Published online Jun 18, 2025. doi: 10.5312/wjo.v16.i6.103875
Revised: April 24, 2025
Accepted: May 27, 2025
Published online: June 18, 2025
Processing time: 197 Days and 2.3 Hours
Long head of biceps tendon (LHBT) transposition is a novel technique based on the double-row suture bridge method, utilizing autologous reconstruction to treat massive rotator cuff tears.
To evaluate the mid-to-long-term clinical outcomes following the double-row repair method for massive rotator cuff tears.
This retrospective analysis included data from 53 patients with massive rotator cuff tears treated at our hospital between 2020 and 2021. The patients were divided into the double-row repair group (conventional group) and the double-row repair combined with the LHBT transposition group (transposition group). Postoperative pain was assessed using the visual analogue scale at one week, one year, and the final follow-up. Shoulder function was evaluated using the American Shoulder and Elbow Surgeons and Constant-Murley scores at one year and the final follow-up. Rotator cuff healing was assessed postoperatively for one year using the Sugaya classification, which categorizes tendon integrity based on magnetic resonance imaging findings.
No perioperative complications were observed in any of the patients at any time. There were no significant differences between the groups regarding operative time and intraoperative blood loss. The transposition group had significantly lower visual analogue scale scores than the conventional group at one week postoperatively; however, there were no significant differences between the groups at one year or the final follow-up. At one year postoperatively, the transposition group showed significantly higher American Shoulder and Elbow Surgeons and Constant-Murley scores than the conventional group; no significant differences were observed at the final follow-up. There were no significant differences in rotator cuff healing between the groups at one year postoperatively.
Compared to double-row repair alone, double-row repair combined with LHBT transposition for treating massive rotator cuff tears more effectively alleviates short-term postoperative pain and improves shoulder function within the first year.
Core Tip: Our study shows that combining double-row repair with biceps tendon transposition for massive rotator cuff tears reduces early pain, speeds recovery, and improves function by 15% at one year - without added complications. At three years, 88% of patients maintained good tendon healing. This method offers a simpler and more economical alternative to traditional graft-based reconstructions for massive rotator cuff tears.
- Citation: Zhou YJ, Wang BB, Wen HW, Xu L, Feng J, Xu FS. Clinical comparison of arthroscopic double-row rotator cuff repair with or without long head of biceps tendon transposition. World J Orthop 2025; 16(6): 103875
- URL: https://www.wjgnet.com/2218-5836/full/v16/i6/103875.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i6.103875
Massive rotator cuff tears are a common clinical condition, typically defined as a tear length greater than 5 cm or involving two or more rotator cuff tendons[1]. They are a frequent cause of shoulder pain and functional impairment and represent a severe type of shoulder joint disease, predominantly occurring in older adults over 60 years of age[2]. These tears are associated with rotator cuff degeneration and trauma. Currently, the primary treatment modality is arthroscopic rotator cuff repair. Despite the widespread adoption of this technique, the prognosis for patients with massive rotator cuff tears remains unsatisfactory, with a high rate of repair failure[3]. It is estimated that massive rotator cuff tears account for approximately 20% of all rotator cuff tears and 80% of recurrent tears[4,5].
Arthroscopic suture repair of massive rotator cuff tears is currently the most widely utilized surgical technique in clinical practice, with significant postoperative functional improvements reported by patients[6]. Suture techniques include single-row, double-row, and double-row suture bridge methods. Studies have demonstrated that the double-row technique offers superior biomechanical advantages and lower re-tear rates than the single-row technique[7,8]. In recent years, a consensus among researchers has emerged, suggesting that double-row suture bridge repair of massive rotator cuff tears provides enhanced biomechanical properties, resulting in a more stable repair and better functional recovery for patients than other existing techniques[9-11].
However, massive rotator cuff tears are often associated with notable muscle atrophy and fat infiltration. They may also involve complications such as humeral head migration, tendon retraction, and scar tissue formation at the rupture site. Even with extensive tissue release and repair performed intraoperatively, many patients experience significant pain due to the high tension on the repaired rotator cuff, leading to postoperative adhesions and severe functional limitations[12]. As a result, many scholars emphasize the importance of maximizing footprint coverage during surgery to create a biomechanical environment that effectively promotes tendon-bone healing.
Patients with high functional demands present new challenges for rotator cuff repair, and superior capsular reconstruction has emerged as a novel option. Mihata et al[13] were the first to propose using autologous fascia lata as a graft material for superior capsular reconstruction in treating massive rotator cuff tears. Their one-year follow-up findings indicated significant improvements in patient functional scores, achieving satisfactory clinical outcomes; however, the high cost of materials limits its widespread application.
Building upon this, Boutsiadis et al[14] proposed an alternative approach to superior capsular reconstruction in 2017, referred to as “the Chinese Way”. This technique involves fixing the long head of biceps tendon (LHBT) transposition to the footprint area on the greater tuberosity, aiding in the reconstruction of the superior capsule while maintaining the stability of the humeral head to prevent superior migration. This method also minimizes friction between the acromion and the rotator cuff while providing an anterior superior blocking effect that reduces tension on the rotator cuff tissue, promoting tendon-bone healing. The early efficacy of 'the Chinese Way' has been clinically validated[15,16]; however, further verification of its mid- to long-term clinical outcomes remains lacking.
Therefore, this study aimed to investigate the clinical efficacy of patients in the conventional (double-row repair) and the transposition (double-row repair with LHBT transposition) groups in terms of the following factors: (1) Duration of surgery, intraoperative blood loss, and postoperative complications (including wound infection, axillary nerve injury, vastus lateralis muscle hernia, and sensory abnormalities); (2) Pain levels at one week, one year, and the final follow-up; (3) Shoulder function recovery at one year and the final follow-up; and (4) The integrity of rotator cuff healing was assessed at one year.
This study was a retrospective analysis of patients treated at our hospital from January 2020 to December 2021. We strictly adhered to a blinded approach in data analysis, ensuring that the researchers could not identify patients based on case records. All research findings presented in the article maintain patient privacy and anonymity. We applied for and received approval for an informed consent waiver from our hospital, approval No. AF/KYSQ-09/04.0. The study was also approved by the Ethics Committee of Wuhan Fourth Hospital, approval No. KY2023-035-01.
Patients were required to meet all of the following inclusion criteria: (1) Preoperative magnetic resonance imaging (MRI) demonstrated massive rotator cuff tears involving two or more rotator cuff tendons or a tendon defect greater than 5 cm; (2) Conservative treatment for more than three months with unsatisfactory results, indicating this was the first surgical intervention; (3) LHBT intact with possible mild degeneration; (4) MRI showed residual rotator cuff tissue with fat infiltration classified as Goutallier grade < 3 and tendon retraction classified as Patte grade < 3[17,18]; (5) Intraoperative confirmation of massive rotator cuff tear, with tendons able to be mobilized back to the footprint for fixation; and (6) Ability to undergo regular follow-up for at least three years. Exclusion criteria were as follows: (1) Adequate shoulder function with minimal pain symptoms; (2) Age < 45 years or > 75 years; (3) Presence of severe osteoporosis; and (4) MRI revealing residual rotator cuff tissue with fat infiltration classified as Goutallier grade > 2 and tendon retraction classified as Patte grade > 2.
This study included 53 patients and demographic data and general clinical characteristics were collected. The demographic data comprised age, sex, history of trauma, and other comorbidities (such as common chronic conditions like hypertension and diabetes). The general clinical characteristics included the duration of preoperative symptoms, surgery side, associated injuries, pain scores, and baseline shoulder function scores. The two groups showed no significant differences in baseline demographic and clinical characteristics (Table 1).
| Characteristic | Conventional group (n = 28) | Transposition group (n = 25) | P value |
| Age (years), mean ± SD | 59.82 ± 6.74 | 60.48 ± 7.38 | 0.736a |
| Sex (men/women) | 16/12 | 11/14 | 0.339b |
| Duration of preoperative symptoms (months), mean ± SD | 16.64 ± 3.14 | 18.12 ± 3.62 | 0.513a |
| Surgery side (left/right) | 11/17 | 7/18 | 0.386b |
| Goutallier grade (I/II) | 13/15 | 13/12 | 0.685b |
| History of trauma (yes/No) | 7/21 | 6/19 | 0.856b |
| Other comorbidities (yes/No) | 8/20 | 5/20 | 0.489b |
| With SST (yes/No) | 10/18 | 7/18 | 0.455b |
| With SLAP (yes/No) | 2/26 | 0/25 | 0.484b |
| VAS pain score, mean ± SD | 6.61 ± 1.87 | 6.96 ± 1.90 | 0.500a |
| ASES score, mean ± SD | 36.43 ± 7.62 | 35.68 ± 7.59 | 0.722a |
| Constant score, mean ± SD | 45.11 ± 6.36 | 44.84 ± 5.44 | 0.871a |
Conventional group: After successful general anesthesia combined with brachial plexus block, patients were placed in a lateral decubitus position, with the affected limb suspended under 3-4 kg of traction, the shoulder abducted to 45°-60°, and flexed forward to 20°. Posterior, anterior, anterolateral, and posterolateral portals were sequentially established to perform arthroscopic examination of the shoulder joint, and synovial hypertrophy proliferative synovial tissue was debrided. The rotator cuff tendons were inspected for damage and potential concomitant injuries such as LHBT injury, superior labrum anterior and posterior lesion, or adhesive capsulitis. For patients with adhesive capsulitis, arthroscopic release was performed. Patients with intact LHBT were included in the study cohort. Any associated subscapularis and/or infraspinatus tendon injuries were repaired, followed by thorough release of the supraspinatus tendon superiorly and inferiorly while carefully protecting the suprascapular nerve. The extent of supraspinatus tendon defect and retraction was assessed; if the tendon could be mobilized back to the medial edge of the footprint, the footprint area was prepared using an abrasive drilling to freshen the greater tuberosity by removing bone spurs and some cortical bone. Single-row anchors or double-row suture bridge techniques were used to repair the supraspinatus and infraspinatus tendons, depending on the tendon's reduction and tension. Patients who underwent double-row repair were included in the conventional group. Hemostasis was achieved arthroscopically; a drainage tube was placed within the joint cavity, and the surgical incisions were sutured.
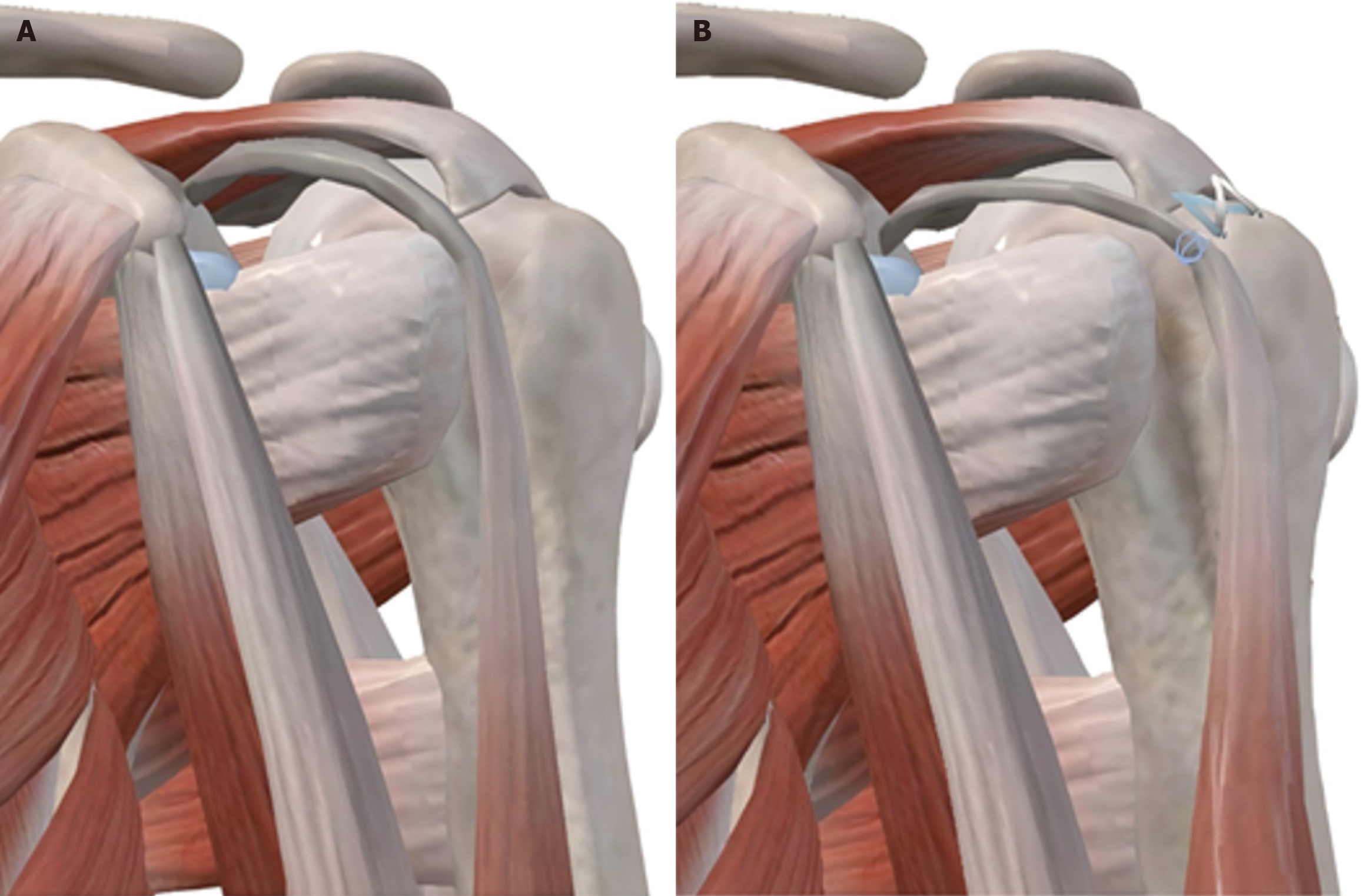
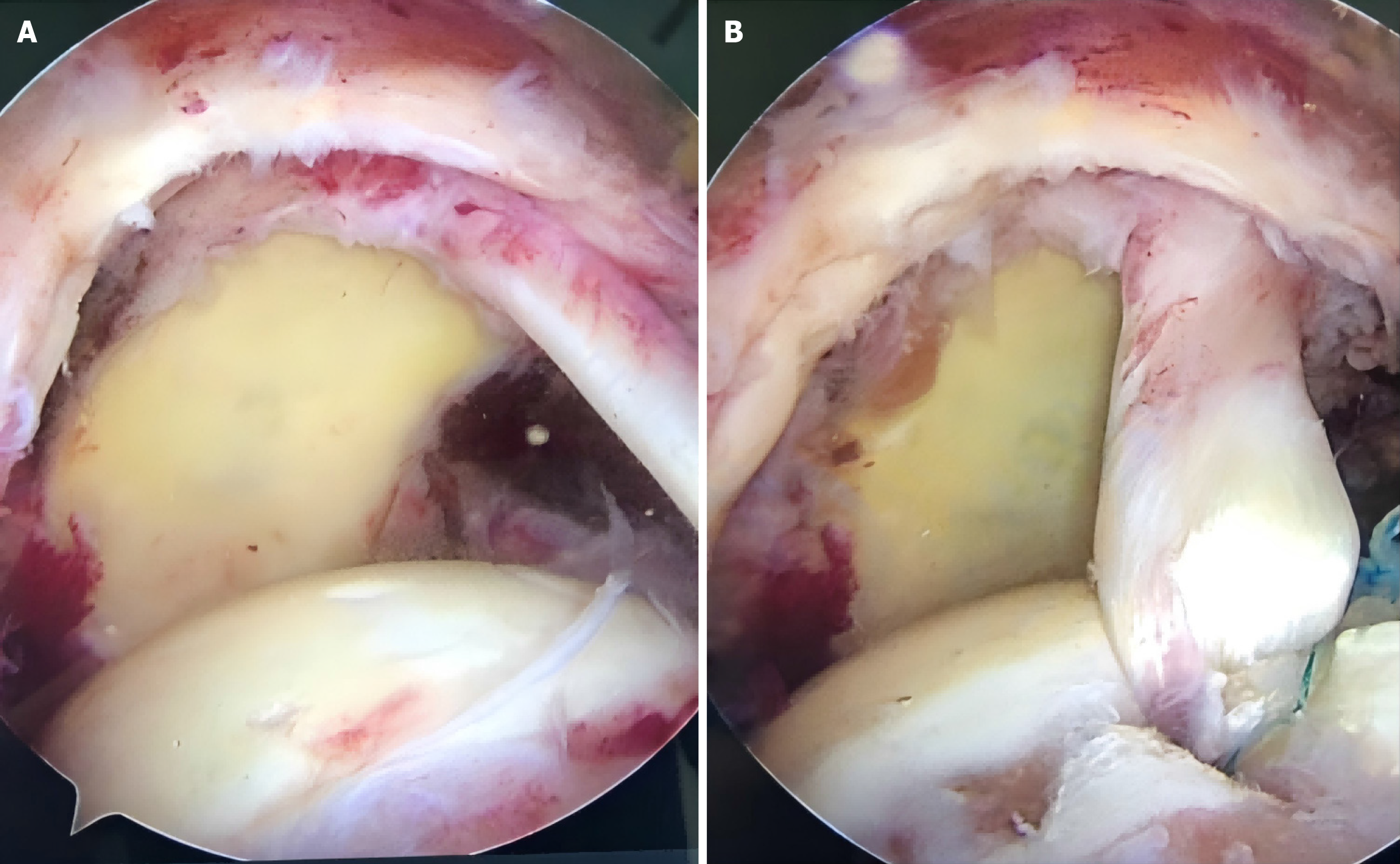
Transposition group: For patients in the LHBT transposition group, the LHBT was first examined. If the LHBT was intact and of acceptable quality, one 4.5 cm Healix double-thread anchor (Mitek) was implanted approximately 1.0-1.5 cm posterior to the bicipital groove, near the articular cartilage of the supraspinatus footprint area. The LHBT was then transposed and sutured to this site using a double-locking technique. The remaining steps were the same as those in the conventional group (Figure 1). An intraoperative image illustrating the LHBT transposition and its fixation to the footprint area is shown in Figure 2.
The postoperative rehabilitation protocol for all patients was developed and supervised by the same rehabilitation therapist in our department. Both groups of patients had to wear a shoulder abduction brace, which strictly maintained the shoulder in 60°abduction and 20°external rotation for six weeks. Immediately following surgery, patients were encouraged to begin wrist joint exercises, including active chest expansion, shoulder shrugging, and passive shoulder muscle relaxation training (such as pendulum exercises, circular movements, and table climbing). Between 6 weeks to 8 weeks postoperatively, passive shoulder abduction and flexion-extension exercises and active scapular mobility exercises were initiated. From 8 weeks 12 weeks postoperatively, active shoulder abduction, flexion, and extension exercises were introduced. Active resistance training for the shoulder began at three months postoperatively, and patients were allowed to resume light physical labor or sports activities at six months postoperatively.
Statistical analysis was performed on the demographic information and general clinical characteristics of all patients at the time of consultation. First, we compared the duration of surgery and intraoperative blood loss between the two groups, assessing the intraoperative observation parameters.
The primary outcomes of this study were to assess pain, shoulder function recovery, and rotator cuff integrity at one year and at the final follow-up (approximately three years) postoperatively. Pain levels were evaluated using the visual analogue scale (VAS), a tool with validated reliability and validity for pain measurement in patients, where scores range from 0 to 10, with higher scores indicating greater pain intensity[19]. Shoulder function recovery was assessed using the Constant-Murley Shoulder Score and the American Shoulder and Elbow Surgeons (ASES) score, both of which range from 0 to 100, with higher scores indicating better shoulder function[20,21]. The integrity of rotator cuff healing was evaluated using the Sugaya classification[22]: Type I: The cuff is of normal thickness and homogeneous with no structural defect; type II: The cuff is of normal thickness with a high-intensity area; type III: The cuff is less than half the normal thickness but remains intact, indicating a partial-thickness tear; Type IV: Discontinuity is seen in one or two layers on oblique coronal and sagittal views, indicating a small full-thickness tear; Type V: Discontinuity is seen in more than two layers on oblique coronal and sagittal views, indicating a medium to large retear. Types IV and V represent postoperative retears of the rotator cuff.
Data analyses were conducted using SPSS version 26.0. For continuous variables, normality was first tested. Variables such as age, preoperative symptom duration, duration of surgery, intraoperative blood loss, VAS scores, ASES scores, and Constant-Murley scores were found to follow a normal distribution, with homogeneity of variance between the two groups. Independent sample t-tests were used for comparisons between groups, while paired sample t-tests were applied for within-group comparisons. For categorical variables such as sex, Goutallier classification, affected shoulder, Sugaya classification, and χ2 tests were employed. A two-tailed P-value of < 0.05 was considered statistically significant.
All patients completed surgery, and the drainage tube was removed 24 hours postoperatively. The duration of surgery was 82.68 ± 27.10 minutes for the conventional group and 96.40 ± 31.77 minutes for the transposition group, with the transposition group requiring slightly more time. However, the difference was not statistically significant (P > 0.05). Intraoperative blood loss was 36.96 ± 4.97 mL for the conventional group and 38.20 ± 4.98 mL for the transposition group, with no statistically significant difference between the groups (P > 0.05).
All patients were followed up for a period ranging from 25 months to 46 months, with an average of 36.5 months. No perioperative complications were observed, such as wound infection, axillary nerve injury, or sensory abnormalities. Postoperatively, 2 cases in the conventional group and 3 in the transposition group developed shoulder joint adhesions with no evidence of tendon retear. All five patients regained bare shoulder joint range of motion within six months postoperatively after enhanced rehabilitation (Table 2).
| Characteristic | Conventional group (n = 28) | Transposition group (n = 25) | P value |
| VAS scores | |||
| 1 week postoperatively | 3.64 ± 1.95 | 2.08 ± 1.19 | 0.001a |
| 1 year postoperatively | 1.71 ± 0.94 | 1.64 ± 1.00 | 0.781 |
| Final follow-up | 1.25 ± 0.65 | 1.24 ± 0.66 | 0.956 |
Pain: As shown in Table 2, the VAS score at the 1-week postoperative follow-up was lower in the transposition group than in the conventional group, with the difference being statistically significant. However, there were no statistically significant differences in VAS scores between the two groups preoperatively, at the 1-year follow-up or final follow-up.
Shoulder function: In both groups, the ASES and Constant-Murley scores at one year postoperatively were significantly better in the transposition group compared to the conventional group, with statistical significance noted. However, at the final follow-up, the two groups showed no significant differences in ASES and Constant-Murley scores (Table 3).
| Characteristic | Conventional group (n = 28) | Transposition group (n = 25) | P value |
| ASES scores | |||
| 1 year postoperatively | 63.29 ± 4.21 | 73.40 ± 5.91 | < 0.001a |
| Final follow-up | 78.96 ± 5.02 | 79.92 ± 4.59 | 0.474 |
| Constant-Murley scores | |||
| 1 year postoperatively | 58.04 ± 8.43 | 67.31 ± 6.56 | < 0.001a |
| Final follow-up | 78.86 ± 7.55 | 80.56 ± 4.06 | 0.305 |
Rotator cuff healing: At the one-year postoperative follow-up, an MRI of the affected shoulder revealed the following Sugaya classifications: In the conventional group, there were 8 cases of grade I, 15 cases of grade II, and 5 cases of grade III. In the transposition group, there were 7 cases of grade I, 15 cases of grade II, and 3 cases of grade III. The differences between the two groups were not statistically significant (Table 4). MRI results showed that 82.1% (25/28) of the reconstructed tissue in the transposition group and 88.0% (22/25) in the conventional group maintained structural integrity, which may be related to the relatively short follow-up period for MRI re-examination. There were no retears during follow-up, and the LHTB maintained structural integrity.
| Characteristic | Conventional group (n = 28) | Transposition group (n = 25) | χ2 | P value |
| Sugaya classification | ||||
| I | 8 | 7 | 0.400 | 0.819 |
| II | 15 | 15 | ||
| III | 5 | 3 | ||
This study investigated the treatment of patients with massive rotator cuff tears using double-row repair combined with LHBT transposition, compared to simple double-row repair. Building on previous research, we extended the follow-up period to compare the efficacy of both methods over a longer time frame. The results indicated no significant differences in surgical duration and intraoperative blood loss. At one week postoperatively, the transposition group experienced lower pain levels, while at one year postoperatively, this group achieved higher shoulder function scores. There were no differences in rotator cuff healing between the two groups.
Regarding intraoperative observation parameters, the two groups had no significant differences in surgical duration and intraoperative blood loss. This suggests that although the LHBT transposition technique requires a higher level of surgical skill, it does not increase the duration of surgery or intraoperative blood loss. Furthermore, it does not affect the difficulty of intraoperative management, anesthesia risk, or the postoperative healing period for patients.
The study results also showed that pain scores (VAS scores) in the transposition group at one week postoperatively were significantly lower than those in the conventional group. These results indicate that double-row repair combined with LHBT transposition can quickly reduce early postoperative pain. Studies have shown that early postoperative pain (within one week) significantly impacts patients’ mental health and quality of life[23], and mental health is closely related to disease recovery[24]. Therefore, this surgical approach may promote physical and psychological recovery more effectively than conventional methods.
At one year postoperatively, shoulder function scores (ASES and Constant-Murley scores) in the transposition group were significantly higher than those in the conventional group. However, the scores were comparable at the final follow-up, with no significant differences observed. These findings suggested that although the double-row repair combined with LHBT transposition was relatively more complex, there were no significant differences in terms of promoting long-term rotator cuff tissue healing and the resolution of inflammation compared to the conventional method. Furthermore, the transposition procedure facilitated early shoulder joint function recovery without increasing the risk of postoperative complications such as pain and limited joint mobility caused by long-term shoulder joint adhesions, and did not make long-term shoulder joint rehabilitation more difficult for patients. This suggests that patients who underwent double-row repair combined with LHBT transposition experienced faster recovery within the first year post-surgery compared to the conventional group. This conclusion is consistent with previous studies, indicating that LHBT transposition and fixation can enhance the mechanical strength of the rotator cuff and create a larger subacromial space without significantly increasing surgical difficulty, thereby facilitating early recovery of shoulder function[25]. Additionally, the one-year postoperative rotator cuff healing outcomes (Sugaya classification) showed no significant differences between the two groups, indicating that although the transposition procedure is complex, it does not adversely affect routine healing of the rotator cuff tissue compared to the conventional method. This is consistent with findings observed in other studies on LHBT transposition surgery[26,27].
In summary, double-row repair combined with LHBT transposition presents more advantages compared to conventional methods. First, the use of LHBT transposition in repairing massive rotator cuff tears functions similar to the autologous fascia lata technique, aiming to reinforce the superior joint capsule and better protect the repaired remnants of the rotator cuff. This method preserves the continuity and blood supply of the LHBT, increasing the chances of self-healing and creating optimal conditions for rotator cuff tissue recovery[28]. Second, it typically does not require the use of fascia lata grafts, thereby avoiding the donor-site morbidity and infection risks occasionally reported in graft-based reconstructions, while effectively reducing costs[29,30]. Third, after LHBT transposition, the humeral head remains depressed, increasing the subacromial space and effectively preventing recurrent rotator cuff tears[31]. Finally, compared to conventional double-row suturing, the duration of surgery does not increase significantly. In this study, all cases included had tendons that could be pulled back and sutured to the footprint area. Consistent with previous reports on clinical outcomes, the double-row anchor suture bridge technique combined with LHBT transposition effectively alleviates short-term postoperative pain, significantly improves joint mobility, and more substantially restores shoulder function[32]. This study further validates these findings by examining the mid- to long-term efficacy of this approach.
This study has several limitations. First, residual LHBT pathology or excessive tension may lead to new pain. Second, compared to conventional double-row suture repair, LHBT transposition might increase the likelihood of postoperative shoulder joint adhesions. Future research with larger sample sizes and more extended follow-up periods is needed to observe the occurrence of these phenomena. Additionally, the retrospective nature of this study and the relatively small sample size may limit the generalizability of our results. Therefore, further prospective studies with larger cohorts are needed to validate these findings and enhance their applicability to broader populations.
Based on postoperative and follow-up data collection, we found that compared with the conventional double-row repair method, the double-row repair combined with LHBT transposition exhibited similar intraoperative parameters, resulted in less postoperative pain, facilitated faster shoulder function recovery, and ensured stable rotator cuff healing.
| 1. | Lädermann A, Denard PJ, Collin P. Massive rotator cuff tears: definition and treatment. Int Orthop. 2015;39:2403-2414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 114] [Article Influence: 11.4] [Reference Citation Analysis (4)] |
| 2. | Zhao J, Luo M, Pan J, Liang G, Feng W, Zeng L, Yang W, Liu J. Risk factors affecting rotator cuff retear after arthroscopic repair: a meta-analysis and systematic review. J Shoulder Elbow Surg. 2021;30:2660-2670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 111] [Article Influence: 27.8] [Reference Citation Analysis (4)] |
| 3. | Shah NS, Suriel Peguero E, Umeda Y, Crawford ZT, Grawe BM. Long-Term Outcomes of Massive Rotator Cuff Tear Repair: A Systematic Review. HSS J. 2022;18:130-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 31] [Article Influence: 10.3] [Reference Citation Analysis (4)] |
| 4. | Lo IK, Burkhart SS. Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy. 2004;20:250-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 100] [Article Influence: 4.8] [Reference Citation Analysis (4)] |
| 5. | Burkhart SS, Danaceau SM, Pearce CE Jr. Arthroscopic rotator cuff repair: Analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy. 2001;17:905-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 273] [Article Influence: 11.4] [Reference Citation Analysis (4)] |
| 6. | Berth A, Neumann W, Awiszus F, Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol. 2010;11:13-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 156] [Article Influence: 10.4] [Reference Citation Analysis (5)] |
| 7. | Hein J, Reilly JM, Chae J, Maerz T, Anderson K. Retear Rates After Arthroscopic Single-Row, Double-Row, and Suture Bridge Rotator Cuff Repair at a Minimum of 1 Year of Imaging Follow-up: A Systematic Review. Arthroscopy. 2015;31:2274-2281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 206] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 8. | Sobhy MH, Khater AH, Hassan MR, El Shazly O. Do functional outcomes and cuff integrity correlate after single- versus double-row rotator cuff repair? A systematic review and meta-analysis study. Eur J Orthop Surg Traumatol. 2018;28:593-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Mihata T, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Fujiwara K, Kinoshita M. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med. 2011;39:2091-2098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 156] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 10. | Hantes ME, Ono Y, Raoulis VA, Doxariotis N, Venouziou A, Zibis A, Vlychou M. Arthroscopic Single-Row Versus Double-Row Suture Bridge Technique for Rotator Cuff Tears in Patients Younger Than 55 Years: A Prospective Comparative Study. Am J Sports Med. 2018;46:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 11. | Fei W, Guo W. A biomechanical and histological comparison of the suture bridge and conventional double-row techniques of the repair of full-thickness rotator cuff tears in a rabbit model. BMC Musculoskelet Disord. 2015;16:148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Kovacevic D, Suriani RJ Jr, Grawe BM, Yian EH, Gilotra MN, Hasan SA, Srikumaran U, Hasan SS, Cuomo F, Burks RT, Green AG, Nottage WM, Theja S, Kassam HF, Saad MA, Ramirez MA, Stanley RJ, Williams MD, Nadarajah V, Konja AC, Koh JL, Rokito AS, Jobin CM, Levine WN, Schmidt CC; American Shoulder and Elbow Surgeons Massive Cuff Evaluation and Research Initiative (ASES MERIT) Investigators. Management of irreparable massive rotator cuff tears: a systematic review and meta-analysis of patient-reported outcomes, reoperation rates, and treatment response. J Shoulder Elbow Surg. 2020;29:2459-2475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 132] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 13. | Mihata T, Lee TQ, Hasegawa A, Kawakami T, Fukunishi K, Fujisawa Y, Itami Y, Ohue M, Neo M. Arthroscopic Superior Capsule Reconstruction Can Eliminate Pseudoparalysis in Patients With Irreparable Rotator Cuff Tears. Am J Sports Med. 2018;46:2707-2716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 160] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 14. | Boutsiadis A, Chen S, Jiang C, Lenoir H, Delsol P, Barth J. Long Head of the Biceps as a Suitable Available Local Tissue Autograft for Superior Capsular Reconstruction: "The Chinese Way". Arthrosc Tech. 2017;6:e1559-e1566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 15. | Liu T, Zhang MT, Zhou JP, Wu D, Yang ZT, Zhang BR, Yun XD. [Progress on arthroscopic surgery for massive rotator cuff tears]. Zhongguo Gu Shang. 2022;35:1177-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Ming WY, Wu XD, Dai HD, Li ZM, Chen L, Lin HM, Zhao JY. [Treatment of massive rotator cuff tears with modified Chinese-way technique]. Zhongguo Gu Shang. 2024;37:921-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Somerson JS, Hsu JE, Gorbaty JD, Gee AO. Classifications in Brief: Goutallier Classification of Fatty Infiltration of the Rotator Cuff Musculature. Clin Orthop Relat Res. 2016;474:1328-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 96] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 18. | Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;81-86. [PubMed] |
| 19. | Chiarotto A, Maxwell LJ, Ostelo RW, Boers M, Tugwell P, Terwee CB. Measurement Properties of Visual Analogue Scale, Numeric Rating Scale, and Pain Severity Subscale of the Brief Pain Inventory in Patients With Low Back Pain: A Systematic Review. J Pain. 2019;20:245-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 340] [Article Influence: 56.7] [Reference Citation Analysis (0)] |
| 20. | Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;160-164. [PubMed] |
| 21. | Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 755] [Cited by in RCA: 813] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 22. | Saccomanno MF, Cazzato G, Fodale M, Sircana G, Milano G. Magnetic resonance imaging criteria for the assessment of the rotator cuff after repair: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:423-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Taylor RS, Ullrich K, Regan S, Broussard C, Schwenkglenks M, Taylor RJ, Gordon DB, Zaslansky R, Meissner W, Rothaug J, Langford R; PAIN-OUT investigators. The impact of early postoperative pain on health-related quality of life. Pain Pract. 2013;13:515-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 24. | Britteon P, Cullum N, Sutton M. Association between psychological health and wound complications after surgery. Br J Surg. 2017;104:769-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 25. | Ma D, Yuan B, Li YM. [Comparison of clinical outcomes between long head of biceps tendon transposition and tenotomy in the treatment of massive rotator cuff tears]. Shiyong Guke Zazhi. 2022;28:679-685. [DOI] [Full Text] |
| 26. | Wan RW, Luo ZW, Yang YM, Zhang HL, Chen JN, Chen SY, Shang XL. Long head of biceps tendon transposition for massive and irreparable rotator cuff tears: A systematic review and meta-analysis. World J Orthop. 2023;14:813-826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Reference Citation Analysis (1)] |
| 27. | Kawashima K, Terabayashi N, Asano H, Akiyama H. Arthroscopic Long Head of the Biceps Transposition for Superior Capsular Augmentation Results in Comparable Clinical Outcomes to Arthroscopic Partial Repair for Irreparable Rotator Cuff Tears. Arthrosc Sports Med Rehabil. 2022;4:e425-e434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Deng B, Deng X, Liu S, Hao L. [Research progress of arthroscopic long head of biceps tendon transposition in treatment of irreparable massive rotator cuff tears]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36:249-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Teng Q, Mo ZY, Zheng XF, Li JR, Wang HJ, Zhang CW, Chen L, Hou HG. [Early clinical outcomes of arthroscopic long head of biceps tendon bridge graft combined with latissimus dorsi transfer for irreparable massive rotator cuff tears]. Zhonghua Jianzhou Waike Dianzi Zazhi. 2021;9: 341-347. [DOI] [Full Text] |
| 30. | Sugo H, Kawai M, Miyano S, Watanobe I, Machida M, Kitabatake T, Lee Y, Kojima K. Surgical Repair With Free Fascia Lata Graft in Patients at Risk of Surgical Site Infection: A Case Series. In Surg. 2019;104:69-74. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Kang Y, Guo B, Xu J, Bi W, Ma W, Yang D, Cui H, Fu P, Liu Y, Tian J, Liu Y. [Effectiveness of arthroscopic long head of biceps tendon transposition combined with Swivelock anchor double fixation for massive and irreparable rotator cuff tears]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36:1459-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Shang XL, Lv JY, Chen JW, Li H, Ge YS, Chen SY. [Clinical efficacy of arthroscopic lhbt transposition fixation-assisted superior capsular reconstruction (chinese way) for repairing massive and irreparable rotator cuff tears]. Zhongguo Yundong Yixue Zazhi. 2019;38:652-657. [DOI] [Full Text] |