Published online Nov 6, 2015. doi: 10.4292/wjgpt.v6.i4.244
Peer-review started: April 24, 2015
First decision: July 17, 2015
Revised: August 31, 2015
Accepted: October 1, 2015
Article in press: October 8, 2015
Published online: November 6, 2015
Processing time: 202 Days and 1.7 Hours
AIM: To look at the relationship between eosinophilic oesophagitis (EO) and food bolus impaction in adults.
METHODS: We retrospectively analysed medical records of 100 consecutive patients who presented to our hospital with oesophageal food bolus obstruction (FBO) between 2012 and 2014. In this cohort, 96 were adults (64% male), and 4 paediatric patients were excluded from the analysis as our centre did not have paediatric gastroenterologists. Eighty-five adult patients underwent emergency gastroscopy. The food bolus was either advanced into the stomach using the push technique or retrieved using a standard retrieval net. Biopsies were obtained in 51 patients from the proximal and distal parts of the oesophagus at initial gastroscopy. All biopsy specimens were assessed and reviewed by dedicated gastrointestinal pathologists at the Department of Pathology, University Hospital Geelong. The diagnosis of EO was defined and established by the presence of the following histological features: (1) peak eosinophil counts > 20/hpf; (2) eosinophil microabscess; (3) superficial layering of eosinophils; (4) extracellular eosinophil granules; (5) basal cell hyperplasia; (6) dilated intercellular spaces; and (7) subepithelial or lamina propria fibrosis. The histology results of the biopsy specimens were accessed from the pathology database of the hospital and recorded for analysis.
RESULTS: Our cohort had a median age of 60. Seventeen/51 (33%) patients had evidence of EO on biopsy findings. The majority of patients with EO were male (71%). Classical endoscopic features of oesophageal rings, furrows or white plaques and exudates were found in 59% of patients with EO. Previous episodes of FBO were present in 12/17 patients and 41% had a history of eczema, hay fever or asthma. Reflux oesophagitis and benign strictures were found in 20/34 patients who did not have biopsies.
CONCLUSION: EO is present in approximately one third of patients who are admitted with FBO. Biopsies should be performed routinely at index endoscopy in order to pursue this treatable cause of long term morbidity.
Core tip: Eosinophilic oesophagitis (EO) is a clinical entity that is becoming more frequent in patients seeking medical attention for food bolus obstruction (FBO). The main symptom in adult patients is dysphagia. Various studies have shown the presence of EO in 20% to 54% of the patients presenting with food bolus impaction. Approximately one in three patients who presents with FBO has EO. Biopsies should be performed routinely at index endoscopy in order to pursue this treatable cause of long term morbidity.
- Citation: Heerasing N, Lee SY, Alexander S, Dowling D. Prevalence of eosinophilic oesophagitis in adults presenting with oesophageal food bolus obstruction. World J Gastrointest Pharmacol Ther 2015; 6(4): 244-247
- URL: https://www.wjgnet.com/2150-5349/full/v6/i4/244.htm
- DOI: https://dx.doi.org/10.4292/wjgpt.v6.i4.244
Eosinophilic oesophagitis (EO) is an emerging cause of food bolus impaction and dysphagia in adults and children[1]. According to Kerlin et al[2], acute food bolus obstruction (FBO) is frequently encountered as a gastrointestinal emergency. FBO is the third most common gastrointestinal emergency after gastrointestinal bleed in the upper and lower gastrointestinal tracts[2]. Approximately two thirds of FBO in adults of the Western world are caused by food bolus impaction with meat in comparison to fish bones in Asia[1]. The condition of the oesophagus and the type of food bolus play a role in food impaction. Risk factors for FBO include edentulous individuals and known oesophageal pathology amongst others[3]. With regards to the management of FBO, Ikenberry et al[4] recommended a time frame of 6 h to remove the food bolus due to the potential risk of ischaemia, necrosis and perforation.
There is a paucity of data on the epidemiological changes in FBO and its link to EO. According to a study, EO was found in 54% of patients presenting with oesophageal food bolus impaction[5]. The incidence of EO is rising as clinicians become more familiar with this condition. Currently, EO is a clinicopathologic entity defined by symptoms related to oesophageal dysfunction and eosinophil-predominant inflammation on oesophageal biopsies characterised by a peak value of ≥ 15 eosinophils per high power field[6,7].
Our aim of this study was to evaluate the association of EO with FBO in adults. We retrospectively analysed medical records relating to 100 consecutive patients who presented to a tertiary hospital with oesophageal FBO between 2012 and 2014. There were a total of 96 adult patients and 4 paediatric patients (age < 16), whom were excluded from this study. Sixty-four percent of the adult patients were males. Out of this 96 patients, 11 of them required ear, nose and throat intervention or declined gastroscopy. These patients have also been excluded from this analysis. A total of 85 adult patients with FBO underwent gastroscopy and during this procedure, the food bolus was either advanced into the stomach using push technique or removed using retrieval net. Biopsies were obtained in 51 patients from proximal and distal parts of the esophagus.
Biopsies were analysed in the laboratory by experienced gastrointestinal pathologists and the cut off point of more than 20 eosinophils per high power field (hpf) was considered in cases of EO.
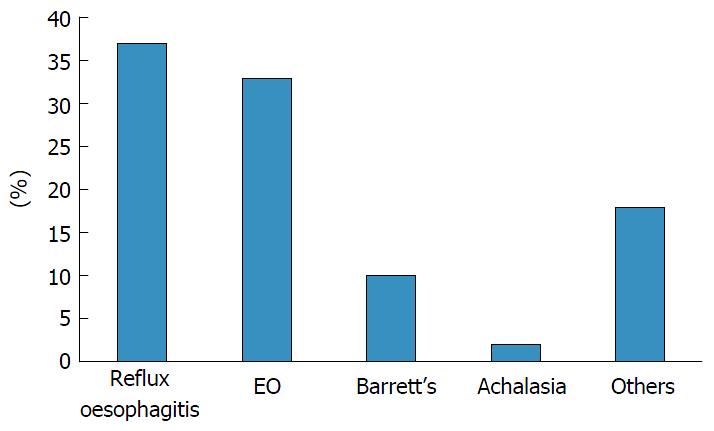
The median age of the cohort was 60. Out of the 51 patients who had biopsies, 19 (37%) patients had reflux oesophagitis confirmed histologically, which made up the majority of patients with FBO. This was followed by EO (33%), barrett’s oesophagus (10%) and achalasia (2%). eighteen percent of these biopsies were attributed to other causes, which included benign changes and non-specific inflammation. The results are shown in Figure 1.
The majority of patients with EO were male (71%). Classical endoscopic features of oesophageal rings, furrows or white plaques and exudates were found in 59% of patients with EO. The median age for EO patients was 3O. Twelve out of the 17 patients (59%) had prior episodes of FBO and 41% had a history of atopy (hay fever, asthma and eczema).
Among the 34 patients who did not have biopsies, 20 of them had endoscopic changes consistent with gastro-oesophageal reflux disease or pre-existing benign strictures.
There is an increasing awareness towards EO. This condition refers to symptoms related to oesophageal dysfunction with evidence of eosinophil-predominant inflammation on oesophageal biopsies which is characterised by a peak value of EO ≥ 15 eosinophils per high power field. The exclusion of secondary causes of oesophageal eosinophilia and the presence of mucosal eosinophilia being isolated to the oesophagus and persisting after a proton pump inhibitor trial are also included in the diagnostic criteria for EO[6]. Eosinophils are not normally present in the normal esophageal epithelia. The presence of eosinophilia indicates abnormality but unfortunately, this does not point towards EO but also other causes such as reflux esophagitis. EO usually affects young adults and in our study, the mean age of patients with EO was 3O. Our results have shown that one in three patients who presents with FBO has EO. Endoscopic evidence of EO was not present in all the patients which confirms findings from previous studies[8]. They demonstrated 10%-20% of EO patients can have an endoscopically normal appearing oesophagus. According to Kerlin et al[2], there is increased awareness of EO as a contributing factor to dysphagia and chest discomfort especially in young men. Our results are consistent with the Kerlin study which showed that up to one third of patients who presented with food bolus impaction have EO.
Besides being a retrospective study with its own intrinsic limitations, this is a small study with 100 patients’ medical records analysed. Therefore, our analysis will have Type 1 error. Our laboratory uses the cut-off point of 20 eosinophils/hpf. According to the current guidelines, EO is defined histologically with eosinophils count of 15 or more eosinophils/hpf. The current recommendation is to take at least two to four biopsies from the distal and proximal oesophagus. We did not have a uniform protocol for the number of biopsies to be taken for each patient.
This study demonstrates that EO plays an essential role in food bolus impaction of the oesophagus. Patients who present with FBO have approximately a1 in 3 chance of having EO. This condition is not always associated with clear macroscopic changes or a history of atopy. In patients with no obvious cause for FBO, biopsies should be performed routinely at index endoscopy in order to pursue this treatable cause of long term morbidity.
Since the first description of eosinophilic oesophagitis (EO) in 1962 by Schreiber, there has been a growing recognition and understanding of this condition. Food bolus obstruction (FBO) in the esophagus is most commonly related to reflux-related oesophageal diseases and oesophageal dysmotility. EO has been reported as an uncommon cause of FBO. Epidemiological data on FBO and its relationship to EO remain limited.
FBO in the oesophagus is becoming a common mode of presentation for EO. The authors recommend that biopsies should be performed at index endoscopy in order not to miss the diagnosis.
The authors’ findings suggest that EO should be thought of in all cases of FBO and biopsies should be performed in all instances where there is no macroscopic abnormality on upper endoscopy. The results confirm the findings of a previous retrospective study done in Australia and highlight the need for large prospective studies to assess the demographics and aetiology of FBO.
The changes in the aetiology of FBO can be attributed to an increasing recognition and prevalence of EO especially in the younger population. Proximal and distal oesophageal biopsies should be attempted at index endoscopy in order to pursue this treatable cause of long term morbidity.
The conceptual definition of EO is considered as a chronic, immune antigen-mediated oesophageal disease characterised clinically by symptoms related to oesophageal dysfunction and histologically by eosinophil-predominant inflammation.
This retrospective report focuses on patients presenting with food bolus impaction.
P- Reviewer: Day AS, Franzen T S- Editor: Ji FF
L- Editor: A E- Editor: Li D
| 1. | Attwood SE, Furuta GT. Eosinophilic esophagitis: historical perspective on an evolving disease. Gastroenterol Clin North Am. 2014;43:185-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Kerlin P, Jones D, Remedios M, Campbell C. Prevalence of eosinophilic esophagitis in adults with food bolus obstruction of the esophagus. J Clin Gastroenterol. 2007;41:356-361. [PubMed] |
| 3. | Chauvin A, Viala J, Marteau P, Hermann P, Dray X. Management and endoscopic techniques for digestive foreign body and food bolus impaction. Dig Liver Dis. 2013;45:529-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Decker GA, Fanelli RD, Fisher LR, Fukami N. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73:1085-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 501] [Article Influence: 35.8] [Reference Citation Analysis (1)] |
| 5. | Desai TK, Stecevic V, Chang CH, Goldstein NS, Badizadegan K, Furuta GT. Association of eosinophilic inflammation with esophageal food impaction in adults. Gastrointest Endosc. 2005;61:795-801. [PubMed] |
| 6. | Furuta GT, Liacouras CA, Collins MH, Gupta SK, Justinich C, Putnam PE, Bonis P, Hassall E, Straumann A, Rothenberg ME. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007;133:1342-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1253] [Cited by in RCA: 1155] [Article Influence: 64.2] [Reference Citation Analysis (0)] |
| 7. | Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, Bonis PA, Burks AW, Chehade M, Collins MH, Dellon ES. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3-20.e6; quiz 21-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1605] [Cited by in RCA: 1486] [Article Influence: 106.1] [Reference Citation Analysis (1)] |
| 8. | Dellon ES, Aderoju A, Woosley JT, Sandler RS, Shaheen NJ. Variability in diagnostic criteria for eosinophilic esophagitis: a systematic review. Am J Gastroenterol. 2007;102:2300-2313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |