Published online Dec 5, 2018. doi: 10.4292/wjgpt.v9.i6.47
Peer-review started: October 9, 2018
First decision: October 22, 2018
Revised: October 28, 2018
Accepted: November 15, 2018
Article in press: November 15, 2018
Published online: December 5, 2018
Processing time: 57 Days and 23.7 Hours
Management of acute cholecystitis includes initial stabilization and antibiotics. However, the most definitive treatment is cholecystectomy. A small percentage of patients who are not suitable for surgery due to the severity of cholecystitis or comorbidities will require a temporary measure as a bridge to surgery or permanent nonoperative management to decrease the mortality and morbidity. Most of these patients who require conservative management were managed with percutaneous transhepatic cholecystostomy or trans-papillary drainage of gallbladder drainage with cystic duct stenting through endoscopic retrograde cholangiopancreaticography (ERCP). Although, these conservative measures are effective, they can cause significant discomfort to the patients especially if used as a long-term measure. In view of this, there is a need for further minimally invasive procedures, which is safe, effective and comfortable to patients. Endoscopic ultrasound (EUS) guided gallbladder drainage is a novel method of gallbladder drainage first described in 2007[1]. Over the last decade, EUS guided gallbladder drainage has evolved as an effective alternative to percutaneous cholecystostomy and trans-papillary gallbladder drainage. Our goal is to review available literature regarding the scope of EUS guided gallbladder drainage as a viable alternative to percutaneous cholecystostomy or cystic duct stenting through ERCP among patients who are not suitable for cholecystectomy.
Core tip: Acute cholecystitis can be a medical emergency if not treated. The definitive treatment for it is cholecystectomy. However, some patients are not surgically fit and will need to be managed conservatively. Endoscopic ultrasound guided gall bladder drainage is a novel technique and is a means to manage these patients conservatively either as a bridge to surgery until they become surgically fit or a long term management. We discuss the advantages and disadvantages of this technique as an alternative to other known conservative measures.
- Citation: Boregowda U, Umapathy C, Nanjappa A, Wong H, Desai M, Roytman M, Theethira T, Saligram S. Endoscopic ultrasound guided gallbladder drainage - is it ready for prime time? World J Gastrointest Pharmacol Ther 2018; 9(6): 47-54
- URL: https://www.wjgnet.com/2150-5349/full/v9/i6/47.htm
- DOI: https://dx.doi.org/10.4292/wjgpt.v9.i6.47
Acute cholecystitis is a life-threatening inflammatory condition of the gallbladder usually presents with nausea, vomiting, fever and right upper quadrant abdominal pain[2]. Acute cholecystitis is classified into two broad categories based on etiological factors. That is calculous cholecystitis and acalculous cholecystitis.
Gallstones cause more than 90% of the acute cholecystitis, and acalculous cholecystitis accounts for the remaining 5%-10% of the acute cholecystitis. Nearly 10% of the western population is estimated to have gallstones, and 1%-3% of these patients develop symptomatic gallstones. Only 20% of the symptomatic patients eventually develop acute gallstone cholecystitis[3]. Mortality due to acute cholecystitis is approximately 1%-10%[4]. The rate of mortality goes much higher (30% to 90%) depending on the timing of diagnosis[5]. Gallstones cholecystitis is three times more common among women compared to men under age fifty[6].
Acalculous cholecystitis occurs commonly among patients who are on prolonged parenteral nutrition and intensive care stay, trauma, and burns. Other risk factors include uncontrolled diabetes, congestive heart failure, vascular disease, acquired immune deficiency syndrome, drugs (oral contraceptive pills, thiazides) and elderly male patients[7].
Definitive treatment for acute cholecystitis is cholecystectomy. Risk of systemic infection is high if untreated. Complications of acute cholecystitis include gangrenous cholecystitis, gallbladder perforation, biliary peritonitis, cholecystoenteric fistula, pericholecystic abscess, and biliary ileus. The timing of cholecystectomy is usually dependent on the clinical condition of the patient and comorbidities. Approximately 20% of the patients require emergent cholecystectomy. Early laparoscopic cholecystectomy less than 48 h from the time of presentation reduces morbidity, mortality, hospital stay, and costs[8].
Patients with multiple medical comorbidities not suitable for surgery are managed conservatively with gallbladder drainage through cholecystostomy or cystic duct stenting. Early cholecystostomy within 24 h from the time of presentation has shown to reduce hospital stay and procedure related bleeding[9]. Endoscopic ultrasound (EUS) guided gallbladder drainage has created a new paradigm in treating patients with acute cholecystitis who have a contraindication for surgery.
Percutaneous cholecystostomy is a minimally invasive and safe procedure performed to provide immediate decompression of the distended gallbladder using ultrasound or computed tomography guidance. It can be used as a bridge to elective cholecystectomy or as a definitive treatment in severely ill patients who are not candidates for elective cholecystectomy[10-12]. It allows further evaluation of etiology of acute cholecystitis through cholangiogram. Cystic duct or common bile duct stones could be managed through a percutaneous approach.
Common adverse events due to percutaneous cholecystostomy include bleeding, tube dislodgement, bile leak and peritonitis in approximately 12% of the patients[13]. Percutaneous cholecystostomy is contraindicated in patients with massive ascites, intervening bowel loop, uncorrected coagulopathy or those who require anticoagulation. Intrahepatic gallbladder, shrunken/thick-walled gallbladder or concern for patient’s non-adherence is considered as relative contraindications.
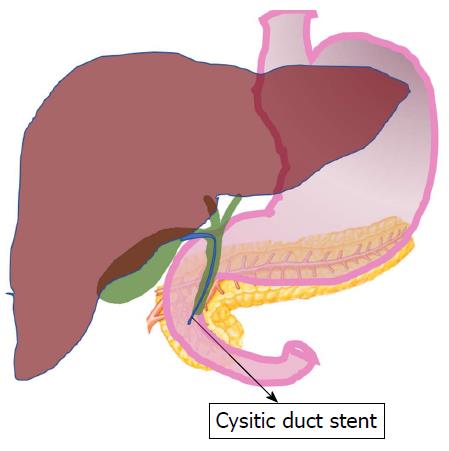
Gallbladder decompression through trans-papillary cystic duct stenting with the help of endoscopic retrograde pancreatography and cholangiography (ERCP) can be used to manage acalculous cholecystitis. After cannulating the common bile duct, a guidewire is passed, and the cystic duct is then selectively cannulated. Cystic duct stent is placed to drain the gallbladder content (Figure 1).
In a retrospective case study on 43 patients who underwent ERCP and cystic duct stent for cholecystitis, 83.7% patients had technical success, and 97% had a clinical success of whom 91.7% improved within 72 h[14]. There were no significant adverse events, and 9% of the patients had an elevated amylase level without abdominal pain.
A retrospective study compared percutaneous cholecystostomy (n = 38) and trans-papillary gallbladder drainage (n = 57) using plastic cystic duct stent with ERCP. Technical success of trans-papillary drainage (89% vs 93%) was lower compared to percutaneous cholecystostomy. However, recurrent cholecystitis in trans-papillary drainage (2%) group was lower compared to percutaneous cholecystostomy (11%) with similar adverse events (8% vs 4%). Patients who underwent cystic duct stenting had the stent in place much longer compared to percutaneous cholecystostomy (three months vs one month)[15].
The role of trans-papillary drainage is limited since it is restricted to patients with acalculous cholecystitis.
The procedure is usually performed using therapeutic linear array echoendoscope. A trans-gastric or trans-duodenal gallbladder puncture is performed under the EUS guidance using a 19-gauge needle. After removing the stylet biliary aspiration and cholecystography are performed in sequence. A 0.035 or 0.025-inch guidewire is introduced through the cannula and coiled in the gallbladder. The gallbladder puncture site is dilated with a Cystotome or needle, and a stent is introduced into the gallbladder. Various types of stents have been used in the past including plastic stent, a self-expandable metal stent and recently lumen apposing metal stents (LAMS). The technical and clinical success of EUS guided drainage by plastic stents is 100%, and pooled analysis showed the adverse events occurred in 5.4% of the patients (Table 1). The technical and clinical success of EUS guided drainage by Naso-biliary drainage is 95.2% and 73.7% respectively, and pooled analysis showed the adverse events occurred in 27.2% of the patients (Table 2). The technical and clinical success of EUS guided drainage by the self-expandable metal stent is 97.5% and 98.5% respectively, and pooled analysis showed the adverse events occurred in 10.4% of the patients (Table 3).
| Author | Study design | Year of publication | Number of patients | Technical success | Clinical success | Adverse event rate |
| Baron et al | Case report | 2007 | 1 | 1 (100%) | 1 (100%) | 0 (0%) |
| Kwan et al | Case series | 2007 | 3 | 3 (100%) | 3 (100%) | 1 (33.3%) |
| Kamala et al | Case report | 2009 | 1 | 1 (100%) | 1 (100%) | 0 (0%) |
| Takasawa et al | Case report | 2009 | 1 | 1 (100%) | 1 (100%) | 0 (0%) |
| Subtil et al | Case series | 2010 | 4 | 4 (100%) | 4 (100%) | 0 (0%) |
| Song et al | Prospective | 2010 | 8 | 8 (100%) | 8 (100%) | 2 (25%) |
| Itoi et al | Case series | 2011 | 2 | 2 (100%) | 2 (100%) | 0 (0%) |
| Author | Study design | Year of publication | Number of patients | Technical success | Clinical success | Adverse event rate |
| Lee et al | Prospective | 2007 | 9 | 9 (100%) | 9 (100%) | 0 (0%) |
| Hikichi et al | Retrospective | 2007 | 1 | 1 (100%) | 1 (100%) | |
| Jang et al | Prospective | 2012 | 30 | 29 (97%) | 29 (100%) | 0 (0%) |
| Itoi et al | Retrospective | 2008 | 43 | 36 (84%) | 35 (95%) | 4 (9%) |
| Author | Type of study | Year of publication | Number of patients included in the study | Technical success (%) | Clinical success (%) | Adverse events (%) |
| Widmer et al | Retrospective | 2015 | 11 | 100 | 100 | 8 |
| Choi et al | Retrospective | 2017 | 14 | 85.7 | 91.7 | 28.5 |
| Jang et al | Prospective | 2011 | 15 | 100 | 100 | 13 |
| Moon et al | Prospective | 2014 | 7 | 100 | 100 | 0 |
| Takagi et al | Retrospective | 2016 | 16 | 100 | 100 | 6 |
| Ahmed et al | Retrospective | 2017 | 13 | 100 | 92.3 | 7.7 |
| Oh et al | Retrospective | 2018 | 76 | 99.3 | 99.3 | 7.1 |
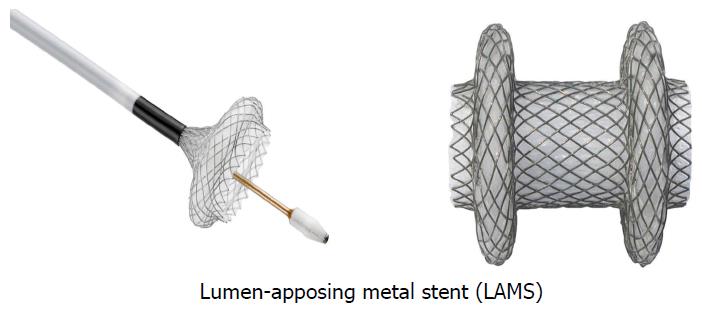
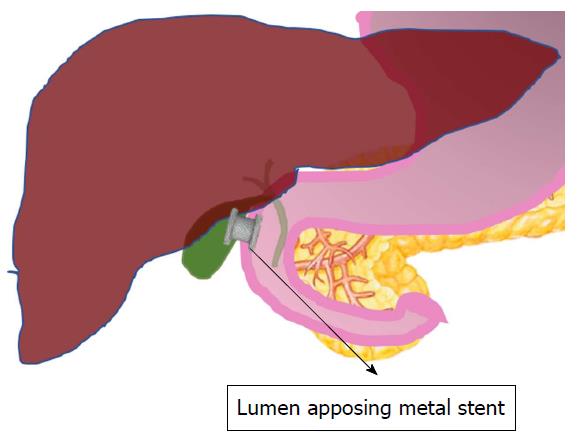
The recent success of LAMS in the drainage of pancreatic pseudocyst and walled off pancreatic necrosis lead to the development of similar LAMS for gallbladder drainage. An electrocautery-enhanced LAMS (EC-LAMS) has made the procedure simpler and reduced the number of instrument exchanges (Figure 2 and Figure 3). The stent can be delivered in a single step[16].
A meta-analysis included 13 studies (7 retrospective studies, five prospective studies, and 1 case-control study) using LAMS involving 233 patients showed EUS guided gallbladder drainage to be an effective, safe and viable alternative to percutaneous cholecystostomy. Technical success and clinical success were 93.86%, and 92.48% respectively. Overall procedure related adverse events were 18.31% and stent-related adverse events were 8.16%[16]. In most cases the stent was left in situ permanently since patients were not suitable for surgery. Outcomes of prior studies on EUS guided gallbladder drainage by LAMS is shown in Table 4.
| Author | Type of study | Year of publication | Number of patients | Technical success (%) | Clinical success (%) | Adverse events (%) |
| de la Serna-Higuera et al | Retrospective | 2013 | 13 | 86.4 | 100 | 18 |
| Irani et al | Retrospective | 2015 | 15 | 93 | 100 | 13 |
| Walter et al | Prospective | 2016 | 30 | 90 | 96 | Not available |
| Law et al | Retrospective | 2016 | 7 | 100 | 100 | 0 |
| Kahaleh et al | Retrospective | 2016 | 35 | 91.4 | 89 | 11 |
| Irani et al | Retrospective | 2017 | 45 | 98 | 96 | 11 |
| Dollhopf et al | Retrospective | 2017 | 75 | 98.7 | 95.9 | 10.7 |
| Teoh et al | Prospective | 2017 | 59 | 100 | 100 | 23.7 |
Electrocautery enhanced LAMS can be placed in a single step using EUS scope alone without the need for fluoroscopy, guidewire placement, and tract dilation. LAMS provides better tissue apposition at both the ends and reduces the risk of stent migration. Presence of silicon lining reduces the risk of leakage and prevents tissue ingrowth, which can aid in the removal of the stent once the fistula matures. The large diameter of the LAMS reduces the risk of stent stenosis or obstruction and allows extraction of gallstones or cholecystography.
Patients with EUS gallbladder drainage procedure have a lower rate of post-procedure pain and the stent can remain patent for a prolonged period. It also adds to the patient’s comfort since there is no need for external drainage to be carried around and mimics natural drainage of biliary secretions into the duodenum. LAMS can be potentially left in situ indefinitely, according to the published literature the longest period of follow up of 3 years, stent patency of 86% was noted[17].
One recent retrospective analysis of long-term outcomes in 21 patients who had documented follow up for more than 12 mo, there were no significant adverse events. Only two patients required repeat endoscopy and found to have tissue overgrowth in one and patent fistula in the other[18].
Most common complications of EUS guided gallbladder drainage are transient abdominal pain, pneumoperitoneum, biliary peritonitis, and stent migration requiring repeat intervention[19]. Bleeding occurs in up to 13% and stent migration in up to 8% of the patients[20]. Other complications include fever, duodenal perforation, stent occlusion, and hematochezia without anemia. Late complications due to EUS guided gallbladder drainage include recurrent cholecystitis in up to 3.2% of the patients and abscess formation[21,22].
Gallbladder drainage with LAMS can be performed though trans-duodenal or trans-gastric approach. Though there is no clear evidence to show that one is better than the other, most endoscopists prefer trans-duodenal approach since the duodenum is retroperitoneal and has minimal peristaltic movements compared to the stomach, which has stronger peristaltic movements. It reduces the chance of stent migration[23]. Due to the presence of larger food particles, stent occlusion is likely to be more in common in the stomach compared the duodenum.
Large multicenter studies are required to define the advantages and disadvantages of each approach. The invention of electrocautery-enhanced LAMS has reduced the need for instrumentation, the time needed for the procedure, and the stent can be delivered in one step.
EUS guided gallbladder drainage can complicate future cholecystectomy and may not be used as bridge therapy. Previous studies have reported up to 79% of the patients who underwent EUS guided gallbladder drainage had successful cholecystectomy[24]. Remaining patients who did not have surgery were either nonsurgical or refused the procedure. However, the real concern is a permanent fistula could have been created due to EUS guided gallbladder drainage, which could have prevented definitive surgery. While most fistulas can close on their own, it is unclear from prior literature the exact number of the fistulas that can close spontaneously.
A recent multicenter study on 34 patients showed that 21 patients with percutaneous cholecystostomy tube and 13 patients who had undergone EUS guided gallbladder drainage by LAMS as a bridge therapy all successfully underwent cholecystectomy[25]. There was no difference in the comorbidity index or post-surgical adverse events. However, data on large multicenter studies are still lacking. The areas that need further research are the technique (trans-gastric vs trans-duodenal) that creates fewer fistulas and the exact rate of spontaneous closure of the fistula so that it can be used a bridge therapy prior to surgery.
In a prospective study, Jang et al[24] compared percutaneous cholecystostomy and EUS guided gallbladder drainage as an alternative for acute cholecystitis in patients who are not candidates for cholecystectomy. A total of 59 patients were randomized into either percutaneous cholecystostomy (n = 29) or EUS guided gallbladder drainage (n = 30) after the failure of medical treatment. Both EUS guided gallbladder drainage and percutaneous cholecystostomy had comparable technical success (97% vs 97%, P = 0.001 for non-inferiority margin of 15%), clinical success (96% vs 100%, P = 0.0001 for non-inferiority margin of 15%), and complications (7% vs 3%, P = 0.999 in the Fisher exact test) rates. The rate of conversion to open cholecystectomy was 9% and 12% respectively. Post-procedure pain score was significantly low among patients who underwent EUS guided drainage compared to percutaneous cholecystostomy (P = 0.001)[24].
In another retrospective comparative study, technical and clinical successes in EUS guided gallbladder drainage (n = 45) and percutaneous cholecystostomy (n = 45) were similar. Technical success was achieved in 98% and 100% respectively (P = 0.88), whereas clinical success was 96% and 91% respectively (P = 0.20). Post-procedure pain score (2.5 vs 6.5; P < 0.05), hospital stay (three days vs nine days, P = 0.05) and repeat interventions (11 vs 12) were significantly low in EUS guided gallbladder drainage compared to percutaneous cholecystostomy. This study also demonstrated a non-significant trend towards lower adverse events (11% vs 32%; P = 0.27) in EUS guided gallbladder drainage compared to percutaneous cholecystostomy[26].
In a prospective cohort study of 118 patients technical success and clinical success for EUS guided gallbladder drainage (n = 59) and percutaneous cholecystostomy (n = 59) were comparable. The rate of overall adverse events (32.2% vs 74.6%; P < 0.001), serious adverse events (23.7% vs 74.6%; P < 0.001) and procedure related readmission rates (6.8 % vs 71.2 %; P < 0.001), were significantly lower in EUS guided gallbladder drainage compared to percutaneous cholecystostomy. Recurrent acute cholecystitis was also lower in the EUS group (0% vs 6.8%) compared to percutaneous cholecystostomy[27].
In a multicenter retrospective study, technical success of EUS guided drainage (n = 42) and percutaneous cholecystostomy (n = 113) drainage (95% vs 99%; P = 0.179) as well as clinical success (95% vs 86%; P = 0.157). EUS guided drainage required a lower number of repeat procedures compared to percutaneous drainage (10% vs 24%; P = 0.037). There was no significant difference in readmission rate or adverse events between the two[28].
A retrospective study evaluated the role of EUS guided gallbladder drainage (n = 14) and percutaneous cholecystostomy (n = 19) in patients with malignant cystic duct obstruction. The technical success (85.7% vs 100%) and clinical successes (91.7% vs 86.4%) were comparable. Adverse events were similar in both the groups (28.5% vs 21.1%). In this study, none of the patients who had clinically successful EUS guided gallbladder drainage required stent removal until endo of life. The mean duration of stent patency was 130.3+/- 35.3 d. However, only in 35.5% of the patients, the cholecystostomy tube was kept until the end of life[29].
The above studies have clearly shown that in appropriately selected patients EUS guided gallbladder drainage is an efficient and safe alternative to percutaneous cholecystostomy for acute cholecystitis among non-surgical patients. EUS guided gallbladder drainage is associated with a reduced hospital stay, adverse events and requires fewer repeat interventions, and is associated with less severe procedure-related pain. The rate of adverse events is either similar or trend lower than percutaneous cholecystostomy. In a retrospective study, the rate of recurrent cholecystitis (17.2% vs 0%; P = 0.043) was also noted to be significantly low in patients who had EUS guided gallbladder drainage when compared to percutaneous cholecystostomy[30].
EUS guided gallbladder drainage unlike percutaneous cholecystostomy obviates the need for external drainage tube, discomfort, and pain caused by percutaneous cholecystostomy. EUS procedures may require general anesthesia and can take a longer time to complete the procedure compared to percutaneous cholecystostomy. Since patients who are not suitable for surgery also tend to be high-risk for general anesthesia[31]. LAMS allows extraction of gallstones and provides better tissue apposition. They reduce the risk of biliary leak and peritonitis but do not completely mitigate the risk and therefore the caution has to be exercised when using it in patients with coagulopathy and ascites[32-34]. Even though lumen-apposing metal stents can be left in situ, permanently stent migration, occlusion and dislodgement have occurred. The reported adverse events after EUS guided gallbladder drainage by LAMS are recurrent cholecystitis (5.1%), gastrointestinal bleeding (2.6%) and stent migration (1.1%)[35].
A percutaneous cholecystostomy tube can be replaced with EUS guided gallbladder drainage through LAMS. It can be considered when percutaneous cholecystostomy tube is used as a bridge therapy for surgery, but the disease course of the patient makes them unsuitable for surgery. This will prevent unwanted discomfort the external drain that comes with percutaneous cholecystostomy.
The gallbladder is usually shrunken after the placement of a percutaneous cholecystostomy. Saline with some contrast can be injected through the tube to enlarge the shrunken gallbladder, and subsequently, it can be punctured under direct visualization by EUS and placement of LAMS. A retrospective study of 7 patients demonstrated 100% technical and clinical success with successful removal of the cholecystostomy tube[36].
In another retrospective study, 21 patients had a replacement of percutaneous cholecystostomy tube with EUS guided LAMS gallbladder drainage with 90.5% technical success. There were no early adverse events. However, two patients required repeat interventions[37]. Larger studies are lacking at this time to accurately predict the risks and benefits of replacing percutaneous cholecystostomy with EUS guided LAMS drainage.
A recent retrospective study compared EUS guided gallbladder drainage to endoscopic trans-papillary drainage. EUS guided gallbladder drainage had significantly better technical success (100% vs 77.3%; P = 0.028). Clinical success (88.9% vs 72.4%; P = 0.076) and adverse events (19.1% vs 16.3%; P = 0.76) were comparable[38].
In a multicenter comparative study, 372 patients were included in the study, 102 patients underwent EUS guided gallbladder drainage, 124 by endoscopic trans-papillary drainage and 146 by percutaneous cholecystostomy. The mean follow up period was 5.2 mo (range 1-34). The technical success for EUS guided gallbladder (94%) and percutaneous cholecystostomy (98%) were significantly higher than trans-papillary drainage (88%) (P = 0.004). The clinical success rate for EUS guided drainage (90%) and percutaneous cholecystostomy was also significantly higher (P = 0.001) compared to trans-papillary drainage (80%). Mean number of procedures required for clinical success was significantly lower for EUS guided drainage compared to trans-papillary and percutaneous cholecystostomy drainage (1 vs 1.7 vs 2.2; P < 0.001). EUS guided drainage and trans-papillary drainage had significantly lower adverse events (13% vs 7% vs 20%; P = 0.01) and unplanned hospital admissions (4% vs 3.2% vs 19.8%; P < 0.001) compared to percutaneous cholecystostomy. Mean hospital stay for EUS drainage was significantly lower compared to both trans-papillary drainage and percutaneous cholecystostomy (16 vs 18 vs 19 d; P = 0.01)[39].
A retrospective study compared EUS guided gallbladder drainage (n = 76) to trans-papillary gallbladder drainage (n = 96). Technical success (98.8%, 82/83 vs 83.3%, 80/96, P < 0.01) and clinical success (98.8%, 82/83 vs ETC: 82.3%, 79/96, P < 0.01) of EUS guided gallbladder drainage was significantly better compared to trans-papillary drainage. Post-procedure adverse events were significantly lower in EUS guided gallbladder drainage compared to trans-papillary gallbladder drainage[22].
Above studies and previously published data has shown a clear advantage of EUS guided gallbladder drainage to be a safe and efficient procedure compared to trans-papillary drainage with significantly better technical and clinical success with lower adverse events and lesser hospital stay and fewer repeat procedures.
Cholecystectomy is the gold standard for treatment of acute cholecystitis, and early cholecystectomy is preferred over delayed or interval cholecystectomy. Elderly patients with significant comorbidities and not candidates for surgery are usually managed with non-surgical interventions like percutaneous cholecystostomy or ERCP. Recent advances in endoscopic methods and utilization of EUS guided LAMS has led to the development of EUS guided gallbladder drainage. Over last decade EUS guided gallbladder drainage has gained significant popularity with high technical and clinical success comparable to that of percutaneous cholecystostomy or trans-papillary drainage. It has lower adverse events, hospital stay and requires fewer repeat procedures[24,26-28,32].
EUS guided gallbladder drainage is a safe, effective and viable non-surgical method of gallbladder drainage for acute cholecystitis, in patients who are deemed to never undergo cholecystostomy as they are not fit for surgery. Although the limited available evidence is promising, prospective large multicenter studies are needed before EUS guided gallbladder drainage can be used as a first-line treatment instead of percutaneous cholecystostomy as a bridge therapy for all patients who are non-surgical candidates initially and require definitive surgical intervention later for acute cholecystitis.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Aoki H, Poullis A, Abbasnezhad S- Editor: Dou Y L- Editor: A E- Editor: Bian YN
| 1. | Baron TH, Topazian MD. Endoscopic transduodenal drainage of the gallbladder: implications for endoluminal treatment of gallbladder disease. Gastrointest Endosc. 2007;65:735-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Katabathina VS, Zafar AM, Suri R. Clinical Presentation, Imaging, and Management of Acute Cholecystitis. Tech Vasc Interv Radiol. 2015;18:256-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Friedman GD. Natural history of asymptomatic and symptomatic gallstones. Am J Surg. 1993;165:399-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 251] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 4. | Kimura Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Windsor JA, Mayumi T, Yoshida M. TG13 current terminology, etiology, and epidemiology of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:8-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 5. | Huffman JL, Schenker S. Acute acalculous cholecystitis: a review. Clin Gastroenterol Hepatol. 2010;8:15-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 181] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 6. | Indar AA, Beckingham IJ. Acute cholecystitis. BMJ. 2002;325:639-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 153] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 7. | Kimura Y, Takada T, Kawarada Y, Nimura Y, Hirata K, Sekimoto M, Yoshida M, Mayumi T, Wada K, Miura F. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:15-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 241] [Cited by in RCA: 302] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 8. | Zafar SN, Obirieze A, Adesibikan B, Cornwell EE 3rd, Fullum TM, Tran DD. Optimal time for early laparoscopic cholecystectomy for acute cholecystitis. JAMA Surg. 2015;150:129-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Chou CK, Lee KC, Chan CC, Perng CL, Chen CK, Fang WL, Lin HC. Early Percutaneous Cholecystostomy in Severe Acute Cholecystitis Reduces the Complication Rate and Duration of Hospital Stay. Medicine (Baltimore). 2015;94:e1096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Molavi I, Schellenberg A, Christian F. Clinical and operative outcomes of patients with acute cholecystitis who are treated initially with image-guided cholecystostomy. Can J Surg. 2018;61:195-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Leveau P, Andersson E, Carlgren I, Willner J, Andersson R. Percutaneous cholecystostomy: a bridge to surgery or definite management of acute cholecystitis in high-risk patients? Scand J Gastroenterol. 2008;43:593-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Zarour S, Imam A, Kouniavsky G, Lin G, Zbar A, Mavor E. Percutaneous cholecystostomy in the management of high-risk patients presenting with acute cholecystitis: Timing and outcome at a single institution. Am J Surg. 2017;214:456-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Sanjay P, Mittapalli D, Marioud A, White RD, Ram R, Alijani A. Clinical outcomes of a percutaneous cholecystostomy for acute cholecystitis: a multicentre analysis. HPB (Oxford). 2013;15:511-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 107] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 14. | Itoi T, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Ishii K, Tsuji S, Ikeuchi N, Tsukamoto S, Takeuchi M. Endoscopic transpapillary gallbladder drainage in patients with acute cholecystitis in whom percutaneous transhepatic approach is contraindicated or anatomically impossible (with video). Gastrointest Endosc. 2008;68:455-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 118] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 15. | Luangsukrerk T, Ridtitid W, Angsuwatcharakon P, Kongkam P, Rerknimitr R. Outcome of endoscopic transpapillary gallbladder stent placement versus percutaneous cholecystostomy in patients with acute cholecystitis and gallstone-related disease who are high risk for surgery. Gastrointest Endosc. 2018;87:AB586-AB587. |
| 16. | Peñas-Herrero I, de la Serna-Higuera C, Perez-Miranda M. Endoscopic ultrasound-guided gallbladder drainage for the management of acute cholecystitis (with video). J Hepatobiliary Pancreat Sci. 2015;22:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 17. | Choi JH, Lee SS, Choi JH, Park DH, Seo DW, Lee SK, Kim MH. Long-term outcomes after endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis. Endoscopy. 2014;46:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 117] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 18. | Torres-Yuste R, Penas-Herrero I, Sánchez-Ocana R, Cimavilla M, de Benito M, Santos J, Gil-Simon P, la Serna CD, Manuel Perez-Mirandaet M. Long-Term Clinical Outcomes of Eus-Guided Gallbladder Drainage Eus-Gbd With Lumen-Apposing Metal Stents (LAMS). Gastrointest Endosc. 2017;85:AB61. [DOI] [Full Text] |
| 19. | Kalva NR, Vanar V, Forcione D, Bechtold ML, Puli SR. Efficacy and Safety of Lumen Apposing Self-Expandable Metal Stents for EUS Guided Cholecystostomy: A Meta-Analysis and Systematic Review. Can J Gastroenterol Hepatol. 2018;2018:7070961. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 20. | Saumoy M, Novikov A, Kahaleh M. Long-term outcomes after EUS-guided gallbladder drainage. Endosc Ultrasound. 2018;7:97-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 21. | Kahaleh M, Perez-Miranda M, Artifon EL, Sharaiha RZ, Kedia P, Peñas I, De la Serna C, Kumta NA, Marson F, Gaidhane M. International collaborative study on EUS-guided gallbladder drainage: Are we ready for prime time? Dig Liver Dis. 2016;48:1054-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Oh D, Song TJ, Cho DH, Park DH, Seo DW, Lee SK, Kim MH, Lee SS. EUS-guided cholecystostomy versus endoscopic transpapillary cholecystostomy for acute cholecystitis in high-risk surgical patients. Gastrointest Endosc. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 74] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 23. | Walter D, Teoh AY, Itoi T, Pérez-Miranda M, Larghi A, Sanchez-Yague A, Siersema PD, Vleggaar FP. EUS-guided gall bladder drainage with a lumen-apposing metal stent: a prospective long-term evaluation. Gut. 2016;65:6-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 146] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 24. | Jang JW, Lee SS, Song TJ, Hyun YS, Park DY, Seo DW, Lee SK, Kim MH, Yun SC. Endoscopic ultrasound-guided transmural and percutaneous transhepatic gallbladder drainage are comparable for acute cholecystitis. Gastroenterology. 2012;142:805-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 180] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 25. | Saumoy M, Tyberg A, Brown E, Eachempati SR, Lieberman M, Afaneh C, Kunda R, Cosgrove N, Siddiqui A, Gaidhane M. Successful Cholecystectomy After Endoscopic Ultrasound Gallbladder Drainage Compared With Percutaneous Cholecystostomy, Can it Be Done? J Clin Gastroenterol. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 61] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 26. | Irani S, Ngamruengphong S, Teoh A, Will U, Nieto J, Abu Dayyeh BK, Gan SI, Larsen M, Yip HC, Topazian MD. Similar Efficacies of Endoscopic Ultrasound Gallbladder Drainage With a Lumen-Apposing Metal Stent Versus Percutaneous Transhepatic Gallbladder Drainage for Acute Cholecystitis. Clin Gastroenterol Hepatol. 2017;15:738-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 149] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 27. | Teoh AYB, Serna C, Penas I, Chong CCN, Perez-Miranda M, Ng EKW, Lau JYW. Endoscopic ultrasound-guided gallbladder drainage reduces adverse events compared with percutaneous cholecystostomy in patients who are unfit for cholecystectomy. Endoscopy. 2017;49:130-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 28. | Tyberg A, Saumoy M, Sequeiros EV, Giovannini M, Artifon E, Teoh A, Nieto J, Desai AP, Kumta NA, Gaidhane M. EUS-guided Versus Percutaneous Gallbladder Drainage: Isn’t It Time to Convert? J Clin Gastroenterol. 2018;52:79-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 29. | Choi JH, Kim HW, Lee JC, Paik KH, Seong NJ, Yoon CJ, Hwang JH, Kim J. Percutaneous transhepatic versus EUS-guided gallbladder drainage for malignant cystic duct obstruction. Gastrointest Endosc. 2017;85:357-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 30. | Inoue T, Okumura F, Kachi K, Fukusada S, Iwasaki H, Ozeki T, Suzuki Y, Anbe K, Nishie H, Mizushima T. Long-term outcomes of endoscopic gallbladder stenting in high-risk surgical patients with calculous cholecystitis (with videos). Gastrointest Endosc. 2016;83:905-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 31. | Baars JE, Kaffes AJ, Saxena P. EUS-guided biliary drainage: A comprehensive review of the literature. Endosc Ultrasound. 2018;7:4-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 32. | Dollhopf M, Larghi A, Will U, Rimbaş M, Anderloni A, Sanchez-Yague A, Teoh AYB, Kunda R. EUS-guided gallbladder drainage in patients with acute cholecystitis and high surgical risk using an electrocautery-enhanced lumen-apposing metal stent device. Gastrointest Endosc. 2017;86:636-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 121] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 33. | Anderloni A, Attili F, Sferrazza A, Rimbas M, Costamagna G, Repici A, Larghi A. EUS-guided gallbladder drainage using a lumen-apposing self-expandable metal stent in patients with coagulopathy or anticoagulation therapy: a case series. Endosc Int Open. 2017;5:E1100-E1103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 34. | Jamwal KD, Sharma MK, Maiwall R, Sharma BK, Sarin SK. EUS-guided Gall Bladder Drainage in Severe Liver Disease: A Single-center Experience in Critically Ill Cirrhotics. J Clin Transl Hepatol. 2018;6:35-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 35. | Jain D, Bhandari BS, Agrawal N, Singhal S. Endoscopic Ultrasound-Guided Gallbladder Drainage Using a Lumen-Apposing Metal Stent for Acute Cholecystitis: A Systematic Review. Clin Endosc. 2018;51:450-462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 36. | Law R, Grimm IS, Stavas JM, Baron TH. Conversion of Percutaneous Cholecystostomy to Internal Transmural Gallbladder Drainage Using an Endoscopic Ultrasound-Guided, Lumen-Apposing Metal Stent. Clin Gastroenterol Hepatol. 2016;14:476-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 37. | Minaga K, Yamashita Y, Ogura T, Takenaka M, Shimokawa Y, Hisa T, Itonaga M, Kato H, Nishikiori H, Okuda A. Clinical efficacy and safety of endoscopic ultrasound-guided gallbladder drainage replacement of percutaneous drainage: A multicenter retrospective study. Dig Endosc. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 38. | Matsubara S, Nakai Y, Isayama H, Ishigaki K, Umefune G, Watanabe T, Takagi K, Akiyama D, Takahara N, Uchino R. Endoscopic ultrasonography-guided gallbladder drainage is superior to endoscopic transpapillary gallbladder drainage for acute cholecystitis. Gastrointest Endosc. 2016;83:AB339. [DOI] [Full Text] |
| 39. | Kunda R, Sharaiha RZ, Siddiqui A, Tyberg A, Arain MA, Noor A, Mumtaz T, Iqbal U, Loren DE, Kowalski TE. Endoscopic Ultrasound-Guided Transmural Gallbladder Drainage Using Lumen-Apposing Metal Stents Versus Endoscopic Transpapillary Drainage Versus Percutaneous Cholecystostomy for Gallbladder Drainage in High-Risk Surgical Patients With Acute Cholecystitis: Clinical Outcomes and Success in an International, Multicenter, Comparative Trial. Gastrointest Endosc. 2017;85:AB60-AB61. [DOI] [Full Text] |