bindal S, Pooni HS, Garg R, Jain D. Functional outcomes of radial head arthroplasty in Mason type III and IV fractures. World J Orthop 2025; 16(6): 106871
- URL: https://www.wjgnet.com/2218-5836/full/v16/i6/106871.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i6.106871
Elbow fractures make up about 5% of all fractures, with radial head fractures comprising approximately one-third of these cases. Given the relatively high incidence, this condition can adversely affect a considerable portion of the young and active population[1].
Radial head injuries range from minimal displacement to large, comminuted fractures with accompanying bone and ligament injuries. These injuries often result from an application of axial load to the forearm, causing the “radial head to impact the capitellum of the humerus, such as during a fall on an outstretched hand”. The management varies on the severity of these fractures from minimal treatment to surgical excision, or replacement[1-3].
The primary treatment for such fractures is open reduction internal fixation also known as open reduction and internal fixation (ORIF). It is highly effective in reducing the fractures and aiding in union, especially in cases of displaced fractures of radial head with minimal comminution. However, in case of comminuted fractures, the complications rate may be high enough and the procedure may become unsuccessful[4-6]. Radial head arthroplasty (RHA) also known as RHA is an alternative to ORIF with comparable results in terms of efficacy with minimal complications[7]. Compared to the past where excision of the radial head was performed for severely displaced and comminuted radial head fractures, in today's world RHA has become popular in view of the complications following excision such as instability of the valgus elbow, stiffness, decreased grip strength and proximal migration of the radius[8]. Nowadays, RHA forms the primary treatment for a variety of radial head fractures which may even be accompanied by other injuries of ligament or bone. Also, for patients who have complications or failure of fixation following ORIF, RHA becomes the primary cornerstone for treatment[9,10].
The surgical treatment of comminuted radial head fractures (modified Mason types III and IV) presents significant challenges and is still a topic of debate. Options include ORIF, radial head resection, and RHA, with no clear consensus on the best approach[11]. Previous systematic reviews and meta-analyses have assessed the outcomes of ORIF and RHA. One meta-analysis found that the optimal surgical method for radial head and neck fractures depends on the Mason classification (ORIF for type II and RHA for types III and IV)[12]. Majority of the meta-analyses indicate that RHA offers better elbow function and fewer complications compared to ORIF for Mason type III fractures in the short term. However, the quality of this evidence is low, and many studies on radial head replacement involve a diverse group of patients, various treatments, and different outcome measures[13,14]. These studies often do not distinguish between acute or delayed treatment, isolated radial head fractures vs those with associated injuries, or the use of different types of implants. Further, limited studies have been conducted about radial head replacement outcomes in Indian population.
Selecting the best treatment for Mason type III and IV radial head fractures requires evaluating multiple factors. These include stability of the fracture, degree of displacement, comminution, the extent of articular involvement, and the presence of any associated injuries to the forearm or elbow. While classification systems can inform treatment decisions, they should not be the sole determinant.
The Mason classification system aims to categorize treatment options, though Mason type III fracture treatments remain contentious. Non-operative treatments often lead to poor outcomes. Fragment excision is seldom recommended; however, if fragments constitute less than 25% of the radial head's surface area and elbow stability is maintained, excision without replacement is possible. For Mason type III fractures where ORIF are impractical, radial head replacement is suggested. Fractures with three or more fragments treated with ORIF may result in unpredictable ulno-humeral and forearm motion, fixation failure, fragment nonunion, and osteonecrosis[15,16].
Using metallic radial head prosthesis to stabilize the elbow is attractive due to the frequent failure of internal fixation in multi-fragmentary and displaced fractures of the radial head. Radial head replacement has been associated with enhanced patient satisfaction, reduced complications, and superior outcomes compared to ORIF[14].
This study aims to provide data on the functional outcomes of up to six months for patients undergoing RHA with a modular metallic prosthesis for irreparable mason type III and IV radial head fractures. An irreparable Mason type III or IV fracture refers to a comminuted radial head fracture in which anatomical reconstruction is not feasible due to the extent of fragmentation, displacement, or bone loss, making stable fixation with internal hardware unreliable.
With a focus on the Indian population, this study calls for a particular assessment of several contextual elements. Injuries typically include high-energy trauma, such as traffic accidents or work-related injuries, which can lead to more complex fracture patterns. Patients also frequently arrive later because they have less access to expert orthopedic treatments. Additionally, the availability of resources and socioeconomic circumstances might impact treatment options, which can impact the time and selection of surgical intervention. Notwithstanding these factors, the results of RHA in India are not well documented, underscoring the necessity of doing research tailored to the region to help guide clinical practice.
This study was conducted over a period of thirty-two months from 1st January 2021 to 31st August 2023 (fourteen months retrospectively, from 1st January 2021 to 28th February 2022 and eighteen months prospectively, from 1st March 2022 to 31st August 2023).
The study was a retrospective and prospective hospital-based study.
The study was conducted at Dayanand Medical College and Hospital, which is tertiary care, referral hospital of North India.
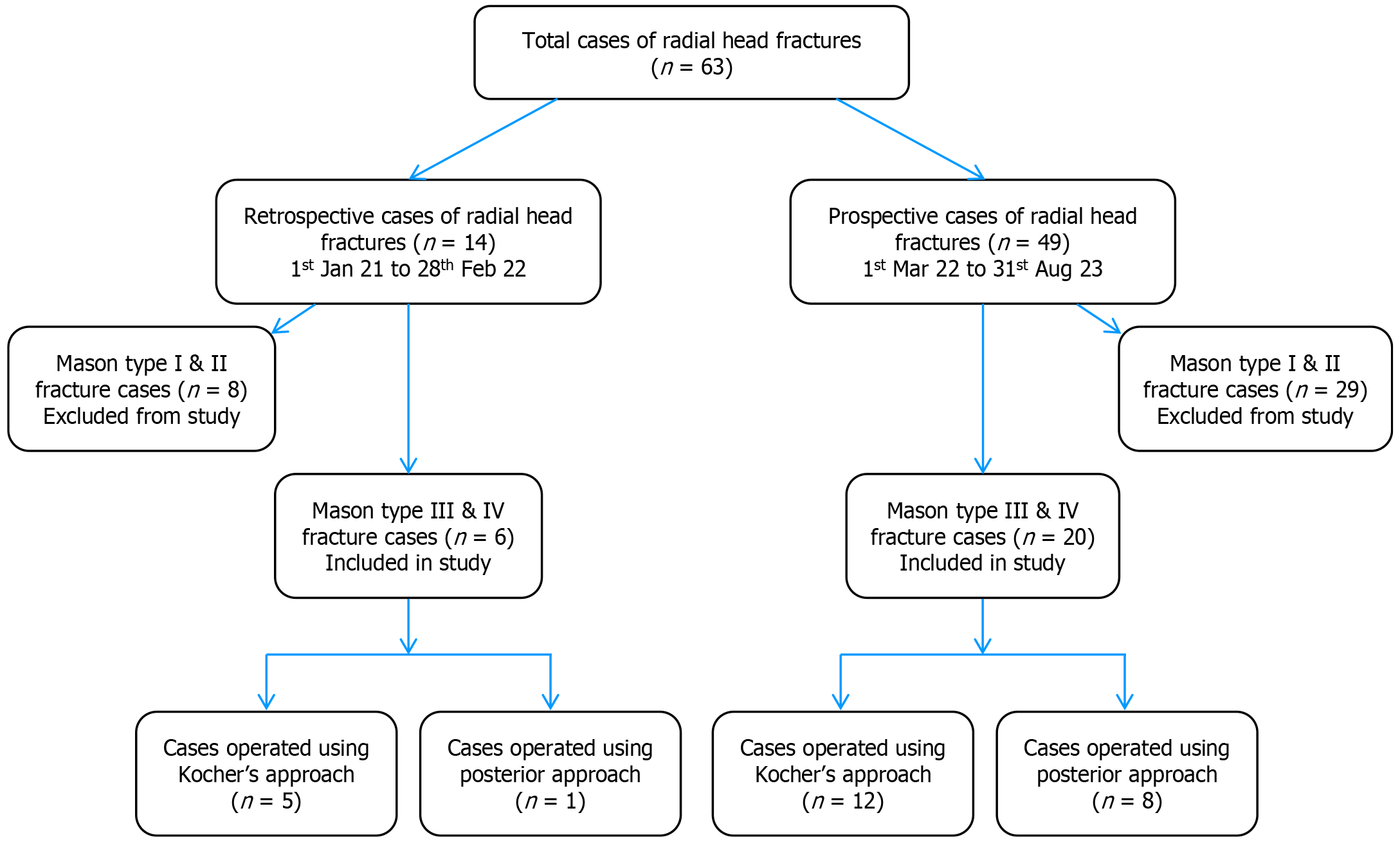
All patients admitted to Dayanand Medical College and Hospital, with Mason type III and IV radial head fractures scheduled to undergo radial head replacement between 1st January 2021 and 31st August 2023 were selected for the study. Six retrospective cases and twenty prospective cases were identified according to inclusion and exclusion criteria, and a total sample size of twenty-six cases was obtained (Figure 1).
The sample size for the study was calculated by formula taking the results of a previous study by Kulkarni et al[17] 65 as reference. The study observed that Mayo Elbow Performance Score (MEPS) demonstrated poor outcomes in 1 (3.33%) patient. With 7.5% margin of error and 5% level of significance, after formula application, the minimum samples needed were 22 patients.
n ≥ [P (1 - P)]/(ME/Zα)2
Where Zα is value of Z at two-sided alpha error of 5%, ME is margin of error, P is proportion of patients with poor outcome.
n ≥ [0.033 × (1-0.033)]/(0.075/1.96)2 = 21.79 = 22 (approx).
In our study, 26 patients were enrolled, which represents an approximately 18% increase over the minimum requirement. A post hoc power analysis based on these parameters indicates that our study achieved an estimated power of approximately 85% to detect a clinically significant difference in functional outcomes.
All patients presenting with Mason type III and IV radial head fractures planned for RHA. All patients undergoing RHA using metallic head implant prosthesis (cobalt chromium and titanium head implants). Patients undergoing radius head arthroplasty by any surgical approach (posterior, medial, lateral, anterior or global approaches).
Any patient not giving consent. Any patient below the age of eighteen years or with incomplete fusion of epiphysis. Any patient with radial head fracture planned for ORIF or radial head excision. Any patient with pre-existing prosthesis or metal work in situ.
All patients were evaluated based on MEPS, elbow flexion, elbow extension deficit, supination and pronation, in the immediate post-operative period, at 3 months and then at 6 months respectively to analyse the functional outcomes in patients. Standard predesigned structured proforma was filled in direct interview with patient.
The study was conducted in the Department of Orthopaedics, Dayanand Medical College and Hospital, Ludhiana over a period of thirty-two months from 1st January 2021 to 31st August 2023, after due approval from the institutional ethics committee and review board (Faculty of Medical Sciences, Dayanand Medical College and Hospital, No. BFUHS/2K23p-TH/62).
Written informed consent was obtained from all participants in the study. For prospective cases, consent was secured at the time of enrollment after providing a detailed explanation of the study’s purpose, procedures, and potential risks. For retrospective cases, written consent was obtained either during routine follow-up visits or, when in-person follow-up was not feasible, through documented telephone communication followed by mailed consent forms. This approach ensured that all participants, regardless of the time of enrollment, were adequately informed and voluntarily agreed to the use of their clinical data for research purposes. The study protocol was reviewed and approved by the institutional ethics committee, and all procedures adhered to relevant ethical guidelines and regulations.
Six retrospective cases, between January 2021 and February 2022 and twenty prospective cases, between March 2022 and August 2023, above the age of eighteen with Mason type III or IV radial head fractures were enrolled in the study. The demographic details included age, gender, religion and occupation of the patient. Details of mode of injury, type of fracture, and associated injuries were noted. Detailed preoperative history was taken. Physical examination was conducted prior to surgery. The patient was provided with a detailed explanation of the procedure through a patient information sheet.
Surgical approach was either Kocher's or posterior, based on treatment of associated injuries around the elbow joint. Cases with associated fractures of the olecranon with radial head fracture (Mason type III or type IV) were treated using the posterior approach. Cases with isolated radial head fractures or radial head fractures (Mason type III or IV) associated with fracture of coronoid process or collateral ligament injuries of the elbow were treated using Kocher’s approach.
In the Kocher’s approach, Kocher interval was identified between the extensor carpi ulnaris and anconeus muscles. Proximal fibres of the supinator muscle were split staying on the posterior cortex of the radius away from the posterior interosseous nerve. Annular ligament was divided in line with the muscle interval and capsule was incised longitudinally to expose the radial head.
In the posterior approach Olecranon osteotomy was performed and the olecranon fragment was retracted proximally with the attached triceps muscle. Fascia covering anconeus and extensor carpi ulnaris was identified and incised longitudinally. Anconeus and extensor carpi ulnaris were elevated subperiosteally to reveal the supinator muscle which was also elevated, capsule was identified and incised to expose the radial head.
The OSKARTM Radial Head Implant (Biotek, India) was used for RHA in all patients. This titanium, one-piece intramedullary-stemmed prosthesis is intended to retain joint space and the relationships of the proximal radio-ulnar and radio-humeral joints. Seven sizes of the implant are available to meet different anatomical requirements. The prosthesis was press-fit without the use of cement, adhering to the manufacturer’s surgical protocol.
All patients underwent a uniform rehabilitation protocol following surgery. Initially, the elbow was placed in a posterior splint at 90 degrees of flexion for 5 days to 7 days to support soft tissue recovery. Thereafter, patients began a structured physiotherapy program, starting with passive range-of-motion exercises, progressing to active-assisted movements, and eventually to active mobilization. Strengthening exercises were typically introduced around the six-week mark, based on individual recovery progress. Both prospective and retrospective cases followed the same physiotherapy regimen, as outlined in the institution’s standard rehabilitation protocol, ensuring consistency in post-operative management.
Duration of surgery and blood loss during surgery were noted. Assessment of elbow flexion, elbow extension deficit, supination, pronation at immediate post-operative, post-operative 3 months and 6 months was done. Assessment of pain by Visual Analog Scale (VAS) score, motion arc, elbow joint stability, activities of daily living (ADL) and MEPS at immediate post-operative, post-operative 3 months and 6 months was done for all prospective cases. For retrospective cases, data was obtained from retrospective analysis of inpatient file data and monthly follow up outpatient department cards. Data on assessment of pain, ADL and MEPS was obtained using direct interview with the patient.
To address the potential for selection and recall bias introduced by the inclusion of six retrospective cases, several measures were implemented. The same inclusion and exclusion criteria were applied uniformly across all cases and a standardized data extraction proforma was used to ensure consistency between retrospective and prospective cases. Clinical and radiographic data were cross verified with hospital records to minimize inaccuracies. Additionally, all cases were evaluated using uniform assessment methods, including the MEPS, goniometric range of motion (ROM) measurements, and VAS for pain. To further assess the impact of retrospective data, a sensitivity analysis was conducted, confirming that their inclusion did not significantly alter study outcomes. These steps were taken to enhance the study’s internal validity and mitigate potential biases (Figure 2).
The presentation of the Categorical variables was done in the form of number and percentage (%). The quantitative data were presented as the means ± SD and as median with 25th and 75th percentiles (interquartile range). Shapiro-Wilk test was used for assessing data normality. The cases in which the data was not normal, we used nonparametric tests. The following statistical tests were applied for the results: (1) The comparison of the variables which were quantitative and not normally distributed in nature were analysed using Friedman Test followed by multiple pairwise comparisons using Nemenyi's procedure and variables which were quantitative and normally distributed in nature were analysed using repeated measure analysis of variance followed by multiple pairwise comparisons using Bonferroni correction for paired comparison; (2) The comparison of the variables which were quantitative and not normally distributed in nature were analysed using Mann-Whitney Test and variables which were quantitative and normally distributed in nature were analysed using independent t test; and (3) The comparison of the variables which were qualitative in nature were analysed using Bhapkar test for paired proportions. The comparison of the variables which were qualitative in nature were analysed using Fisher’s exact test as at least one cell had an expected value of less than 5.
The data entry was done in the Microsoft EXCEL spreadsheet, and the final analysis was done with the use of Statistical Package for Social Sciences software, IBM manufacturer, Chicago, United States, ver 25.0. For statistical significance, P value of less than 0.05 was considered statistically significant.
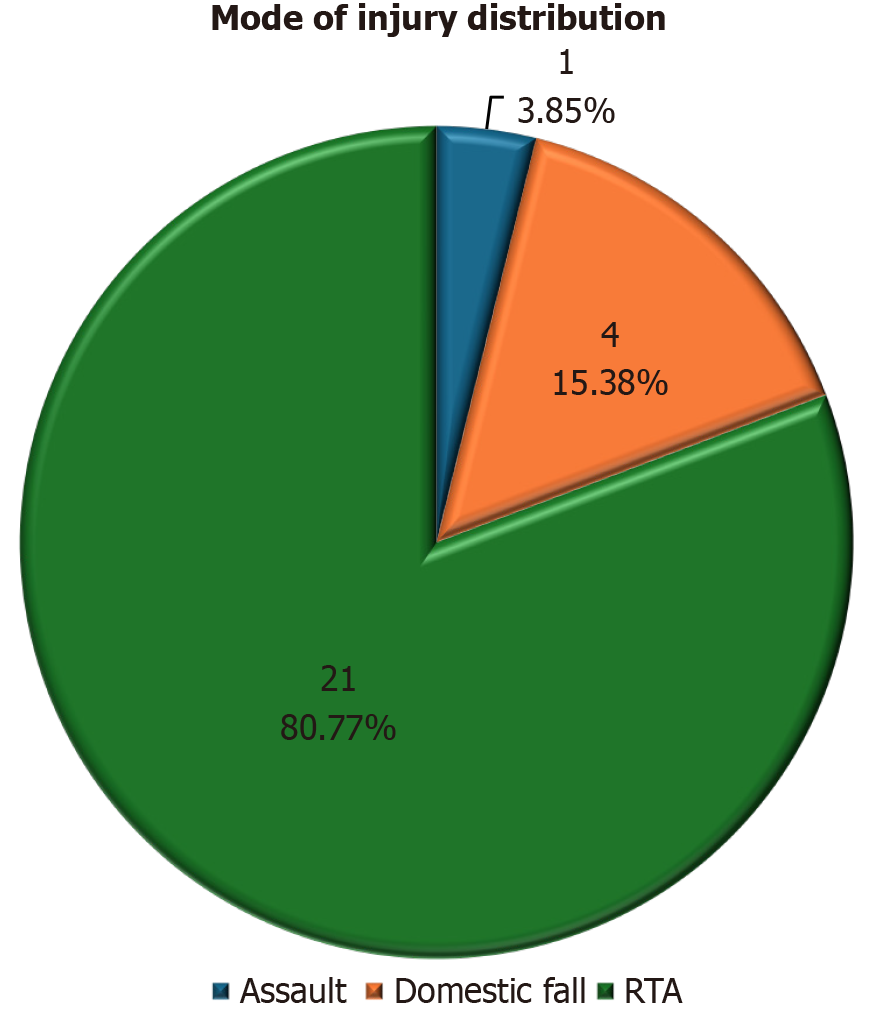
Of twenty-six adults the mean age of the study subjects was 49.08 years ± 16 years, with a median (25th-75th percentile) of 51 years [interquartile range (IQR): 32.5-61.5 years]. Total 14 patients (53.85%) were female, and 12 patients (46.15%) were male (Table 1). Modes of injury were distributed as follows: (1) 21 cases (80.77%) were due to road traffic accidents (RTA); (2) 4 cases (15.38%) were due to domestic falls; and (3) 1 case (3.85%) was due to assault (Figure 2). The surgical approach was Kocher's in 17 cases (65.38%) and posterior in 9 cases (34.62%) (Table 1). The mean duration of surgery was 2.05 hours ± 0.49 hours, with a median of 1.88 hours (IQR: 1.667-2.458 hours) and a range of 1.33-3.17 hours. The mean blood loss was 61.35 mL ± 35.6 mL, with a median of 50 mL (IQR: 30-75 mL) and a range of 30-150 mL (Table 2).
| Category | n | % | |
| Age (years) | 21-30 | 5 | 19.23 |
| 31-40 | 3 | 11.54 | |
| 41-50 | 5 | 19.23 | |
| 51-60 | 6 | 23.08 | |
| > 60 | 7 | 26.92 | |
| mean ± SD | 49.08 ± 16.04 | ||
| Median (25th-75th percentile) | 51 (32.5-61.5) | ||
| Gender | Female | 14 | 53.85 |
| Male | 12 | 46.15 | |
| Diagnosis | Type III | 13 | 50 |
| Type IV | 13 | 50 | |
| Approach | Kocher's | 17 | 65.38 |
| Posterior | 9 | 34.62 |
| Variable | Duration of surgery (hours) | Blood loss (mL) |
| mean ± SD | 2.05 ± 0.49 | 61.35 ± 35.6 |
| Median (25th-75th percentile) | 1.88 (1.667-2.458) | 50 (30-75) |
| Range | 1.33-3.17 | 30-150 |
The results presented highlight the significant improvements observed over time following surgery, with key metrics demonstrating notable recovery. In terms of elbow function, maximum elbow flexion improved steadily from 114.23° ± 8.57° immediately post-operative to 131.31° ± 7.72° at 6 months, with significant improvements at both 3 months and 6 months (P < 0.0001). Elbow extension deficit also showed significant reduction, from 68.15° ± 9.47° immediately post-operative to 6.5° ± 6.95° at 6 months (P < 0.0001).
Regarding rotational movements, both supination and pronation saw considerable gains, with supination increasing from 39.77° ± 9.61° immediately post-operative to 75.88° ± 12.68° at 6 months, and pronation improving from 28.88° ± 6.9° to 75.04° ± 9.57° in the same timeframe (P < 0.0001). Pain levels decreased significantly over time, with no moderate or severe pain reported by 3 months and 6 months, compared to 30.77% of patients experiencing severe pain immediately post-operative (P < 0.0001).
In addition, the motion arc showed considerable improvement from 46.08° ± 16.9° immediately post-operative to 124.81° ± 13.04° at 6 months (P < 0.0001). Stability of the elbow joint remained intact, with all cases showing stable joints at each time point. ADL scores also improved significantly, from a median score of 5 immediately post-operative to 25 at both 3 months and 6 months (P < 0.0001). Lastly, the MEPS classification demonstrated a marked improvement, with 100% of cases rated as good or excellent at six months, compared to 84.62% classified as poor immediately post-operative (P < 0.0001). These findings collectively underscore the positive outcomes of the surgery and its long-term benefits for elbow function and pain reduction (Table 3).
| Parameter | Immediate post-operative | At 3 months | At 6 months | P value | Comparisons (P values) |
| Maximum elbow flexion (°) | 114.23 ± 8.57 (100-130) | 129.73 ± 7.05 (115-142) | 131.31 ± 7.72 (110-142) | < 0.0001 | Immediate vs 3 months: < 0.0001; immediate vs 6 months: < 0.0001; 3 months vs 6 months: 0.104 |
| Elbow extension deficit (°) | 68.15 ± 9.47 (45-82) | 11 ± 10.25 (0-32) | 6.5 ± 6.95 (0-24) | < 0.0001 | Immediate vs 3 months: < 0.0001; immediate vs 6 months: < 0.0001; 3 months vs 6 months: 0.0003 |
| Supination (°) | 39.77 ± 9.61 (20-60) | 71.38 ± 14.28 (30-92) | 75.88 ± 12.68 (45-92) | < 0.0001 | Immediate vs 3 months: < 0.0001; immediate vs 6 months: < 0.0001; 3 months vs 6 months: 0.0002 |
| Pronation (°) | 28.88 ± 6.9 (18-46) | 70.69 ± 11.22 (44-90) | 75.04 ± 9.57 (48-90) | < 0.0001 | Immediate vs 3 months: < 0.0001; immediate vs 6 months: < 0.0001; 3 months vs 6 months: < 0.0001 |
| Pain | Severe: 8 (30.77%), moderate: 14 (53.85%), mild: 4 (15.38%), none: 0 (0%) | Severe: 0 (0%), moderate: 0 (0%), mild: 6 (23.08%), none: 20 (76.92%) | Severe: 0 (0%), moderate: 0 (0%), mild: 4 (15.38%), none: 22 (84.62%) | < 0.0001 | Immediate vs 3 months: < 0.0001; immediate vs 6 months: < 0.0001; 3 months vs 6 months: < 0.0001 |
| Motion arc (°) | 46.08 ± 16.9 (18-85) | 118.73 ± 15.48 (88-142) | 124.81 ± 13.04 (86-142) | < 0.0001 | Immediate vs 3 months: < 0.0001; immediate vs 6 months: < 0.0001; 3 months vs 6 months: 0.0001 |
| Stability | 26 (100% stable) | 26 (100% stable) | 26 (100% stable) | Not applicable | No changes observed |
| Activities of daily living score | 5.38 ± 4.88 (0-15) | 23.27 ± 3.45 (15-25) | 24.81 ± 0.98 (20-25) | < 0.0001 | Immediate vs 3 months: < 0.0001; immediate vs 6 months: < 0.0001; 3 months vs 6 months: 0.683 |
| Mayo elbow performance score | Poor: 22 (84.62%), fair: 4 (15.38%), good: 0, excellent: 0 | Poor: 0 (0%), fair: 3 (11.54%), good: 10 (38.46%), excellent: 13 (50%) | Poor: 0 (0%), fair: 0 (0%), good: 4 (15.38%), excellent: 22 (84.62%) | < 0.0001 | Immediate vs 3 months: < 0.0001; immediate vs 6 months: < 0.0001; 3 months vs 6 months: < 0.0001 |
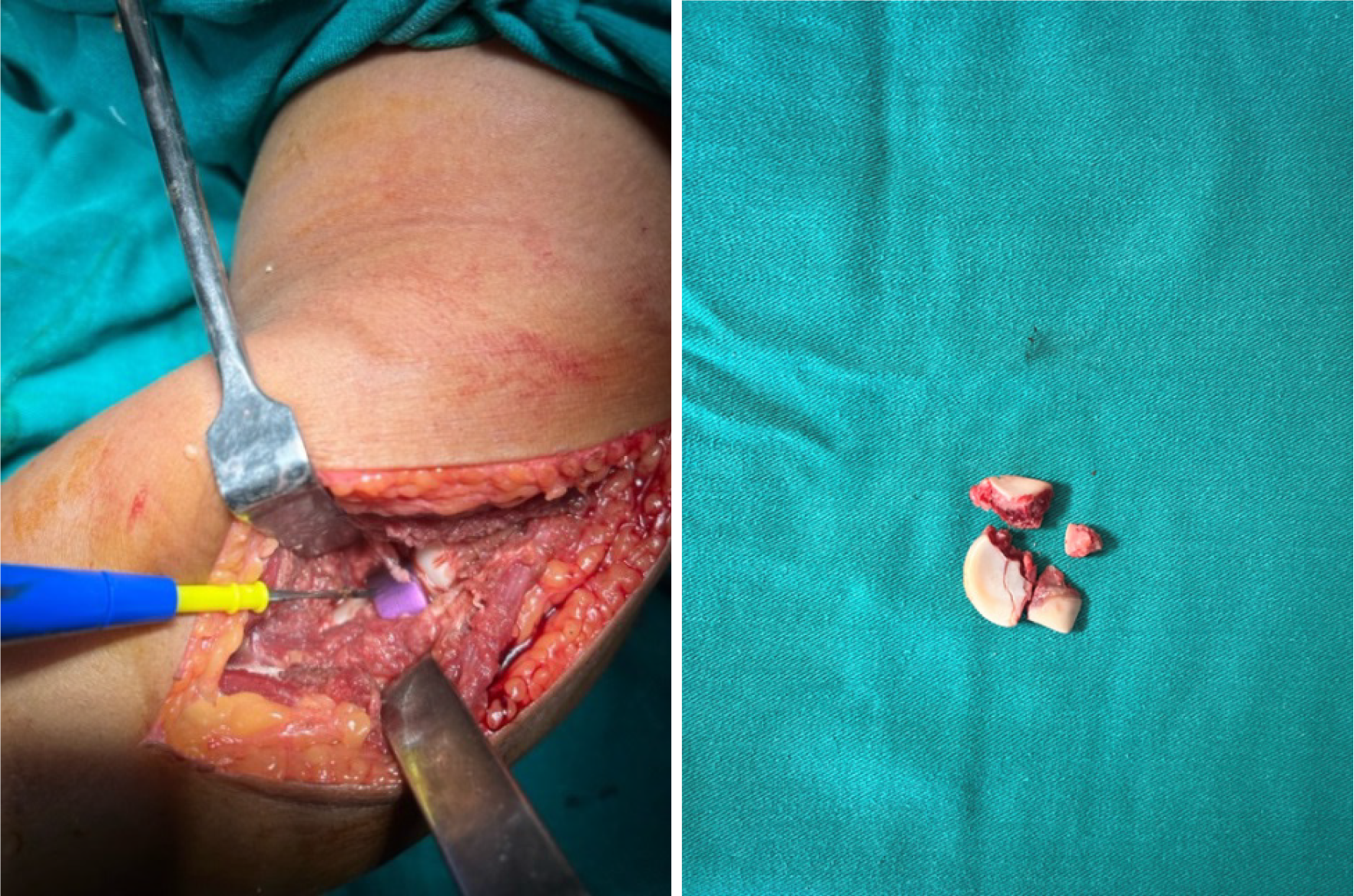
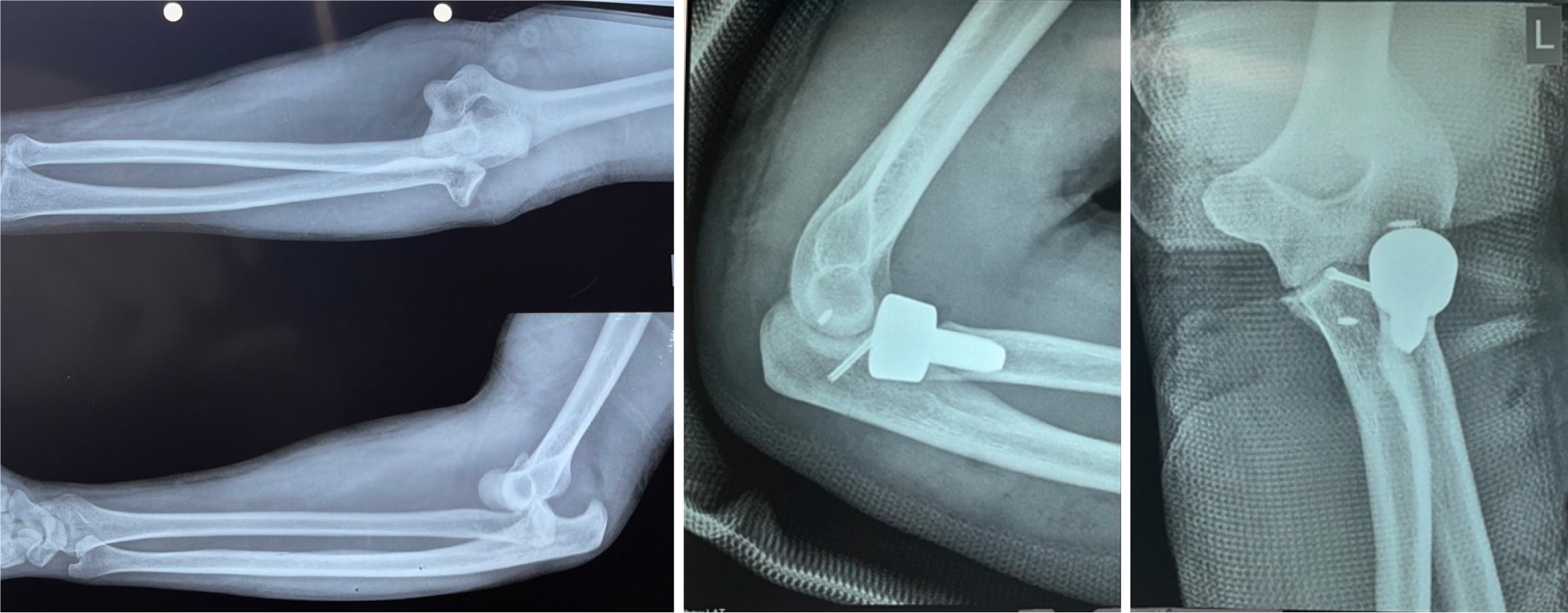
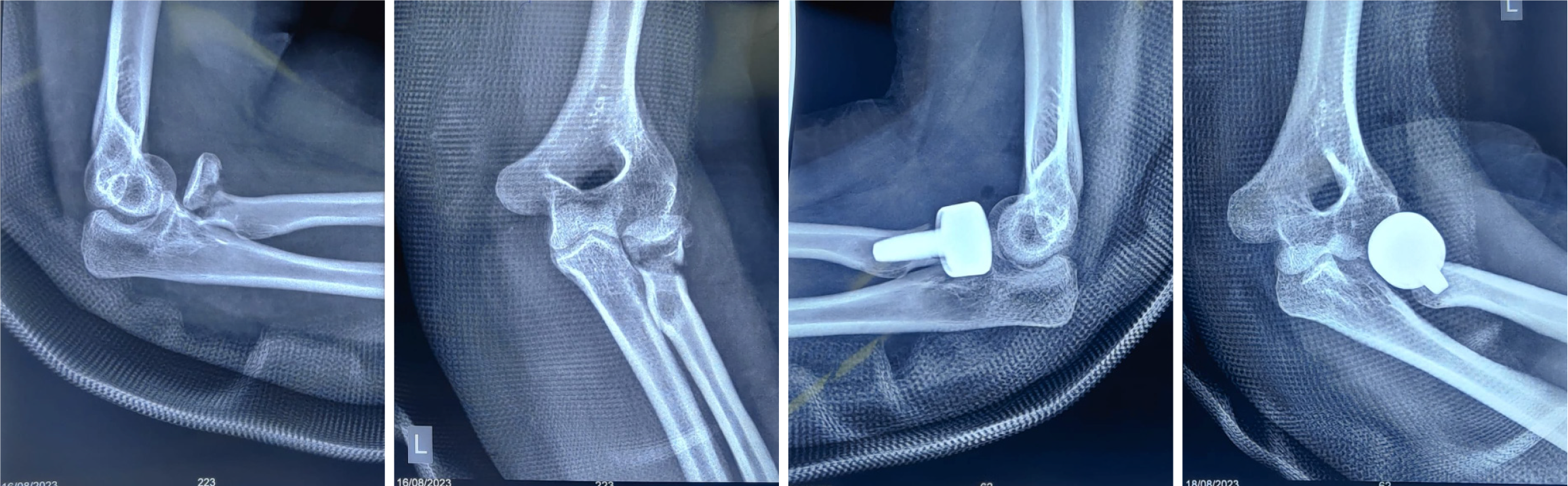
None of the patients had elbow instability after radial head replacement and 22 cases (84.62%) had no complications, while 3 cases (11.54%) had a stiff elbow (defined as a flexion-extension arc or forearm pronation-supination of less than 100°, which may limit daily activities. One patient met this criterion and was managed with extended physiotherapy), and 1 case (3.85%) had heterotopic ossification (Figures 3, 4 and 5).
Radial head and neck fractures account for approximately 20% of elbow injuries. The radial head plays a crucial role in stabilizing the elbow joint, particularly in cases with associated coronoid fractures or ligament injuries (medial collateral ligament, lateral ulnar collateral ligament). In our study RHA appears to restore the native biomechanics of the elbow by re-establishing joint congruity and improving load distribution, thereby stabilizing the elbow and reducing abnormal stress on the surrounding soft tissues. The modular metallic prosthesis, by closely replicating the native radial head’s dimensions and allowing for optimal ligamentous tension, likely contributes to significant improvements in ROM and pain reduction.
The mean age in our study was 49.08 years ± 16 years. This aligns with findings by Mulders et al[18], where the mean age was 50 years (IQR: 45.5-58.0 years). Similar results were reported by Kaur et al[19] (48.4 years) and Kulkarni et al[17] (40.3 years). Grewal et al[20] observed mean ages of 54 years ± 14.6 years. The high incidence in this age group is likely due to age-related decline in bone mineral density.
In this study, 14 patients (53.85%) were female and 12 patients (46.15%) were male. Baek et al[21] reported a similar distribution (11 females, 13 males). Songy et al[22] found a female predominance (56% female, 44% male) in 114 patients undergoing RHA. Foroohar et al[23] and Mulders et al[18] also reported higher female prevalence (60.6% and 56%, respectively). Increased susceptibility in females, particularly in older age groups, is attributed to osteoporosis.
High-energy trauma due to RTA was the most common cause (80.77%), followed by domestic falls (15.38%) and assault (3.58%). Kulkarni et al[17] observed RTA as the leading cause (18 cases), followed by falls (12 cases). Ajrawat et al[24] reported similar findings (14 cases RTA, 11 cases domestic fall)[24]. Kaur et al[19] found that falls on an outstretched hand (68.4%) were the most common cause, followed by falls from height (14%) and RTAs (9.2%).
Our study had an equal distribution of Mason type III (13 cases, 50%) and Type IV fractures (13 cases, 50%). Kulkarni et al[17] observed a higher prevalence of type III fractures (73.33%) and type IV fractures (26.67%). Ajrawat et al[24] reported 76% type III and 24% type IV fractures.
The Kocher’s approach was used in 17 cases (65.38%), while the posterior approach was used in 9 cases (34.62%). While both Kocher’s and posterior approaches yielded similar functional outcomes at six months, each method may influence the immediate post-operative period differently. The Kocher’s approach potentially offers better preservation of lateral soft tissues and more precise implant positioning, whereas the posterior approach might be advantageous when addressing associated fractures, such as those of the olecranon. However, the differences between these approaches diminish over time as healing progresses. Further biomechanical studies are warranted to elucidate these nuances.
The mean duration of surgery in our study was 2.05 hours ± 0.49 hours (median: 1.88 hours, IQR: 1.667-2.458 hours), comparable to Weissman et al[25], where the mean surgery time was 111.6 minutes ± 59 minutes. Al-Burdeni et al[26] reported a shorter mean duration (96.8 minutes) in 17 patients undergoing RHA. The longer operative time in our study was due to 57.7% of cases having associated injuries (olecranon/coronoid fractures or ligamentous injuries requiring fixation), whereas for isolated radial head fractures (42.3%), the operative time was significantly shorter.
Elbow flexion improved significantly from 114.23° ± 8.57° post-operative to 129.73° ± 7.05° at 3 months and 131.31° ± 7.72° at 6 months (P < 0.0001), aligning with Baek et al[21] (132.7° ± 7.4°) and Songy et al[22] [133° (IQR: 60-150°)]. Extension deficit reduced from 68.15° ± 9.47° post-operative to 6.5° ± 6.95° at 6 months (P < 0.0001), comparable to Baek et al[21] (4.7° ± 10.8°) and Songy et al[22] [14° (IQR: 0-90°)].
Supination improved from 39.77° ± 9.61° post-operative to 75.88° ± 12.68° at 6 months, and pronation from 28.88° ± 6.9° to 75.04° ± 9.57° (P < 0.0001), consistent with Baek et al[21] and Songy et al[22].
Pain levels significantly improved (P < 0.0001), with 53.85% moderate pain and 30.77% severe pain post-operative, reducing to 76.92% pain-free at 3 months. Findings align with Baek et al[21] (VAS: 0.6 ± 1.1) and Mercer et al[27] (VAS at rest: 0.9).
MEPS improved from 37.69 ± 18.23 post-operative (poor: 84.62%, fair: 15.38%) to 97.31 ± 6.67 at 6 months (excellent: 84.62%, good: 15.38%) (P < 0.0001), consistent with Baek et al[21] (mean MEPS: 88.7 ± 11.5, excellent: 58.3%) and Ajrawat et al[24] (excellent: 80%).
ADL scores improved significantly (P < 0.0001), from 5 (0-10) post-operative to 25 (25-25) at 3 months, consistent with Chen et al[28] dietary approach to stop hypertension scores (12.2 ± 12.6 at 2 years, 14.1 ± 14.3 at 10 years).
Most patients (84.62%) had no complications, 11.54% developed stiffness, and 3.85% had heterotopic ossification. Findings align with Baek et al[21] (16.7% complications), Songy et al[22] (revision surgery: 14 cases), and Mercer et al[27] (7.6% complications, 5.7% reoperations).
In conclusion, RHA effectively restored the stability and congruency of the elbows with radial head fractures. There was a significant improvement in the ROM involving flexion, extension deficit, supination and pronation during our follow up period with minimal complications. There was also a significant improvement in the ADL and MEPS scores during follow up of immediate post op, 3 months and 6 months-indicating improved quality of life after the surgery.
A key limitation of this study is the relatively small sample size (n = 26), which may reduce the statistical power to detect smaller yet clinically meaningful differences. While a post hoc power analysis indicated that the study had sufficient power to detect large effect sizes, it may have been underpowered for detecting smaller variations in outcomes. Future studies with larger sample sizes are needed to further validate our findings and improve generalizability.
Another significant limitation of this study is the absence of a control group, such as patients treated with ORIF or non-operative management. While comparisons were made to previously published literature, these indirect comparisons do not provide the same level of evidence as a controlled study design. Future research incorporating a control group or a randomized comparative study would help strengthen the conclusions and provide more definitive insights into the efficacy of RHA relative to other treatment options.
The relatively short 6-month follow-up period may not fully capture long-term complications such as implant loosening, heterotopic ossification progression, or post-traumatic osteoarthritis. These issues often develop over an extended period, requiring longer follow-up for a more comprehensive assessment. Future studies with extended follow-up are needed to better evaluate the durability and long-term outcomes of RHA.
Finally, the inclusion of retrospective data presents a potential for selection and recall bias, as retrospective data may be incomplete or less accurate compared to prospectively collected data. Although efforts were made to standardize data collection and verification, this remains a limitation of the study.
| 1. | Kaas L, van Riet RP, Vroemen JP, Eygendaal D. The incidence of associated fractures of the upper limb in fractures of the radial head. Strategies Trauma Limb Reconstr. 2008;3:71-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Iannuzzi NP, Leopold SS. In brief: the Mason classification of radial head fractures. Clin Orthop Relat Res. 2012;470:1799-1802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Sheps DM, Kiefer KR, Boorman RS, Donaghy J, Lalani A, Walker R, Hildebrand KA. The interobserver reliability of classification systems for radial head fractures: the Hotchkiss modification of the Mason classification and the AO classification systems. Can J Surg. 2009;52:277-282. [PubMed] |
| 4. | Dou Q, Yin Z, Sun L, Feng X. Prosthesis replacement in Mason III radial head fractures: A meta-analysis. Orthop Traumatol Surg Res. 2015;101:729-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Heijink A, Kodde IF, Mulder PGH, Veltman ES, Kaas L, van den Bekerom MPJ, Eygendaal D. Radial Head Arthroplasty: A Systematic Review. JBJS Rev. 2016;4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Sun H, Duan J, Li F. Comparison between radial head arthroplasty and open reduction and internal fixation in patients with radial head fractures (modified Mason type III and IV): a meta-analysis. Eur J Orthop Surg Traumatol. 2016;26:283-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Struijs PA, Smit G, Steller EP. Radial head fractures: effectiveness of conservative treatment versus surgical intervention. A systematic review. Arch Orthop Trauma Surg. 2007;127:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Faldini C, Nanni M, Leonetti D, Capra P, Bonomo M, Persiani V, Galante C, Giannini S. Early radial head excision for displaced and comminuted radial head fractures: considerations and concerns at long-term follow-up. J Orthop Trauma. 2012;26:236-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Thyagarajan DS. Radial head replacement - A comprehensive review. J Orthop. 2023;36:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 10. | Bonnevialle N. Radial head replacement in adults with recent fractures. Orthop Traumatol Surg Res. 2016;102:S69-S79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Li N, Chen S. Open reduction and internal-fixation versus radial head replacement in treatment of Mason type III radial head fractures. Eur J Orthop Surg Traumatol. 2014;24:851-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Zwingmann J, Welzel M, Dovi-Akue D, Schmal H, Südkamp NP, Strohm PC. Clinical results after different operative treatment methods of radial head and neck fractures: a systematic review and meta-analysis of clinical outcome. Injury. 2013;44:1540-1550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Harrington IJ, Sekyi-Otu A, Barrington TW, Evans DC, Tuli V. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: a long-term review. J Trauma. 2001;50:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 177] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Ashwood N, Bain GI, Unni R. Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization. J Bone Joint Surg Am. 2004;86:274-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 82] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84:1811-1815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 266] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 16. | Ruan HJ, Fan CY, Liu JJ, Zeng BF. A comparative study of internal fixation and prosthesis replacement for radial head fractures of Mason type III. Int Orthop. 2009;33:249-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Kulkarni V, Lambat N, Patil T, Joshi S, Jadhav S, Dattu V. A study on functional outcome of radial head arthroplasty in comminuted radial head fracture. Int J Orthop Sci. 2020;6:690-695. [DOI] [Full Text] |
| 18. | Mulders MAM, Schep NWL, de Muinck Keizer RO, Kodde IF, Hoogendoorn JM, Goslings JC, Eygendaal D. Operative vs. nonoperative treatment for Mason type 2 radial head fractures: a randomized controlled trial. J Shoulder Elbow Surg. 2021;30:1670-1678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Kaur MN, MacDermid JC, Grewal RR, Stratford PW, Woodhouse LJ. Functional outcomes post-radial head arthroplasty: a systematic review of literature. Shoulder Elbow. 2014;6:108-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Grewal R, MacDermid JC, Faber KJ, Drosdowech DS, King GJ. Comminuted radial head fractures treated with a modular metallic radial head arthroplasty. Study of outcomes. J Bone Joint Surg Am. 2006;88:2192-2200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 107] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 21. | Baek CS, Kim BS, Kim DH, Cho CH. Short- to mid-term outcomes of radial head replacement for complex radial head fractures. Clin Shoulder Elb. 2020;23:183-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Songy CE, Kennon JC, Barlow JD, Sanchez-Sotelo J, O'Driscoll SW, Morrey ME. Radial Head Replacement for Acute Radial Head Fractures: Outcome and Survival of Three Implant Designs With and Without Cement Fixation. J Orthop Trauma. 2021;35:e202-e208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Foroohar A, Prentice HA, Burfeind WE, Navarro RA, Mirzayan R, Zeltser DW. Radial head arthroplasty: a descriptive study of 970 patients in an integrated health care system. J Shoulder Elbow Surg. 2022;31:1242-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 24. | Ajrawat S, Mal J, Talwar K, Goyal C. Functional outcomes of patients with comminuted radial head fracture undergoing radial head arthroplasty. Natl J Physiol Pharm Pharmacol. 2023;. [DOI] [Full Text] |
| 25. | Weissman JP, Plantz MA, Gerlach EB, Cantrell CK, Butler B. 30-Day outcomes analysis of surgical management of radial head fractures comparing radial head arthroplasty to open reduction internal fixation. J Orthop. 2022;30:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Al-Burdeni S, Abuodeh Y, Ibrahim T, Ahmed G. Open reduction and internal fixation versus radial head arthroplasty in the treatment of adult closed comminuted radial head fractures (modified Mason type III and IV). Int Orthop. 2015;39:1659-1664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 27. | Mercer DM, Bolano LE, Rubio F, Bamberger HB, Figueroa JS, Gonzalez GA. A radial head prosthesis that aligns with the forearm axis of rotation: a retrospective multicenter study. Seminars in Arthroplasty: JSES. 2022;32:511-518. [DOI] [Full Text] |
| 28. | Chen AC, Cheng YH, Chiu CH, Cheng CY, Chan YS. Long-Term Outcomes of Radial Head Arthroplasty in Complex Elbow Fracture Dislocation. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |