Published online Jun 28, 2025. doi: 10.4329/wjr.v17.i6.105632
Revised: March 30, 2025
Accepted: May 21, 2025
Published online: June 28, 2025
Processing time: 138 Days and 3.8 Hours
Lower abdominal pain presents as a common complaint with diverse etiologies ranging from benign conditions to surgical emergencies. Computed tomography (CT) imaging has become instrumental in accurate diagnosis and management planning, though clinicians must carefully balance its benefits against radiation exposure concerns and resource allocation constraints.
To comprehensively evaluate the diagnostic accuracy, utility and clinical impli
This retrospective review included 230 patients who underwent CT scans for acute lower abdominal pain at Juntendo University Shizuoka Hospital throughout 2014. CT findings were systematically correlated with the final clinical diagnoses. Cases with diagnostic uncertain underwent independent reviewed by two expe
Idiopathic pain was the most common diagnosis (104 cases, 45.2%), followed by appendicitis (46 cases, 20.0%) and diverticulitis (27 cases, 11.7%). Right lower qua
CT significantly aids in the diagnosis of lower abdominal pain, especially given limited access to ultrasonography and MRI during emergency hours in Japan. Awareness of the anatomical variations and pregnancy-related con
Core Tip: This study highlights computed tomography (CT) as the primary imaging modality for diagnosing acute lower abdominal pain, especially in emergency settings with limited availability of ultrasonography and magnetic resonance ima
- Citation: Asahi K. Retrospective analysis of computed tomography examinations in patients with lower abdominal pain: A single-center experience. World J Radiol 2025; 17(6): 105632
- URL: https://www.wjgnet.com/1949-8470/full/v17/i6/105632.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i6.105632
Acute lower abdominal pain is a frequent emergency presentation, with diagnoses ranging from benign gastrointestinal issues to surgical emergencies. Accurate diagnosis is essential to minimize complications[1]. Computed tomography (CT) remains preferred for acute abdominal pain owing to its high sensitivity and specificity, yet concerns about radiation exposure persist[2,3]. Japanese emergency settings face challenges in utilizing ultrasonography (US) due to a shortage of trained personnel and limited access after-hours[4]. Although point-of-care US is promising, its adoption is limited to Japanese hospitals[5]. Magnetic resonance imaging (MRI) is rarely practical for urgent abdominal imaging because of its lengthy examination times, limited availability, and technical constraints during emergencies[6]. This study assessed the performance of CT in diagnosing acute lower abdominal pain, focusing on rare anatomical variations, pregnancy-related conditions, and practical imaging strategies.
This retrospective study reviewed 230 patients who underwent CT for lower abdominal pain at the Juntendo University Shizuoka Hospital during 2014. Clinical records and CT reports were analyzed. CT was performed using a GE Discovery CT750 HD with standardized contrast protocols tailored to renal function. The decision to perform contrast-enhanced CT and arterial-phase imaging was made by the attending emergency physician. Contrast-enhanced scans were typically acquired in the portal venous phase (90-120 seconds post injection). Arterial phase imaging (30-45 seconds post-injection or the SmartPrep technique) was performed in selected cases. The contrast media included Iopamiron 300/370 (Bayer), Omnipaque 300 (Daiichi Sankyo), and Optiray 320 (Mallinckrodt), with standard doses of 520-600 mg I/kg, adjusted according to body weight and renal function. Equilibrium-phase images were captured approximately 100 seconds post-injection. Additional imaging was performed in hemodynamically unstable patients. The diagnostic accuracy was veri
Pain distribution and CT usage: (1) Right lower quadrant: 94 patients (40.9%); contrast-enhanced CT: 79 (84.0%); (2) Left lower quadrant: 58 patients (25.2%); contrast-enhanced CT: 40 (69.0%); and (3) Nonspecific lower abdomen: 78 cases (33.9%); contrast-enhanced CT: 51 cases (65.4%).
Idiopathic pain was the most common diagnosis, with 40 cases (43%) of right lower limb pain, 29 cases (50%) of left lower quadrant pain, and 35 cases (45%) of nonspecific lower abdominal pain. Appendicitis was prominent in the right lower quadrant (19 patients, 20%), whereas diverticulitis was prevalent in the left lower extremity (3 patients, 5%). Other diagnoses included ileocecal inflammation, ischemic colitis, ileus, colonic malignancies, mesenteric lymphadenitis, ente
| Diagnosis | Right lower pain (n = 94) | Left lower pain (n = 58) | Lower abdominal pain (n = 78) |
| Idiopathic pain | 40 (43) | 29 (50) | 35 (45) |
| Appendicitis | 19 (20) | 2 (3) | 2 (3) |
| Diverticulitis | 11 (12) | 3 (5) | 3 (5) |
| Ileocecal inflammation | 6 (6) | - | 2 (3) |
| Ischemic colitis | - | 2 (4) | 1 (1) |
| Ileus | 2 (2) | 1 (2) | 4 (2) |
| Colonic malignancies | 2 (2) | 1 (2) | 1 (2) |
| Mesenteric lymphadenitis | - | 1 (2) | 2 (3) |
| Enteritis | - | - | 4 (5) |
| Chronic constipation | - | - | 2 (3) |
| Urological conditions | 10 (11) | 10 (17) | 10 (17) |
| Gynecological emergencies | 2 (2) | 6 (10) | 5 (6) |
| Intraperitoneal abscess | - | - | 2 (4) |
| Abdominal wall hernia | - | 1 (2) | 1 (1) |
| Ascites of unknown origin | - | - | 1 (1) |
| Advanced gastric cancer | - | - | 1 (1) |
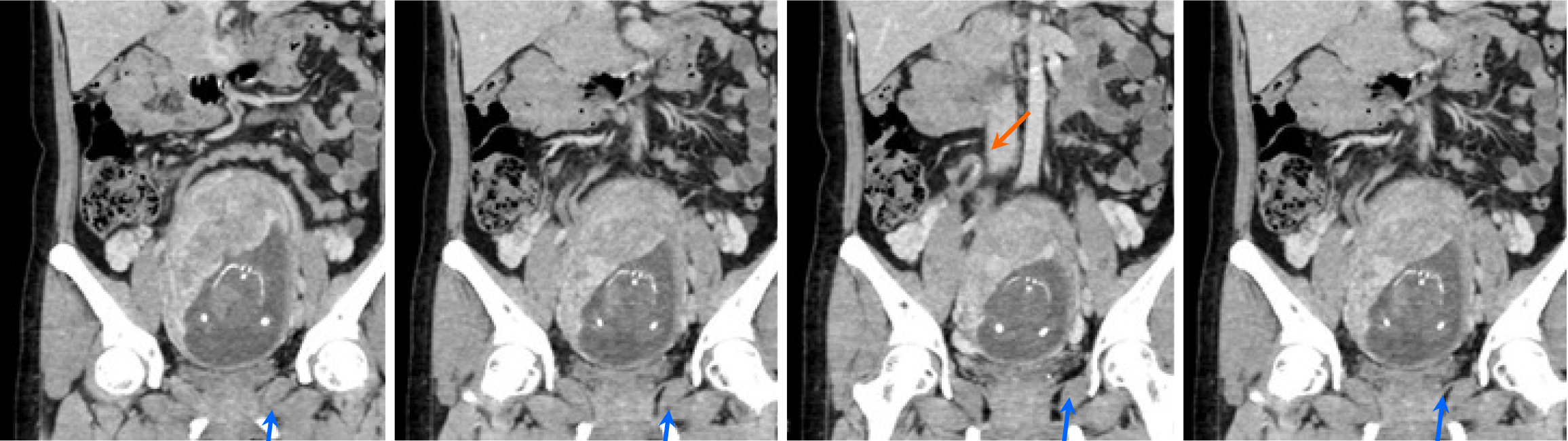
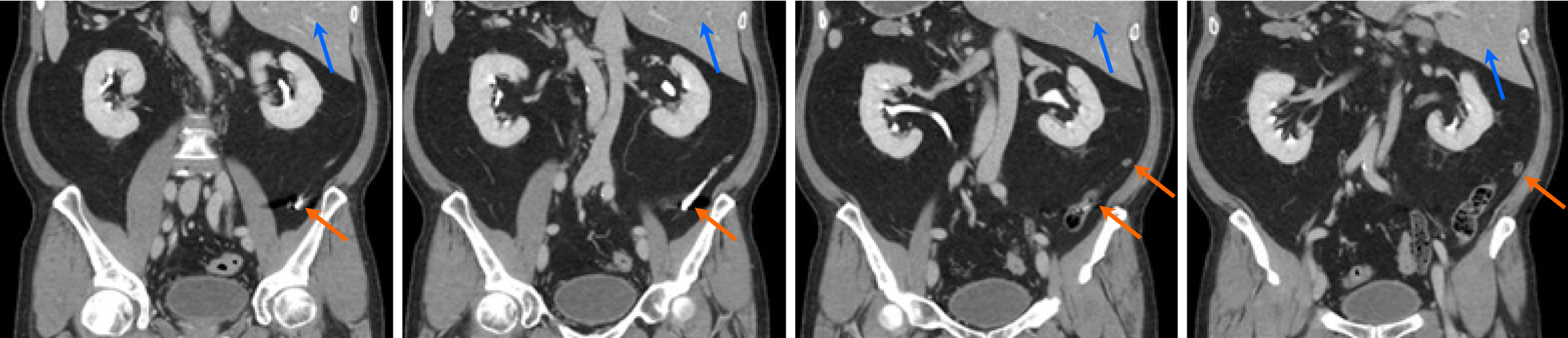
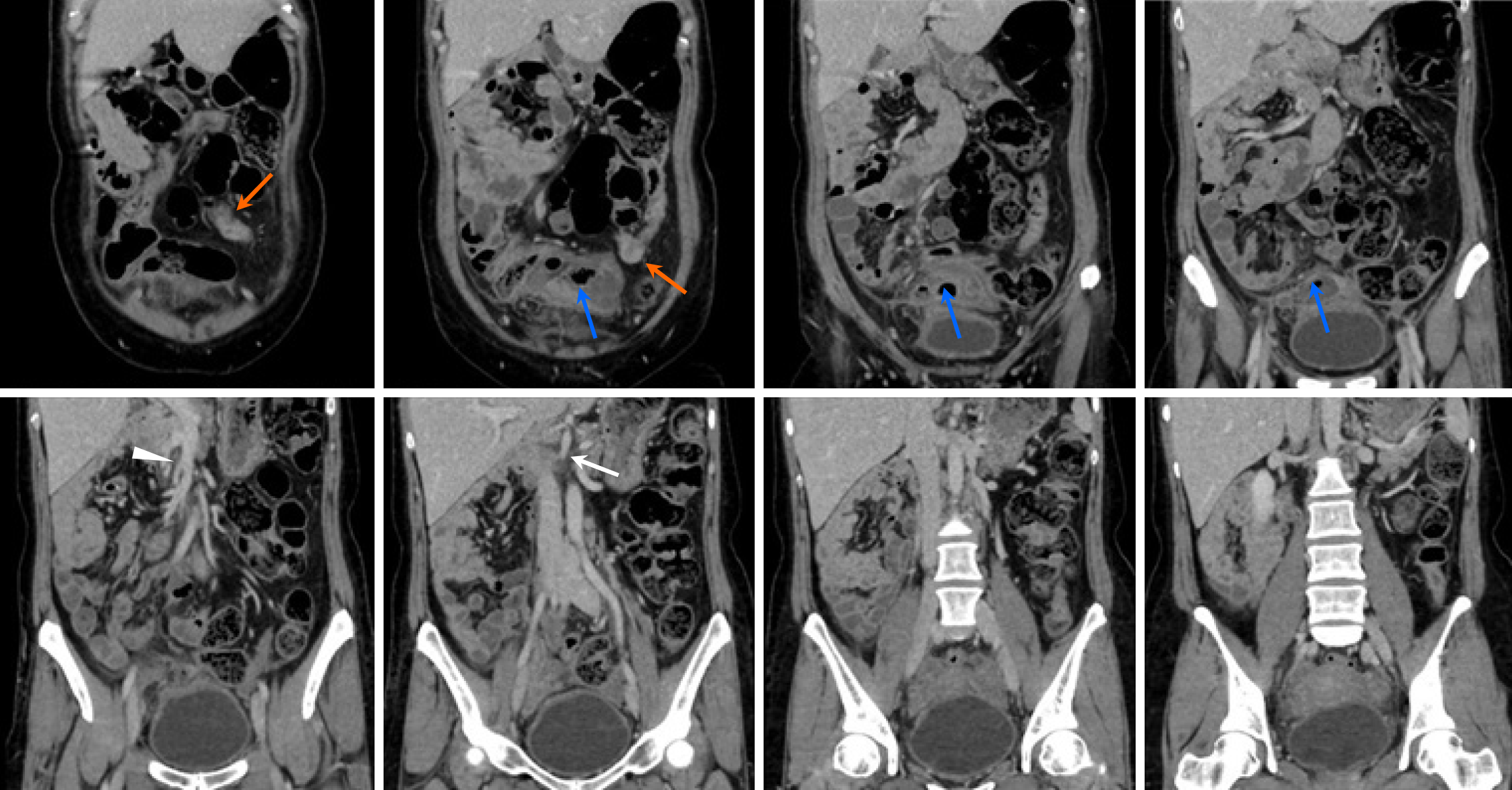
Rare anatomical variations identified: (1) Appendicitis in pregnancy (1 case): Mild inflammation in a pregnant patient (19 weeks) (Figure 1); (2) Situs inversus (1 case): Complete visceral inversion with appendicitis (Figure 2); and (3) Intestinal malrotation (1 case): Abnormal vascular positioning with appendicitis and abscess (Figure 3).
CT consistently demonstrated high diagnostic for acute lower abdominal pain evaluation, strongly corroborating pre
This single-center retrospective study has limited generalizability. The high prevalence of idiopathic pain suggests the potential overuse of CT; however, practical constraints on US and MRI justify this usage pattern in Japan.
CT is essential for evaluating acute lower abdominal pain, particularly considering the limitations of alternative moda
| 1. | Cartwright SL, Knudson MP. Evaluation of acute abdominal pain in adults. Am Fam Physician. 2008;77:971-978. [PubMed] |
| 2. | Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de González A, Miglioretti DL. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169:2078-2086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1844] [Cited by in RCA: 1715] [Article Influence: 107.2] [Reference Citation Analysis (0)] |
| 3. | Stoker J, van Randen A, Laméris W, Boermeester MA. Imaging patients with acute abdominal pain. Radiology. 2009;253:31-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 220] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 4. | Kameda T, Taniguchi N. Overview of point-of-care abdominal ultrasound in emergency and critical care. J Intensive Care. 2016;4:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 5. | Yamada T, Soni NJ, Minami T, Kitano Y, Yoshino S, Mabuchi S, Hashimoto M. Facilitators, barriers, and changes in POCUS use: longitudinal follow-up after participation in a national point-of-care ultrasound training course in Japan. Ultrasound J. 2024;16:34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 6. | Singh A, Danrad R, Hahn PF, Blake MA, Mueller PR, Novelline RA. MR imaging of the acute abdomen and pelvis: acute appendicitis and beyond. Radiographics. 2007;27:1419-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 78] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Raman SS, Osuagwu FC, Kadell B, Cryer H, Sayre J, Lu DS. Effect of CT on false positive diagnosis of appendicitis and perforation. N Engl J Med. 2008;358:972-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med. 2011;154:789-796, W. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 9. | Pinto Leite N, Pereira JM, Cunha R, Pinto P, Sirlin C. CT evaluation of appendicitis and its complications: imaging techniques and key diagnostic findings. AJR Am J Roentgenol. 2005;185:406-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 148] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 10. | Móré D, Erdmann S, Bischoff A, Wagner V, Kauczor HU, Liesenfeld LF, Abbasi Dezfouli K, Giannakis A, Klauß M, Mayer P. Comparison of Non-Contrast CT vs. Contrast-Enhanced CT with Both Intravenous and Rectal Contrast Application for Diagnosis of Acute Colonic Diverticulitis: A Multireader, Retrospective Single-Center Study. Diagnostics (Basel). 2024;15:29. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, Babyn PS, Dick PT. US or CT for Diagnosis of Appendicitis in Children and Adults? A Meta-Analysis. Radiology. 2006;241:83-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 475] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 12. | Yun SJ, Ryu CW, Choi NY, Kim HC, Oh JY, Yang DM. Comparison of Low- and Standard-Dose CT for the Diagnosis of Acute Appendicitis: A Meta-Analysis. AJR Am J Roentgenol. 2017;208:W198-W207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 13. | Patel SJ, Reede DL, Katz DS, Subramaniam R, Amorosa JK. Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose considerations. Radiographics. 2007;27:1705-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 265] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 14. | Akbulut S, Ulku A, Senol A, Tas M, Yagmur Y. Left-sided appendicitis: review of 95 published cases and a case report. World J Gastroenterol. 2010;16:5598-5602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 71] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (1)] |