Published online Mar 18, 2020. doi: 10.5312/wjo.v11.i3.167
Peer-review started: November 11, 2019
First decision: November 22, 2019
Revised: December 2, 2019
Accepted: March 1, 2020
Article in press: March 1, 2020
Published online: March 18, 2020
Processing time: 126 Days and 18.4 Hours
The uncemented ArcosTM Modular Femoral Revision System (ARCOS) is a new comprehensive, press-fit revision design. The modular design offers a wide range of possible combinations to accommodate different variations of anatomy and bone stock. The ARCOS is made by a proximal body and a distal stem. As probably the only ones worldwide we predominantly use a combination of body and stem which supports proximal fixation and load, since this mimics the concept of the primary total hip arthroplasty with proximal weight-bearing, leading to bone stock preservation and no stress shielding or thigh pain.
To evaluate the early results after femoral revision in a consecutive series of patients undergoing surgery over 3 years.
We included 116 patients in the study. They were operated in the period August 2011 to December 2014 and we got a clinical mean observation time of 4 (0.5-6) years. Clinical and radiographical follow-up included present function of the hip assessed by Harris Hip Score, Oxford Hip Score, and EQ5D (measure of health outcome). Of the 116 patients, 17 died in the interim and were consequently included only in the implant survivorship analysis; 46 patients attended the follow-up control.
In total 6 (5%) hips were re-revised due to infection (n = 3), fracture (n = 2) or subsidence (n = 1). No patient was re-revised due to aseptic loosening. The 1-, 2- and 5-year probability of implant survival (95%CI) were 97% (93%-100%), 97% (93%-100%) and 96% (92%-99%), respectively. In this cohort 95 patients received a combination of a proximal broach and a distal curved and slotted stem (BS), aiming for proximal fixation and load bearing; 21 patients received a different combination. When comparing these two groups the BS-group had a 5-year implant survival probability (95%CI) of 97% (93%-100%) compared with the group of other combinations with a 5-year implant survival probability (95%CI) of 90% (78%-100%) (P = 0.3). Our regression analysis showed that periprosthetic fracture as an indication for the ARCOS operation was the only significant negative outcome predictor. The mean Harris Hip Score result (100 points being best) was 83 (range 5-98). The mean Oxford Hip Score result (48 points being best) was 40 (range 19-48).
The early results of the ARCOS are promising compared with similar studies. We encourage the use of the BS combination whenever the bone stock proximally is adequate.
Core tip: The ArcosTM Modular Femoral Revision System is a new comprehensive, press-fit revision design. We have evaluated the early results after femoral revision in a consecutive series of 116 patients in a period of three years. This is a fairly large cohort when dealing with arthroplasty reoperations and the special feature of our cohort is that we use a combination of implant-modules which strives for proximal load bearing and fixation, mimicking the concept of the primary hip replacements.
- Citation: Dyreborg K, Petersen MM, Balle SS, Kjersgaard AG, Solgaard S. Observational study of a new modular femoral revision system. World J Orthop 2020; 11(3): 167-176
- URL: https://www.wjgnet.com/2218-5836/full/v11/i3/167.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i3.167
In 2011 we began using the new Arcos Modular Femoral Revision System (ARCOS) for hip revision surgery (Zimmer Biomet Inc., Warsaw, Indiana, USA). This was part of a development over some years, going from using monoblock prostheses to using modular prostheses. The uncemented modular prosthesis is now worldwide the most common choice in hip revision surgery[1,2].
The idea behind the modular implants compared to the one-piece implants, is to provide flexibility to adjust leg length and apply the optimal rotation to address stability during surgery. In addition, both metaphyseal and diaphyseal defects may be addressed independently[3,4]. It is essential to evaluate the efficacy of new technology or new designs[5] . With this study we aimed to evaluate the early results after surgery with ARCOS, focusing on early reoperation rate and clinical results.
In this retrospective observational study with clinical and radiographical follow-up, we included 116 consecutive patients who were operated on any indication with the ARCOS at Herlev-Gentofte Hospital, Denmark, department of Orthopaedic Surgery by two chief surgeons per operation. The first patient was operated on August 30, 2011 and the last on December 17, 2014. All study participants or their legal guardian provided informed written consent about personal and medical data collection prior to study enrolment. The Danish Patient Safety Authority granted access to patient files for those patients whom we were unable to contact (case number 3-3013-1695/1/).
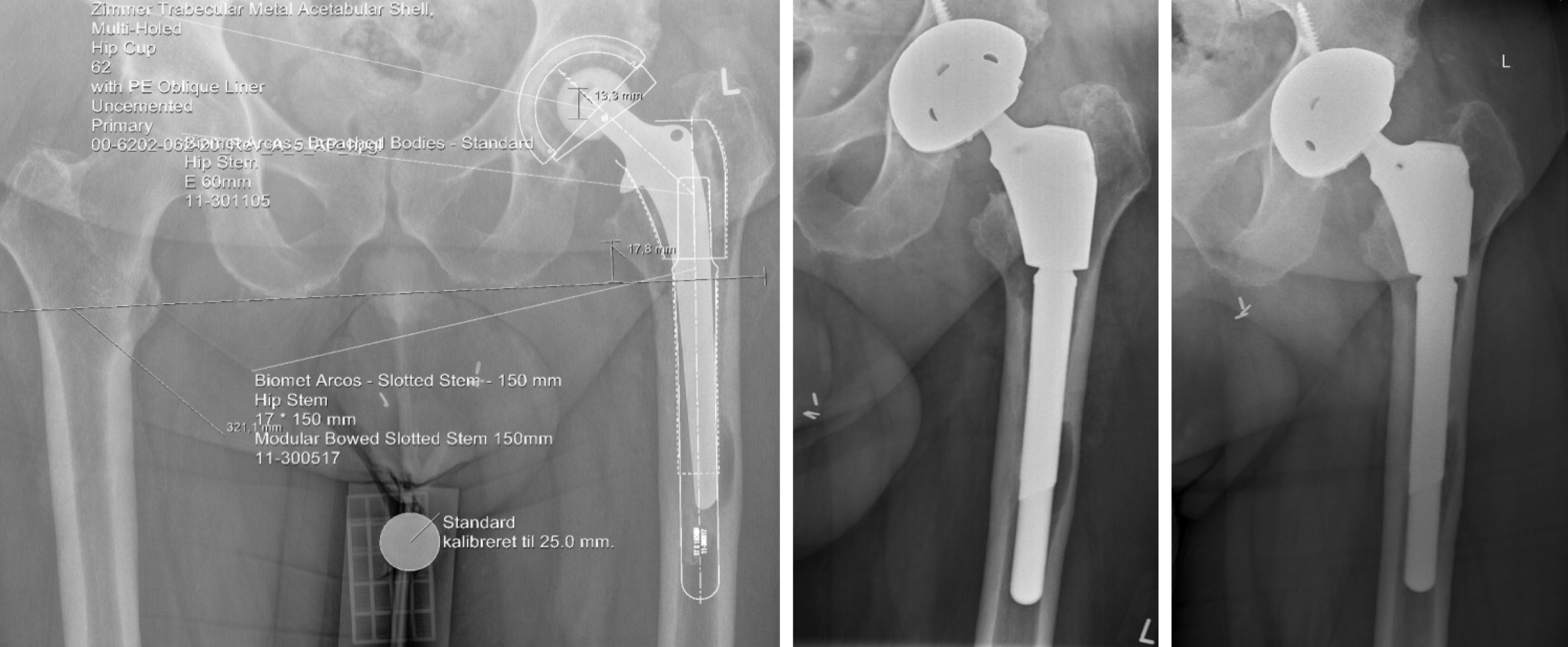
The acetabular cup was replaced only if it was loose, or in cases of polywear. The revision implant was an uncemented cup with a surface of trabecular metal with a poly liner. Accordingly, all patients had a metal-on-poly bearing. The ARCOS is a wide-ranging, press-fit revision stem design providing the surgeon with multiple styles of modular proximal and distal bodies for reconstruction of various defects commonly seen in femoral revision surgery. That being the case, the ARCOS is formed by a proximal body and a distal stem (Figure 1). The proximal bodies are broach, calcar-replacing or cone-style implants. All proximal bodies are made from Ti-6Al-4V (ASTM F-136 or F-620). The proximal implants are offered in a range of sizes with standard and high offset neck geometries.
The distal stems consist of slotted, bullet-tip and splined tapered stem (STS) versions made to address differing quality of diaphyseal bone, desired fixation and surgical technique. The distal stems are also made from Ti-6Al-4V (ASTM F-136) in a range of diameters and lengths. All proximal bodies and distal stems are available without Bonemaster hydroxyapatite coating for use in the United States and with Bonemaster hydroxyapatite coating for use in Europe. The ARCOS with Bonemaster coating was used in this study.
In theory, more than 200 combinations of proximal body and distal stem exist. In reality two combinations or concepts apply for the majority of revision cases. These are: (1) A broach proximal body + a distal slotted and curved stem (BS) and (2) A cone proximal body + a distal STS (CS).
The BS combination strives for instant load and fixation proximally. A good fit can be achieved and in time ingrowth distally around the cylindrical and anatomically curved stem will occur. The modules are assembled on the operating table.
On the other hand, the CS combination aims for immediate distal fixation around the conical stem with the possibility of adjustment after stem placement since the cone body comes in three different lengths and is fitted in situ after placement of the distal stem. No proximal fixation or weight bearing is accomplished.
The choice of implant combination was solely decided by the surgeon. Both combinations include the possibility of restoring off-set and leg length. However, in the opinion of the authors the BS combination has the resemblance of a primary implant, thus favouring its use.
Preoperatively templating on calibrated X-rays was made on the entire cohort, optimizing the end result of the operation, regarding the biomechanical parameters such as leg length and offset (Figure 2). This is especially important when aiming for preservation of bone stock with the BS combination, since it is assembled prior to insertion.
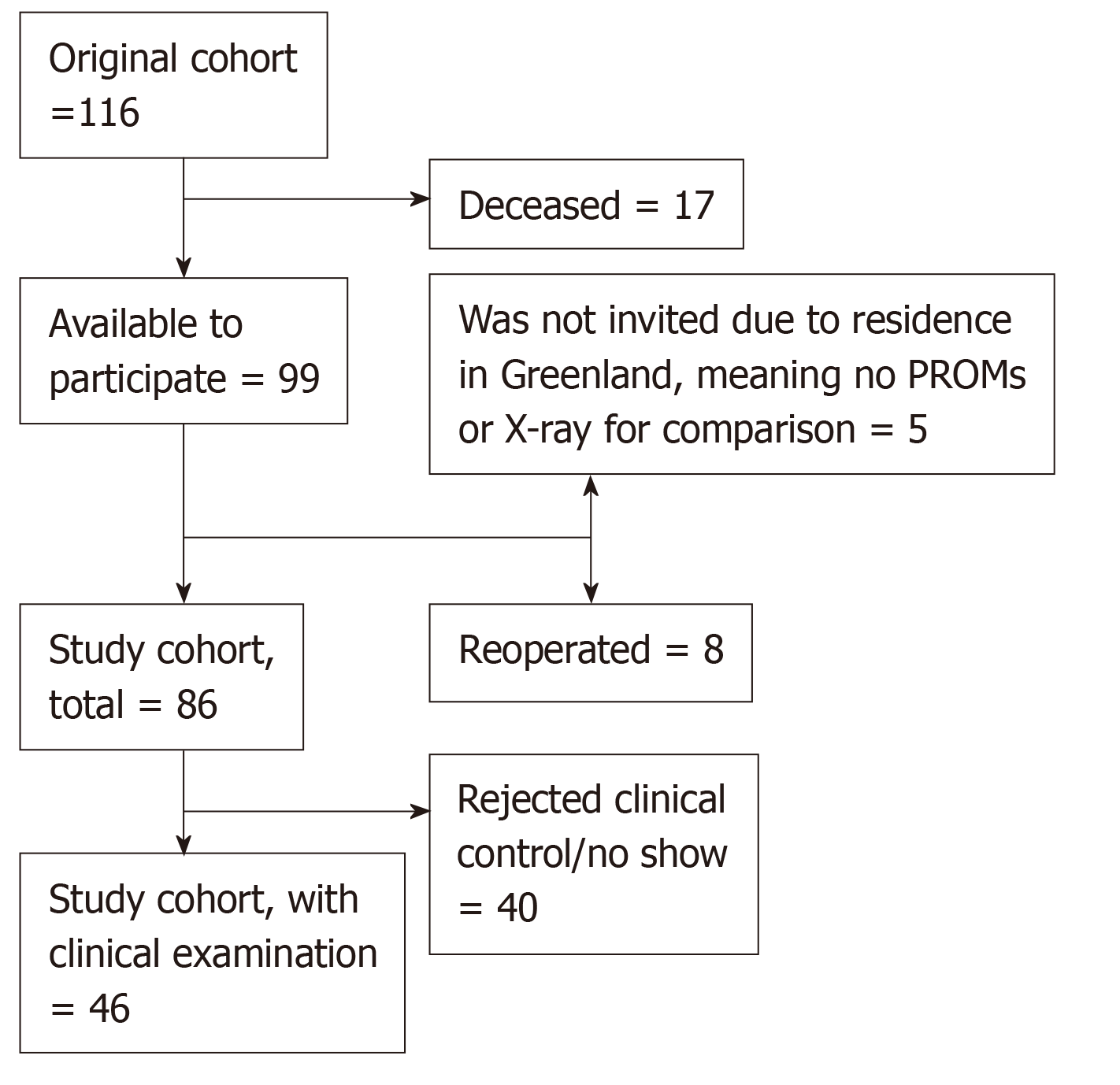
Six experienced hip-surgeons in the department performed 123 consecutive total hip arthroplasty revisions with the ARCOS in the period August 2011 to December 2014; 6 patients were operated twice on the same side (they appear in the study just once with their first ARCOS-operation). Hence, 116 individuals were suitable for enrolment. These patients were invited to participate in the study according to the inclusion criteria (Figure 3). The mean observation time was 4 (0.5-6) years. The only reason for follow up shorter than 2 years was death.
The follow-up took place at Herlev-Gentofte Hospital and included evaluation by Harris Hip Score (HHS) (objective), Oxford Hip Score (OHS) and EQ-5D (the two latter are Patient Reported Outcome Measures)[6,7]. The HHS has a maximum score of 100 points (as the best possible outcome) covering pain (1 item, 0–44 points), function (7 items, 0–47 points), absence of deformity (1 item, 4 points), and range of motion (2 items, 5 points). The OHS is an outcome measure to assess pain, functional ability and daily activities. It produces overall scores running from 0 to 48, with 48 being the best outcome possible[6,8]. The EQ-5D consists of 2 parts, the first called Dimensions, covering Mobility, Self-care, Usual activities, Pain/discomfort, and Anxiety/depression. The second part is the EQ-5D VAS-score, an overall self-assessment of wellbeing scoring from 0 to 100 (100 being the best possible). Only the VAS-score is reported in this article. All the radiographic X-rays were jointly evaluated by the same orthopedic surgeon and radiologist. Compared to the post-surgery X-rays in two planes, the most recent anterior-posterior X-ray was classified as: Stationary conditions, subsidence, fracture, re-revision or clearing in the Gruen Zones.
The following factors were recorded from the electronic journal system: Age, gender, alive/dead, American Society of Anaesthesiologists’ score (ASA), year of primary total hip arthroplasty, revision number, cause for revision, cemented/uncemented status to be revised, stem to be revised, date of ARCOS surgery, operation-code, proximal body (ARCOS), distal stem (ARCOS), complications during surgery, complications during admission, reoperation of ARCOS (only femur stem, not the cup), date of ARCOS-reoperation.
From the Danish Hip Arthroplasty Registry: Information on bone stock classification[9-11] during surgery, revision number, cause for revision, cemented/uncemented status to be revised, stem to be revised, date of ARCOS surgery and operation-code were obtained. The Impax Client (Agfa) was used for: Date of X-ray post-surgery, date of the most recent X-ray, analysis of both the post-surgery and the most recent X-ray.
All patients who underwent surgery in the given period were asked to participate in the follow-up study; 40 patients declined participation in clinical and radiographical follow-up due to e.g., old age, poor function or simply “no time” or “not interested” (see flow chart Figure 3). Of course this meant some level of selection bias, but only with regards to clinical follow-up, not the survival analysis.
Non-parametric statistics were used for risk factors between the re-revision-group and the no-re-revision-group. Competing risk and Kaplan Meier survival analysis were used for the ARCOS stem combination(s). For preoperative factors a multivariate cox method was used to estimate stem failure (cause for revision + ASA + gender + age + revision number + bone stock classification + ARCOS combination). A statistical review of the study was performed by a professor with extensive experience in statistics.
The baseline demographics and the clinical findings are shown in Table 1. Patients were equally distributed between genders, and a normal distribution was seen in age, ASA and bone stock classification. All patients in this study were in ASA group 1-3. The cause for revision was aseptic loosening for the majority of cases. Of the 14 patients with infection, 4 received a two-stage operation.
| Count (valid percent) | Mean (range) | |
| Sex | ||
| Male | 57 (49) | |
| Female | 59 (51) | |
| Age at operation (yr) | 73 (39-95) | |
| ASA | ||
| 1 | 21 (20) | |
| 2 | 54 (51) | |
| 3 | 31 (30) | |
| 4 and 5 | 0 | |
| Missing data | 10 | |
| Cause for revision | ||
| Aseptic loosening | 80 (69) | |
| Periprosthetic fracture | 17 (15) | |
| Infection | 14 (12) | |
| Other | 5 (4) | |
| Missing data | 2 | |
| Revised stem | ||
| BiMetric | 38 (32) | |
| Spotorno | 20 (17) | |
| Lubinus | 22 (19) | |
| Spectron | 7 (6) | |
| Corail | 6 (5) | |
| Taperloc | 2 (2) | |
| Scanhip | 2 (2) | |
| Müller | 4 (3) | |
| Girdlestone | 4 (3) | |
| Osteostynthesis | 3 (3) | |
| Other | 7 (6) | |
| Missing data | 1 | |
| Cemented | 72 (62) | |
| Not cemented | 44 (38) |
The stems being removed were largely BiMetric, Spotorno and Lubinus, an expression of which stems had been used most in the previous years. Perioperatively the bone stock was classified according to Saleh et al[9,10] and we found 48% with type II, 34% with type I, 14% with type III and 2% with type IV and V respectively. Our regression analysis (Table 2) showed that periprosthetic fracture as an indication for the ARCOS operation was the only significant negative outcome predictor.
| Hazard Ratio | 95%CI | P value | ||
| Cause for revision | Aseptic loosening (n = 80) | 1.00 | (1.00, 1.00) | 1.000 |
| Infection (n = 14) | 3.02 | (0.01, 1108.00) | 0.713 | |
| Fracture (n = 17) | 14.22 | (1.07, 189.61) | 0.045 | |
| ASA | 1-2 (n = 75) | 1.00 | (1.00, 1.00) | 1.000 |
| 3 (n = 31) | 1.33 | (0.08, 23.26) | 0.846 | |
| Gender | Male (n = 55) | 1.00 | (1.00, 1.00) | 1.000 |
| Female (n = 61) | 2.64 | (0.26, 26.48) | 0.410 | |
| Age group | < 73 (n = 64) | 1.00 | (1.00, 1.00) | 1.000 |
| ≥ 73 (n = 52) | 0.44 | (0.04, 4.50) | 0.485 | |
| Revision | No revisions (n = 2) | 1.00 | (1.00,1.00) | 1.000 |
| First revision (n = 86) | 11.00 | (0.04, 2902.06) | 0.399 | |
| Bone stock quality | 1 + 2 (n = 95) | 1.00 | (1.00, 1.00) | 1.000 |
| 3-5 (n = 20) | 2.23 | (0.25, 19.51) | 0.470 | |
| Arcos stem | Other combinations (n = 21) | 1.00 | (1.00, 1.00) | 1.000 |
| Broach + Slotted (n = 95) | 0.11 | (0.01, 1.42) | 0.091 | |
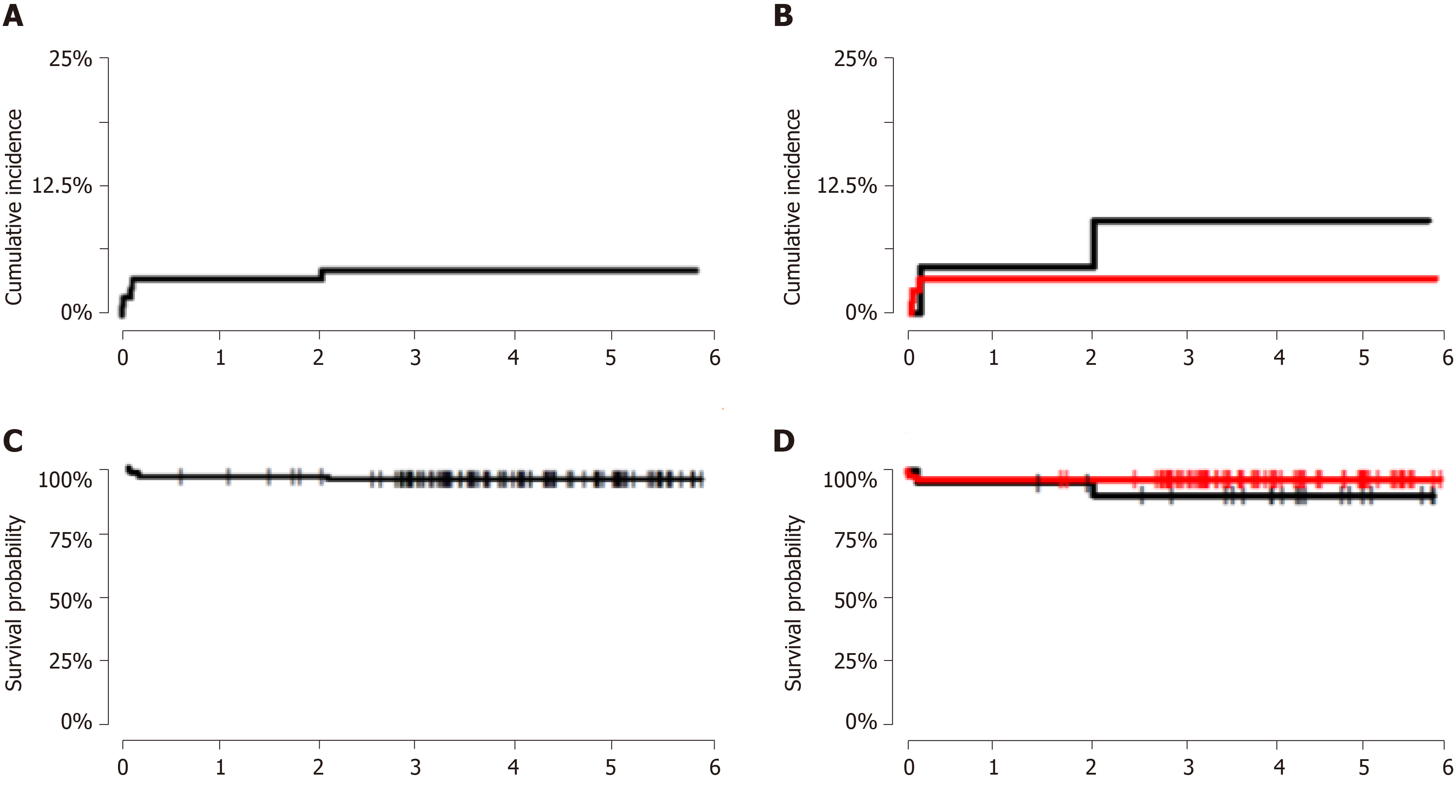
The overall 1-, 2- and 5-year probability of implant survival estimated using Kaplan Meier and competing risk analysis (with 95%CI) were 97% (93%-100%), 97% (93%-100%) and 96% (92%-99%), respectively (Figure 4). The BS combination was used in 95 patients. When we compared the re-revision risk for this group to the 21 patients with other combinations, we got a 1-, 2- and 5-year probability as seen in Figure 3. The “other combinations” were CS = 9, Calcar + Slotted = 11 and Cone + ETO = 1.
The index operation for BS was in 61 cases due to aseptic loosening, in 16 cases due to periprosthetic fracture, in 14 due to infection, in 1 due to subsidence and in 2 because of a broken stem. For the CS combination 8 patients had aseptic loosening, 1 had a periprosthetic fracture and finally, there was a single case of a broken stem as cause for index operation (and one missing value). The Calcar+Slotted combination was used in 10 cases operated due to aseptic loosening and in 1 case because of a broken stem. The Cone + ETO combination was used just once on the indication of aseptic loosening.
At the clinical evaluation at follow up (n = 46) we found that the mean EQ-5D VAS result (100 being best) was 72 (range 20-100). The mean HHS result (100 being best) was 83 (range 5-98). The mean OHS result (48 being best) was 40 (range 19-48). At the radiographical evaluation we found 84 hips with stationary conditions, 6 were re-revised, 2 had a cup-revision, 16 had some subclinical subsidence or clearing, 2 had a healed fracture and 6 patients had no X-rays for comparison (5 because of residence in Greenland, 1 due to unknown causes).
Our study describes short-term results and the primary outcome parameter being evaluated is the failure rate. We find a survival of 96% in total after 5 years very satisfying. In other early to midterm studies of cementless modular femoral revision systems, survival of the prosthesis is reported to be 76%-97% (observation time 4-7 years)[12-16], leaving the ARCOS in the upper end of this interval. The important preliminary message is clear; the stem is functioning well and has the character of a so-called "safe procedure". The strengths of this study are that it is the first consecutive record of this widely used prosthesis and provides early results of a new product, which is very important to obtain for research and development purposes. With the present study we have included a large cohort of the BS combination and we find the concept is performing well. This is interesting since the tendency worldwide is to use the concept of distal fixation (i.e., the CS combination). The BS concept relies on both proximal and distal fixation, using a curved design for better fit, avoiding stress shielding and thigh pain[17,18]. According to Wolff’s law, bone responds to any changes in mechanical conditions by remodelling and thus changing density and structure[19-21], through what is known as adaptive remodelling. If no mechanical load is present, bone will become weaker and the risk of fracture will increase. With the use of the broach body design, we attempt to create a situation with a proximal load like the concept of the primary implants. Furthermore, we find that the versatility of the ARCOS implants also makes it possible to address a situation with extreme proximal bone loss by using the CS combination to obtain rigid distal fixation.
The limitations of the present investigation are the retrospective design, the short follow-up and that no randomization has been done. On the other hand, the fact that the surgeons – two at a time – had the sole right to decide what they found to be the best solution for the individual patient, may not have been disadvantageous. Unfortunately, we did not have preoperative HHS, OHS and EQ-5D scores and 40 patients declined participation in the clinical and X-ray follow-up. However, only six patients had no X-rays to compare with at all. Looking at the clinical follow-up we find these results generally satisfying although the many who did not attend must be considered. There were three patients we considered as outliers with very low scores in all three categories. They all had their revision with ARCOS done due to infection and had complications with chronic pain or poor function in the subsequent time. Two of these patients were more than 85 years of age and suffered from competing disorders.
When it comes to the risk factors and evaluation of factors influencing stem failure it is extremely difficult to compare different revision concepts. Many factors affect the outcome, resulting in very small patient groups. Periprosthetic fracture is associated with complications and was the only significant negative prognostic factor in our study. We did not find infection to be a significant risk factor, even though the three worst clinical outcome scores came from patients with an infection. This has also been reported in earlier studies[22,23]. Another important variable is bone loss[24]. In the present study we could not prove a correlation between bone loss and risk of re-revision. The degree and location of the bone loss is important for the choice of revision concept. We have attempted to use the BS concept in patients with bone loss below the metaphysis, and our analysis showed that this has been a satisfying strategy. Although not statistically significant, there was a tendency towards better survival rates when using the BS concept.
Most orthopedic surgeons advocate using the STS concept, often in combination with extended trochanteric osteotomy (ETO). ETO was seldom used in this study; removal of cement was performed from “the top” to avoid damaging the integrity of the femoral canal. We therefore recommend a differentiated use of the various concepts depending on the individual bone quality and bone stock.
The generalisability of this study is considered low-to-medium since it is an observational study with e.g., no randomization or blinding, including only a selected population with a specific need for surgery for various reasons. Nonetheless this will most often be the premise for studies concerning revision implants.
In conclusion: The early results show satisfying durability for the ArcosTM Modular Femoral Revision System in its entirety. We encourage surgeons to consider using the BS combination for proximal load and fixation for better preservation of bone stock, less stress shielding and less thigh pain in order to obtain a situation as close to a cementless primary total hip as possible.
The uncemented ArcosTM Modular Femoral Revision System (ARCOS) is a new comprehensive, press-fit revision design. The modular design offers a wide range of possible combinations to accommodate different variations of anatomy and bone stock. The ARCOS is made by a proximal body and a distal stem. As probably the only ones worldwide we predominantly use a combination of body and stem which supports proximal fixation and load, since this mimics the concept of the primary total hip arthroplasty with proximal weight-bearing, leading to bone stock preservation and no stress shielding or thigh pain.
With this study we wanted to evaluate the early results after femoral revision with the new ARCOS in a consecutive series of patients who underwent surgery over a period of 3 years. We also found it very interesting to find out whether a specific ARCOS combination is performing superiorly compared to the most widely used to date.
In the 1990’s Denmark, we had a scare scenario with bone cement not tested on humans before clinical implementation. It became an arthroplasty-scandal and led to financial compensation to thousands of patients. We became fearfully aware how essential it is to evaluate the efficacy of new technology or new design. With this study we aimed to evaluate the early results after surgery with ARCOS, focusing on reoperation rate and clinical results.
In this retrospective observational study with clinical and radiographical follow-up, we included 116 patients. They were operated in the period August 2011 to December 2014 and we got a clinical mean observation time of 4 (0.5-6) years. The only reason for follow up shorter than 2 years was death.
Clinical and radiographical follow-up included present function of the hip assessed by Harris Hip Score, Oxford Hip Score, and EQ5D (measure of health outcome). Compared to the post-surgery X-rays in two planes, the most recent anterior-posterior X-ray was classified as: Stationary conditions, subsidence, fracture, re-revision or clearing in the Gruen Zones.
Of the 116 patients, 17 died in the interim and were consequently included only in the implant survivorship analysis; 46 patients attended the follow-up control. Statistics: Non-parametric statistics was used for risk factors between the re-revision-group and the no-re-revision-group. Competing risk and Kaplan Meier survival analysis were used for the ARCOS stem combination(s). For preoperative factors multivariate cox method was used to estimate stem failure.
In total 6 (5%) hips were re-revised due to infection (n = 3), fracture (n = 2) or subsidence (n = 1). No patient was re-revised due to aseptic loosening. The 1-, 2- and 5-year probability of implant survival (95%CI) was 97% (93%-100%), 97% (93%-100%) and 96% (92%-99%) respectively. I this cohort 95 patients received a combination of a proximal broach and a distal curved and slotted stem (BS), aiming for proximal fixation and load bearing; 21 patients received a different combination. When comparing these two groups the BS-group had a 5-year implant survival probability (95%CI) of 97% (93%-100%) compared with the group of other combinations with a 5-year implant survival probability (95%CI) of 90% (78%-100%) (P = 0.3).
Our regression analysis showed that periprosthetic fracture as an indication for the ARCOS operation was the only significant negative outcome predictor. The mean Harris Hip Score result (100 being best) was 83 (range 5-98). The mean Oxford Hip Score result (48 being best) was 40 (range 19-48).
Perioperatively the bone stock was classified according to Saleh et al and we found 48% with type II, 34% with type I, 14% with type III and 2% with type IV and V respectively. At the radiographical evaluation we found 84 hips with stationary conditions, 6 were re-revised, 2 had a cup-revision, 16 had some subclinical subsidence or clearing, 2 had a healed fracture and 6 patients had no X-rays for comparison.
Our study describes short-term results and the primary outcome parameter being evaluated is the failure rate. Our findings support the hypothesis that an ARCOS combination with proximal load-bearing and fixation reduces the reoperation rate. Of course it is interesting to further investigate how the long-term outcome with these prostheses is, especially since the tendency worldwide is to use the concept of distal fixation.
We find survival of the ARCOS prosthesis of 96% in total after 5 years very satisfying. We encourage surgeons to consider using the combination for proximal load and fixation for better preservation of bone stock, less stress shielding and less thigh pain in order to obtain a situation as close to a primary total hip as possible. It is essential to evaluate the efficacy of new technology or new designs. The ARCOS stem is functioning well and has the character of a so-called “safe procedure”. Proximal fixation and load-bearing is desirable in both primary total hip arthroplasty and in revision total hip arthroplasty to reduce the incidence of stress shielding and thigh pain, and preserve bone stock.
The ARCOS is an uncemented stem design for revision hip arthroplasty. It is combined by a proximal body and a distal stem and in theory more than 200 combinations of proximal body and distal stem exist. In reality two combinations or concepts apply for the majority of revision cases. These are: (1) A broach proximal body + a distal slotted and curved stem (proximal load and fixation) and (2) A cone proximal body + a distal STS (distal load and fixation). The ARCOS is performing above acceptable. We recommend a differentiated use of the various concepts depending on the individual bone quality and bone stock.
We ask surgeons to consider using the ARCOS combination for proximal load and fixation that mimics the primary total hip arthroplasty whenever bone stock is adequate. We are currently investigating how other ARCOS-populations in other hospitals are doing and what combinations of proximal body and distal stem they have received. A randomized controlled trial would be lovely, and it might be possible with a multicenter study setup.
The authors would like to send special thanks to consultant in orthopedic surgery Jens B Retpen and to MD Elisabeth Waagensen for their indispensable contributions to this work.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Denmark
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Castagnini F, Papachristou G S-Editor: Wang J L-Editor: A E-Editor: Xing YX
| 1. | Overgaard S, Pedersen AB, Hjelm AH. National Annual Report 2016. Danish Hip Arthroplasty Register, 2016. |
| 2. | Duwelius PJ, Hartzband MA, Burkhart R, Carnahan C, Blair S, Wu Y, Grunkemeier GL. Clinical results of a modular neck hip system: hitting the "bull's-eye" more accurately. Am J Orthop (Belle Mead NJ). 2010;39:2-6. [PubMed] |
| 3. | Weiss RJ, Beckman MO, Enocson A, Schmalholz A, Stark A. Minimum 5-year follow-up of a cementless, modular, tapered stem in hip revision arthroplasty. J Arthroplasty. 2011;26:16-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 4. | Harkess JW. Cambell’s Operative Orthopaedics. In: Canale ST, editor. 1. 10th ed. United States: Mosby 2003; 315-471. |
| 5. | Nelissen RG, Pijls BG, Kärrholm J, Malchau H, Nieuwenhuijse MJ, Valstar ER. RSA and registries: the quest for phased introduction of new implants. J Bone Joint Surg Am. 2011;93 Suppl 3:62-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 123] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 6. | Paulsen A, Odgaard A, Overgaard S. Translation, cross-cultural adaptation and validation of the Danish version of the Oxford hip score: Assessed against generic and disease-specific questionnaires. Bone Joint Res. 2012;1:225-233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Sørensen J, Davidsen M, Gudex C, Pedersen KM, Brønnum-Hansen H. Danish EQ-5D population norms. Scand J Public Health. 2009;37:467-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 207] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 8. | Beard DJ, Harris K, Dawson J, Doll H, Murray DW, Carr AJ, Price AJ. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol. 2015;68:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 338] [Cited by in RCA: 372] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 9. | Gozzard C, Blom AW, Taylor A. A comparison of the reliability and validity of bone stock loss classification systems used for revision hip surgery. J Arthroplasty. 2003;18:638–642. [RCA] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Saleh KJ, Holtzman J, Gafni A, Saleh L, Davis A, Resig S, Gross AE. Reliability and intraoperative validity of preoperative assessment of standardized plain radiographs in predicting bone loss at revision hip surgery. J Bone Joint Surg Am. 2001;83:1040-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 76] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Parry MC, Whitehouse MR, Mehendale SA, Smith LK, Webb JC, Spencer RF, Blom AW. A comparison of the validity and reliability of established bone stock loss classification systems and the proposal of a novel classification system. Hip Int. 2010;20:50-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Pelt CE, Madsen W, Erickson JA, Gililland JM, Anderson MB, Peters CL. Revision total hip arthroplasty with a modular cementless femoral stem. J Arthroplasty. 2014;29:1803-1807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Amanatullah DF, Howard JL, Siman H, Trousdale RT, Mabry TM, Berry DJ. Revision total hip arthroplasty in patients with extensive proximal femoral bone loss using a fluted tapered modular femoral component. Bone Joint J. 2015;97-B:312-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 14. | Palumbo BT, Morrison KL, Baumgarten AS, Stein MI, Haidukewych GJ, Bernasek TL. Results of revision total hip arthroplasty with modular, titanium-tapered femoral stems in severe proximal metaphyseal and diaphyseal bone loss. J Arthroplasty. 2013;28:690-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Schuh A, Werber S, Holzwarth U, Zeiler G. Cementless modular hip revision arthroplasty using the MRP Titan Revision Stem: outcome of 79 hips after an average of 4 years' follow-up. Arch Orthop Trauma Surg. 2004;124:306-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | McInnis DP, Horne G, Devane PA. Femoral revision with a fluted, tapered, modular stem seventy patients followed for a mean of 3.9 years. J Arthroplasty. 2006;21:372-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 83] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | Huang Y, Zhou Y, Shao H, Gu J, Tang H, Tang Q. What Is the Difference Between Modular and Nonmodular Tapered Fluted Titanium Stems in Revision Total Hip Arthroplasty. J Arthroplasty. 2017;32:3108-3113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Inaba Y, Kobayashi N, Oba M, Ike H, Kubota S, Saito T. Difference in Postoperative Periprosthetic Bone Mineral Density Changes Between 3 Major Designs of Uncemented Stems: A 3-Year Follow-Up Study. J Arthroplasty. 2016;31:1836-1841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 19. | Petersen MM. Bone mineral measurements at the knee using dual photon and dual energy X-ray absorptiometry. Methodological evaluation and clinical studies focusing on adaptive bone remodeling following lower extremity fracture, total knee arthroplasty, and partial versus total meniscectomy. Acta Orthop Scand Suppl. 2000;293:1-37. [PubMed] |
| 20. | Wagner H. [Revision prosthesis for the hip joint in severe bone loss]. Orthopade. 1987;16:295-300. [PubMed] |
| 21. | Nickelsen TN, Erenbjerg M, Retpen JB, Solgaard S. Femoral revision with impaction allografting and an uncemented femoral component. Hip Int. 2008;18:278-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Gundtoft PH, Overgaard S, Schønheyder HC, Møller JK, Kjærsgaard-Andersen P, Pedersen AB. The "true" incidence of surgically treated deep prosthetic joint infection after 32,896 primary total hip arthroplasties: a prospective cohort study. Acta Orthop. 2015;86:326-334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 131] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 23. | Springer BD, Cahue S, Etkin CD, Lewallen DG, McGrory BJ. Infection burden in total hip and knee arthroplasties: an international registry-based perspective. Arthroplast Today. 2017;3:137-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 204] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 24. | Hashem A, Al-Azzawi A, Riyadh H, Mukka S, Sayed-Noor A. Cementless, modular, distally fixed stem in hip revision arthroplasty: a single-center study of 132 consecutive hips. Eur J Orthop Surg Traumatol. 2018;28:45-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |