Published online Nov 28, 2011. doi: 10.4329/wjr.v3.i11.256
Revised: July 4, 2011
Accepted: July 11, 2011
Published online: November 28, 2011
Over the past several years, advances in the technical domain of computed tomography (CT) have influenced the trend of imaging modalities used in the clinical evaluation of the urinary system. Renal collecting systems can be illustrated more precisely with the advent of multi-detector row CT through thinner slices, high speed acquisitions, and enhanced longitudinal spatial resolution resulting in improved reformatted coronal images. On the other hand, a significant increase in exposure to ionizing radiation, especially in the radiosensitive organs, such as the gonads, is a concern with the increased utilization of urinary tract CT. In this article, we discuss the strategies and techniques available for reducing radiation dose for a variety of urinary tract CT protocols with metabolic clinical examples. We also reviewed CT for hematuria evaluation and related scan parameter optimization such as, reducing the number of acquisition phases, CT angiography of renal donors and lowering tube potential, when possible.
- Citation: Sung MK, Singh S, Kalra MK. Current status of low dose multi-detector CT in the urinary tract. World J Radiol 2011; 3(11): 256-265
- URL: https://www.wjgnet.com/1949-8470/full/v3/i11/256.htm
- DOI: https://dx.doi.org/10.4329/wjr.v3.i11.256
In the past decade, developments in computed tomography (CT) technology have changed the trend of imaging modalities used in the evaluation of the urinary system. The introduction of multi-detector row CT (MDCT) allows us to depict the renal collecting systems accurately through thinner section imaging, faster scanning, improved longitudinal spatial resolution, and the subsequent better quality of reformatted coronal images. With these advances, MDCT has largely replaced plain film radiography, excretory urography and tomography for a variety of urinary tract disorders such as urolithiasis, renal masses and mucosal abnormalities of the renal collecting system, ureters and bladder[1-4].
However, an exponential increase in use due to the dramatic evolution of CT over the past decade has also resulted in a substantial increase in exposure to ionizing radiation. From the urinary tract evaluation standpoint with CT scanning, it is important to bear in mind that follow-up or recurrent CT imaging (kidney stones) as well as multiphase contrast-enhanced CT increases radiation dose to patients. Leusmann et al[5] estimated a 35% relative recurrence rate of urinary calculi over 10 years. Kaltz et al[6] reported that 4% (176/4562) of patients who underwent CT examinations for renal colic had three or more CT examinations, resulting in radiation exposure of 20-154 mSv. In addition, most CT protocols for evaluation of the urinary tract such as CT urography or CT for renal donors consist of the acquisition of two or more phases of contrast enhancement, which increases radiation dose to patients.
It is, therefore, important to initiate strategies and efforts to reduce radiation dose associated with CT scanning of the urinary tract. In this article, we discuss the strategies and techniques available for reducing radiation dose for a variety of urinary tract CT protocols with metabolic clinical examples.
In order to maintain a favorable risk vs benefit, it is necessary to ensure that CT is indeed indicated for the clinical information desired. Table 1 summarizes the major clinical indications for CT examinations of the urinary tract. Once CT scanning has been justified, efforts should be made to keep the radiation dose as low as reasonably achievable (ALARA principle) while maintaining the diagnostic confidence of the interpreting radiologists. There are two clinical scenarios for dose reduction in urinary tract CT. Firstly, the presence of high inherent contrast between radio-opaque renal calculi and urinary tract soft tissue allows radiologist to diagnose urinary tract calculi at a lower dose and much higher noise. Similarly, the presence of higher contrast between contrast opacified urinary tract and the adjacent soft tissue can also allow lesion detection and characterization at lower dose noisy images. Secondly, dose reduction is also important for CT performed for the evaluation of healthy and younger renal donors.
| Urinary colic |
| Hematuria |
| Complicated infection |
| Neoplasm |
| Renal donor evaluation |
| Congenital anomalies |
| Structural abnormalities |
| Abdominal trauma |
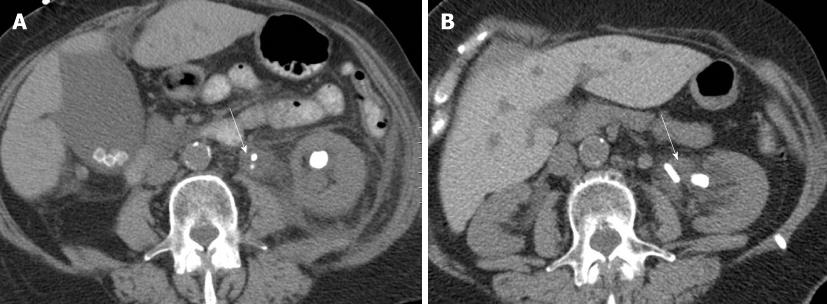
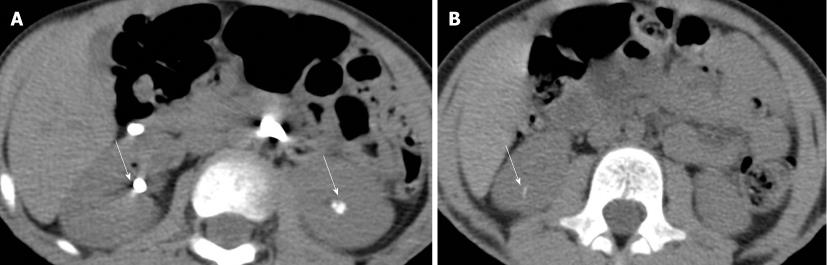
Following its introduction by Smith et al[1], unenhanced helical CT has become the preferred diagnostic method for the evaluation of urolithiasis in patients with acute flank pain referred for urinary stone disease. Patients with urinary stone disease may undergo multiple CT examinations due to recurrence of stone disease, which increases their cumulative radiation dose. Since urolithiasis is a mostly non-fatal disease which is common in younger patients, radiation dose should be reduced. Previous studies have shown that a low dose CT protocol may be suitable for the evaluation of patients with suspected urinary stone disease due to the high contrast between urinary tract stones and the adjacent relatively lower attenuation of soft tissue[7-14]. Table 2 shows radiation dose, scanning parameters, and diagnostic performances of CT examinations using low dose protocols in patients with urinary tract calculi. The protocol used at our institute for the evaluation of renal calculi is shown in Table 3 (Figures 1 and 2). Katz et al[6] reported that the mean effective doses for a single conventional stone protocol using single-detector row CT and MDCT were 6.5 and 8.5 mSv, respectively, which is 1.8-17 times higher than those used in the low dose protocol.
| Authors | Yr | Low dose CT protocols | Diagnostic performance | Effective dose (mSv) | ||||||
| CT scanner | kVp | mA (mAs) | Pitch | S.T. (mm) | Sensitivity (%) | Specificity (%) | Accuracy (%) | |||
| Liu et al[7] | 2000 | SDCT | 120 | (280) | 2 | 7 | 97 | 96 | 97 | 2.8 |
| Meagher et al[8] | 2001 | SDCT, 4MDCT | 120-130 | 63-130 | 1.4-1.8 | 5 | 93 | NA | NA | 3.5 (2.8-4.5) |
| Hamm et al[9] | 2002 | 4MDCT | 120 | 70 | 2 | 5 | 96 | 97 | NA | 1.5 |
| Heneghan et al[10] | 2003 | SDCT | 140 | 100 (76) | 1.5 | 5 | NA | NA | 90-94 | 6.4 |
| 4MDCT | 0.75 | 11 | ||||||||
| Tack et al[11] | 2003 | 4MDCT | 120 | (30) | 1.5 | 3 | 90-95 | 94-100 | 93-98 | 1.2-1.9 |
| Knöpfle et al[12] | 2003 | 4MDCT | 120 | 70 | 2 | 5 | 98 | 97 | NA | 0.97 (male)/ 1.35 (female) |
| Kluner et al[13] | 2006 | 16MDCT | 120 | 20 (6.9) | 1.43 | 5 | 97 | 95 | NA | 0.5-0.7 |
| Poletti et al[14] | 2007 | 4MDCT | 120 | 74 (30) | 1.25 | 5 | 86-96 | 97-100 | NA | NA |
| CT scanner | GE (64 MDCT) | Siemens (64 MDCT) |
| Scan range | Top of kidney-pubic symphysis | Top of kidney-pubic symphysis |
| Detector collimation (mm) | 64 × 0.625 | 24 × 1.2 |
| Pitch | 1.375 | 1.2 |
| Rotation time (s) | 0.5 | 0.5 |
| Kvp | 120 | 120 |
| mA | 150-450 | Reference mA = 160 |
| Noise index | 25 (30 if follow-up exam) | |
| Kernel | Standard | B31F |
| Reconstruction mode | Plus | |
| Slice thickness (mm) | 5 (2.5) | 5 (2.5) |
| Slice overlap | 5 (2.5) | 5 (2.5) |
Tube current is the most commonly adjusted scanning parameter for reducing radiation dose in CT. There is a direct linear relationship between tube current and radiation dose. Reduction of tube current by half cuts the radiation dose associated with CT by half. Tube current for dose reduction can be adjusted with the manual selection of a lower fixed tube current or with automatic exposure control.
Previous studies have reported the usefulness of low dose CT protocols with substantial reductions in tube current, which showed sensitivities and specificities close to those of standard dose CT in assessing urolithiasis[11-14]. Tack et al[11] and Poletti et al[14] evaluated low dose CT examinations using a tube current of 30 mA to decrease radiation dose for stone protocol CT. They demonstrated that low dose CT at 30 mA had 90-97% sensitivity and 94-100% specificity, similar to standard dose CT at 120 or 180 mA for correctly identifying renal stones as well as alternative diagnoses. Kluner et al[13] documented 97% sensitivity and 95% specificity for the detection of urinary calculi using an ultra low dose protocol performed at a mere 6.9 mA. Recently, Jellison et al[15] reported the use of a very low dose protocol CT performed at 7.5 mA for the detection of distal ureteral calculi in a cadaveric model, with a decrease of up to 95% in radiation dose to a level equivalent to the dose of a single kidney-ureter-bladder radiograph.
The limitation of the initial low dose CT studies using a fixed tube current was that a single lower tube current is not appropriate for obese patients with the possibility of missing an alternative clinical diagnosis because of insufficient image quality. The introduction of automatic tube current modulation techniques helps in these circumstances[16-18]. These techniques modulate tube current on the basis of the size, shape, geometry and attenuation of the body region being scanned, while preserving image quality. Three types of automatic tube current modulation methods have been described for non-cardiac CT scanning; based on projection angle-based modulations (angular or, xy-axis modulation), modulation along the longitudinal direction or along patient length (z-axis or longitudinal modulation), or in both angular positions and longitudinal directions (combined or xyz-axis modulation)[16].
Kalra et al[17] found that use of the z-axis modulation technique (Auto mA, GE Healthcare, Milwaukee, Wisconsin, USA) (noise indices of 10.5-12, 10-380 mA) resulted in a 43%-66% reduction in radiation dose without compromising stone depiction in patients undergoing follow up CT for kidney stones when compared with a previous fixed tube current (200-300 mA) technique. Mulkens et al[18] reported on the usefulness of low dose CT using a combined modulation technique (CareDose 4D, Siemens Medical Solutions, Forchheim, Germany) for the evaluation for urolithiasis, even in overweight and obese patients. In this study, low dose CT examinations (6-MDCT, 51 effective mA at 110 kV; 16-MDCT, 70 effective mA at 120 kV) had a sensitivity of 96%-99%, specificity of 92%-94%, and accuracy of 94%-95% for the detection of kidney stones with a 51%-64% reduction in radiation, compared to standard dose CT examinations (6-MDCT, 95 effective mA at 130 kV; 16-MDCT, 120 effective mA at 120 kV). The effective mA is the product of tube current and gantry rotation time divided by the pitch.
In single-detector row helical CT, as pitch increases the radiation dose decreases if all other parameters are held constant. Each reconstructed image is taken from a wider section of the patient giving equal noise at the expense of z-axis resolution. Diel et al[19] reported that increasing the pitch on unenhanced helical CT for suspected renal colic to 2.5:1 or 3.0:1 was an effective method of reducing radiation dose with high diagnostic accuracy and acceptable image quality for suspected renal colic. Modern MDCT scanners take the reconstructed image data from a fixed “slab” of the patient. As pitch is increased, fewer projections make up the image, increasing the noise. To compensate for this increase in pitch, most modern scanners automatically increase the tube current to maintain constant image noise, and therefore, a relatively constant radiation dose. Conversely, when the pitch is decreased, tube current is automatically decreased too. Most vendors also let their automatic tube current modulation techniques increase or decrease the tube current automatically according to any change in the pitch in order to maintain constant image noise and radiation dose.
Most studies on low dose CT protocols have been limited in assessing the effect of multiple levels of tube current reductions on overall diagnostic accuracy, as repeat CT images cannot be acquired in the same patient at a variety of radiation exposures due to ethical considerations. Previous studies have reported the use of a simulated dose reduction technique to obtain simulated low dose or lower tube current images at multiple dose levels in the same patient[20-23]. This technique, therefore, helps avoid repeat exposure of patients in dose-related research. Mayo et al[20] introduced the use of this technique to modify the noise and simulate reduced tube current images in single detector helical chest CT. This software operates by adding simulated noise to source raw data of CT acquisition. Frush et al[21] adopted this in abdominal CT of pediatric patients and showed that abdominal MDCT using computer-simulation techniques in the urinary tract resulted in 33%-67% reduction in radiation dose. Karmazyn et al[22] reported the usefulness of computer-simulated dose reduction techniques for determining the diagnostic threshold for MDCT detection of renal stones in children. In their study, use of the 80 mA setting for all children and 40 mA for children weighing 50 kg or less did not significantly affect the diagnosis of renal stones. Ciaschini et al[23] recently assessed the use of simulated low dose images at 100% (177 mA), 50% (88 mA), and 25% (44 mA) of the original tube current by using simulation software. These authors demonstrated sensitivities of 92%, 83%, and 67% for the 100%, 50%, and 25% tube current reconstructions, respectively, for the detection of all calculi. There was no difference between the full dose CT images and the 50% and 25% lower dose images for the detection of urinary stones greater than 3 mm. However, sensitivity for 3 mm or smaller calculi, which were deemed as not clinically important due to their high probability of spontaneous passage, was reduced in the 25% radiation dose CT images.
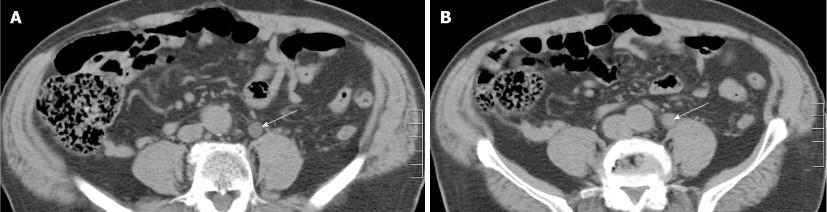
Multi-detector computed tomography urography (MDCTU) offers considerable advantages in the evaluation of the upper urinary tract compared to excretory urography due to higher contrast resolution and ability to perform high quality three dimensional rendering of the urinary tract[24]. A variety of CT urography techniques have been evaluated for producing adequate opacification of the urinary tract at the lowest radiation exposure[25-37]. Due to multiphase scanning, with some CT urography protocols patients undergoing MDCTU may receive a radiation dose as much as three or four times higher than that with a single phase abdominal CT examination. Nawfel et al[25] reported a mean effective dose of 14.8 ± 3.1 mSv with three phase MDCTU protocols, which was about 1.5 times higher than the conventional excretory urography dose of 9.7 ± 3 mSv. Table 3 summarizes the effective radiation dose for different MDCTU protocols. A two-pronged strategy is applied to reduce radiation exposure with MDCTU protocols, which includes reducing the number of acquisitions and optimizing scan parameters.
There is no consensus on the optimal protocol for MDCTU. Previous studies have reported the use of 2-4 phase scanning for MDCTU as different components of the urinary tract opacify with contrast at different time points following administration of iodinated contrast agents (Table 4). The most commonly described MDCTU protocol comprises a three-phase protocol, which typically consists of non-contrast (for the detection of hemorrhage and stones), nephrographic (for renal parenchymal evaluation), and excretory phases (for assessing the collecting system, ureters and urinary bladder). The double excretory or corticomedullary phase is optionally acquired instead of the nephrographic phase. Some studies have described acquiring arterial phase images for patients who may require surgery[31]. As some CT protocols for renal or urinary tract evaluations require acquisition of two or more scan series, they are associated with higher radiation dose. In such circumstances, modifications of the contrast injection protocol or scanning parameters may be required to reduce radiation dose. For example, for certain scan series, scan length can be reduced or confined to the most important region of interest.
| Authors | Yr | CT scanner | Acquisiton phase | kVp | mA (mAs) | Pitch | Effective dose (mSv) | Supplement |
| Standard CT urographic protocols | ||||||||
| Caoili et al[26] | 2002 | 4MDCT | Unenhanced | 120 | 150-240 | 0.75 | 25-35 | |
| Nephrographic | 100-280 | 0.75 | ||||||
| Excretory | 150-280 | 1.5 | ||||||
| Nawfel et al[25] | 2004 | 4MDCT | Unenhanced | 120 | (155-200) | 1.0-1.25 | 6.4 ± 1.3 | |
| Nephrographic | (155-200) | 1.0-1.25 | 2.5 ± 0.34 | |||||
| Excretory | (165-185) | 0.65-1.0 | 5.9 ± 1.5 | |||||
| Low dose CT urographic protocols | ||||||||
| Coppenrath et al[27] | 2006 | 4MDCT | Excretory | 90 | (15-100) | 0.875-1.75 | 0.78 (male)/1.08 (female) | |
| 16MDCT | 100 | (17-100) | 1-1.5 | 1.06-1.19 (male) | ||||
| 0.76-0.86 (female) | ||||||||
| Kemper et al[28] | 2007 | 4MDCT | Excretory | 120 | (70) | 1.25 | 2.7 (male)/4.1(female) | |
| Yanaga et al[29] | 2009 | 40MDCT | Excretory | 80 | (300) | 0.781 | 2.9 | Adaptive noise reduction filter |
| Kekelidze et al[30] | 2010 | 16MDCT | Unenhanced | 120 | (55) | 0.75 | 3.4 | AEC |
| Enhanced | (165) | 1.25 | 9.8 | Split-bolus technique | ||||
A major disadvantage of the multi-phase scanning techniques most commonly performed in many institutions is high radiation exposure as well as increased time required to interpret a large number of images. In an effort to overcome these important issues, Chai et al[32] proposed the use of a split-bolus technique that allows the reduction of radiation dose by reducing the total number of scanning phases in a single intravenous injection. The authors described the use of a small bolus of intravenous contrast medium (30 mL) after acquisition of images in the non-contrast phase. After 5 to 10 min, a larger bolus of contrast medium (100 mL, 2 mL/s) was administered and images were acquired 100 s after the administration of the second contrast bolus. This split-bolus technique allowed the combination of two phases of information, that is, the nephrographic phase from the larger second bolus and the excretory phase from the smaller initial bolus into one set of two phases. Raptopoulos et al[33] proposed a modification of the split-bolus multi-detector CT urographic approach, combining arterial and excretory phases using 30 mL of contrast material for urinary tract opacification for the excretory phase, and re-injecting 70-100 mL contrast approximately 2-3 min later and scanning for the corticomedullary phase, 60 s after the start of the last contrast injection. In our institute, this split-bolus technique is used for MDCTU (Table 5), in which a bolus of 40 mL contrast medium (Iopamidol 370 mg% Bracco Diagnostics, Princeton, NJ, USA) is injected at a rate of 3 mL/s after acquisition of images in the non-contrast phase. Then, 250 mL of saline infusion is given to the patient over 10 min. After 10 min, 80 mL of contrast medium is injected at a rate of 3 mL/s and scanning is start at administration of the second contrast medium.
| Non-contrast | Post-contrast1 | |
| Scan range | Top of kidney to base of bladder | Top of kidney to base of bladder |
| Detector collimation (mm) | 64 × 0.625 | 64 × 0.625 |
| Pitch | 1.375 | 1.375 |
| kVp | 120 | 120 |
| mA | 150-450 | 150-450 |
| Noise index | 25 (30 for follow-up exam) | 10 (< 60 kg) |
| 12.5 (61-90 kg) | ||
| 15 (> 90 kg) | ||
| Table speed (mm/rotation) | 55 | 55 |
Although split-bolus MDCTU has led to reduced scan series, this technique has been criticized as opacification of the kidneys and the urinary tract can be diminished due to the lower volumes of contrast medium used[34]. Kekelidz et al[30] recently described a triple-bolus protocol designed to combine all renal contrast-enhancement phases in a single phase post-contrast CT. The authors used a triple-bolus protocol in which 30 mL of contrast medium was administered at 0 min followed by an injection of 50 mL at 7 min, then 65 mL of contrast was injected at 8 min, with CT scanning starting at 8.5 min. In their study, triple-bolus MDCTU allowed visualization of renal parenchymal, excretory, and vascular contrast-enhancement phases in a single phase. The radiation dose for triple-bolus acquisition (9.8 mSv) was 44% less than that for conventional CT urography composed of the three-phase protocol (23.4 mSv).
A hybrid technique has also been considered to reduce radiation exposure, particularly for the excretory phase, if more than a single excretory-phase acquisition is required for complete opacification of the urinary tract. This technique is a combination of CT and conventional excretory urography or CT digital radiography during the excretory phase in a single imaging session. It requires only a single intravenous injection of contrast material for both parts of the examination with hybrid imaging techniques. CT images can be acquired after a conventional urography or, more frequently, conventional urographic images are obtained subsequent to a CT examination. Sudakoff et al[35] reported that hybrid imaging accomplished with a series of three enhanced CT digital radiography images delivers an effective radiation dose of only 1.6 mSv.
Attempts to reduce radiation dose have been proposed which modify scanning parameters for the individual phases like low dose CT protocols for the evaluation of urolithiasis[28,29]. Kemper et al[28] demonstrated that the low dose MDCTU protocol using 70 effective mA at 120 kVp can provide acceptable image quality for the excretory phase with a 64% dose reduction compared to standard dose CT in their 75-kg porcine model.
One strategy for reducing the radiation dose during MDCTU includes lowering the tube voltage. Use of low tube voltage CT reduces the radiation dose as the tube output is proportional to the square of the tube voltage. In addition, iodine attenuation increases as tube voltage decreases because the energy in the X-ray beam moves closer to the k-absorption edge of iodine. The use of low tube voltage techniques has been described for contrast-enhanced CT examinations such as CT urography and CT angiography[36,37].
However, a reduction in tube voltage also results in a large increase in image noise. Yanaga et al[29] assessed the feasibility of MDCTU using a combination of low tube voltage of 80 kVp and an adaptive noise reduction filter. In this study, the quality of post-processed filtered 80-kVp images was comparable with that of 120-kVp images for evaluation of the upper urinary tract with a 59% reduction in the mean effective dose using this technique. The authors reported that evaluation of the pelvic ureter and urinary bladder was not sufficient, and a compensatory increase in tube current is necessary to allow 80-kVp scanning. Furthermore, automatic exposure control techniques help to decrease radiation dose by 20%-45% without compromising the image quality in the abdomen and pelvis[38-40] (Figure 3).
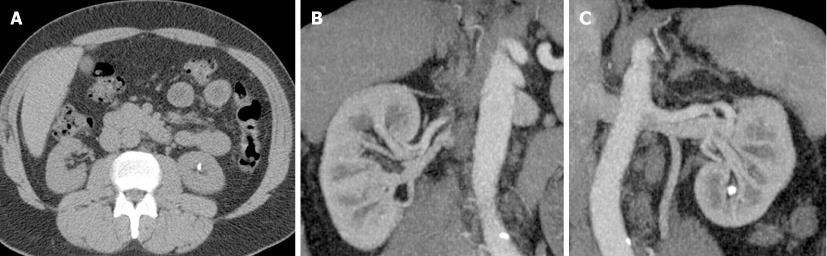
MDCT is now routinely used in the preoperative evaluation of living renal donors for transplantation. The multiphase scanning protocol usually includes non-contrast, arterial, venous and excretory phases which are generally obtained to assess renal and abdominal vasculature, and the urinary excretory tract to exclude urinary tract and retroperitoneal disorders. Given the fact that living renal donors are relatively young, “disease free and healthy” individuals, radiation dose reduction assumes a more critical dimension. Strategies for reducing radiation dose with renal donor protocol CT have been proposed for preoperative CT examinations and include a reduction in the number of acquired series or phases and use of lower kilovoltage settings[41-44]. Table 6 summarizes radiation doses for different CT protocols in the evaluation of living renal donors. The CT protocol used for living renal donors at our institute is shown in Table 7 (Figure 4).
| Author | Yr | CT scanner | Acquisition phase | kVp | mA(mAs) | Pitch | CTDIvol in mGy | DLP in mGy cm | Supplements |
| Kim et al[49] | 2003 | 4MDCT | Unenhanced | 120 | 200 | 1.5 | 10.19 | NA | |
| Renal CTA | 12.88 | NA | |||||||
| Excretory | 10.19 | NA | |||||||
| Wintersperger et al[50] | 2005 | 16MDCT | Abdominal CTA | 120 | 400 (200) | 1 | 15.6 | 673.9 | |
| 100 | 10.0 | 447.0 | |||||||
| Sahani et al[45] | 2007 | 16MDCT | Renal CTA | 140 | (210) | 0.94 | 25 ± 3 | NA | AEC |
| 120 | 17 ± 4 | NA | Using NI of 15 | ||||||
| 100 | 12 ± 3 | NA | |||||||
| Zamboni et al[42] | 2010 | 64MDCT | Low dose 4-phase | 120 | 50-150 | NA | NA | 2021 ± 545 | |
| Low dose 3-phase | NA | 1501 ± 418 | AEC | ||||||
| Low dose 2-phase | NA | 981 ± 381 | Using NI of 15.86 | ||||||
| Low dose 2-phase* | NA | 676 ± 284 |
| Unenhanced | Arterial | Excretory | |
| Scan range | Dome of liver-iliac crest | Dome of liver-iliac crest | Top of kidney-iliac crest |
| Detector collimation (mm) | 64 × 0.625 | 64 × 0.625 | 64 × 0.625 |
| Pitch | 1.375 | 1.375 | 1.375 |
| kVp | 120 | 120 | 100 |
| mA | 150-450 | 150-550 (150-800 for patient > 135 kg) | 150-450 |
| Noise index | 20 | 28 (< 60 kg) | 18 |
| 32 (61-90 kg) | |||
| 35 (> 90 kg) | |||
| Table speed (mm/rotation) | 55 | 55 | 55 |
The appropriateness of clinical indications for the multiphase renal donor protocol should be monitored closely to reduce the radiation dose. Previous studies have assessed the feasibility of reducing the number of acquired phases[41,42]. Caoili et al[26] reported a radiation dose reduction by omitting the non-contrast series or replacing the excretory phase with a localizer radiograph or an abdominal radiograph.
Namasivayam et al[41] reported that venous phase MDCT acquisition is not necessary for the evaluation of renal vein anatomy as the arterial phase can provide information on renal vein anomalies and help identify small left renal veins. Zamboni et al[42] proposed combined vascular-excretory phase imaging with a split-bolus contrast injection technique. In their study, the CT protocol was comprised of low dose non-contrast phase scanning of the abdomen and pelvis (120 kVp and 50-150 mA with the automatic exposure control technique), and a combined vascular-excretory phase after split-bolus contrast medium injection, with 50 mL of contrast material injected at 2.5 mL/s followed by a 100 mL bolus at 4-6 mL/s with bolus tracking. Arterial phase scanning of the abdomen started 5 s after CT attenuation in the abdominal aorta reached a predetermined threshold, and venous phase scanning of the abdomen and pelvis was initiated at a 20 s delay from the predetermined threshold. An additional localizer or conventional radiograph was acquired if there was an abnormality in the excretory system on the vascular phases. Namasivayam et al[43] also reported on the use of a low kilovoltage triple bolus single phase CT protocol for the evaluation of renal donors, in which non-contrast images are excluded and excretory phase images are replaced with localizer radiography acquired at 80-kVp. Furthermore, use of the arterial and venous phases is also combined into one phase acquired with differential contrast enhancement in the arteries and veins.
The presence of high inherent tissue contrast allows the use of higher background noise without affecting the diagnostic quality of the images. As described earlier, low peak kilovoltage techniques also increases iodine attenuation in vessels and consequently improve vessel conspicuity[37,44]. Based on this rationale, lower kVp values have been used in the evaluation of renal donors undergoing renal CT angiography, while decreasing the amount of iodinated contrast medium. Sahani et al[45] reported no difference in image quality between 120 and 140 kVp, whereas use of 100 kVp resulted in greater noise although with diagnostically acceptable images and substantial radiation dose reduction compared with CT at 120 or 140 kVp in the evaluation of renal donors. When the tube potential is decreased to reduce radiation dose, it may be necessary to increase the tube current to obtain acceptable image quality. On the other hand, with increased image contrast at lower tube potential, images with greater noise may be acceptable for diagnostic evaluation. A reduction in tube potential in adults, particularly in those with large body habitus, should be performed carefully because increased image noise and streak artifacts can have an adverse affect on the diagnostic acceptability of CT images.
Scan length is another important determinant of radiation dose to patients undergoing CT scanning. Larger scan length delivers radiation dose to larger areas of the body, thus increases radiation dose to patients. Radiation dose can be reduced by restricting the scan length to the region of interest, for example, scanning from the top of the kidneys instead of the top of the liver for evaluation of kidney stones or for CT urography. Scanning only the upper abdomen or the kidneys for the corticomedullary and nephrographic phases and scanning from the kidneys to the bladder for the excretory phase can help reduce radiation dose with multiphase imaging. It is also imperative that all efforts are made to determine prior scanning in order to minimize repetition of CT scanning for CT urography, and it is important to assess complete opacification and adequate distension of the collecting system combining oral or intravenous hydration, diuretics, and abdominal compression devices and ensure optimal timing of image acquisition. Likewise, appropriate triggering of CT following contrast injection is important for CT angiography in the evaluation of renal donors. In the case of non-opacification of a portion of the ureter or remaining collecting system, localizer radiography or even conventional radiography can be obtained instead of transverse CT images. In instances where repeat transverse CT images are deemed “unavoidable” or “necessary”, radiation dose should be reduced with the use of substantially smaller scanning length at reduced radiation dose.
Use of noise reduction filters to improve image quality of “noisier” images can also allow radiation dose reduction. Singh et al[46] showed that two-dimensional adaptive noise reduction filters (SharpView CT, Linkoping, Sweden) can allow 25%-30% reduction in tube current or radiation dose while maintaining the detectability of small urinary tract calculi. Similarly, recent publications on non-filtered back projection reconstruction techniques such as adaptive statistical iterative reconstruction (ASiR, GE Healthcare) allow reduced image noise and thus enable scanning at a reduced radiation dose[47,48]. At our institution, we reduce the radiation dose for patients undergoing CT scanning of the urinary tract by 30%-40% on an ASiR enable CT scanner compared to older non-ASiR capable CT equipment. Such a dose reduction is generally accomplished with the use of a 30%-40% lower tube current.
MDCT has virtually replaced conventional imaging techniques for the evaluation of urinary tract abnormalities. This is partly due to impressive improvements in CT technology which allow isotropic resolution with faster scan coverage in a single, short breath-hold, and high diagnostic performance. However, increasing use of CT necessitates the assessment, and if necessary, reduction of radiation dose. Therefore, all efforts should be made to optimize the radiation dose necessary for adequate imaging through the collaboration of all parties including the radiologist, medical physicist, technologist, and manufacturers.
Peer reviewers: Ian Negus, MSc, MIPEM, CSCI, Department of Medical Physics and Bioengineering, Bristol Heart Institute, Bristol Royal Infirmary, Bristol, BS1 6SY, United Kingdom; Mohamed Abou El-Ghar, MD, Radiology dep, Urology and Nephrology center-Mansoura University, 72 El-gomhoria st, Mansoura, 35516, Egypt; Haiquan Yang, PhD, President, Midorino Research Corporation, 5-15-13, Chuo-Rinkan-Nishi, Yamato, Kanagawa 242-0008, Japan
S- Editor Cheng JX L- Editor Webster JR E- Editor Zheng XM
| 1. | Smith RC, Rosenfield AT, Choe KA, Essenmacher KR, Verga M, Glickman MG, Lange RC. Acute flank pain: comparison of non-contrast-enhanced CT and intravenous urography. Radiology. 1995;194:789-794. [PubMed] |
| 2. | Niall O, Russell J, MacGregor R, Duncan H, Mullins J. A comparison of noncontrast computerized tomography with excretory urography in the assessment of acute flank pain. J Urol. 1999;161:534-537. [PubMed] |
| 3. | Cowan NC, Turney BW, Taylor NJ, McCarthy CL, Crew JP. Multidetector computed tomography urography for diagnosing upper urinary tract urothelial tumour. BJU Int. 2007;99:1363-1370. [PubMed] |
| 4. | Caoili EM, Cohan RH, Inampudi P, Ellis JH, Shah RB, Faerber GJ, Montie JE. MDCT urography of upper tract urothelial neoplasms. AJR Am J Roentgenol. 2005;184:1873-1881. [PubMed] |
| 5. | Leusmann DB, Niggemann H, Roth S, von Ahlen H. Recurrence rates and severity of urinary calculi. Scand J Urol Nephrol. 1995;29:279-283. [PubMed] |
| 6. | Katz SI, Saluja S, Brink JA, Forman HP. Radiation dose associated with unenhanced CT for suspected renal colic: impact of repetitive studies. AJR Am J Roentgenol. 2006;186:1120-1124. [PubMed] |
| 7. | Liu W, Esler SJ, Kenny BJ, Goh RH, Rainbow AJ, Stevenson GW. Low-dose nonenhanced helical CT of renal colic: assessment of ureteric stone detection and measurement of effective dose equivalent. Radiology. 2000;215:51-54. [PubMed] |
| 8. | Meagher T, Sukumar VP, Collingwood J, Crawley T, Schofield D, Henson J, Lakin K, Connolly D, Giles J. Low dose computed tomography in suspected acute renal colic. Clin Radiol. 2001;56:873-876. [PubMed] |
| 9. | Hamm M, Knopfle E, Wartenberg S, Wawroschek F, Weckermann D, Harzmann R. Low dose unenhanced helical computerized tomography for the evaluation of acute flank pain. J Urol. 2002;167:1687-1691. [PubMed] |
| 10. | Heneghan JP, McGuire KA, Leder RA, DeLong DM, Yoshizumi T, Nelson RC. Helical CT for nephrolithiasis and ureterolithiasis: comparison of conventional and reduced radiation-dose techniques. Radiology. 2003;229:575-580. [PubMed] |
| 11. | Tack D, Sourtzis S, Delpierre I, de Maertelaer V, Gevenois PA. Low-dose unenhanced multidetector CT of patients with suspected renal colic. AJR Am J Roentgenol. 2003;180:305-311. [PubMed] |
| 12. | Knöpfle E, Hamm M, Wartenberg S, Bohndorf K. [CT in ureterolithiasis with a radiation dose equal to intravenous urography: results in 209 patients]. Rofo. 2003;175:1667-1672. [PubMed] |
| 13. | Kluner C, Hein PA, Gralla O, Hein E, Hamm B, Romano V, Rogalla P. Does ultra-low-dose CT with a radiation dose equivalent to that of KUB suffice to detect renal and ureteral calculi? J Comput Assist Tomogr. 2006;30:44-50. [PubMed] |
| 14. | Poletti PA, Platon A, Rutschmann OT, Schmidlin FR, Iselin CE, Becker CD. Low-dose versus standard-dose CT protocol in patients with clinically suspected renal colic. AJR Am J Roentgenol. 2007;188:927-933. [PubMed] |
| 15. | Jellison FC, Smith JC, Heldt JP, Spengler NM, Nicolay LI, Ruckle HC, Koning JL, Millard WW, Jin DH, Baldwin DD. Effect of low dose radiation computerized tomography protocols on distal ureteral calculus detection. J Urol. 2009;182:2762-2767. [PubMed] |
| 16. | Kalra MK, Maher MM, Toth TL, Hamberg LM, Blake MA, Shepard JA, Saini S. Strategies for CT radiation dose optimization. Radiology. 2004;230:619-628. [PubMed] |
| 17. | Kalra MK, Maher MM, D'Souza RV, Rizzo S, Halpern EF, Blake MA, Saini S. Detection of urinary tract stones at low-radiation-dose CT with z-axis automatic tube current modulation: phantom and clinical studies. Radiology. 2005;235:523-529. [PubMed] |
| 18. | Mulkens TH, Daineffe S, De Wijngaert R, Bellinck P, Leonard A, Smet G, Termote JL. Urinary stone disease: comparison of standard-dose and low-dose with 4D MDCT tube current modulation. AJR Am J Roentgenol. 2007;188:553-562. [PubMed] |
| 19. | Diel J, Perlmutter S, Venkataramanan N, Mueller R, Lane MJ, Katz DS. Unenhanced helical CT using increased pitch for suspected renal colic: an effective technique for radiation dose reduction? J Comput Assist Tomogr. 2000;24:795-801. [PubMed] |
| 20. | Mayo JR, Whittall KP, Leung AN, Hartman TE, Park CS, Primack SL, Chambers GK, Limkeman MK, Toth TL, Fox SH. Simulated dose reduction in conventional chest CT: validation study. Radiology. 1997;202:453-457. [PubMed] |
| 21. | Frush DP, Slack CC, Hollingsworth CL, Bisset GS, Donnelly LF, Hsieh J, Lavin-Wensell T, Mayo JR. Computer-simulated radiation dose reduction for abdominal multidetector CT of pediatric patients. AJR Am J Roentgenol. 2002;179:1107-1113. [PubMed] |
| 22. | Karmazyn B, Frush DP, Applegate KE, Maxfield C, Cohen MD, Jones RP. CT with a computer-simulated dose reduction technique for detection of pediatric nephroureterolithiasis: comparison of standard and reduced radiation doses. AJR Am J Roentgenol. 2009;192:143-149. [PubMed] |
| 23. | Ciaschini MW, Remer EM, Baker ME, Lieber M, Herts BR. Urinary calculi: radiation dose reduction of 50% and 75% at CT--effect on sensitivity. Radiology. 2009;251:105-111. [PubMed] |
| 24. | Dillman JR, Caoili EM, Cohan RH. Multi-detector CT urography: a one-stop renal and urinary tract imaging modality. Abdom Imaging. 2007;32:519-529. [PubMed] |
| 25. | Nawfel RD, Judy PF, Schleipman AR, Silverman SG. Patient radiation dose at CT urography and conventional urography. Radiology. 2004;232:126-132. [PubMed] |
| 26. | Caoili EM, Cohan RH, Korobkin M, Platt JF, Francis IR, Faerber GJ, Montie JE, Ellis JH. Urinary tract abnormalities: initial experience with multi-detector row CT urography. Radiology. 2002;222:353-360. [PubMed] |
| 27. | Coppenrath E, Meindl T, Herzog P, Khalil R, Mueller-Lisse U, Krenn L, Reiser M, Mueller-Lisse UG. Dose reduction in multidetector CT of the urinary tract. Studies in a phantom model. Eur Radiol. 2006;16:1982-1989. [PubMed] |
| 28. | Kemper J, Regier M, Bansmann PM, Begemann PG, Stork A, Nagel HD, Adam G, Nolte-Ernsting C. Multidetector CT urography: experimental analysis of radiation dose reduction in an animal model. Eur Radiol. 2007;17:2318-2324. [PubMed] |
| 29. | Yanaga Y, Awai K, Funama Y, Nakaura T, Hirai T, Roux S, Yamashita Y. Low-dose MDCT urography: feasibility study of low-tube-voltage technique and adaptive noise reduction filter. AJR Am J Roentgenol. 2009;193:W220-W229. [PubMed] |
| 30. | Kekelidze M, Dwarkasing RS, Dijkshoorn ML, Sikorska K, Verhagen PC, Krestin GP. Kidney and urinary tract imaging: triple-bolus multidetector CT urography as a one-stop shop--protocol design, opacification, and image quality analysis. Radiology. 2010;255:508-516. [PubMed] |
| 31. | Lang EK, Macchia RJ, Thomas R, Watson RA, Marberger M, Lechner G, Gayle B, Richter F. Improved detection of renal pathologic features on multiphasic helical CT compared with IVU in patients presenting with microscopic hematuria. Urology. 2003;61:528-532. [PubMed] |
| 32. | Chai RY, Jhaveri K, Saini S, Hahn PF, Nichols S, Mueller PR. Comprehensive evaluation of patients with haematuria on multi-slice computed tomography scanner: protocol design and preliminary observations. Australas Radiol. 2001;45:536-538. [PubMed] |
| 33. | Raptopoulos V, McNamara A. Improved pelvicalyceal visualization with multidetector computed tomography urography; comparison with helical computed tomography. Eur Radiol. 2005;15:1834-1840. [PubMed] |
| 34. | Silverman SG, Leyendecker JR, Amis ES. What is the current role of CT urography and MR urography in the evaluation of the urinary tract? Radiology. 2009;250:309-323. [PubMed] |
| 35. | Sudakoff GS, Guralnick M, Langenstroer P, Foley WD, Cihlar KL, Shakespear JS, See WA. CT urography of urinary diversions with enhanced CT digital radiography: preliminary experience. AJR Am J Roentgenol. 2005;184:131-138. [PubMed] |
| 36. | Nakayama Y, Awai K, Funama Y, Hatemura M, Imuta M, Nakaura T, Ryu D, Morishita S, Sultana S, Sato N. Abdominal CT with low tube voltage: preliminary observations about radiation dose, contrast enhancement, image quality, and noise. Radiology. 2005;237:945-951. [PubMed] |
| 37. | Nakayama Y, Awai K, Funama Y, Liu D, Nakaura T, Tamura Y, Yamashita Y. Lower tube voltage reduces contrast material and radiation doses on 16-MDCT aortography. AJR Am J Roentgenol. 2006;187:W490-W497. [PubMed] |
| 38. | Greess H, Nömayr A, Wolf H, Baum U, Lell M, Böwing B, Kalender W, Bautz WA. Dose reduction in CT examination of children by an attenuation-based on-line modulation of tube current (CARE Dose). Eur Radiol. 2002;12:1571-1576. [PubMed] |
| 39. | Rizzo S, Kalra M, Schmidt B, Dalal T, Suess C, Flohr T, Blake M, Saini S. Comparison of angular and combined automatic tube current modulation techniques with constant tube current CT of the abdomen and pelvis. AJR Am J Roentgenol. 2006;186:673-679. [PubMed] |
| 40. | Kalra MK, Maher MM, Toth TL, Kamath RS, Halpern EF, Saini S. Comparison of Z-axis automatic tube current modulation technique with fixed tube current CT scanning of abdomen and pelvis. Radiology. 2004;232:347-353. [PubMed] |
| 41. | Namasivayam S, Kalra MK, Waldrop SM, Mittal PK, Small WC. Multidetector row CT angiography of living related renal donors: is there a need for venous phase imaging? Eur J Radiol. 2006;59:442-452. [PubMed] |
| 42. | Zamboni GA, Romero JY, Raptopoulos VD. Combined vascular-excretory phase MDCT angiography in the preoperative evaluation of renal donors. AJR Am J Roentgenol. 2010;194:145-150. [PubMed] |
| 43. | Namasivayam S, Kalra M, Waldrop S, Sahani D, Small W. Single phase mesenteric MDCT angiography using a split-bolus contrast injection technique: comparison with biphasic MDCT protocol using single bolus contrast injection. Available from: http://rsna2006.rsna.org/rsna2006/V2006/conference/event_display.cfm?em_id=4440796. |
| 44. | Ertl-Wagner BB, Hoffmann RT, Bruning R, Herrmann K, Snyder B, Blume JD, Reiser MF. Multi-detector row CT angiography of the brain at various kilovoltage settings. Radiology. 2004;231:528-535. [PubMed] |
| 45. | Sahani DV, Kalva SP, Hahn PF, Saini S. 16-MDCT angiography in living kidney donors at various tube potentials: impact on image quality and radiation dose. AJR Am J Roentgenol. 2007;188:115-120. [PubMed] |
| 46. | Singh S, Kalra M, Westra S, Moore M. Can adaptive filters help reduce radiation dose for follow-up chest and abdominal CT in children? Available from: http://rsna2008.rsna.org/event_display.cfm?em_id=6016172. |
| 47. | Singh S, Kalra MK, Hsieh J, Licato PE, Do S, Pien HH, Blake MA. Abdominal CT: comparison of adaptive statistical iterative and filtered back projection reconstruction techniques. Radiology. 2010;257:373-383. [PubMed] |
| 48. | Singh S, Kalra MK, Gilman MD, Hsieh J, Pien HH, Digumarthy SR, Shepard JA. Adaptive statistical iterative reconstruction technique for radiation dose reduction in chest CT: a pilot study. Radiology. 2011;259:565-573. [PubMed] |
| 49. | Kim JK, Park SY, Kim HJ, Kim CS, Ahn HJ, Ahn TY, Cho KS. Living donor kidneys: usefulness of multi-detector row CT for comprehensive evaluation. Radiology. 2003;229:869-876. [PubMed] |
| 50. | Wintersperger B, Jakobs T, Herzog P, Schaller S, Nikolaou K, Suess C, Weber C, Reiser M, Becker C. Aorto-iliac multidetector-row CT angiography with low kV settings: improved vessel enhancement and simultaneous reduction of radiation dose. Eur Radiol. 2005;15:334-341. [PubMed] |