Published online May 18, 2025. doi: 10.5312/wjo.v16.i5.106004
Revised: March 31, 2025
Accepted: April 11, 2025
Published online: May 18, 2025
Processing time: 92 Days and 19.9 Hours
Total knee arthroplasty (TKA) aims to restore motion and alleviate pain, enabling patients to return to daily activities. Despite advances in implants, surgery, and perioperative care, patient dissatisfaction rates remain significant.
To determine whether ankle symptoms are associated with inferior results of functional recovery of the knee following TKA.
This prospective study included all patients with advanced knee osteoarthritis who underwent a primary unilateral TKA between August 2019 and December 2019 with data documented by the treating surgeon and outpatient physical therapists. Patients were categorized based on ankle symptoms using the Ame
Postoperative KOOS, ROM, and VAS significantly improved in both groups (P < 0.001). However, at three months, KOOS (P = 0.02) and extension motion (P = 0.01) improvements were significantly greater in group 2.
These findings suggest that preoperative ankle symptoms may negatively impact early knee functional recovery, particularly in KOOS scores and extension motion.
Core Tip: Preoperative ankle symptoms may negatively impact early functional recovery following total knee arthroplasty (TKA). This study found that patients with ankle symptoms had significantly lower Knee Injury and Osteoarthritis Outcome Scores and reduced knee extension three months postoperatively compared to those without ankle symptoms. These findings highlight the importance of assessing and addressing ankle pathology before TKA to optimize postoperative outcomes. A comprehensive approach considering the biomechanical interplay between the knee and ankle may improve functional recovery and patient satisfaction after TKA.
- Citation: Buterin A, Vuckovic M, Spanja Prpic S, Zaharija V, Nonkovic M, Prpic T. Comparison of functional recovery of the knee following total knee arthroplasty in patients with and without ankle symptoms. World J Orthop 2025; 16(5): 106004
- URL: https://www.wjgnet.com/2218-5836/full/v16/i5/106004.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i5.106004
Osteoarthritis (OA) is a degenerative and progressive disease that affects all joint structures, ultimately leading to complete loss of cartilage in its terminal stage. Total knee arthroplasty (TKA) is considered the definitive treatment option for advanced knee OA. The global increase in TKA procedures has been documented worldwide, with more than 250 million affected individuals[1]. The goal of TKA is to restore motion and relieve pain in the knee, allowing the patient to resume daily activities, including work and sports. If knee function does not sufficiently recover, patients may experience knee stiffness, which can limit their quality of life[2]. Despite improvement in implant design, surgical techniques, and perioperative management, the patient dissatisfaction rate is still relatively high, up to 20%[3,4]. The causes of unsatisfactory outcomes following TKA can be both intra-articular and extra-articular.
The clinical presentation of patients awaiting or after TKA often includes ankle pain. Although the impact of knee OA on degenerative changes in the ankle joint is not yet fully understood, a clear association exists between the altered axial alignment of the thigh and knee and concurrent changes in the morphology of the ankle joint.
Studies have shown that knee varus or valgus can lead to ankle malalignment and an increase in ankle tilt[5,6]. After surgery, attention is fully focused on the knees; however, the pathological changes and the other adaptational changes in the ankle may affect the functional recovery in total. It is indicated that foot and ankle disorders may contribute to postoperative pain following TKA[7]. However, to date, there is no scientific evidence to support whether ankle symptoms affect the functional recovery of the knee following TKA. Therefore, the aim of this study is to determine whether ankle symptoms are associated with inferior results of functional recovery of the knee following TKA.
This prospective, single-center study with a level III of evidence was conducted from August 2019 to December 2019 at the University Hospital for Orthopaedics and Traumatology Lovran, Faculty of Medicine, University of Rijeka, Croatia. The study was conducted in accordance with the ethical standards of the institutional research committee (No. 02-272/2019) and with the 1964 Helsinki Declaration and its later amendments. Informed consent was obtained from all patients. It included all patients with advanced knee OA who underwent a primary unilateral TKA with data documented by the treating surgeon and outpatient physical therapists. The study was registered at Clinicaltrials.gov (NCT05751954) prior to patient inclusion. This study was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology checklist for observational research.
Inclusion criteria for the study included all patients undergoing a primary, unilateral TKA with advanced primary knee OA classified as Kellgren-Lawrence Grade 4[8]. Exclusion criteria included secondary OA of the knee (post-traumatic, rheumatoid, and other types of arthritis), previous surgical procedures on the knee and ankle involving deformity correction (corrective osteotomies) or joint fusion (arthrodesis), a history of knee or ankle osteosynthesis (including post-traumatic OA of the ankle), and an American Society for Anesthesiologists (ASA) score[9]. Following this criteria, 79 patients were included in the study. The patients were divided into two groups by their American Orthopaedic Foot and Ankle Society (AOFAS) score[10]. Patients with ankle symptoms (AOFAS score ≤ 85) were categorized into group 1, and patients without ankle symptoms (AOFAS score > 85) into group 2. AOFAS score of ≤ 85 was used to define symptomatic ankles, based on prior literature where this threshold has been interpreted as indicative of clinically relevant functional impairment[11]. This cutoff reflects a score below which patients typically report clinically relevant symptoms affecting pain, function, and alignment. Although AOFAS is a composite score and not solely symptom-based, it remains the most widely used and validated tool for evaluating ankle-related morbidity in orthopedic clinical evaluation. To determine the number of participants in the study, we used the number of participants in similar studies[12,13]. The absence of a power analysis represents a limitation and may affect the strength of the statistical conclusions.
The surgeries were performed by highly experienced senior orthopaedic surgeons specializing TKA. After surgical draping and inflating the air tourniquet to 250 mmHg in spinal anesthesia, a medial parapatellar arthrotomy was performed. The implant used was a posterior stabilized-type model of knee endoprosthesis with cemented femoral and tibial components. The patients started their range-of-motion and gait training one day after surgery with weight bearing as tolerated. During their hospital stay, patients performed protective exercises to improve the range of motion (ROM) of the knee joint, focusing on flexion and full extension, as well as strengthening exercises for the quadriceps and hamstring muscles. In addition, various physical modalities were used to reduce pain and joint swelling. Patients were advised to perform these exercises by themselves multiple times per day and to maintain this regimen after discharge. All patients were also referred to outpatient physical therapy.
Standard surgeon-based and physical therapist clinical assessments were performed. All measurements were conducted preoperatively and three months postoperatively during a regular follow-up in an outpatient clinic by a surgeon. The physical therapist conducted functional measurements and administered questionnaires. The questionnaires were completed under the supervision of clinicians to avoid incomplete or poorly filled-out forms. The following data were collected: (1) Age at the time of surgery; (2) Gender; (3) Body mass index (BMI); (4) Operated side (right or left); (5) ASA score; (6) Previous surgeries; (7) Comorbidities; (8) Knee active ROM; (9) Visual analogue scale (VAS) score; (10) AOFAS score; and (11) Knee Injury and Osteoarthritis Outcome Score (KOOS).
ROM: The active ROM in the knee joint, in terms of flexion and extension, was measured in the supine position using a goniometer.
Questionnaires: The AOFAS and KOOS scores were performed. AOFAS is patient-reported outcome measures for ankle conditions were assessed using the AOFAS questionnaire with a maximum score of 100 points[10]. It consists of a clinical evaluation that includes both a subjective and an objective evaluation of the patient. Patients describe their level of pain while the examiner measures the ROM of the ankle joint.
Patient-reported outcome measures for knee conditions were assessed using the KOOS questionnaire. The total scores from the five outcomes (symptoms, pain, activities of daily living, sports, and quality of life) were aggregated and scaled to a maximum of 100 points[14].
Pain: The VAS was used to evaluate pain in the knee, it ranges from 0 (no pain) to 10 (worst imaginable pain)[15]. The VAS scale is simple to use in clinical practice and has proven to be a valid measurement tool.
Normal distribution was determined with the Shapiro-Wilk test. Student t-test for independent samples was used to analyze normally distributed parameters, Mann Whitney U-test for non-normal distribution, Wilcoxon Signed-Rank test for paired data and χ2 test for nominal samples. Multivariable linear and logistic regression analyses were performed to identify independent predictors of postoperative outcomes. Normally distributed variables were presented using means and SD. Non-normal variables were reported as median and interquartile range (IQR). A P value < 0.05 was considered statistically significant. All statistical analyses were performed using IBM Statistical Package for the Social Sciences Statistics version 29.0.2.0 for MacOS.
From the total number of 79 patients enrolled in this study 30 patients with concomitant ankle symptoms (AOFAS score before TKA ≤ 85) were categorized into group 1, and 49 patients without ankle symptoms (AOFAS score before TKA > 85) were categorized into group 2 (Table 1).
| Group 1 (n = 30) | Group 2 (n = 49) | ||
| Gender | Male | 6 (20) | 26 (53.06) |
| Female | 24 (80) | 23 (46.94) | |
| Male-to-female ratio | 0.25 | 1.13 | |
| Operated side | Right | 18 (60) | 26 (53.06) |
| Left | 12 (40) | 23 (46.94) | |
| Age (years) | Mean SD | 73.33 ± 6.94 | 68.98 ± 7.18 |
| Minimum | 61 | 49 | |
| Maximum | 86 | 84 | |
| Body mass index (kg/m2) | Mean SD | 30.79 ± 5.54 | 30.72 ± 4.56 |
| American Society for Anesthesiologists score | 1 | 1 (3.33) | 12 (24.49) |
| 2 | 14 (46.67) | 18 (36.73) | |
| 3 | 15 (50) | 19 (38.78) |
Analysis of baseline characteristics showed a statistically significant difference in both age and gender between the two groups. Patients in group 1 were, on average, older than those in group 2, and the proportion of male participants was lower. Patients were included consecutively as they presented for surgical treatment, which reflects the actual gender distribution of patients undergoing TKA in clinical practice (Table 2).
| Group 1 | Group 2 | P value | |
| Age (years) (mean SD) | 73.33 ± 6.94 | 68.98 ± 7.18 | 0.01 |
| Male-to-female ratio | 0.25 | 1.13 | 0.01 |
| Body mass index (kg/m2) (mean SD) | 30.79 ± 5.54 | 30.72 ± 4.56 | 0.96 |
The following measured parameters do not have a normal distribution as tested by the Shapiro-Wilk test. A statistically significant difference was observed in the preoperative AOFAS scores, flexion motion and VAS between the two groups, while no significant difference was noted in KOOS scores and extension motion (Table 3).
| Group 1 | Group 2 | P value | |
| Median (IQR) | Median (IQR) | ||
| American Orthopaedic Foot and Ankle Society | 77.5 (71.25-82) | 97 (93-99) | < 0.001 |
| Knee Injury and Osteoarthritis Outcome Score | 36 (26.25-42.75) | 40 (32-49) | 0.18 |
| Flexion | 95 (80-100) | 110 (100-120) | 0.03 |
| Extension | 5 (0-15) | 0 (0-10) | 0.16 |
| Visual analogue scale | 6 (4-7) | 7 (5-8) | 0.04 |
Preoperative ROM, KOOS, and VAS scores in both groups were unsatisfactory. Postoperative analysis revealed significant improvements in KOOS, ROM, and VAS within each group, indicating positive surgical outcomes. Statistically significant differences were noted in flexion, extension, KOOS, and VAS three months postoperatively compared to preoperative values (P < 0.001). No intraoperative or postoperative complications were reported in any patient.
In group 1, the AOFAS score improved significantly at three months postoperatively in patients with ankle complaints and a lower preoperative AOFAS score. The preoperative AOFAS score (median = 77.5, IQR = 71.25–82) increased significantly to 87.5 (IQR = 83–96) three months postoperatively (P < 0.001).
For patients in group 2, no statistically significant differences were found between the preoperative and three months postoperative AOFAS scores (P = 0.73).
When comparing the functional outcomes between group 1 and group 2, significant differences were found in KOOS and in extension motion at three months postoperatively (Table 4). However, no significant differences were observed in flexion motion, or VAS at three months postoperatively.
| Group 1 | Group 2 | P value | |
| Median (IQR) | Median (IQR) | ||
| American Orthopaedic Foot and Ankle Society | 87.5 (83-96) | 96 (94-100) | < 0.001 |
| Knee Injury and Osteoarthritis Outcome Score | 67 (59.25-71.75) | 72 (65-78) | 0.02 |
| Flexion | 100 (90-110) | 110 (100-120) | 0.05 |
| Extension | 0 (0-5) | 0 (0-0) | 0.01 |
| Visual analogue scale | 2 (1-4) | 3 (2-4) | 0.17 |
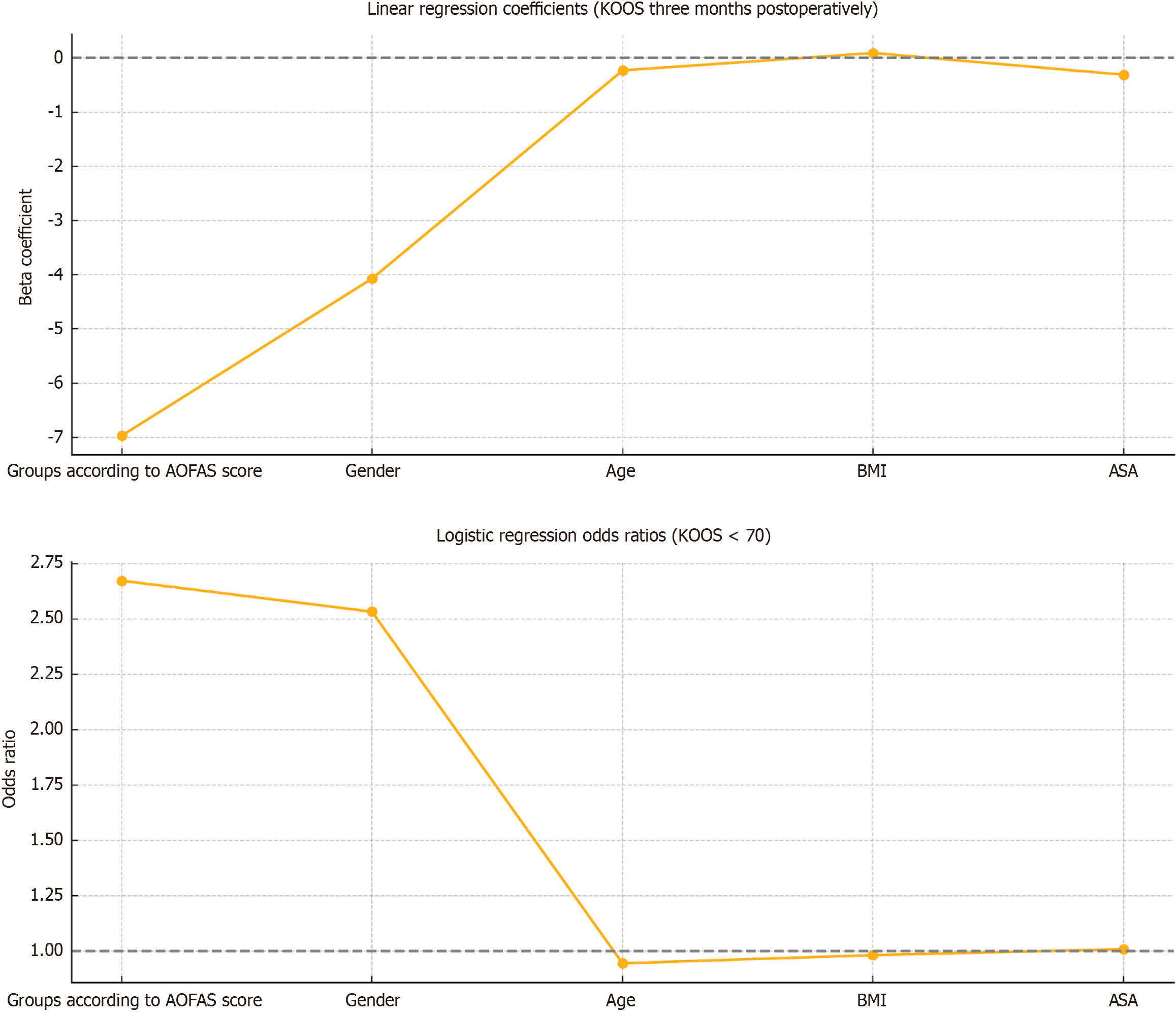
We acknowledge the potential influence of baseline differences in gender and age between groups. To account for this, we performed multivariable linear and logistic regression analyses including gender, age, BMI, and ASA score as covariates. In multivariable linear regression analysis, preoperative ankle symptoms (AOFAS ≤ 85) were identified as an independent predictor of lower KOOS scores at three months postoperatively (β = –6.97, P = 0.04), after adjusting for age, sex, BMI, and ASA score. Furthermore, logistic regression revealed a trend toward increased odds of a suboptimal functional outcome (defined as KOOS < 70) in patients with ankle symptoms (odds ratio = 2.67, P = 0.07), although this did not reach statistical significance (Figure 1).
This study assessed the strengths of the relationship between preoperative ankle symptoms and the functional recovery following TKA and yielded important insights into how these symptoms may influence knee outcomes. The principal findings of this study were as follows: Patients with ankle symptoms before TKA showed significantly inferior KOOS and extension three months postoperatively compared to patients without ankle symptoms prior to TKA and the AOFAS score improved significantly at three months postoperatively in patients with ankle symptoms before TKA. These associations remained significant even after controlling for potential confounding variables. Multivariable linear regression confirmed that ankle symptoms were an independent predictor of poorer KOOS outcomes, while logistic regression demonstrated a trend toward increased risk of suboptimal recovery. Poorer outcomes were defined as KOOS scores below 70, a threshold commonly used in the literature to indicate moderate functional limitation after TKA[16].
These results suggest that preoperative ankle symptoms may negatively impact certain functional outcomes following TKA. The observation that patients with preoperative ankle symptoms had inferior KOOS and extension outcomes at three months postoperatively highlights the potential impact of extra-articular factors on early recovery after TKA. The biomechanical interplay between the knee and ankle might affect postoperative outcomes, as a misaligned or symptomatic ankle could contribute to altered gait patterns and weight distribution.
The fact that the AOFAS score improves after TKA in patients who had preoperative ankle symptoms raises a series of questions about how knee arthroplasty affects the ankle. This improvement suggests that despite the presence of ankle-related issues before surgery, these patients can experience meaningful recovery in ankle function after TKA. One possible explanation is the improvement in overall lower limb alignment and gait mechanics following TKA, which may reduce compensatory overload on the ankle. However, this remains speculative, and future studies incorporating radiographic measurements and pedobarography could provide a more detailed understanding of how TKA affects the ankle. According to the available scientific literature, the suggested approach for performing multiple joint arthroplasties on the same limb when both hip and knee issues are present is to proceed from the proximal to the distal joint, as this is thought to optimize alignment control[17]. However, no consensus has been reached in the scientific literature regarding the optimal sequence of surgeries for patients with both knee and ankle symptoms.
According to Ro et al[18], a significant number of patients have changes in multiple joints of the lower extremity, indicating that dysfunction in one joint is biomechanically related to changes in other joints. Many patients undergoing TKA have both knee and ankle pathology, it appears likely that compensatory changes occur in each joint in response to deformity in the other[16].
Varus or valgus deformity of the knee should be corrected to a neutral position following TKA to ensure longer survival of the implant. Few studies have addressed how ankle alignment changes after TKA, but none of them included functional questionnaires. Chandler et al[19] concluded that the alignment of the ankle joint decreased by half of the total preoperative value after TKA. Larger preoperative deformities resulted in greater postoperative changes. Valgus deformities of the talocrural and subtalar joints remained in the valgus, and varus deformities remained in the varus, but the degree of the deformity was reduced by half[19]. In contrast, Takenaka et al[20] and Hara et al[21] reported different findings, suggesting that correction of varus knee deformity in patients with compensatory ankle valgus postoperatively leads to the development of ankle varus. Hara et al[21] also noted that in 30% of patients with varus knee deformity, varus ankle deformity was present due to the absence of a compensatory mechanism. It is assumed that in such patients, clinical deterioration may be expected following TKA. Gursu et al[22] highlight that although TKA is well-known for its success in alleviating knee pain and restoring lower limb alignment, there is still no consensus regarding its effects on the ankle and hip joints, which remains unclear. It has been reported that foot and ankle disorders can be a potential source of pain following TKA. While the knee joint is the primary focus of TKA, findings suggest that the overall biomechanical alignment of the lower limb, including the ankle, may play a crucial role in determining the success of the surgery[22]. Diao et al[23] indicate that correction of hip-knee-ankle angle after TKA tends to promote adjustment in the ankle alignment toward re-balance of the whole lower limb weight-bearing axis and that this mechanism weakens in elderly patients. Their study was also prospective in nature, and in addition to radiological analysis, they evaluated AOFAS scores both before and three months after TKA (76.5 ± 10.89 vs 90.4 ± 6.05, P < 0.001)[23]. Their results are consistent with the findings of our study.
However, it remains important to note that those early postoperative deficits in function, particularly in terms of extension, could still have a substantial impact on short-term quality of life and rehabilitation progress. Although the difference in KOOS between groups reached statistical significance (P = 0.02), the observed median difference of 5 points may not fully meet the threshold for clinical relevance. A recent prospective study by Nishimoto et al[24] reported minimal clinically important differences for KOOS ranging from 6 points to 10 points at three months postoperatively in patients undergoing TKA.
Interestingly, although KOOS scores showed statistically significant differences between groups postoperatively, VAS scores did not (P = 0.17). The absence of significant differences in VAS scores despite differences in KOOS suggests a possible dissociation between pain and functional capacity. This discrepancy may reflect the multidimensional nature of the KOOS questionnaire, which assesses not only pain but also function, symptoms, and quality of life, whereas VAS captures only the subjective intensity of pain at a single time point. Therefore, the lower KOOS scores in group 1 may indicate that these patients had more difficulty with everyday activities or experienced a slower recovery, even if their pain levels were similar. Other factors, such as individual rehabilitation involvement, comorbidities, or psychological factors—may have contributed to this discrepancy.
Furthermore, these findings may encourage clinicians to consider an entire and more individual approach to the assessment of patients with knee OA, looking beyond the knee joint itself and evaluating the ankle for potential malalignment or degeneration that could influence TKA outcomes.
We must note that the limitation of this study was the relatively small sample size, which could limit the applicability of our findings. Additionally, this study was conducted at a single center, and the results may not be reflective of practices in other settings. Future studies with larger, more diverse populations, longer follow-up periods, and radiological analysis are needed to confirm these findings and further investigate the relationship between ankle pathology and knee recovery after TKA.
This study highlights the importance of considering preoperative ankle symptoms when evaluating functional recovery following TKA. We conclude that ankle symptoms affect early functional recovery in patients undergoing TKA. Early recognition and management of ankle symptoms may improve overall postoperative outcomes and lead to more individualized rehabilitation strategies for patients undergoing TKA.
| 1. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2079] [Cited by in RCA: 3260] [Article Influence: 181.1] [Reference Citation Analysis (0)] |
| 2. | Kornuijt A, de Kort GJL, Das D, Lenssen AF, van der Weegen W. Recovery of knee range of motion after total knee arthroplasty in the first postoperative weeks: poor recovery can be detected early. Musculoskelet Surg. 2019;103:289-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1654] [Cited by in RCA: 1851] [Article Influence: 123.4] [Reference Citation Analysis (0)] |
| 4. | Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J Arthroplasty. 2017;32:3854-3860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 530] [Article Influence: 66.3] [Reference Citation Analysis (0)] |
| 5. | Xie K, Jiang X, Han X, Ai S, Qu X, Yan M. Association Between Knee Malalignment and Ankle Degeneration in Patients With End-Stage Knee Osteoarthritis. J Arthroplasty. 2018;33:3694-3698.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 6. | Canovas F, Dagneaux L. Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res. 2018;104:S41-S46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 243] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 7. | Manning BT, Lewis N, Tzeng TH, Saleh JK, Potty AG, Dennis DA, Mihalko WM, Goodman SB, Saleh KJ. Diagnosis and Management of Extra-articular Causes of Pain After Total Knee Arthroplasty. Instr Course Lect. 2015;64:381-388. [PubMed] |
| 8. | Kohn MD, Sassoon AA, Fernando ND. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474:1886-1893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 852] [Cited by in RCA: 850] [Article Influence: 94.4] [Reference Citation Analysis (0)] |
| 9. | Knuf KM, Maani CV, Cummings AK. Clinical agreement in the American Society of Anesthesiologists physical status classification. Perioper Med (Lond). 2018;7:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 10. | Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3199] [Cited by in RCA: 3117] [Article Influence: 100.5] [Reference Citation Analysis (0)] |
| 11. | D'souza JJ. American Orthopedic Foot-and-Ankle Society Score, Where Are We Now? – A Narrative Review of Quality of Life Measures in Foot-and-Ankle Surgery. Open Access Maced J Med Sci. 2020;8:133-136. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Mansur H, Rocha FA, Garcia PBL, de Alencar FHU, Guilme P, de Castro IM. Alteration of Hindfoot Axis After Total Knee Arthroplasty. J Arthroplasty. 2019;34:2376-2382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Mansur H, Rocha FA, Sousa PGT, Castro IM. Relationship Between the Knee and Hindfoot Axes in Patients with Severe Knee Osteoarthritis. Acta Ortop Bras. 2020;28:229-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Gandek B, Ware JE Jr. Validity and Responsiveness of the Knee Injury and Osteoarthritis Outcome Score: A Comparative Study Among Total Knee Replacement Patients. Arthritis Care Res (Hoboken). 2017;69:817-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. 2008;31:165-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 364] [Cited by in RCA: 546] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 16. | Norton AA, Callaghan JJ, Amendola A, Phisitkul P, Wongsak S, Liu SS, Fruehling-Wall C. Correlation of knee and hindfoot deformities in advanced knee OA: compensatory hindfoot alignment and where it occurs. Clin Orthop Relat Res. 2015;473:166-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 122] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 17. | Head WC, Paradies LH. Ipsilateral hip and knee replacements as a single surgical procedure. J Bone Joint Surg Am. 1977;59:352-354. [PubMed] |
| 18. | Ro DH, Lee J, Lee J, Park JY, Han HS, Lee MC. Effects of Knee Osteoarthritis on Hip and Ankle Gait Mechanics. Adv Orthop. 2019;2019:9757369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 19. | Chandler JT, Moskal JT. Evaluation of knee and hindfoot alignment before and after total knee arthroplasty: a prospective analysis. J Arthroplasty. 2004;19:211-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | Takenaka T, Ikoma K, Ohashi S, Arai Y, Hara Y, Ueshima K, Sawada K, Shirai T, Fujiwara H, Kubo T. Hindfoot alignment at one year after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:2442-2446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Hara Y, Ikoma K, Arai Y, Ohashi S, Maki M, Kubo T. Alteration of hindfoot alignment after total knee arthroplasty using a novel hindfoot alignment view. J Arthroplasty. 2015;30:126-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 22. | Gursu S, Sofu H, Verdonk P, Sahin V. Effects of total knee arthroplasty on ankle alignment in patients with varus gonarthrosis: Do we sacrifice ankle to the knee? Knee Surg Sports Traumatol Arthrosc. 2016;24:2470-2475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Diao N, Yu F, Yang B, Ma L, Yin H, Guo A. Association between changes in hip-knee-ankle angle and hindfoot alignment after total knee arthroplasty for varus knee osteoarthritis. BMC Musculoskelet Disord. 2021;22:610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Nishimoto J, Tanaka S, Inoue Y, Tanaka R. Minimal clinically important differences in short-term postoperative Knee injury and Osteoarthritis Outcome Score (KOOS) after total knee arthroplasty: A prospective cohort study. J Orthop Trauma Reha. 2024;31:15-20. [DOI] [Full Text] |