Published online Apr 18, 2019. doi: 10.5312/wjo.v10.i4.192
Peer-review started: January 4, 2019
First decision: January 29, 2019
Revised: February 15, 2019
Accepted: March 16, 2019
Article in press: March 16, 2019
Published online: April 18, 2019
Processing time: 106 Days and 14.3 Hours
Growing pains is the most common cause of musculoskeletal pain in early childhood and was first described in 1823 by French physician Marcel Duchamp. Although it has been researched extensively, the etiology is still unknown. Several theories have been proposed throughout the years.
Analyze the available scientific literature to provide an update on the latest evidence on the etiology.
According to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, the scientific literature on the etiology of growing pains was systematically reviewed using the following inclusion criteria: studies of any level of evidence reporting clinical or preclinical results and dealing with the etiology of growing pains. The medical electronic databases PubMed and Web of Science were searched by two independent authors on October 20, 2018. The search string used was “(growing pains OR benign nocturnal limb pains OR musculoskeletal pains) AND (etiology OR pathogenesis) AND (pediatrics)”.
A total of 32 articles were included. The etiology of growing pains still remains poorly understood. Many theories have been proposed, but none of them are decisive. A lower pain threshold has been found among patients suffering from growing pains in comparison to healthy controls. Furthermore, evidence suggests an association between growing pains and reduced bone strength in young patients, although this finding still remains controversial. Changes in the vascular perfusion pattern have also been studied. However, the etiology of growing pains does not seem related to a vascular component. The anatomical/mechanical theory has not been supported, but the role of vitamin D deficiency has been investigated many times. Strong recent evidence indicates a genetic susceptibility in the pathogenesis of growing pains. Furthermore, psychological factors also seem to play a strong role in the onset.
The scientific literature about the etiology of growing pains presents heterogeneity and lack of consensus; more studies are needed to understand the genesis of benign musculoskeletal pain syndrome of childhood.
Core tip: Growing pains are benign nocturnal limb pains and the most common cause of musculoskeletal pain in early childhood. Intermittent non-articular pain during the late afternoon or the night with intervals of pain-free days and no objective signs of inflammation are the main clinical features. Despite the etiology of the disease has been widely researched, it is still not fully understood. Lower pain threshold, vascular perfusion changes, anatomical and genetic abnormalities, vitamin D deficiency and psychological factors have been proposed to explain the pathogenesis of growing pain. More studies are needed to understand the complex genesis of the disease.
- Citation: Pavone V, Vescio A, Valenti F, Sapienza M, Sessa G, Testa G. Growing pains: What do we know about etiology? A systematic review. World J Orthop 2019; 10(4): 192-205
- URL: https://www.wjgnet.com/2218-5836/full/v10/i4/192.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i4.192
French physician Marcel Duchamp first described growing pains as a recurrent leg pain syndrome of early childhood[1]. No evidence has linked growing pains with a phase of especially high growth velocity, which has led physicians to coin new terms for this condition, including “benign nocturnal limb pains of childhood” and “recurrent limb pains of childhood”[2]. However, the term “growing pains” still remains the most commonly used since it has the advantage of not implicating any particular disease and also emphasizes childhood as the period when these pains are most common[3]. The range of prevalence is 2.6% to 49.6%[4,5]. Growing pains are defined by specific clinical features, and Peterson reported diagnostic criteria: intermittent pain that usually occurs once or twice per week late in the afternoon or during the night with intervals of pain-free days; non-articular pain mostly located in the shins, calves, thighs, or popliteal fossa and almost always bilateral; and a lack of pain by the next morning with no objective signs of inflammation[6].
Pain attacks might be very variable in terms of duration, frequency, or severity. Diagnosis is purely clinical since it is mainly based on anamnesis and physical examination with no need for laboratory tests[7]. Although the diagnosis of growing pain seems easy, several entities should be excluded, such as injuries, tumors, and infections, which might mimic the features of growing pains[8]. Growing pains is benign and has a tendency to self-limit once the child grows and reaches adolescence[9]. Thus, treatment might be provided through muscle stretching programs for the quadriceps, hamstrings, and triceps surae groups[9], as well as massaging the affected sites or analgesics[10].
Many studies have tried to investigate the etiology of growing pains over the years without being able to understand it completely. Therefore, the etiopathogenetic mechanisms underlying the phenomena still remain poorly understood. The purpose of this systematic review is to analyze the available literature to provide an update on the latest evidence related to the etiology of growing pains.
This systematic review was conducted according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)[11]. The medical electronic databases PubMed and Web of Science were searched by two independent authors (VF and VA) on October 20, 2018. The search string used was “(growing pains OR benign nocturnal limb pains OR musculoskeletal pains) AND (etiology OR pathogenesis) AND (pediatrics)”.
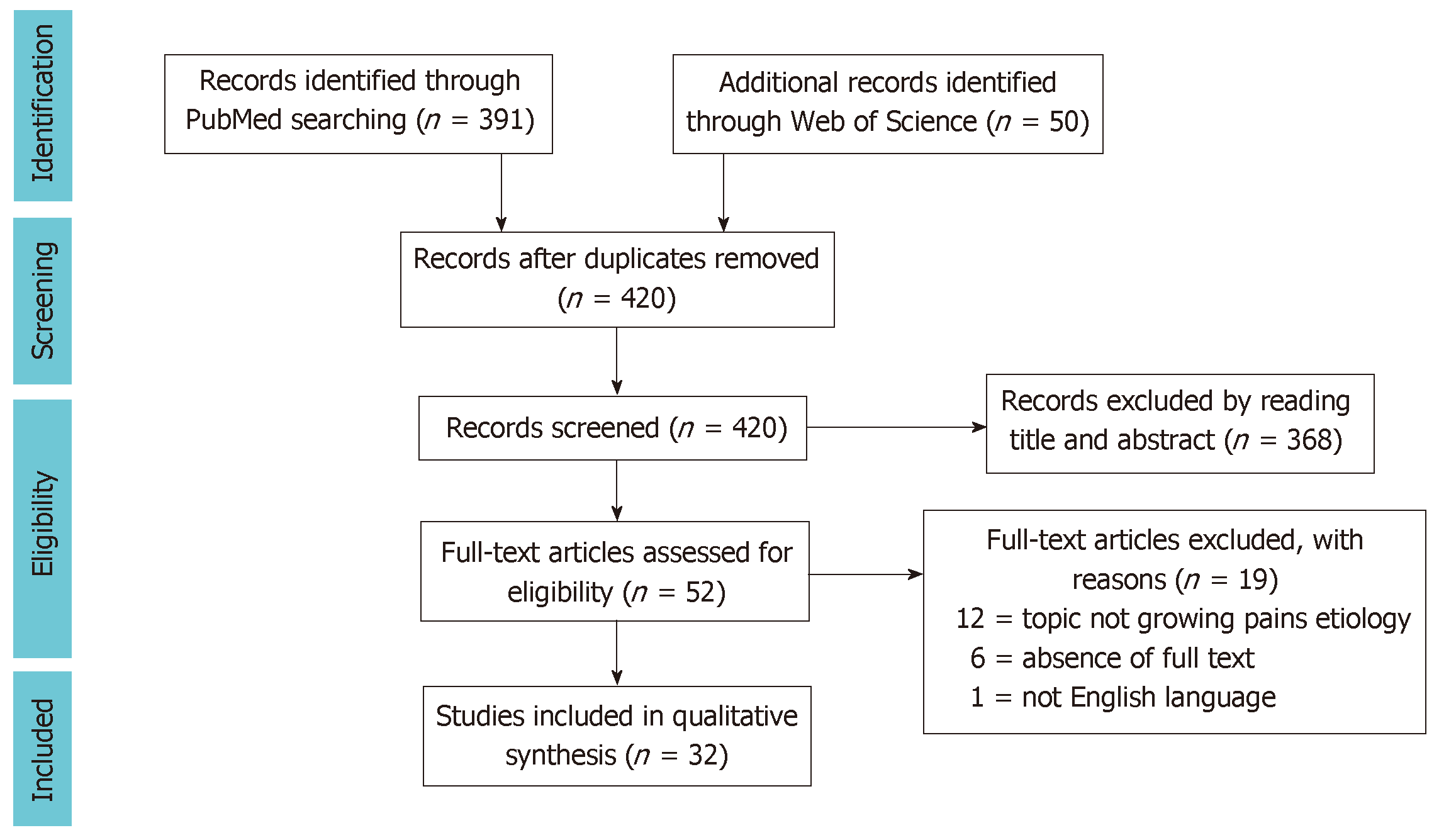
The initial titles and abstracts were screened using the following inclusion criteria: studies of any level of evidence, reporting clinical or preclinical results, and dealing with the etiology of growing pains. The exclusion criteria were articles written in other languages or studies with a strict focus on diagnosis, differential diagnosis, or treatment of growing pains. We also excluded all the remaining duplicates and articles dealing with other topics, poor scientific methodology, or no accessible abstract. Study quality was assessed in duplicate by two independent reviewers (VF and VA), and conflicts about data were resolved by consultation with a senior surgeon (PV). Reference lists from the selected papers were also screened. A PRISMA[11] flowchart of the selection and screening method is provided in Figure 1.
A total of n = 440 articles were found. After excluding duplicates, n = 419 articles were selected. At the end of the first screening, we selected n = 51 articles that were eligible for full text reading. After reading the full text, we ultimately selected n = 32 articles that satisfied the criteria. The included articles[12-43] mainly focus on lower pain threshold, reduced bone strength, changes in vascular perfusion, anatomical factors, vitamin D deficiency, genetic susceptibility, psychological abnormalities, and associations. The main findings of the included articles were summarized (Table 1).
| Ref. | Author | Subjects | Etiology | Results |
| [10] | Pavone et al (2011) | 30 with growing were enrolled and prospectively followed up for 1 yr. Laboratory tests, including complete blood count, erythrocyte sedimentation rate, and serum calcium and phosphorus levels, were performed in all children | Family history | A family history of growing pains was positive in 20% of patients |
| [12] | Hashkes et al (2004) | In 44 children with growing pains and 46 healthy controls, pain thresholds were measured using a Fisher type dolorimeter with pressure applied to areas associated with increased tenderness in fibromyalgia, control points and anterior tibia | Lower pain threshold | Children with growing pains have more tender points and show lower pain thresholds if compared to healthy children. Growing pains might represent a non inflammatory pain syndrome in young children |
| [13] | Uziel et al (2010) | In the 44 previously studied children with growing pains and in 38 healthy controls, current status of growing pains and other pain syndromes were assessed by parental questionnaires. Pain threshold was also measured by using a Fisher-type dolorimeter | Lower pain threshold | The prognosis of growing pains is benign and with a tendency to self limitation. Growing pains might represent a pain amplification syndrome of early childhood |
| [14] | Oster et al (1972) | 635 children were examined annually for five consecutive years or more. Of these, 185 experienced abdominal pain and/or headache for three consecutive years or more while 166 children never had experience of them. Questionnaires were sent to the parents in whom they were ask whether they experienced abdominal pain, headache and/or limb pains in childhood or at the time of investigation | Changes in vascular perfusion | A high prevalence of migraine headaches among children with growing pains have been reported. Recurring abdominal pain, migraine headaches and growing pains are strongly associated and might be part of a reaction pattern based on child’s constitution and domestic environment |
| [15] | Hashkes et al (2005) | 11 patients with growing pains and 12 healthy controls underwent technetium-99 methylene diphosphate bone scans. The uptake in the blood pool phase, static images, and blood pool phase/static image ratio were measured in the right mid-tibia region (painful among patients with growing pains) and right mid-femur (non-painful). Measurements at painful and painless regions among growing pains children were done. Also children with or without growing pains were compared | Changes in vascular perfusion | There were no significant differences between children with growing pains and healthy controls in the blood pool, static images, and blood pool/static images in all localities. There were also no significant differences among painful regions and non-painful regions in children with growing pains. Growing pains are not associated with vascular perfusion changes in painful regions |
| [16] | Kaspiris et al (2016) | The syudy examined 276 children whose data were collected by using a combination of questionnaires, clinical examinations and medical charts of the children and the obstetric history of the mothers. 78 children presenting growing pains met Peterson’s criteria. The tibiofemoral angle and the intermalleolar distance were measured. The perinatal characteristics regarding gestational age, birth weight, length, head circumference, Apgar score, maternal infection, mode of delivery, use of medication and antenatal use of corticosteroids, alcohol or smoking during pregnancy which were based on the medical charts of the children and the maternal obstetrical history were recorded | Genu valgum and perinatal risk factors | Genu valgum severity was a significant factor for growing pains manifestation and increment in frequency and intensity. Perinatal factors including gestational age, Apgar score, head circumference and birth length or weight seemed to be important in growing pains’ onset. Conversely, antenatal corticosteroid treatment, increased maternal age and maternal smoking during pregnancy were not predictive of growing pains. |
| [17] | Kaspiris et al (2007) | The study included 532 children, aged 4 to 12 yr. 130 children presented growth pains. Children which had been breastfed were compared to those which were not | Breastfeeding | There is a statistically significant dependence between the presentation of pains and whether the child had been breastfed or not, as well as the duration of breastfeeding during infancy. However, in children with growing pains, breastfeeding does not affect the type or frequency of pain |
| [18] | Lee et al. (2015) | 20 patients (seven boys, 13 girls), mean age 9.10 ± 2.32 yr, complaining of musculoskeletal pains in the lower extremities treated with custom made foot orthoses | Foot posture | Twenty children completed the study. Seventeen (75%) had overpronated feet. Significant improvements were noted after 1 and 3 mo in pain degree and frequency, and after 3 mo in balancing ability |
| [19] | Evans (2003) | 8 children complaining of aching legs and with pronated foot posture were treated by wearing triplane wedges or orthoses | Foot posture | In-shoe wedges and foot orthoses are effective in the treatment of young children with growing pains and a pronated foot posture. A relationship between foot posture and growing pains is tenuously inferred |
| [20] | Evans and Scutter (2007) | 180 children underwent foot posture measurements including navicular height, navicular drop, resting calcaneal stance position, foot posture index criteria FPI4 calcaneal inversion/eversion, FPI5 talo-navicular region, FPI6 medial longitudinal arch | Foot posture | No meaningful relationship between foot posture or functional health measures and leg pain in young children does exist |
| [21] | Viswanathan and Khubchandani (2008) | The study group consisted of 433 children. Joint hypermobility was assessed by using Beighton criteria Children were considered to have growing pains when fulfilling Petersons criteria | Hypermobility | Joint hypermobility and growing pains in schoolchildren are strongly associated. Joint hypermobility might play a role in the pathogenesis of growing pains |
| [22] | Friedland et al (2005) | In 39 children with growing pains, bone speed of sound was measured by quantitative ultrasound in both mid-tibial and radius bones. Patients’ findings were compared to norms of healthy controls | Reduced bone strenght | Bone speed of sound was significantly reduced in children with growing pains, especially in painful tibial regions. Growing pains might represent a local overuse (stress) syndrome |
| [23] | Uziel et al (2012) | In 39 previously studied children with growing pains, current growing pains status was assessed by parental questionnaires. Bone strength was measured by using quantitative ultrasound. Controls were normograms based on the measurement of bone speed of sound in 1085 healthy children | Reduced bone strenght | Pain improves parallel to the increase in bone strength. Growing pains might represent a local overuse syndrome |
| [24] | Qamar et al (2008) | 100 children with growing pains were investigated for serum total calcium, inorganic phosphorus, alkaline phosphatase, vitamin D3 and parathormone levels. On the basis of serum vitamin D3 level, patients were divided into 3 groups; normal level of vitamin D3, vitamin D insufficiency, vitamin D deficiency | Hypovitaminosis D | Hypovitaminosis D might have a role in pathogenesis of growing pains. Children with unexplained limb pains should be tested for vitamin D status, and treated, if needed |
| [25] | Morandi et al (2005) | In 33 children affected by growing pains pain intensity was evaluated through a questionnaire using the Wong–Baker Faces Pain Rating Scale for pain assessment. Serum 25-OH-D, parathyroid hormone, and alkaline phosphatase levels were also measured. QUS measured both bone density and cortical thickness. After 3 and 24 mo of vitamin D supplementation, pain intensity and laboratory results were re-evaluated. After 24 mo, also QUS parameters we re-assessed | Hypovitaminosis D | After 3 mo of vitamin D supplementation, 25 OH-D levels increased while both parathyroid hormone levels and pain intensity decreased. After 24 mo, parathyroid hormone levels and pain intensity further decreased while QUS parameters improved. A relationship between growing pains, vitamin D levels and bone mineral status might exists |
| [26] | Vehapoglu et al (2015) | In 120 children with growing pains, serum 25(OH)D and bone mineral levels were evaluated at the time of enrollment. The pain intensity of those children with vitamin D deficiency was assessed by the pain VAS. After a single oral dose of vitamin D, the pain intensity was re measured at 3 mo. The 25(OH)D levels and VAS scores before and after oral vitamin D administration were compared | Hypovitaminosis D | Supplementation with oral vitamin D resulted in a significant reduction in pain intensity among those children affected by growing pains who also had hypovitaminosis D |
| [27] | Park et al (2015) | In 140 children with growing pains, levels of serum 25-(OH) D were measured. | Hypovitaminosis D | The high prevalence of vitamin D deficiency or insufficiency in Korean children with nonspecific lower-extremity pains, indicative the association between vitamin D deficiency and growing pains have been found |
| [28] | Insaf (2015) | 36 child with growing pains underwent serum levels of vitamin D measurement at the time of presentation. Patients with low level of vitamin D were incorporated into a prospective cohort study and their pain intensity was measured utilizing a pain VAS. After a single oral or intramuscular dose of vitamin D given to those with low vitamin D levels, pain intensity was re measured at 1 mo. The vitamin D levels and (VAS) scores prior and then vitamin D treatment were compared | Hypovitaminosis D | Many children with growing pain had low vitamin D levels. Treatment with vitamin D resulted in diminishing pain severity in those children with growing pains which also had low vitamin D levels |
| [29] | Evans and Scutter (2004) | The prevalence of growing pains in children 4 to 6 yr of age in South Australia were reported. A survey of the parents of children, using a validated questionnaire previously developed for this purpose was used. The sample was systematic and randomized across rural and urban regions, with a total of 1445 valid responses achieved | Family history | Family history in growing pains have been reported |
| [30] | Champion et al (2012) | A twin family design study was applied to 88 pairs with at least one twin individual fulfilling criteria for growing pains. Questionnaires for history of growing pains and restless legs syndrome were completed for these twin pairs, their siblings and parents | Family history | Growing pains might have a genetic etiology and a genetic relationship with restless legs syndrome |
| [31] | Haque et al (2016) | Across sectional study included children from four kindergarten schools was carried out. Questionnaires were distributed among the children for indentifying children with limb pain which were selected for further history and clinical examination. Age and sex matched healthy children were selected as controls for comparison of risk factors | Family history | Obesity, over activity and especially family history were identified as growing pains’ risk factors |
| [32] | Naish and Apley (1951) | 721 children and their mother were questioned regarding the occurrence of pains. Those children with a history satisfying the criteria were examined at the time and subsequently more fully. The assessment was particularly directed to history of pain, family and personal history and mentality whose assessment included school attainments, school and home behavior. Healthy children were questioned and examined in a similar manner as controls | Psychological disturbances | Few children ad an evident over-reaction to all forms of pain, accompanied by emotional instability. The mother’s emotional reactions were also excessive. Emotional disturbances were commoner in children with growing pains. Those children were frequently irritable, nervous, afraid of the dark and also suffering from bad dreams, nightmares, nocturnal enuresis or tics |
| [33] | Oberklaid et al (1997) | 160 children with growing pains were compared with a group of 160 healthy controls. In assessing children’s behavior and temperament at home and school, mothers and teachers were ask to complete several questionnaires | Psychological disturbances | Children with growing pains were rated by their parents but not by their teachers as having different behavioral and temperamental if compared to healthy controls suggesting the psychological contribution to growing pains’ onset |
| [35] | Makay (2009) | - | Melatonin hormone | The author suggested that some activities including the child’s awakening and putting on lights by parents to see what is happening to the child might reduce pain by decreasing melatonin hormone levels |
| [36] | Lech (2002) | Electrolytes contents of hair taken from 173 children aged 1 to 15 yr and young people aged 16 to 18 yr with growing pains were measured, using the flame atomic absorption spectrometry method, and then compared with those of 108 normal, healthy children | Electrolytes contents | Increased levels of lead and zinc and decreased levels of copper were found in children suffering from growing pains if compared with controls. Magnesium levels for ill children were also enhanced, but in the youngest children, the levels were reduced. Mg/Pb and Mg/Zn ratios were lower and Zn/Cu were higher in the group of children suffering from growing pains than in the healthy children |
| [37] | Pathirana et al (2011) | 33 children aged 5 to 12 yr with growing pains were compared to 29 healthy controls. Evidence for peripheral neuropathic disorder was tested by somatosensory testing involved threshold determination and/or response magnitude to non painful stimuli including touch, dynamic brush, cold, vibration, and deep pressure applied to limb and abdominal sites | Somatosensory disorder | Growing pains might be a regional pain syndrome with evidence of mild widespread disorder of somatosensory processing |
| [38] | Golding et al (2012) | Prenatal and postnatal diet, blood measures and variants in fatty acid desaturase genes that influence the metabolism of fatty acids were compared. The study included 1676 children with growing pains at age 8 and 6155 healthy controls | Fatty acids status | No evidence that ω-3 fatty acids status protects against the development of growing pains in childhood have been found |
| [39] | Ekbom (1975) | A family in which the mother has typical restless legs syndrome and also growing pains since her childhood was observed. Severe growing pains were also showed by her three sons | Restless legs syndrome | Growing pains and restless legs are different conditions |
| [40] | Rajaram et al (2004) | 11 children with growing pains were interviewed with their parent to determine if their symptoms of growing pains also met criteria for restless legs syndrome. Those who met clinical criteria for Restless legs syndrome underwent polysomnography whose results were compared to those of 10 healthy controls | Restless legs syndrome | Some children with growing pains also meet diagnostic criteria for restless legs syndrome. A family history of restless legs syndrome have been found among those children |
| [43] | Evans et al (2018) | Foot arches, foot strength, joint mobility, vitamin D and iron levels were examined in 64 children with leg pain and in 13 healthy controls. Children with leg pain were divided into three groups: growing pains, restless legs syndrome, both syndromes are defined for the first time | Increased strength of ankle dorsiflexors and joint mobility were found to be predictive for all types of leg pain. Hypovitaminosis D was detected in 87% of the sample, and anaemia in 13%. Increased body weight, waist girth, and BMI were also found to be associated with leg pain |
Hashkes et al[12] hypothesized that growing pains are a non-inflammatory pain syndrome of early childhood that might be associated with a lower pain threshold. The study revealed that the pain threshold was actually lower at all tested points in children suffering from growing pains except for pressure points on the lower back. However, the anterior tibia area is known to be one of the most painful regions among children with growing pains. In a middle-term follow-up study, Uziel et al[13] highlighted that patients with persistent growing pains still showed lower pain thresholds at all tested points when compared with both controls and children whose growing pains had resolved.
Oster[14] reported a high prevalence of migraine headaches among children with growing pains, and therefore, Hashkes et al[15] tested whether the etiology of growing pains derives from vascular perfusion changes similar to migraine headaches. No significant differences were found among patients with growing pains between painful and painless regions. Furthermore, no significant differences have been identified between children with and without growing pains in both the tibia and femur.
Kaspiris et al[16] analyzed the association of the onset and intensity of growing pains with some perinatal risk factors. The study revealed that a short gestation period, low Apgar score, low birth length or weight, and lower head circumference were positively correlated with the development of growing pains in childhood. There was also a positive correlation with a higher degree of genu valgum. The use of corticosteroids, high maternal age, and tobacco smoking during pregnancy were found not to be predictive of the disorder. Kaspiris et al[17] also reported that children who have been breastfed for fewer than 40 d and those who have not been breastfed at all seemed to have higher chances of developing growing pains.
Many children who undergo observations due to aching legs might also present anatomical abnormalities such as pronated foot posture, which is usually treated using triplane wedges or orthoses. Lee et al[18] investigated whether there is an association between foot posture and growing pains and whether shoe inserts were effective in reducing the frequency and severity of growing pain. In this study, 75% of pediatric patients complaining growing pains had overpronated feet and were treated with customized foot orthoses for 3 mo: Pain episodes were significantly reduced, as well as static, dynamic, and functional balancing abilities. Evans[19] revealed that most of the patients who used triplane wedges or orthoses had no remaining symptoms after the first period of intervention. After the treatment’s withdrawal, symptoms returned in almost all of the patients but decreased in frequency and intensity.
In a subsequent study, Evans and Scutter[20] compared the findings of foot posture and functional health in children aged 4 to 6 years with or without growing pains. However, the results did not reveal any relationship between foot posture, functional health, and growing pains in young children. Viswanathan and Khubchandani[21] assessed the possible association between joint hypermobility and the appearance of growing pains in a cross sectional study. The statistical analysis revealed that joint hypermobility and growing pains were highly related, but to date, this is the only study that has been done to examine this association.
Friedland et al[22] hypothesized that growing pains might represent a local overuse or stress syndrome since pain usually occurs late in the day and is often reported on days of activity. The possible association between growing pains and decreased bone strength was investigated by determining the bone speed of sound (SOS) in children with growing pains. Tibial SOS was significantly reduced in both boys and girls suffering from growing pains in comparison to healthy controls.
Uziel et al[23] examined children with growing pains who had been previously studied to assess the correlation between bone strength and pain symptoms after 5 years of follow up. Compared to previous study results, bone strength seemed to be significantly increased in both males and females, and there were no differences in bone strength between children whose growing pains continued and those whose pains had resolved. Growing pains still persisted in with a low Z-score (SOS Z-score less than 1 or 2 standard deviations of the population mean).
A cross-sectional study performed by Qamar et al[24] showed that patients with vitamin D insufficiency had normal alkaline phosphatase and parathormone levels. Hypocalcemia and hypophosphatemia were found to be more common in patients with vitamin D deficiency, but the findings were not statistically significant. Morandi et al[25] showed an increase in 25-OH-D and a decrease in serum levels of parathyroid hormone after 3 mo of oral treatment. Pain intensity was also found to be lower and even disappeared completely in some cases. At 24 mo, vitamin D serum levels were higher than at the beginning of treatment, but pain intensity was found to have decreased further.
Vehapoglu et al[26] found that 104 out of 120 patients had vitamin D deficiency, and 25% of them presented vitamin D insufficiency. After 3 mo of oral supplementation with vitamin D, pain intensity decreased significantly. Based on these findings, Park et al[27] found lower levels of 25-(OH)D among older patients and also during winter, and the children included in the study mostly suffered from growing pains in winter (41.4%) rather than in summer (12.9%). Insaf[28] estimated serum vitamin D levels in 36 children with growing pains aged 3 to 12 years, and the clinical features improved after oral supplementation with vitamin D. The lowest levels have been reported among children with severe pain, which primarily appeared during the afternoon and was mostly located in the knee and popliteal fossa. Patients who mostly complained of moderate or severe pain before vitamin D supplementation showed a significant reduction of pain severity after treatment, with 31 out of 36 of children being pain free.
A family history of growing pains has been reported by many authors, such as Evans and Scutter[29] and Pavone et al[10] Therefore, Champion et al[30] performed a twin family design study to investigate genetic susceptibility to growing pains. There were higher concordance estimates for growing pains in monozygotic twins, as well as a high prevalence of growing pains in at least one parent of the affected children. Haque et al[31] assessed the frequency of growing pains in a cross sectional study, which revealed that risk factors were significantly more common in children with growing pains, especially when considering their family history.
Naish and Apley[32] support the theory that growing pains might have a psychological component. Children suffering from growing pains showed irritability, nervousness, fear of the dark, nightmares, nocturnal enuresis, tics, and an over-reaction to pain. There was also an association with the emotional instability of the mother. Oberklaid et al[33] found that children with growing pains tend to have behavior problems and to be more anxious, aggressive, and hyperactive. Lowe et al[34] also tried to determine whether the association between growing pains and psychological abnormalities might be related to a familiar pattern. Quality of life and depression levels were found to be the same among parents whose children had growing pains and parents whose children did not. However, mothers of children complaining of growing pains showed higher anxiety levels.
Makay[35] first proposed an association between the levels of the hormone melatonin and the appearance of growing pains. The author suggested that awakening the child due to pain and turning on the lights to see what is happening to the child are some of the activities that might reduce pain by suppressing melatonin levels. Lech et al[36] revealed that electrolyte levels were different between ages and genders. Statistically higher levels of lead and zinc were demonstrated in children with growing pains in comparison to healthy controls. Pathirana et al[37] investigated whether growing pains might be associated with some widespread disorders of somatosensory processing. There was no clinical evidence of a peripheral neuropathic pain syndrome and no significant differences in somatosensory test responses between cases and controls at all the tested sites.
Golding et al[38] found that the dietary ω-3 intake of mothers and children at 3 and 7 years and the duration of did not significantly differ between children with growing pains and healthy controls. Furthermore, no differences have been found in plasma levels of ω-3 and ω-6 fatty acids at 7 years or in the maternal prenatal red cell levels. Many studies have investigated the possible association between restless leg syndrome and growing pains. Ekbom[39] concluded that restless leg syndrome and growing pains are not the same thing. Rajaram et al[40] determined that children with a diagnosis of growing pains might also meet the diagnostic criteria for restless leg syndrome.
Walters et al[41] reviewed the scientific literature on the possible association between growing pains and restless leg syndrome with a specific focus on what these two conditions have in common or how they differ. Simakajornboon et al[42] also confirmed several studies in investigating the etiological association between restless leg syndrome and growing pains. Many of the studies found similarities and positive overlapping findings between the two syndromes. Recently, Evans et al[43] examined several factors that might be predictors of the onset of leg pains. The study revealed that an increment in joint mobility and the strength of ankle dorsiflexion muscles were predictive of leg pain as well as increased body weight and hypovitaminosis D.
The etiology of growing pains remains unknown, and no clear mechanisms have been identified as completely responsible for the manifestation of this pain syndrome. Many theories have been suggested throughout the years, but no one has clarified the major roles in the etiopathogenesis. When the pain threshold was evaluated, it was found to be lower than in healthy controls and persistent[12,13]. These findings suggested that growing pains might be a generalized non-inflammatory pain amplification syndrome of early childhood. Growing pains have also been identified as a local overuse syndrome[22,23]. Children with growing pains had less bone strength than healthy children[22,23]. If local stress were actually able to trigger leg pain, it might explain why painful episodes mainly occur in the late afternoon but not why some patients experience pain in the upper limbs or why pain occurs on days that are not physically demanding[22,23]. One theory proposes that growing pains result from changes in vascular perfusion in painful regions.
Growing pains shares many characteristics with migraine headaches, of which the etiology depends on changes in vascular perfusion. However, no evidence supports this etiological model[14,15]. The anatomical/mechanical theory was first proposed by Hawksley[22,23]. In 2015, the study of Lee et al[18] established overloading on supinator foot muscles in patients affected of overpronated foot as a reason of leg pain due to overuse; the use of foot orthoses could be helpful in the treatment of growing pains, according to the previous study of Evans[19], who, at the same times, highlighted only a partially orthoses efficiency. In addition, both studies[18,19] had several limits, as the small size cohort and short follow-up. Moreover, Evans and Shutter[20] found in a cohort of 180 patients only a weak correlation between foot posture and the child’s functional health and no longer supports the anatomical theory. In 2016, Kaspiris et al[16] found a positive correlation with genu valgum.
Viswanathan and Khubchandani[21] reported a strong association between hypermobility and growing pains given that the simultaneous presence of the two syndromes has been demonstrated in many children.
Vitamin D plays a relevant role in determining bone growth and minera-lization[24-28]. Several hypothesis were formulated: In particularly, Morandi et al[25] reported, in case of vitamin D deficiency, osteoblasts continue to deposit a collagen rubbery matrix on both endosteal and periosteal surfaces of the skeleton causing an outward pressure on periosteal sensory pain fibers and consequent growing pains; other studies supported that growing pains could be an early manifestation of underlying histological changes in bone caused by osteopenia[24] or due to vitamin D receptors of musculoskeletal and nervous system cells[26,27]. Oral vitamin D supplementation has also been shown to be effective in increasing serum vitamin D levels, reducing the intensity of painful episodes[25,26,28].
A familial pattern in growing pains has been reported by many studies, and it seems to play a role in the etiology of growing pains’ as a risk factor[10,29-31]. However, only one study[30] suggested that growing pains are genetically determined. A psychological theory was first proposed by Naish and Apley[32] due to the fact that children with growing pains showed a higher prevalence of behavior and temperament disturbances both at home and school according to parents and teachers. Minor nervous troubles were found to be more common in children presenting growing pains, including irritability, nervousness, nocturnal enuresis, nightmares, and tics.
However, these findings partially disagree with those of Oberklaid et al[33], who showed that children with growing pains were rated to be irritable, solitary, unhappy, and distressed by their parents but not by their teachers. This leads to the belief that even if behavioral and temperament abnormalities are present, they are only evident in the eyes of parents and not teachers. However, the importance of the psychological sphere and the family environment seems to be valid because it is also supported by the evidence of high levels of anxiety among the mothers of affected children[34].
Evidence has revealed perinatal risks factors in developing growing pains during childhood[16]. This association suggests that some perinatal risk factors might alter bone metabolism, bone content, and density, and they might be predictors of the manifestation of growing pains in early childhood[16]. Breastfeeding has also been implicated in the prevention of growing pains[17]. The duration of breastfeeding seems to play a role in the appearance of growing pains with durations greater than 40 days correlating with a lower change of growing pains appearing[17].
The role of melatonin is still controversial and has not been widely investigated. If the association between the nocturnal increase of melatonin and the etiology of growing pains is true, light exposure might represent a therapeutic approach[35]. In the same way, despite some electrolyte alterations having been found among children with growing pains[36], the importance of these results still remains to be investigated further. The pain threshold and the somatosensory response to various non-painful stimuli were tested in children suffering from growth pains[37]. In affected children, the response to some of these stimuli was found to be slightly diffuse rather than specifically localized in the lower limbs compared to healthy controls[37]. This evidence has led to the idea that growing pains might be a regional pain syndrome in which a slight diffusion disorder of the somatosensory processing might be found[37].
Arthritis seems to be influenced by diet and to benefit in particular from the introduction of ω-3 fatty acids, which seems to reduce painful manifestations[38]. However, ω-3 fatty acids do not seem to play a role in either preventing the emergence of the growing pains nor in their treatment[38]. The association between restless leg syndrome and growing pains has long been discussed and verified over the years. Ekbom[39], was the first to investigate this topic but concluded that the two conditions were not associated. Nevertheless, several studies[40-42] do support the theory of a correlation between the two syndromes. There are many common characteristics, such as onset at night and involvement of the lower limbs, but the two syndromes differ in various aspects. Furthermore, the lack of standardized diagnostic criteria for growing pains could make it difficult to distinguish these two entities. For this reason, standardized and universally accepted diagnostic criteria for growing pains need to be established.
Finally, growing pains have recently been associated with not only altered leg-muscle strength, but also with an increase in joint mobility[43]. Children with hypermobile joints report more fatigue with activity than children with normal joint range. Thus, localized biomechanical overload during activity is suggested to lead to the onset of leg pain. In addition, in patients complaining of leg pain, body mass index and body circumference measurements should be performed.
The etiological framing of growing surely represents the most enigmatic aspect of the growing pains phenomenon especially when considering the heterogeneity of the proposed theories and the lack of a univocal consensus. This has led to the belief that different factors, whether individually or in association with each other, might be responsible for the onset of the syndrome. Therefore, it would be highly desirable for other studies to focus on investigating and describing the possible causes and the etiopathogenetic mechanisms underlying growing pains.
Growing pains are the most common cause of musculoskeletal pain in early childhood. The etiopathogenesis of the disease was widely investigated but it is still unknown.
Numerous studies tried to explain the major actors in growing pains etiology but there is a lack of summarize of the evidence.
Analyze the available scientific literature to provide an update on the latest evidence on the etiology
Two databases (Pubmed and Science Direct) were systematically searched for relevant article by two independent reviewer. Every step of the review was done according to PRISMA guidelines. Due to article heterogeneity and the topic after data analysis, a descriptive analysis was performed.
N = 32 articles were included in this systematic review after applying our inclusions and exclusion criteria. Available evidence on growing pains etiology is still inconclusive. Several hypotheses have been researched but none of them was considered decisive.
After our systematic review we conclude that growing pains etiology rely on different factors, that individually or in association, might be responsible for the onset of the syndrome.
Further clinical and preclinical studies are strongly encouraged to understand better the possible causes and the etiopathogenetic mechanisms underlying growing pains. Interesting perspective from studies on vitamin D deficit and supplies and anatomic/mechanical theories were found and should be further investigated.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kaspiris A S-Editor: Ji FF L-Editor: A E-Editor: Wu YXJ
| 1. | Al-Khattat A, Capbell J. Recurrent limb pain in childhood ('growing pains'). The Foot. 2000;10:117-123. [DOI] [Full Text] |
| 2. | Lehman PJ, Carl RL. Growing Pains. Sports Health. 2017;9:132-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Leung AK, Robson WL. Growing Pains: How to manage this benign condition successfully. Can Fam Physician. 1991;37:1463-1467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Abu-Arafeh I, Russell G. Recurrent limb pain in schoolchildren. Arch Dis Child. 1996;74:336-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 63] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Williams MF. Rheumatic Conditions in School-Children. An Investigation into Growing Pains and Nodules (Grains). Lancet. 1928;720-721. [DOI] [Full Text] |
| 6. | Peterson H. Growing pains. Pediatr Clin North Am. 1986;33:1365-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 55] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Asadi-Pooya AA, Bordbar MR. Are laboratory tests necessary in making the diagnosis of limb pains typical for growing pains in children? Pediatr Int. 2007;49:833-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Mohanta MP. Growing pains: practitioners' dilemma. Indian Pediatr. 2014;51:379-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Baxter MP, Dulberg C. "Growing pains" in childhood--a proposal for treatment. J Pediatr Orthop. 1988;8:402-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Pavone V, Lionetti E, Gargano V, Evola FR, Costarella L, Sessa G. Growing pains: a study of 30 cases and a review of the literature. J Pediatr Orthop. 2011;31:606-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15040] [Cited by in RCA: 15745] [Article Influence: 1574.5] [Reference Citation Analysis (1)] |
| 12. | Hashkes PJ, Friedland O, Jaber L, Cohen HA, Wolach B, Uziel Y. Decreased pain threshold in children with growing pains. J Rheumatol. 2004;31:610-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 13. | Uziel Y, Chapnick G, Jaber L, Nemet D, Hashkes PJ. Five-year outcome of children with "growing pains": correlations with pain threshold. J Pediatr. 2010;156:838-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 14. | Oster J. Recurrent abdominal pain, headache and limb pains in children and adolescents. Pediatrics. 1972;50:429-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Hashkes PJ, Gorenberg M, Oren V, Friedland O, Uziel Y. "Growing pains" in children are not associated with changes in vascular perfusion patterns in painful regions. Clin Rheumatol. 2005;24:342-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Kaspiris A, Chronopoulos E, Vasiliadis E. Perinatal Risk Factors and Genu Valgum Conducive to the Onset of Growing Pains in Early Childhood. Children (Basel). 2016;3:pii: E34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Kaspiris A, Zafiropoulou C, Tsadira O, Petropoulos C. Can breastfeeding avert the appearance of growth pains during childhood? Clin Rheumatol. 2007;26:1909-1912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Lee HJ, Lim KB, Yoo J, Yoon SW, Jeong TH. Effect of foot orthoses on children with lower extremity growing pains. Ann Rehabil Med. 2015;39:285-293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Evans AM. Relationship between "growing pains" and foot posture in children: single-case experimental designs in clinical practice. J Am Podiatr Med Assoc. 2003;93:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Evans AM, Scutter SD. Are foot posture and functional health different in children with growing pains? Pediatr Int. 2007;49:991-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Viswanathan V, Khubchandani RP. Joint hypermobility and growing pains in school children. Clin Exp Rheumatol. 2008;26:962-966. [PubMed] |
| 22. | Friedland O, Hashkes PJ, Jaber L, Cohen HA, Eliakim A, Wolach B, Uziel Y. Decreased bone speed of sound in children with growing pains measured by quantitative ultrasound. J Rheumatol. 2005;32:1354-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Uziel Y, Chapnick G, Oren-Ziv A, Jaber L, Nemet D, Hashkes PJ. Bone strength in children with growing pains: long-term follow-up. Clin Exp Rheumatol. 2012;30:137-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Qamar S, Akbani S, Shamim S, Khan G. Vitamin D levels in children with growing pains. J Coll Physicians Surg Pak. 2011;21:284-287. [PubMed] |
| 25. | Morandi G, Maines E, Piona C, Monti E, Sandri M, Gaudino R, Boner A, Antoniazzi F. Significant association among growing pains, vitamin D supplementation, and bone mineral status: results from a pilot cohort study. J Bone Miner Metab. 2015;33:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Vehapoglu A, Turel O, Turkmen S, Inal BB, Aksoy T, Ozgurhan G, Ersoy M. Are Growing Pains Related to Vitamin D Deficiency? Efficacy of Vitamin D Therapy for Resolution of Symptoms. Med Princ Pract. 2015;24:332-338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Park MJ, Lee J, Lee JK, Joo SY. Prevalence of Vitamin D Deficiency in Korean Children Presenting with Nonspecific Lower-Extremity Pain. Yonsei Med J. 2015;56:1384-1388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Insaf AI. Growing Pains in Children and Vitamin D Deficiency, The Impact of Vit D Treatment for Resolution of Symptoms. J Hea Med Nurs. 2017;39:80-85. |
| 29. | Evans AM, Scutter SD. Prevalence of "growing pains" in young children. J Pediatr. 2004;145:255-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 30. | Champion D, Pathirana S, Flynn C, Taylor A, Hopper JL, Berkovic SF, Jaaniste T, Qiu W. Growing pains: twin family study evidence for genetic susceptibility and a genetic relationship with restless legs syndrome. Eur J Pain. 2012;16:1224-1231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 31. | Haque M, Laila K, Islam MM, Islam MI, Talukder MK, Rahman SA. Assessment of growing pain and its risk factors in school children. Am J Clin Exp Med. 2016;4:151-155. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Naish JM, Apley J. "Growing pains": a clinical study of non-arthritic limb pains in children. Arch Dis Child. 1951;26:134-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 70] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 33. | Oberklaid F, Amos D, Liu C, Jarman F, Sanson A, Prior M. "Growing pains": clinical and behavioral correlates in a community sample. J Dev Behav Pediatr. 1997;18:102-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Lowe RM, Hashkes PJ. Growing pains: a noninflammatory pain syndrome of early childhood. Nat Clin Pract Rheumatol. 2008;4:542-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Makay B. Is there a role of melatonin in the development of growing pains? Med Hypotheses. 2009;72:225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 36. | Lech T. Lead, copper, zinc, and magnesium content in hair of children and young people with some neurological diseases. Biol Trace Elem Res. 2002;85:111-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Pathirana S, Champion D, Jaaniste T, Yee A, Chapman C. Somatosensory test responses in children with growing pains. J Pain Res. 2011;4:393-400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 38. | Golding J, Northstone K, Emmett P, Steer C, Hibbeln JR. Do ω-3 or other fatty acids influence the development of 'growing pains'? A prebirth cohort study. BMJ Open. 2012;2:pii: e001370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Ekbom KA. Growing pains and restless legs. Acta Paediatr Scand. 1975;64:264-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 40. | Rajaram SS, Walters AS, England SJ, Mehta D, Nizam F. Some children with growing pains may actually have restless legs syndrome. Sleep. 2004;27:767-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 41. | Walters AS, Gabelia D, Frauscher B. Restless legs syndrome (Willis-Ekbom disease) and growing pains: are they the same thing? A side-by-side comparison of the diagnostic criteria for both and recommendations for future research. Sleep Med. 2013;14:1247-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 42. | Simakajornboon N, Dye TJ, Walters AS. Restless Legs Syndrome/Willis-Ekbom Disease and Growing Pains in Children and Adolescents. Sleep Med Clin. 2015;10:311-322, xiv. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Evans AM, Berde T, Karimi L, Ranade P, Shah N, Khubchandani R. Correlates and predictors of paediatric leg pain: a case-control study. Rheumatol Int. 2018;38:1251-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |