Published online May 18, 2022. doi: 10.5312/wjo.v13.i5.494
Peer-review started: March 3, 2021
First decision: July 28, 2021
Revised: September 14, 2021
Accepted: April 22, 2022
Article in press: April 22, 2022
Published online: May 18, 2022
Processing time: 435 Days and 12.2 Hours
Non-steroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed medications in the United States. Although they are safe and effective means of analgesia for children with broken bones, there is considerable variation in their clinical use due to persistent concerns about their potentially adverse effect on fracture healing.
To assess whether NSAID exposure is a risk factor for fracture nonunion in children.
We systematically reviewed the literature reporting the effect of NSAIDs on bone healing. We included all clinical studies that reported on adverse bone healing complications in children with respect to NSAID exposure. The outcomes of interest were delayed union or nonunion. Study quality was assessed using the Newcastle-Ottawa scale for non-randomized studies. A final table was constructed summarizing the available evidence.
A total of 120 articles were identified and screened, of which 6 articles were included for final review. Nonunion in children is extremely rare; among the studies included, there were 2011 nonunions among 238822 fractures (0.84%). None of the included studies documented an increased risk of nonunion or delayed bone healing in those children who are treated with NSAIDs in the immediate post-injury or peri-operative time period. Additionally, children are likely to take these medications for only a few days after injury or surgery, further decreasing their risk of adverse side-effects.
This systematic review suggests that NSAIDS can be safely prescribed to pediatric orthopaedic patients absent other contraindications without concern for increased risk of fracture non-union or delayed bone healing. Additional prospective studies are needed focusing on higher risk fractures and elective orthopaedic procedures such as osteotomies and spinal fusion.
Core Tip: Non-steroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed medications in the United States. To assess whether NSAID exposure is a risk factor for fracture nonunion in children. We systematically reviewed the literature reporting the effect of NSAIDs on bone healing. This systematic review suggests that NSAIDS can be safely prescribed to pediatric orthopaedic patients absent other contraindications without concern for increased risk of fracture non-union or delayed bone healing.
- Citation: Stroud S, Katyal T, Gornitzky AL, Swarup I. Effect of non-steroidal anti-inflammatory drugs on fracture healing in children: A systematic review. World J Orthop 2022; 13(5): 494-502
- URL: https://www.wjgnet.com/2218-5836/full/v13/i5/494.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i5.494
Non-steroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed medications in the United States as well as some of the most frequently purchased over-the-counter analgesics. They work via inhibition of cyclooxygenase (COX) isoforms, including COX-1 and COX-2, to decrease downstream production of pro-inflammatory prostaglandins and thromboxane, a mediator of thrombogenesis and platelet function. COX-2 is involved in chondrocyte differentiation and is expressed in both osteoblasts and fracture callus[1,2]. Relating to fracture healing, a study of human callus found a thirteen-fold decrease in COX-2 expression in the callus of nonunions as compared to that of healed fractures[3].
As a result of these findings, the effects of NSAIDs on bone healing are an active area of study. Although eight animal studies suggest decreased callus formation and quality in animals exposed to NSAIDs[4-11], other investigations have found no difference in callus quality or healing rates[12-15]. One possible explanation for these discordant findings is a lack of standardization of agent, COX enzyme specificity, duration of therapy, and dose. Across the adult fracture nonunion literature, NSAIDs have both been associated with nonunion and found to have no effect on nonunion rates[16-20]. Nevertheless, despite these contradictory findings, a recent survey of orthopaedic surgeons found that 86% believe NSAIDs to be a risk factor for nonunion[21].
Additionally, very little is known about the effects of NSAID use on bone healing in children. Notably, nonunions in pediatric patients are exceedingly rare, with one epidemiological study suggesting that only 1 in 500 pediatric fractures goes on to nonunion[22]. This is an order of magnitude lower than the nonunion rate across all fractures in adults, which is estimated at 1.9%-6.8%[23,24]. The biological underpinnings of this difference in risk are theorized to include a robust periosteum which provides centripetal blood flow, greater innate regenerative potential, ongoing osteogenesis, and increased vascularity with greater fracture hematoma formation[25]. Further supporting their use, evidence has arisen indicating that NSAIDs are equally or more effective for post-fracture pain control than opiates while also leading to fewer side effects[22,26-29]. Reported side effects include bleeding complications due to inhibition of thromboxane formation and gastritis, which are common in adults but rare in children.
Clinically, there is considerable variation in the use of NSAIDs in pediatric fractures, likely due to varying reports in the literature and extrapolation of results from studies in other populations. There have been recent publications focusing on the use of NSAIDs for pediatric fractures and the goal of this systematic review was to assess whether NSAID exposure is a risk factor for fracture nonunion in children. In doing so, we hope to clarify the safety profile of NSAIDs in order to optimize their use in standard, multimodal analgesic regimens across pediatric orthopaedic fracture care.
We performed a computerized search using MEDLINE (PubMed platform), Cochrane Database, and Web of Science. The author (Katyal T) identified and utilized a combination of keywords and MeSH terms for “fracture”, “bone healing”, and “pediatric” patient population. The searches were performed in November 2020. Results were limited by language, English, but not by publication date. We included all English language, full-text articles of human subjects focusing on pediatric patients with fractures, post-fracture NSAID exposure, and control cohorts without NSAID exposure. Outcomes of interest were the reported rates of delayed unions, malunion, growth disturbance, and nonunions. Case reports and case series with less than 10 patients were excluded. All relevant randomized controlled trials, retrospective reviews, cohort, and case-control studies were included.
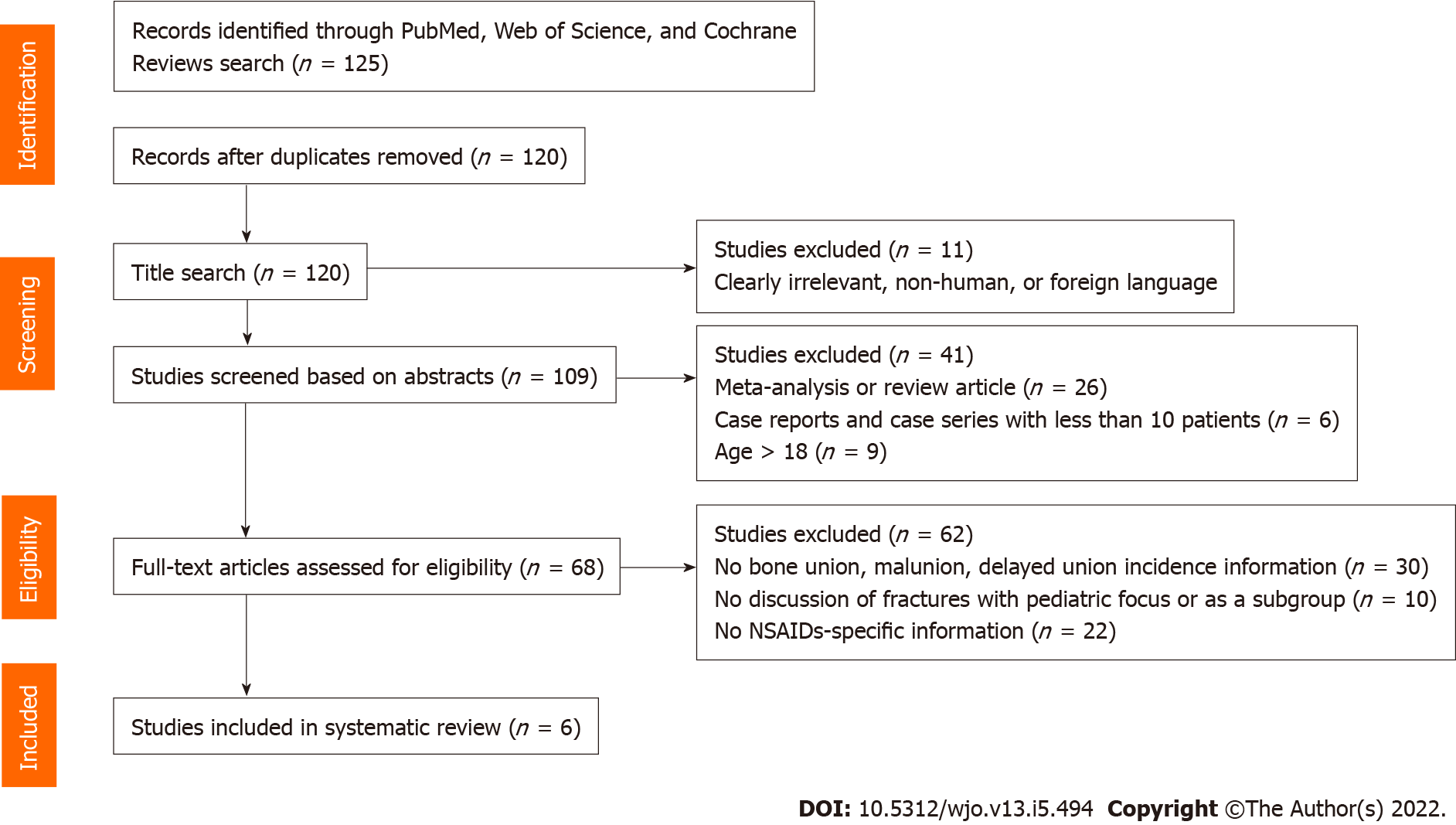
Each title from the performed search was assessed for inclusion based on the specified criteria described above (Figure 1). The relevant abstracts were then independently reviewed by two authors (Katyal T and Stroud S) for inclusion, and if there was any doubt regarding the relevance and applicability, the full-text article was obtained. Full-text articles of the selected abstracts were then appraised by two authors (Katyal T and Stroud S) for inclusion in the systematic review. Any conflicts in screening were resolved by a third author (Gornitzky AL). Two authors (Stroud S and Gornitzky AL) then independently extracted relevant data including age, number of patients in sample size, NSAID class, comparison group, rate of delayed healing and/or nonunion rate, results specific to NSAID type, and details concerning duration of exposure, length of follow-up, and definition of delayed union or nonunion. Study quality was assessed independently using the Newcastle-Ottawa scale (NOS) for the nonrandomized studies from the final list of articles (Table 1). Nonrandomized studies with an NOS score of five or greater on the nine-point scale were included.
| Ref. | Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis | Assessment of outcome | Was follow-up long enough for outcomes to occur? | Adequacy of follow up of cohorts | Total, n |
| Zura et al[30], 2018 | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||
| Kay et al[31], 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||
| Kay et al[32], 2011 | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||
| DePeter et al[33], 2017 | 1 | 1 | 1 | 1 | 2 | 1 | 7 |
In total, 120 unique articles were identified. As demonstrated in the PRISMA flow diagram (Figure 1), 114 articles were excluded from final analysis, including 11 articles after review of titles, 41 studies after screening of abstracts and 62 studies after assessment of full-text articles. Six studies were included for final analysis review (Table 2).
| Study | Ref. | Level of evidence |
| Risk factors for nonunion of bone fracture in pediatric patients: An inception cohort study of 237033 fractures | Zura et al[30], 2018 | Level II |
| Perioperative ketorolac use in children undergoing lower extremity osteotomies | Kay et al[31], 2010 | Level III |
| Complications of ketorolac use in children undergoing operative fracture care | Kay et al[32], 2011 | Level III |
| Does the use of ibuprofen in Children with extremity fractures increase their risk for bone healing complications? | DePeter et al[33], 2017 | Level I |
| A randomized clinical trial of ibuprofen versus acetaminophen with codeine for acute pediatric arm fracture pain | Drendel et al[34], 2009 | Level I |
| Effect of NSAID use on bone healing in pediatric fractures: A preliminary, prospective, randomized, blinded study | Nuelle et al[35], 2020 | Level I |
Analyzing an insurance claims database including more than 237000 pediatric fractures, Zura et al[30] reported a cumulative pediatric nonunion rate of less than 1%, which was 80% lower than adults. Specifically, age was directly related to risk of nonunion, increasing from 0.20% in those 0-6 years old to 0.26% in those 7-11 years and 1.63% in those 12-17 years old. With respect to NSAIDs, the authors found that prescription NSAID use alone did not increase the risk of nonunion [odds ratio (OR) = 1.05; 95% confidence interval (CI): 0.81-1.35; Table 3]. In comparison, the risk of nonunion did increase when NSAIDs were combined with opioids (OR = 2.52; 95%CI: 2.18-2.91), including a more than two-fold increase for those using opioids alone (OR = 2.47; 95%CI: 2.18-2.78)[1].
| Ref. | Study population | Age | Number of patients | NSAID studied | Comparison group | Delayed healing/nonunion rate (%) | NSAID specific results | Notes |
| Zura et al[30], 2018 | 18 most commonly fractures | < 18 yr | 237033 | All prescription NSAIDs | No analgesics | 0.85 | Multivariate OR for nonunion was 1.05 (95% CI: 0.81-1.35) for ‘NSAID’ vs ‘No analgesic’ group | Data from a large, private insurance database in the United States from 2011. Included both operative and nonoperatively managed fractures |
| Kay et al[31], 2010 | Operative fracture care | Mean = 6.7 yr | 221 | Ketorolac | No ketorolac | 0 | There were no cases of delayed union or nonunion in either group | Included 169 patients who received ketorolac vs 52 who did not. Only accounted for NSAID use in the immediate post-operative period. Fractures were predominantly in the upper extremity |
| Kay et al[32], 2011 | Lower extremity osteotomies | Mean = 8.5 yr | 327 patients (682 osteotomies) | Ketorolac | No ketorolac | 0.70 | Delayed healing in 0.6% in the ketorolac group (4/625) vs 1.8% in the control group (1/57; P = 0.89) | Included osteotomies of the pelvis, femur, tibia and foot. Only accounted for NSAID use in the immediate post-operative period |
| DePeter et al[33], 2017 | Fractures of the tibia, femur, humerus, scaphoid or fifth metatarsal | Median = 7 yr | 808 | Ibuprofen | No ibuprofen | 1.4 | 3% (10/338) of ibuprofen group developed a bone healing complication vs 4% (17/470) of controls (OR = 0.8, 95%CI: 0.4-1.8) | Exposure to ibuprofen included either administration during hospitalization or a prescription for ibuprofen at discharge. A bone healing complication was defined as radiographic evidence of nonunion, delayed union or future re-displacement as determined by a pediatric radiologist. Total complications (27/808; 3.5%) included 1% (n = 8) with nonunion, 0.4% (n = 3) with delayed union and 2% (n = 16) with re-displacement |
| Drendel et al[34], 2009 | Upper extremity fractures (non-op) | Mean = 7.8 yr | 244 patients | Ibuprofen | Acetaminophen with codeine | 0 | No documented fracture nonunions | Excluded fractures that required reduction/manipulation or surgery. Four (1.6%) children had another fracture at the same site within 1 yr of the original fracture, including 3 who had received acetaminophen and 1 received ibuprofen |
| Nuelle et al[35], 2020 | Skeletally immature patients with long-bone fractures | Mean = 7.7 yr | 95 patients (97 fractures) | Ibuprofen | Acetaminophen | 0 | At 6 wk, there was radiographic healing in 92% of the NSAID group vs 82% of the control group (P = 0.22). This increased to 100% and 98%, respectively, at 10-12 wk post-injury (P = 0.48) | Included females < 16 and males < 14 with open physes. Fractures managed both operatively and nonoperatively. Healing was documented at a mean of 41 d in the control group and 40 d in the NSAID group (P = 0.76). No cases of nonunion were documented in either group |
In a series of retrospective studies looking at NSAID use in children, some studies concluded that routine perioperative ketorolac use after orthopaedic surgery is not associated with an increased risk of delayed bone healing or nonunion[31,32]. This included both routine operative fracture care (0% nonunion rate after ketorolac use)[31] and lower extremity deformity correction[32]. Looking further at the high-risk osteotomy cohort, only 5 out of 682 osteotomies (0.7%) were complicated by delayed union or nonunion, with all 4 delayed unions in the ketorolac group (4/625; 0.6%) going on to heal completely without surgery[32]. Similarly, DePeter et al[33] retrospectively analyzed all children who presented to their emergency department with a fracture of the tibia, femur, humerus, scaphoid or fifth metatarsal. Comparing those who received ibuprofen to those who did not, the authors found no differences in the rate of nonunion, delayed union or fracture re-displacement on follow-up radiographs, leading them to conclude that ibuprofen administration is not associated with an increased risk for clinically important bone healing complications following traumatic fractures in kids.
There have been two prospective, randomized clinical trials in children looking at fracture healing following ibuprofen administration. First, Drendel et al[34] reported no instances of nonunion at minimum 1-year follow-up in 244 children managed nonoperatively with either ibuprofen or acetaminophen with codeine for pediatric upper extremity fractures. Of those who did have a refracture at the same site within 1 year of the original injury (n = 4; 1.6%), only 1 had received ibuprofen. Finally, Nuelle et al[35] compared ibuprofen to acetaminophen administration following long-bone fractures in 95 skeletally immature children. Overall, they reported no difference in radiographic healing at 6- or 12-wk post-injury, including 100% healing in the NSAID group by 12 wk post-fracture.
Overall, the included studies show that nonunion in children is extremely rare, and no published study to date has documented an increased risk of nonunion or delayed bone healing in those children who are treated with NSAIDs in the immediate post-injury or peri-operative time period.
The present review identified six studies that examined the effects of NSAID exposure on nonunion or delayed union in pediatric patients. Among the studies included, there were 2011 nonunions among 238822 fractures (0.84%). Of these studies, three examined the effects of ibuprofen in the acute post-fracture period, three studied ketorolac in the same time frame, and one was a database study that did not capture the specific agent or the timing of NSAID exposure. None of the six studies found NSAID exposure to be a risk factor for nonunion or delayed union in children, including a retrospective review that focused on bones with an innately higher risk for nonunion[33]. In contrast, in their large database study, Zura et al[30] found age (especially over 11 years), bone (e.g., scaphoid, femoral neck, tibia or fibula), male sex, higher body mass index, open fracture, or multiple concomitant fractures to be risk factors for pediatric nonunion.
From a clinical perspective, NSAID exposure is not associated with increased risk of bleeding, blood transfusions, or wound complications[31,32,35]. Specifically, of the six studies included, four did not examine the rate of wound complications and the two studies that did found no difference between the NSAID and non-NSAID groups[31,32]. In fact, NSAIDs are associated with both a lower risk of adverse effects and a lower rate of functional impairment[34]. Furthermore, NSAIDs are safe, cheap and effective opioid-sparing analgesics[22,26,27,34]. Unfortunately, due in part to persistent concerns regarding delayed fracture healing, they are a frequently underutilized medication[36].
Of note, most of the included studies have methodological limitations. First, Zura et al[30] did not capture whether NSAID exposure was acute or chronic and was focused only on a specific cohort whose parents had employer-supplied health insurance, which may not be generalizable to all patients. Next, while two of the three retrospective reviews were able to report a standardized dose of ketorolac, the third did not. Additionally, none of the three were able to control for concomitant opioid use or medications that may have been purchased over the counter and administered by parents after discharge[31-33]. In one of the two randomized controlled trials, each experimental group was sent home with both drugs and instructed to take the other group’s medication if they experienced breakthrough pain, thus making it difficult to exclude potential cross-over effect[34]. Third, none of the included studies examined COX-2 specific inhibitors or the effects of longer-term NSAID exposure on pediatric nonunion risk. For this reason, conclusions are limited to ibuprofen and ketorolac use in the acute period. Finally, nonunion in children is very rare, and many of the included studies reported zero nonunions, thus suggesting an overall limitation in study power.
Despite these limitations, however, it is still possible to draw several meaningful conclusions. First, nonunion in children is extremely rare across most age groups and fracture types, including those deemed ‘high risk’. Second, at standard doses in the acute post-injury/surgery period, both ibuprofen and ketorolac do not appear to be associated with an increased risk for nonunion or delayed union in pediatric patients. These findings are specific to upper extremity and long bone fractures. Moreover, children are likely to take these medications for only a few days after injury, another factor which decreases their exposure to any potential deleterious effects on osteogenesis. For example, Nuelle et al[35] reported that ibuprofen was used for only 4 d on average in their prospective cohort.
Finally, NSAIDs are safe in children and are associated with a decreased risk of adverse effects and equivalent analgesia to opioid-containing agents. Taken together, this systematic review suggests that NSAIDS can be safely prescribed to pediatric orthopaedic patients absent other contraindications without concern for increased risk of fracture non-union or delayed healing. Additional prospective studies are needed focusing on higher risk fractures and elective orthopaedic procedures such as osteotomies and spinal fusion.
Non-steroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed medications in the United States. Although they are safe and effective means of analgesia for children with broken bones, there is considerable variation in their clinical use due to persistent concerns about their potentially adverse effect on fracture healing.
The goal of this systematic review was to assess whether NSAID exposure is a risk factor for fracture nonunion in children.
The goal of this systematic review was to assess whether NSAID exposure is a risk factor for fracture nonunion in children.
We systematically reviewed the literature reporting the effect of NSAIDs on bone healing. We included all clinical studies that reported on adverse bone healing complications in children with respect to NSAID exposure. The outcomes of interest were delayed union or nonunion. Study quality was assessed using the Newcastle-Ottawa scale for non-randomized studies. A final table was constructed summarizing the available evidence.
A total of 120 articles were identified and screened, of which 6 articles were included for final review. Nonunion in children is extremely rare; among the studies included, there were 2011 nonunions among 238822 fractures (0.84%). None of the included studies documented an increased risk of nonunion or delayed bone healing in those children who are treated with NSAIDs in the immediate post-injury or peri-operative time period. Additionally, children are likely to take these medications for only a few days after injury or surgery, further decreasing their risk of adverse side-effects.
This systematic review suggests that NSAIDS can be safely prescribed to pediatric orthopaedic patients absent other contraindications without concern for increased risk of fracture non-union or delayed bone healing. Additional prospective studies are needed focusing on higher risk fractures and elective orthopaedic procedures such as osteotomies and spinal fusion.
Additional prospective studies are needed focusing on higher risk fractures and elective orthopaedic procedures such as osteotomies and spinal fusion.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Pediatric Spine Study Group (PSSG); CORTICES; International Perthes Study Group (IPSG); SCFE Longitudinal International Prospective Registry (SLIP); Pediatric Orthopaedic Society of North America (POSNA); American Orthopaedic Association (AOA) Emerging Leaders Program; American Academy for Cerebral Palsy and Developmental Medicine; American Academy of Orthopaedic Surgeons (AAOS); Alpha Omega Alpha Medical Honor Society (AOA).
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cure E, Turkey S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Vuolteenaho K, Moilanen T, Moilanen E. Non-steroidal anti-inflammatory drugs, cyclooxygenase-2 and the bone healing process. Basic Clin Pharmacol Toxicol. 2008;102:10-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Spiro AS, Beil FT, Baranowsky A, Barvencik F, Schilling AF, Nguyen K, Khadem S, Seitz S, Rueger JM, Schinke T, Amling M. BMP-7-induced ectopic bone formation and fracture healing is impaired by systemic NSAID application in C57BL/6-mice. J Orthop Res. 2010;28:785-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Daluiski A, Ramsey KE, Shi Y, Bostrom MP, Nestor BJ, Martin G, Hotchkiss R, Stephan DA. Cyclooxygenase-2 inhibitors in human skeletal fracture healing. Orthopedics. 2006;29:259-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Inal S, Kabay S, Cayci MK, Kuru HI, Altikat S, Akkas G, Deger A. Comparison of the effects of dexketoprofen trometamol, meloxicam and diclofenac sodium on fibular fracture healing, kidney and liver: an experimental rat model. Injury. 2014;45:494-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Janssen MP, Caron MM, van Rietbergen B, Surtel DA, van Rhijn LW, Welting TJ, Emans PJ. Impairment of the chondrogenic phase of endochondral ossification in vivo by inhibition of cyclooxygenase-2. Eur Cell Mater. 2017;34:202-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | O'Connor JP, Capo JT, Tan V, Cottrell JA, Manigrasso MB, Bontempo N, Parsons JR. A comparison of the effects of ibuprofen and rofecoxib on rabbit fibula osteotomy healing. Acta Orthop. 2009;80:597-605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Lu C, Xing Z, Wang X, Mao J, Marcucio RS, Miclau T. Anti-inflammatory treatment increases angiogenesis during early fracture healing. Arch Orthop Trauma Surg. 2012;132:1205-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Ochi H, Hara Y, Asou Y, Harada Y, Nezu Y, Yogo T, Shinomiya K, Tagawa M. Effects of long-term administration of carprofen on healing of a tibial osteotomy in dogs. Am J Vet Res. 2011;72:634-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Bergenstock M, Min W, Simon AM, Sabatino C, O'Connor JP. A comparison between the effects of acetaminophen and celecoxib on bone fracture healing in rats. J Orthop Trauma. 2005;19:717-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 78] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Endo K, Sairyo K, Komatsubara S, Sasa T, Egawa H, Ogawa T, Yonekura D, Murakami R, Yasui N. Cyclooxygenase-2 inhibitor delays fracture healing in rats. Acta Orthop. 2005;76:470-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Bissinger O, Kreutzer K, Götz C, Hapfelmeier A, Pautke C, Vogt S, Wexel G, Wolff KD, Tischer T, Prodinger PM. A biomechanical, micro-computertomographic and histological analysis of the influence of diclofenac and prednisolone on fracture healing in vivo. BMC Musculoskelet Disord. 2016;17:383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Brown KM, Saunders MM, Kirsch T, Donahue HJ, Reid JS. Effect of COX-2-specific inhibition on fracture-healing in the rat femur. J Bone Joint Surg Am. 2004;86:116-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 106] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Utvåg SE, Fuskevåg OM, Shegarfi H, Reikerås O. Short-term treatment with COX-2 inhibitors does not impair fracture healing. J Invest Surg. 2010;23:257-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Hak DJ, Schulz KS, Khoie B, Hazelwood SJ. The effect of Cox-2 specific inhibition on direct fracture healing in the rabbit tibia. J Orthop Sci. 2011;16:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Sevimli R, Uzel M, Sayar H, Kalender AM, Dökmeci O. The effect of dexketoprofen trometamol on the healing of diaphysis fractures of rat tibia. Acta Orthop Traumatol Turc. 2013;47:423-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Jeffcoach DR, Sams VG, Lawson CM, Enderson BL, Smith ST, Kline H, Barlow PB, Wylie DR, Krumenacker LA, McMillen JC, Pyda J, Daley BJ; University of Tennessee Medical Center, Department of Surgery. Nonsteroidal anti-inflammatory drugs' impact on nonunion and infection rates in long-bone fractures. J Trauma Acute Care Surg. 2014;76:779-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 17. | Sagi HC, Jordan CJ, Barei DP, Serrano-Riera R, Steverson B. Indomethacin prophylaxis for heterotopic ossification after acetabular fracture surgery increases the risk for nonunion of the posterior wall. J Orthop Trauma. 2014;28:377-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 18. | Donohue D, Sanders D, Serrano-Riera R, Jordan C, Gaskins R, Sanders R, Sagi HC. Ketorolac Administered in the Recovery Room for Acute Pain Management Does Not Affect Healing Rates of Femoral and Tibial Fractures. J Orthop Trauma. 2016;30:479-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Fader L, Whitaker J, Lopez M, Vivace B, Parra M, Carlson J, Zamora R. Tibia fractures and NSAIDs. Does it make a difference? Injury. 2018;49:2290-2294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | Dodwell ER, Latorre JG, Parisini E, Zwettler E, Chandra D, Mulpuri K, Snyder B. NSAID exposure and risk of nonunion: a meta-analysis of case-control and cohort studies. Calcif Tissue Int. 2010;87:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 141] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 21. | Bhandari M, Fong K, Sprague S, Williams D, Petrisor B. Variability in the definition and perceived causes of delayed unions and nonunions: a cross-sectional, multinational survey of orthopaedic surgeons. J Bone Joint Surg Am. 2012;94:e1091-e1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 113] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 22. | Mills LA, Simpson AH. The risk of non-union per fracture in children. J Child Orthop. 2013;7:317-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Ekegren CL, Edwards ER, de Steiger R, Gabbe BJ. Incidence, Costs and Predictors of Non-Union, Delayed Union and Mal-Union Following Long Bone Fracture. Int J Environ Res Public Health. 2018;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 192] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 24. | Schmal H, Brix M, Bue M, Ekman A, Ferreira N, Gottlieb H, Kold S, Taylor A, Toft Tengberg P, Ban I; Danish Orthopaedic Trauma Society. Nonunion - consensus from the 4th annual meeting of the Danish Orthopaedic Trauma Society. EFORT Open Rev. 2020;5:46-57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 25. | Lindaman LM. Bone healing in children. Clin Podiatr Med Surg. 2001;18:97-108. [PubMed] |
| 26. | Poonai N, Datoo N, Ali S, Cashin M, Drendel AL, Zhu R, Lepore N, Greff M, Rieder M, Bartley D. Oral morphine versus ibuprofen administered at home for postoperative orthopedic pain in children: a randomized controlled trial. CMAJ. 2017;189:E1252-E1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 27. | Koller DM, Myers AB, Lorenz D, Godambe SA. Effectiveness of oxycodone, ibuprofen, or the combination in the initial management of orthopedic injury-related pain in children. Pediatr Emerg Care. 2007;23:627-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Neri E, Maestro A, Minen F, Montico M, Ronfani L, Zanon D, Favret A, Messi G, Barbi E. Sublingual ketorolac versus sublingual tramadol for moderate to severe post-traumatic bone pain in children: a double-blind, randomised, controlled trial. Arch Dis Child. 2013;98:721-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 29. | Friday JH, Kanegaye JT, McCaslin I, Zheng A, Harley JR. Ibuprofen provides analgesia equivalent to acetaminophen-codeine in the treatment of acute pain in children with extremity injuries: a randomized clinical trial. Acad Emerg Med. 2009;16:711-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 30. | Zura R, Kaste SC, Heffernan MJ, Accousti WK, Gargiulo D, Wang Z, Steen RG. Risk factors for nonunion of bone fracture in pediatric patients: An inception cohort study of 237,033 fractures. Medicine (Baltimore). 2018;97:e11691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 31. | Kay RM, Directo MP, Leathers M, Myung K, Skaggs DL. Complications of ketorolac use in children undergoing operative fracture care. J Pediatr Orthop. 2010;30:655-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 32. | Kay RM, Leathers M, Directo MP, Myung K, Skaggs DL. Perioperative ketorolac use in children undergoing lower extremity osteotomies. J Pediatr Orthop. 2011;31:783-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | DePeter KC, Blumberg SM, Dienstag Becker S, Meltzer JA. Does the Use of Ibuprofen in Children with Extremity Fractures Increase their Risk for Bone Healing Complications? J Emerg Med. 2017;52:426-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 34. | Drendel AL, Gorelick MH, Weisman SJ, Lyon R, Brousseau DC, Kim MK. A randomized clinical trial of ibuprofen versus acetaminophen with codeine for acute pediatric arm fracture pain. Ann Emerg Med. 2009;54:553-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 35. | Nuelle JAV, Coe KM, Oliver HA, Cook JL, Hoernschemeyer DG, Gupta SK. Effect of NSAID Use on Bone Healing in Pediatric Fractures: A Preliminary, Prospective, Randomized, Blinded Study. J Pediatr Orthop. 2020;40:e683-e689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 36. | Rajput K, Vadivelu N. Acute Pain Management of Chronic Pain Patients in Ambulatory Surgery Centers. Curr Pain Headache Rep. 2021;25:1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |