Published online Aug 28, 2020. doi: 10.4329/wjr.v12.i8.156
Peer-review started: March 28, 2020
First decision: April 22, 2020
Revised: April 30, 2020
Accepted: July 18, 2020
Article in press: July 18, 2020
Published online: August 28, 2020
Processing time: 148 Days and 24 Hours
Kidney transplantation (KT) is an effective treatment for end-stage renal disease. Despite their rate has reduced over time, post-transplant complications still represent a major clinical problem because of the associated risk of graft failure and loss. Thus, post-KT complications should be diagnosed and treated promptly. Imaging plays a pivotal role in this setting. Grayscale ultrasound (US) with color Doppler analysis is the first-line imaging modality for assessing complications, although many findings lack specificity. When performed by experienced operators, contrast-enhanced US (CEUS) has been advocated as a safe and fast tool to improve the accuracy of US. Also, when performing CEUS there is potentially no need for further imaging, such as contrast-enhanced computed tomography or magnetic resonance imaging, which are often contraindicated in recipients with impaired renal function. This technique is also portable to patients’ bedside, thus having the potential of maximizing the cost-effectiveness of the whole diagnostic process. Finally, the use of blood-pool contrast agents allows translating information on graft microvasculature into time-intensity curves, and in turn quantitative perfusion indexes. Quantitative analysis is under evaluation as a tool to diagnose rejection or other causes of graft dysfunction. In this paper, we review and illustrate the indications to CEUS in the post-KT setting, as well as the main CEUS findings that can help establishing the diagnosis and planning the most adequate treatment.
Core tip: Contrast-enhanced ultrasound (CEUS) allows an accurate assessment of renal graft status. When the examination is performed by experienced operators, CEUS is a fast and safe technique that can complement ultrasound even at patients’ bedside. This can maximize the cost-effectiveness and speed of the diagnostic process in patients in whom computed tomography or magnetic resonance imaging are contraindicated due to impaired renal function. CEUS is able to exploit main vascular, urological, and parenchymal complications, improving the diagnostic performance of grayscale ultrasound and color Doppler examination.
- Citation: Como G, Da Re J, Adani GL, Zuiani C, Girometti R. Role for contrast-enhanced ultrasound in assessing complications after kidney transplant. World J Radiol 2020; 12(8): 156-171
- URL: https://www.wjgnet.com/1949-8470/full/v12/i8/156.htm
- DOI: https://dx.doi.org/10.4329/wjr.v12.i8.156
Kidney transplantation (KT) is an effective treatment for end-stage renal disease (ESRD), having the potential of reducing mortality and improving the quality of life as compared to chronic dialysis[1]. Despite the improvements in surgical techniques and immunosuppression regimens occurred over the last decades, post-transplant complications still represent a major clinical issue in KT recipients[2]. Thus, early diagnosis of complications is of paramount importance in improving patients’ outcomes.
Ultrasound (US) with color Doppler analysis has become the preferred imaging tool to evaluate the graft status within the first 24 h after KT[3]. Together with serial biopsies of the allograft parenchyma, this technique plays also a pivotal role in post-KT surveillance, aiming to diagnose post-surgical complications, acute rejection, or chronic allograft nephropathy[3,4]. On the other hand, color Doppler US is characterized by a low specificity, with Doppler-derived measures, such as the resistance index (RI), not directly reflecting the status of microcirculation[5]. Computed tomography (CT) and magnetic resonance imaging (MRI) represent second-line imaging modalities used for assessing inconclusive US findings, providing a panoramic representation of vascular complications, and characterizing perirenal collections or renal masses[3]. However, those modalities are rarely used because of the need to administer contrast medium, which is nephrotoxic in the case of CT, and at risk of raising gadolinium-related safety issues when MRI is planned in patients with impaired renal function.
Contrast-enhanced ultrasound (CEUS) is gaining ever-increasing acceptance as a complement to color Doppler US in the KT setting. In subspecialized centers, this technique is used to assess the graft status after KT due to its portability, safety profile of US contrast agents (UCAs), rapidity of execution, and diagnostic accuracy. Indeed, CEUS allows the evaluation of both macro- and micro-circulation, as well as perirenal collections or parenchymal abnormalities such as those related to rejection, acute tubular necrosis (ATN), impaired perfusion, and focal lesions[4]. CEUS candidates as the ideal first-line examination to screen for post-KT complications and to refer positive patients to prompt intervention.
In this review, we present CEUS technique in brief, KT-related advantages and disadvantages of this tool, and its potential applications in KT recipients in the postoperative period.
The current standard for UCAs is represented by second-generation compounds, consisting of a phospholipidic or albumin shell containing microbubbles of an inert lipophilic gas, such as sulfur hexafluoride [SonoVue©/Lumason© (Bracco, Milan, Italy)], perfluorocarbons [e.g., Definity©/Luminity© (Lantheus Medical Imaging, North Billerica, MA, United States) or Optison© (GE Healthcare, Oslo, Norway)][6]. UCAs used in the KT setting are administered intravenously and show blood-pool pharmacokinetics, i.e., they last in the intravascular compartment for some minutes before dissolving (the gas is excreted through the lungs, while the bio-compatible shell is metabolized by the liver)[7].
After preliminary B-mode and color Doppler evaluation, CEUS is performed with a bolus injection of contrast through a ≥ 20 Gauge catheter inserted in the antecubital vein of the arm. On average, we used a per-injection dose of 1.8 mL of Sonovue© for KT-related applications, followed by a 5-10 mL saline flush. CEUS requires a specific contrast imaging mode to avoid microbubbles being destroyed by excessive acoustic power, e.g., by setting a low mechanical index[8].
The following post-contrast phases can be observed[9]: (1) Corticomedullary phase, characterized by an increased contrast between enhancing cortex and still hypoperfused medulla, lasting between 15 and 30 s after injection; and (2) Nephrographic phase, showing an homogeneous enhancement across the cortex and medulla, lasting between 30 and 70 s after injection. Imaging performed after > 70 s from contrast injection is referred to as delayed phase. Of note, there is no urographic phase, since UCAs are not excreted by the kidney.
If planning to use CEUS, one should consider the related advantages and disadvantages in order to forecast the expected results in the KT scenario.
CEUS is portable near the patient’s bedside, thus avoiding transporting critically ill patients from the intensive care unit to the radiology department. The examination of the transplanted kidney in the iliac fossa can be performed rapidly and without the need for respiratory collaboration. This is an advantage compared to more time-consuming imaging procedures, especially MRI, and can translate into a decreased rate of low image quality examinations.
Contrary to contrast-enhanced CT or MRI, in which the acquisition is performed at definite time-points, CEUS provides a real-time representation of contrast distribution, with the possibility of recording the whole process under the form of dynamic cine-loop. Real-time acquisition allows a correct representation of the corticomedullary phase in all examinations, independently from the patient’s hemodynamic status, without the need for bolus tracking. Continuous data acquisition can be also translated into time-intensity curves (TIC) plotting contrast enhancement intensity versus time, which in turn are the base for extracting quantitative indexes of perfusion with the proper software[10].
UCAs have a favorable safety profile, as demonstrated by a 0.009% rate of major adverse reactions, a rate lower than that reported for CT and comparable to that of MRI contrast agents[11]. Compared to CT, CEUS determines no radiation exposure, especially in case of repeated examinations, and avoids potential nephrotoxic effects of iodinate contrast agents[12]. This is of special importance during the postoperative recovery of renal function, as well as in the follow-up of patients with chronic graft dysfunction. Compared to gadolinium-based contrast agents, UCAs can be administered without the risk of retention or accumulation in the central nervous system or other tissues, as potentially relevant for patients receiving multiple examinations over time. UCAs can be also administered in the case of a glomerular filtration rate < 30 mL/min, which currently represents the threshold for caution in administering MRI contrast agents, given the risk of systemic nephrogenic fibrosis[13]. A robust safety profile translates into the possibility of performing multiple contrast injections within the same examination session. This allows for a better characterization of abnormal findings and/or the evaluation of more than one finding at a time. Differently from the liver or spleen, in which there is late contrast accumulation of UCAs in the sinusoids, in the kidney contrast enhancement decreases with decreasing microbubble blood concentrations[14]. This is of help when performing multiple injections while avoiding interpretative pitfalls related to late UCAs accumulation.
In other clinical scenarios (e.g., assessment of focal liver lesions)[15,16], CEUS has been advocated as a tool to improve the speed and cost-effectiveness of the diagnostic process. One might expect a similar role for CEUS in other abdominopelvic indications, including the KT-related ones.
Similar to grayscale US, the image quality of CEUS can be impaired by patient-related factors, such as presence of bowel gas, large body habitus, or limited cooperation and physical obstacles in the early postoperative period (wounds or surgical bandage). It should be pointed out that those factors are of less impact on image quality than in other body districts, since the renal graft is usually placed extraperitoneally into the right or left iliac fossa[4], i.e., in a superficial and fixed position making the graft easily accessible by US waves.
CEUS requires skilled operators, with adequate knowledge of the examination technique, UCAs characteristics, post-surgical anatomy, and patterns of presentation of KT-related complications[14]. Previous experience in US and color Doppler examinations are a pre-requisite to achieve those goals and perform proper training with CEUS[17].
CEUS is less panoramic than CT and MRI. While this is not a limitation per se when examining one single renal graft, it can make the evaluation of patients with multiple organ transplantations more difficult (e.g., dual kidney transplant or combined liver and kidney transplant). In those cases, multiple contrast injections are required, thus increasing the examination time because of the delay needed to wait for microbubbles to disappear between the injections.
Lastly, there are some CEUS-specific artifacts that can affect image quality and interpretation[8]. Operators should be aware of potential interpretative pitfalls and the technical adjustments needed to minimize their occurrence.
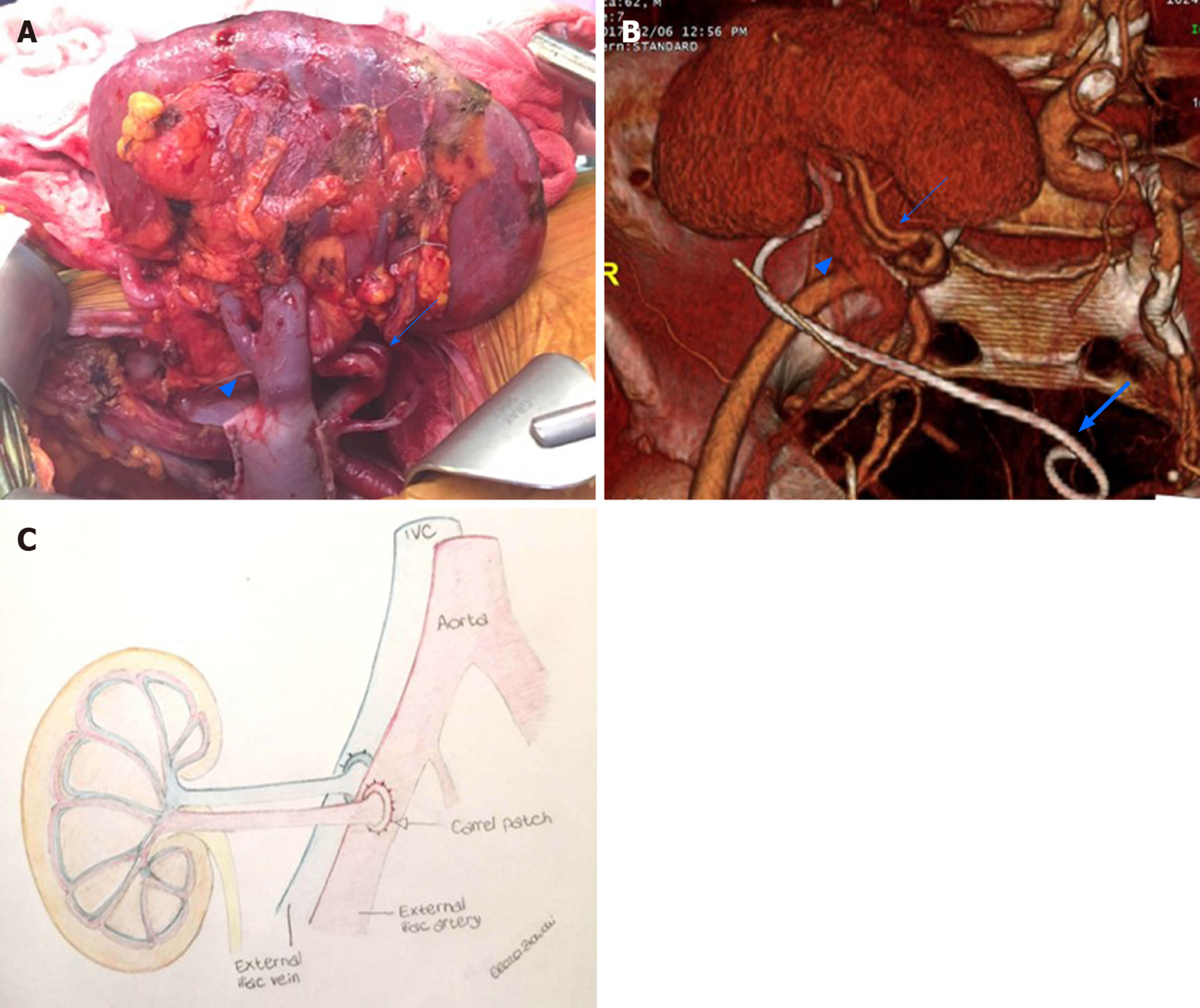
Knowledge of post-transplant anatomy is of paramount importance to interpret CEUS findings (Figure 1). Cadaveric renal graft is usually placed in the extraperitoneal space in the right iliac fossa. The left iliac fossa can be chosen in case of previous surgery on the right side or an atheromatous burden of left arterial axis carrying the risk of suboptimal graft vascularization[4]. The left-sided kidney is the preferred one for living-donor KT because of the longer renal vein, which reduces the risk of postoperative thrombosis. When a dual transplant is planned, both kidneys are usually placed in the same renal fossa.
Arterial anatomy varies depending on the transplant type. In cadaveric KT, the transplanted renal artery (TRA) is linked to a an oval portion of the donor’s aorta surrounding the renal ostium (aortic patch), which is in turn anastomosed with the recipient external iliac artery in an end-to-side fashion[4] (Figure 1). This aortic cuff increases the surface of vascular anastomosis, thus reducing the risk for strictures or thrombosis. In living-donor KT, there is a direct end-to-side anastomosis between the TRA and external iliac artery. The iliac internal artery can be the site of anastomosis if the external iliac artery is athermanous or has been used for a previous transplant. In case of accessory renal arteries, a variety of surgical techniques can be used, such as performing multiple individual anastomoses or harvesting a larger aortic patch including the origin of any accessory artery.
The transplanted renal vein (TRV) is normally anastomosed with the external iliac vein in an end-to-side approach. Urinary drainage is obtained by performing ureteroneocystostomy, usually with an anti-reflux technique (e.g., by tunneling the ureter into the bladder dome). For a variable period of time (e.g., one month in our center), a temporary stent is left in place to prevent ureteral strictures or urinary leakage.
The European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) recommends using CEUS to rule out vascular complications, inflammatory complications, and different post-KT parenchymal abnormalities, including renal lesions[17]. CEUS is recommended as an extension of preliminary grayscale US and color Doppler to be interpreted in light of the overall clinical picture and laboratory tests[17].
Transplant renal artery stenosis: TRA stenosis (TRAS) is the most common vascular complication post-KT, with an incidence up to 23%[18]. Depending on the cause, TRAS can occur at any time, although it is more frequent between 3 mo and 2 years after transplantation[19]. Early TRAS is usually located at the site of end-to-side anastomosis and can be related to intraoperative complications such as trauma to the donor or recipient vessels during clamping or suturing. Late TRAS occurs in patients with atherosclerotic disease in the recipient or immune-mediated endothelial damage[20]. The clinical manifestation is most frequently severe hypertension with or without graft dysfunction[21], which can progress to graft loss if radiologic or surgical intervention is not performed[22].
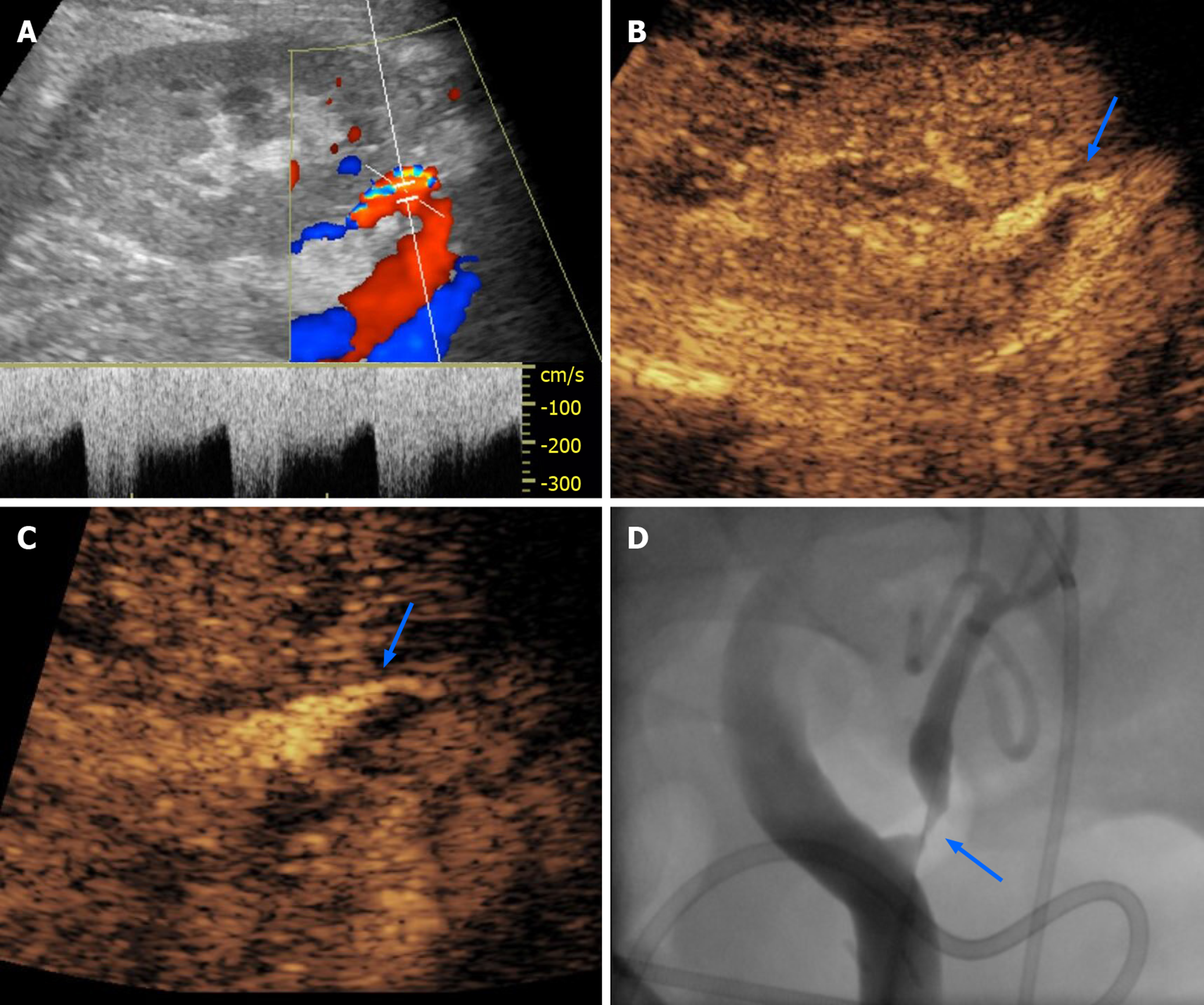
Color Doppler US can show increased TRA velocity, distal spectral broadening, and increased arterial acceleration time of intra-parenchymal arterial vessels[21,23]. The cut-off for pathologic TRA velocity varies between 200 and 300 cm/sec according to different Authors. The lower limit suffers from low specificity, and in turn can cause an excessive number of unnecessary procedures[3]. Controversy exists also with regard to the best RI cut-off[22]. CT angiography can be used to define the site and severity of the stenosis, i.e. as a road-map for subsequent interventional digital subtraction angiography (DSA)[21]. MRI angiography is a valid alternative for diagnosing TRAS, although this technique is less readily available and accessible, and tends to overestimate the degree of strictures[22]. Given the high negative predictive value, CEUS can be used as a complement to color Doppler to rapidly rule out TRAS within a single examination session, thus also sparing unnecessary CT angiography or DSA[24].
After contrast injection, normal TRA can be identified as a tubular enhancing structure running from the external iliac artery to the hilum of the renal allograft. Artery length and tortuosity are quite variable, depending on the surgical technique and length of the vascular pedicle in the transplanted kidney. According to Pan et al[22], quantitative measurement of strictures using CEUS achieves a 87.5% sensitivity for TRAS, with a specificity significantly higher (95.7%) than that of Doppler-derived indexes, such as peak systolic velocity (PSV)-TRA (67.4%) and PSV-ratio. Diagnosis of TRAS can be made when luminal narrowing exceeds 50% as compared to normal post-stenotic TRA (for strictures affecting the anastomotic site), or pre-stenotic TRA (for strictures affecting the main artery course) (Figure 2). Of note, about half of TRAS occurs at the anastomotic site[25].
Transplant renal artery thrombosis: TRA thrombosis (TRAT) is less common than TRAS, as it was reported to occur in 0.4% of patients[26]. Factors related to TRAT development are hyperacute rejection, anastomotic occlusion, arterial kinking, and intimal flap. This condition may translate into diffuse or segmental parenchymal infarcts presenting with anuria, as well as swelling and tenderness over the graft[25].
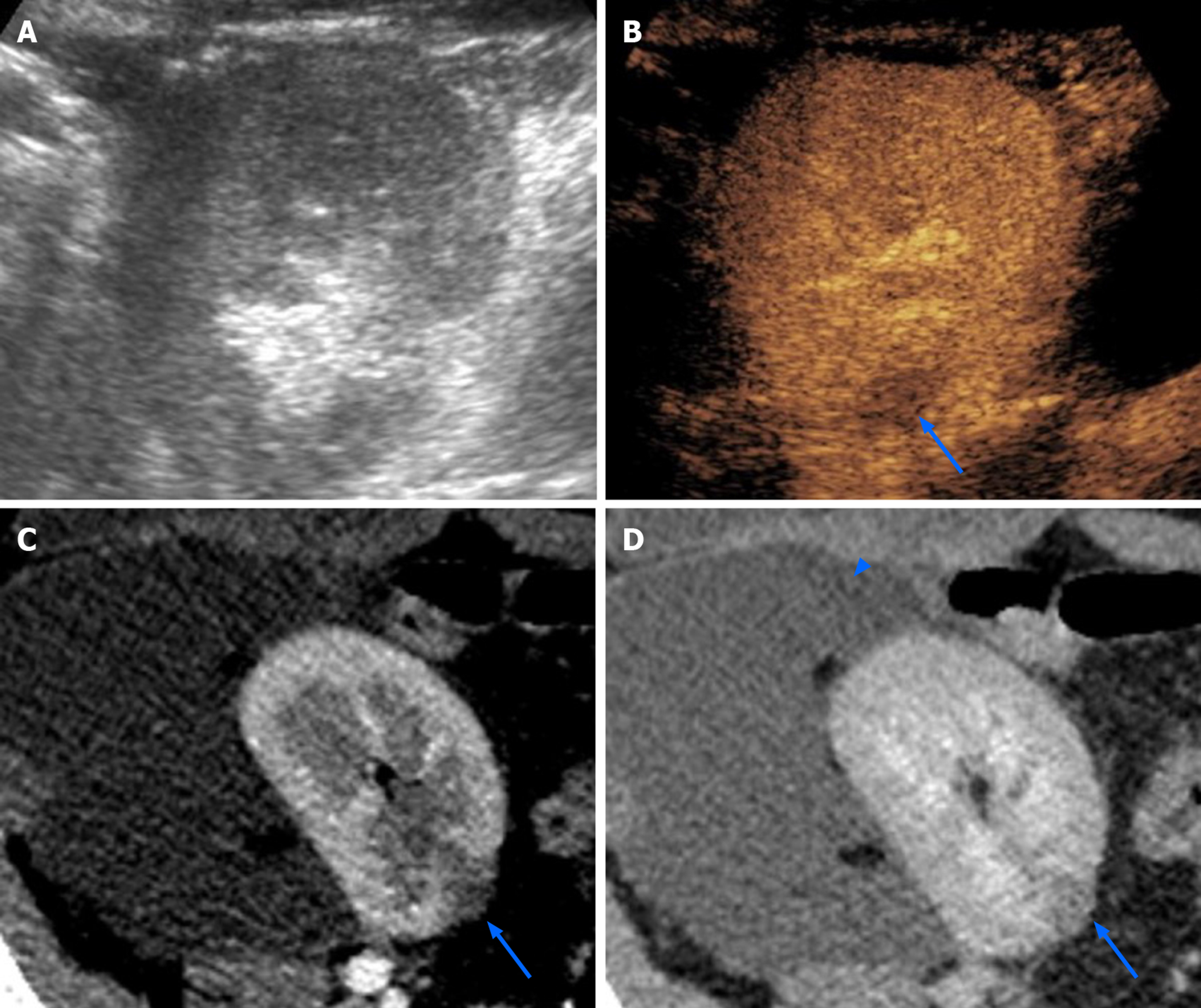
The main color Doppler criterion for diagnosing TRAT is the absence of flow in TRA and intrarenal arteries. However, this finding lacks specificity and can be found also in acute rejection[25]. CEUS can confirm arterial occlusion by showing the absence of contrast enhancement, and by reliably defining the site and extent of endoluminal defects[27]. Additionally, CEUS can exploit hypoperfused or infarcted parenchymal areas (see below), which might be the only imaging findings when TRAT involves a polar artery[28] (Figure 3). In the setting of TRAT, CEUS is expected to provide a better representation of the presence and extent of renal infarction than grayscale US and color Doppler US.
Transplant renal vein thrombosis: TRV thrombosis (TRVT) occurs in 0.2% of patients[26]. Etiology is multifactorial and includes donor-age > 60 years, recipient’s related factors (age > 50 years, diabetic nephropathy, thrombophilia), intra- and postoperative hemodynamic instability, deceased donor, and cold ischemia time > 24 h[29]. Usually, TRVT manifests in the first post-operative week with reduced urinary output as well as swelling and tenderness over the graft[25]. This complication is a major cause of graft loss and should be treated promptly with thrombectomy[25].
On grayscale US, the early phase of disease is characterized by enlargement of the graft and hypoechoic appearance of the cortex[30]. On Doppler examination, the thrombus can be difficult to visualize if venous anastomosis is located deeply in the pelvis. Indirect signs rising the suspicion of TRVT are reversed arterial diastolic flow, spike-like systolic component, and elevated resistive indexes[30]. However, while those findings have good sensitivity, they lack specificity as they occur also in other complications, including allograft torsion, severe rejection, and ATN[31].
CEUS can depict non-enhancing vein defects and hypoperfused parenchymal areas, increasing their conspicuity compared to color Doppler analysis[27]. During the earliest moments of the corticomedullary phase, one can appreciate pulsatile rather than continuous renal enhancement, possibly because of graft congestion and increased resistance to arterial flow. This finding is associated with patchy cortical enhancement[32].
Acute cortical necrosis: Acute cortical necrosis is a rare complication resulting from technical surgical problems, transplantation across ABO-incompatible blood groups, positive cytotoxic antibody crossmatch, pre-existent perfusion lesions in the kidney donor, and prolonged cold ischemia time of the cadaveric allograft[33,34]. This condition causes irreversible renal failure, thus requiring prompt diagnosis and tran-splantectomy[35].
Contrast-enhanced CT and MRI can demonstrate the pathognomonic peripheral rim sign, characterized by unenhanced cortical rim surrounding a normally enhancing medullary region[35]. While US is insensitive to this finding, CEUS can easily depict it, thus achieving prompt diagnosis without the need of further imaging or even biopsy[33]. After administering UCAs, the peripheral rim sign manifests with prompt filling of the main arteries followed by enhancement of medullary pyramids and absent cortical enhancement. The renal cortex appears as a hypovascular hypoechoic band persisting from the corticomedullary phase up to about 5 min after contrast injection[33].
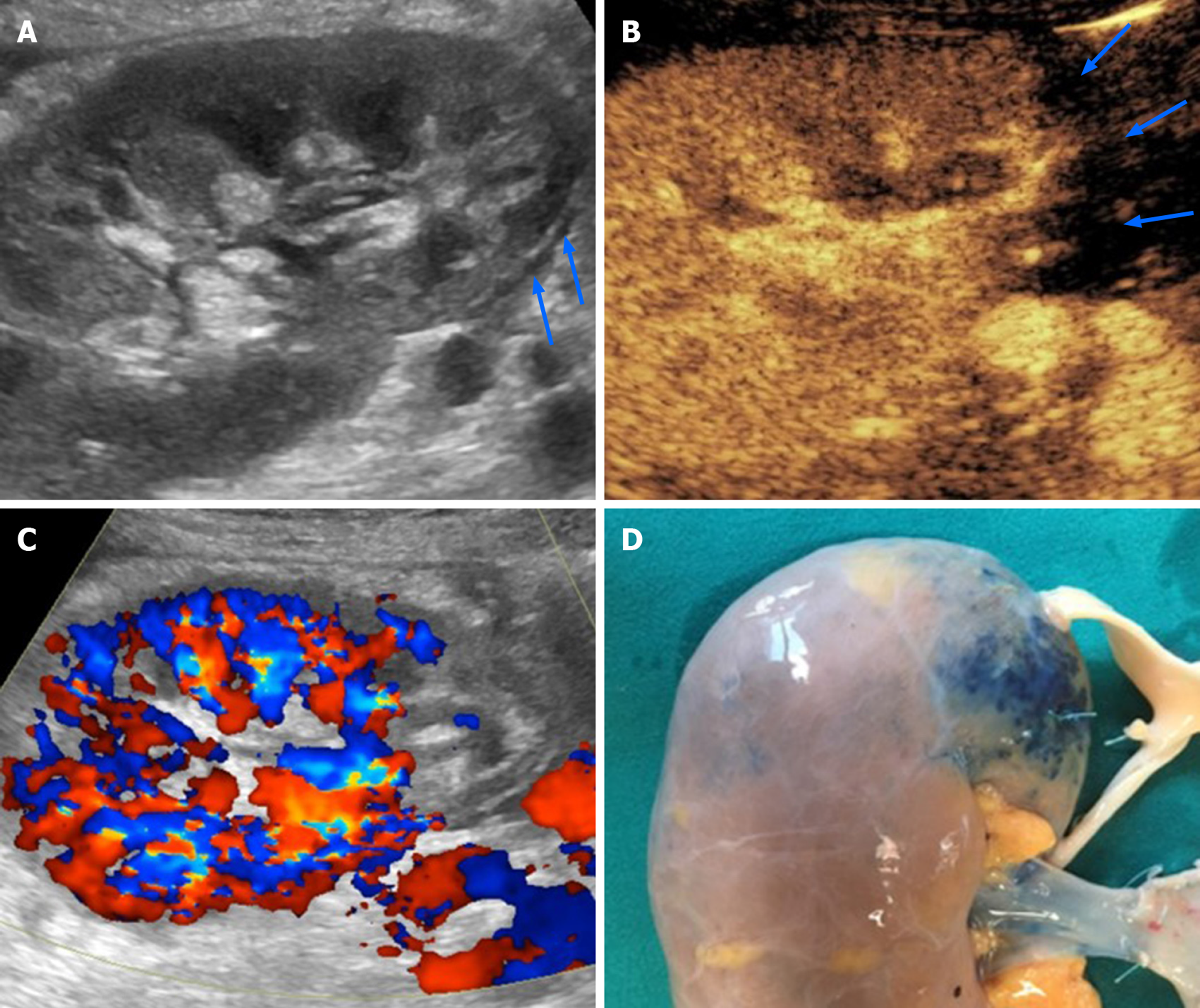
Arteriovenous fistula: Arteriovenous fistula (AVF) is an iatrogenic complication related to biopsy, typically caused by biopsies performed before transplantation, intraoperatively, or during postoperative KT surveillance[4]. AVF usually resolves spontaneously within 1-2 years, while a minority of cases persist and present with hematuria, renal failure, and hypertension. According to a survey by Furness et al[36], spontaneous major bleeding is rare, although it can represent a life-threating condition requiring prompt intervention[36].
On grayscale US and color Doppler examination, AVF appears as a hypoechoic area showing vascular signal, typically under the form of a vortex-like image representing turbulent flow. This area extends outside the distribution of normal vascular structures and is entered by a feeding artery with high velocity and low resistance flow. The efferent vein showing arterialized waveform can also be identified[25]. Once sonographic diagnosis is made, contrast-enhanced CT or MRI can better delineate the AVF anatomy[4].
On CEUS, AVF appears as an intraparenchymal pseudo-nodule with intense contrast-enhancement of vascular type, associated to early enhancement of the efferent vein[27]. UCAs administration can also demonstrate the hemodynamic steel effect of AVF on the surrounding parenchyma, appearing as a hypoperfused area close to the AVF site[37]. In this setting, CEUS is of help in referring patients to AVF embolization or in monitoring the effect of the procedure over time[38].
Perirenal collections: Perirenal collections are common after KT, occurring in up to 50% of patients. Urinomas and hematomas tend to present early after surgery, while lymphocele typically develops 4-8 wk after[25]. Collections are usually asymptomatic, although large ones can displace the graft or cause vascular and/or ureteral compression. Consequently, symptomatic collections should be drained.
US shows limited sensitivity in detecting clinically significant collections, tending to underestimate their size[39]. Moreover, while US can detect perirenal collections, it has a limited capability to distinguish among different origins and types. CT or MRI usually provide a more panoramic representation of symptomatic collections, and can better characterize the content, especially in the case of MRI.
Administering UCAs increases the conspicuity of vessels, graft parenchyma, perirenal tissues and non-enhancing collections[40]. According to Grzelak et al[40], the use of CEUS allowed to detect 17.6% more cases of perirenal hematomas than with US alone, and allowed to visualize collection with a thickness lower than 10 mm, values that were undetectable by grayscale US. Increased conspicuity of collections allows better evaluation of their size and relationship with the major vascular structure and the ureter (Figure 4), thus potentially helping in planning an intervention without the need for further imaging.
Ureteral obstruction: Ureteral obstruction occurs in about 4.1% of renal transplanted patients, mainly within the first 6 mo (mean time of occurrence is 5.4 mo)[41]. The obstruction is generally due to ureteral kinking or scarring-related stenosis secondary to ischemia or rejection[25]. Less commonly, obstructions arise from stones or extrinsic compression from perirenal collections[25]. Clinical manifestation is unspecific, including increase in serum creatinine and reduction in urine output[42]. Grayscale US allows to confirm hydronephrosis and search for intrinsic or extrinsic causes of obstruction along the urinary tract and bladder.
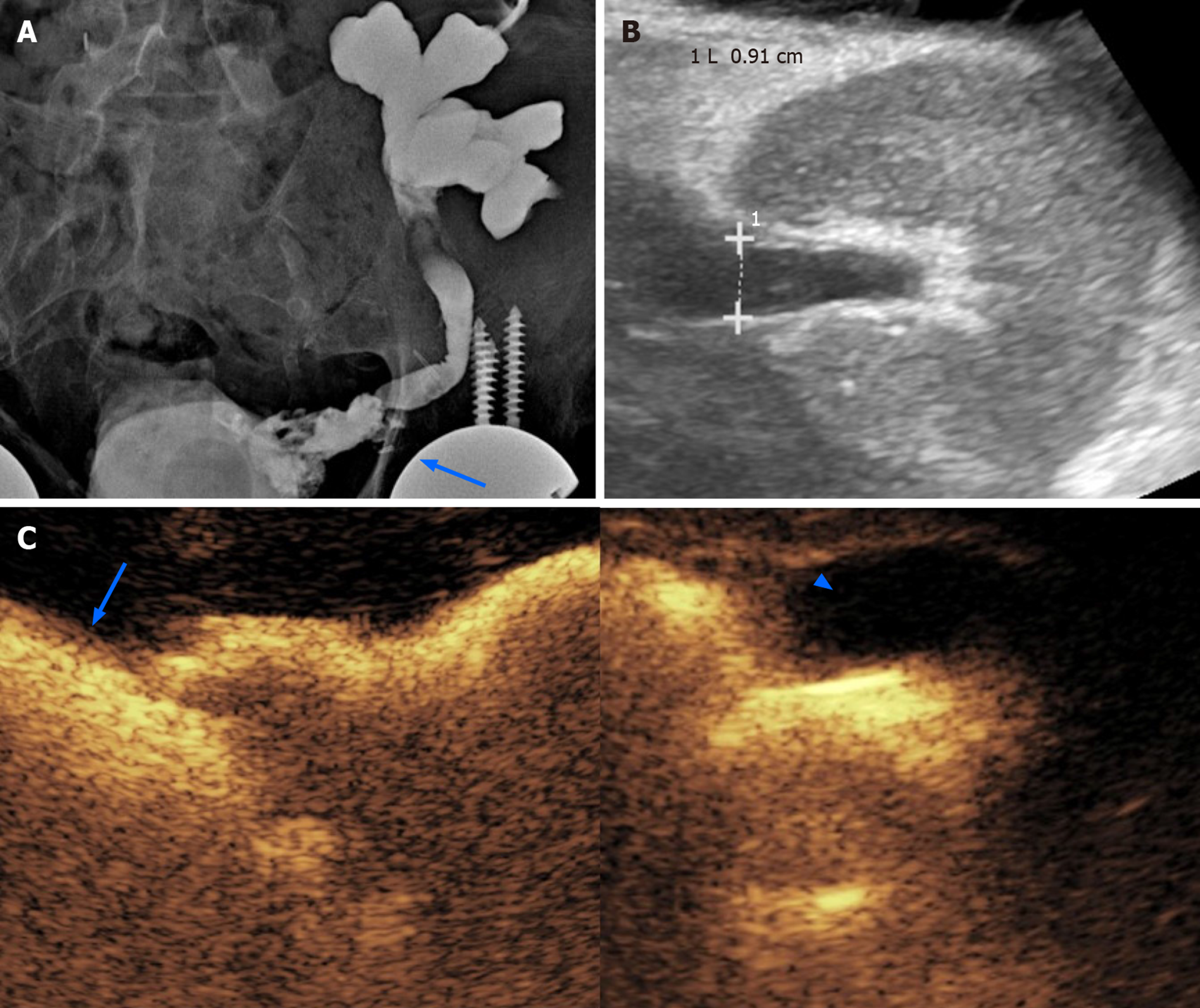
CEUS nephrostogram consists in the injection of UCAs through a percutaneous nephrostomy catheter followed by CEUS examination. This technique has been advocated as an alternative to fluoroscopic nephrostogram for a radiation-free evaluation of catheter and/or ureteral patency[43], showing comparable or even better performance in assessing malignant or benign ureteral obstruction[43,44]. For CEUS nephrostogram, we used 0.5-1.0 mL of SonoVue diluted in 10 mL of saline solution, with slow manual injection under real-time imaging. In our experience, this technique leads to a panoramic representation of the excretory system and documentation of contrast passage into the bladder (Figure 5). Alternatively, other Authors proposed the direct injection of UCAs in the renal collecting system as a mean to enable nephrostomy placement at patient’s bedside[45].
Rejection: Despite its decreased frequency in recent years, rejection remains one of the main complications of KT, with an incidence of 9%[46]. This condition is currently ascribed to two different mechanisms, i.e., T-cell-mediated rejection, and antibody-mediated rejection[47]. Based on temporal onset from KT, rejection can be classified into hyperacute (starting immediately after transplantation), acute (occurring 5-7 d after transplantation), chronic (occurring 3 mo after KT), and acute superimposed to chronic[47,48]. Since clinical presentation is not specific, diagnosis is obtained with a biopsy[48]. Thus, imaging is used to exclude alternative or coexisting complications.
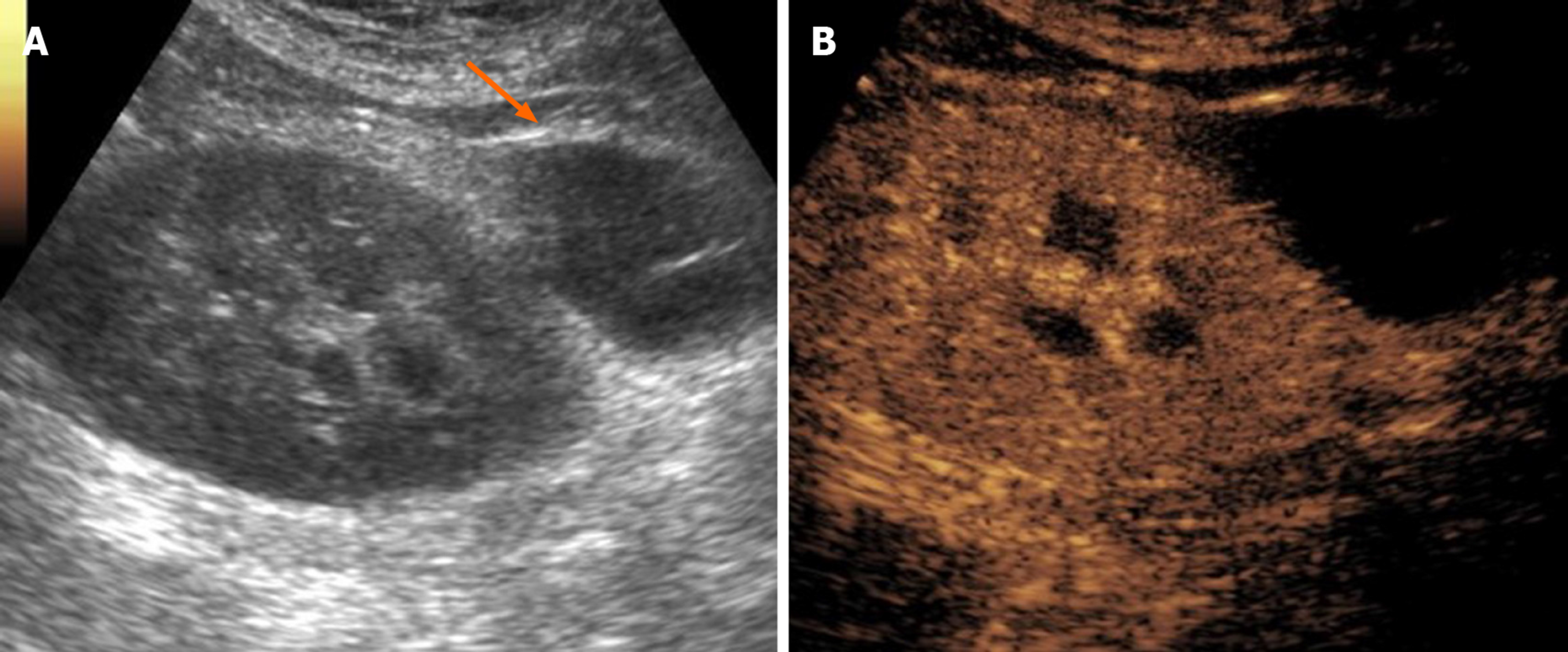
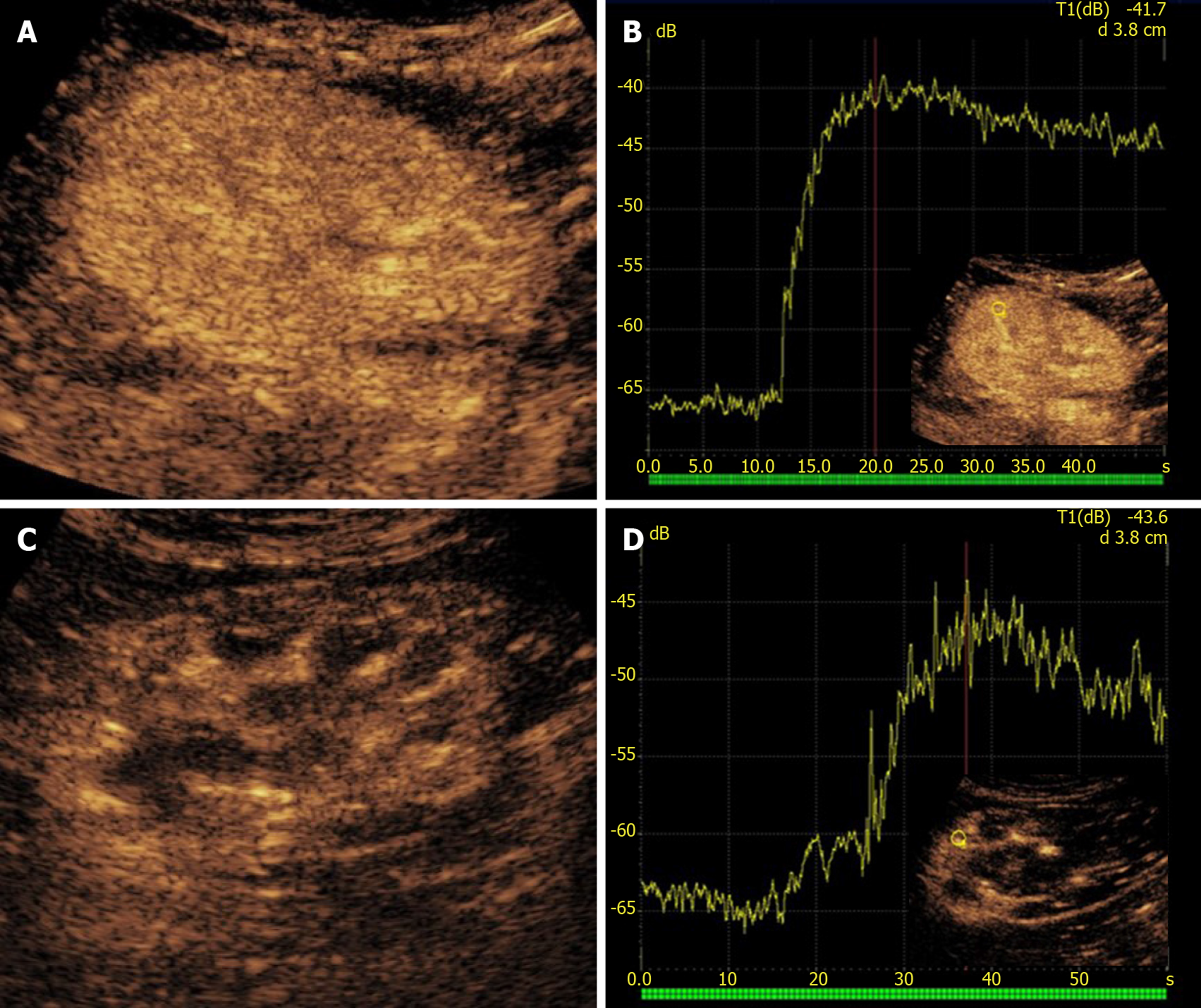
On US, rejection presents with loss of corticomedullary differentiation and edematous cortical thickening[4]. Doppler US can detect increased RI, although this finding is not specific[5]. The main capability of CEUS in this setting is that of adding TIC-derived perfusion analysis under the form of various quantitative indexes, a feature that showed promising potential for diagnosing rejection[49-51]. Benozzi et al[52] found an increased time-to-peak in patients with acute rejection compared to a control group. In the same series, patients with ATN showed a different pattern of abnormalities (lower cortico-medullary ratio of mean transit time and regional blood volume), suggesting that perfusion analysis might be of help in differentiating rejection from other causes of early graft dysfunction. Although these results are promising, there are still no definite rejection-related patterns of perfusion abnormalities. On the other hand, abnormal quantitative indexes in a proper clinical context may reasonably rise the suspicion of rejection (Figure 6).
Acute pyelonephritis and abscess: The reported cumulative incidence for acute pyelonephritis (APN) in renal transplant recipients ranges between 19% and 23%[53,54]. The likelihood of developing APN is increased by episodes of asymptomatic bacteriuria, cytomegalovirus infection, immunosuppression therapy, acute rejection, urological malformations of the native kidney, and placement of a ureteric stent[55,56]. APN may be asymptomatic or manifesting with bacteriuria, fever, graft pain and/or graft function impairment[57].
The role for grayscale US in APN is to exclude urinary obstruction and renal calculi as potential causes of infection[17]. US can also demonstrate renal enlargement, loss of corticomedullary differentiation, and reduced visibility of renal sinus fat due to edema[58]. CT is the preferred imaging modality for diagnosis, with higher specificity and sensitivity than US[58], although at the price of exposing patients to nephrotoxic contrast medium.
CEUS was shown to be as accurate as CT and MRI for assessing parenchymal changes in APN, with a 95% sensitivity and 100% specificity[59,60]. Typical APN findings are round or wedge-shaped hypovascular parenchymal areas in the cortical or corticomedullary region, with increased conspicuity during delayed phase (Figure 7)[61]. Focal APN can be distinguished from abscess, since the latter presents as an anechoic area, within or outside an area of pyelonephritis, sometimes with peripheral rim enhancement or septal enhancement. CEUS is useful in monitoring the effects of therapy and regression of abscesses over time.
Neoplasms: The overall incidence of malignancy in renal transplant recipients is about 3 to 5 times higher than in the general population[62]. Most common malignancies are lymphoproliferative disorders and skin carcinomas, whereas tumors of the genitourinary and reproductive system prevail among visceral neoplasms[62]. The occurrence of de novo renal cell carcinoma in native kidneys and renal graft has a pooled estimated incidence of 0.7% and 0.2%, respectively[63]. Tumors occurring in the graft are prevalently renal cell carcinomas[64].
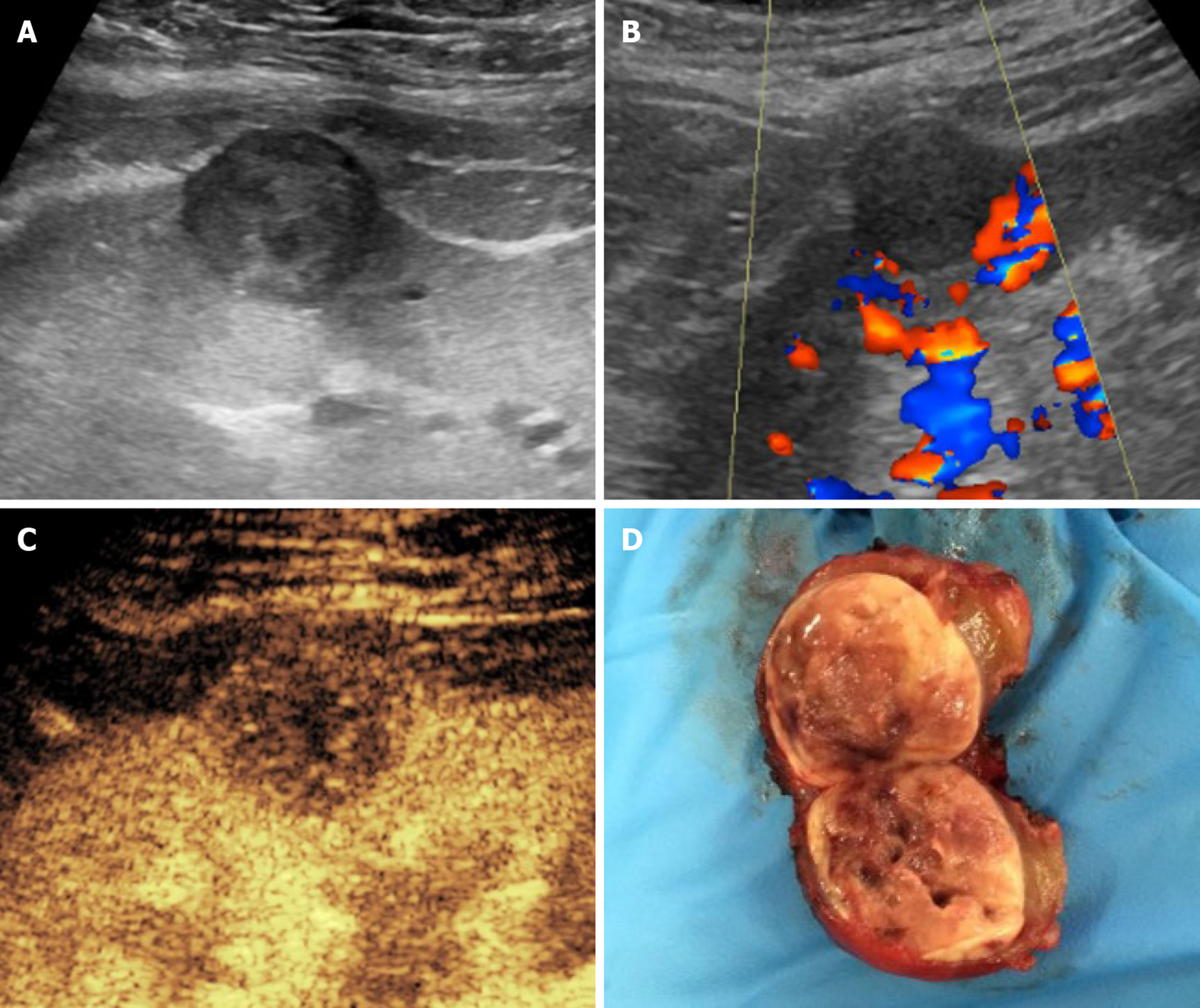
US-based surveillance plays an important role in identifying tumors at an early stage. Grayscale US and color Doppler examination can rule in or out benign findings, such as simple cysts, and can refer suspicious or inconclusive findings to further imaging for characterization. In this setting, CEUS has gained a well-established role in non-transplanted patients (Figure 8), being able to differentiate solid lesions from pseudolesions, and attributing the proper Bosniak category to cystic lesions, as comprehensively described elsewhere[65]. Findings in non-transplanted patients reasonably overlap with those of transplanted ones.
Other parenchymal conditions: There is great interest in finding non-invasive parameters able to detect parenchymal graft dysfunction before morphological alterations become evident, or to predict renal function on a long-term basis. Some Authors advocated a role for quantitative CEUS in this scenario, based on the fact that perfusion indexes are influenced by glomerular filtration rate and urine output, which in turn are commonly used functional indexes. In a study by Schwenger et al[66], renal blood flow measured at 1 wk after transplantation was shown to correlate with renal function at 1 year.
A common cause of graft failure is related to the immunosuppressive therapy. Calcineurin-inhibitor nephrotoxicity is largely present at 10 years after transplantation, being characterized by arteriolar hyalinosis, ischemic glomerulosclerosis, and interstitial fibrosis[67]. CEUS investigation of graft perfusion demonstrated a reduction of renal blood flow in patients receiving therapy with Cyclosporine-A early after KT, thus having the potential to represent altered micro-perfusion as a marker of graft damage[68].
CEUS represents an ideal first-line tool in evaluating KT patients, improving the accuracy of conventional US for a variety of complications. Assumed that the examination is performed by experienced operators, CEUS is a fast and reliable alternative to CT and MRI, which might be contraindicated in patients with impaired renal function. While most established applications of CEUS rely on the capability of identifying major vascular and parenchymal complications, there is increasing research on quantitative perfusion indexes reflecting microcirculation abnormalities electively.
The authors thank Viviana Moroso (MSc, PhD) of MV Medical Writing (Luleå, Sweden) for copyediting the manuscript, and Dr. Clara Zichichi (Institute of Radiology, University of Udine) for having drawn Figure 1C.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: European Society of Urogenital Radiology.
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Huang P, Shi BM S-Editor: Gong ZM L-Editor: A P-Editor: Liu JH
| 1. | Tonelli M, Wiebe N, Knoll G, Bello A, Browne S, Jadhav D, Klarenbach S, Gill J. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11:2093-2109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 1053] [Article Influence: 75.2] [Reference Citation Analysis (0)] |
| 2. | Haberal M, Boyvat F, Akdur A, Kırnap M, Özçelik Ü, Yarbuğ Karakayalı F. Surgical Complications After Kidney Transplantation. Exp Clin Transplant. 2016;14:587-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Expert Panel on Urologic Imaging, Taffel MT, Nikolaidis P, Beland MD, Blaufox MD, Dogra VS, Goldfarb S, Gore JL, Harvin HJ, Heilbrun ME, Heller MT, Khatri G, Preminger GM, Purysko AS, Smith AD, Wang ZJ, Weinfeld RM, Wong-You-Cheong JJ, Remer EM, Lockhart ME. ACR Appropriateness Criteria® Renal Transplant Dysfunction. J Am Coll Radiol. 2017;14:S272-S281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Sugi MD, Joshi G, Maddu KK, Dahiya N, Menias CO. Imaging of Renal Transplant Complications throughout the Life of the Allograft: Comprehensive Multimodality Review. Radiographics. 2019;39:1327-1355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 5. | Naesens M, Heylen L, Lerut E, Claes K, De Wever L, Claus F, Oyen R, Kuypers D, Evenepoel P, Bammens B, Sprangers B, Meijers B, Pirenne J, Monbaliu D, de Jonge H, Metalidis C, De Vusser K, Vanrenterghem Y. Intrarenal resistive index after renal transplantation. N Engl J Med. 2013;369:1797-1806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 144] [Article Influence: 12.0] [Reference Citation Analysis (2)] |
| 6. | Chung YE, Kim KW. Contrast-enhanced ultrasonography: advance and current status in abdominal imaging. Ultrasonography. 2015;34:3-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 121] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 7. | Rafailidis V, Huang DY, Yusuf GT, Sidhu PS. General principles and overview of vascular contrast-enhanced ultrasonography. Ultrasonography. 2020;39:22-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 8. | Dietrich CF, Averkiou M, Nielsen MB, Barr RG, Burns PN, Calliada F, Cantisani V, Choi B, Chammas MC, Clevert DA, Claudon M, Correas JM, Cui XW, Cosgrove D, D'Onofrio M, Dong Y, Eisenbrey J, Fontanilla T, Gilja OH, Ignee A, Jenssen C, Kono Y, Kudo M, Lassau N, Lyshchik A, Franca Meloni M, Moriyasu F, Nolsøe C, Piscaglia F, Radzina M, Saftoiu A, Sidhu PS, Sporea I, Schreiber-Dietrich D, Sirlin CB, Stanczak M, Weskott HP, Wilson SR, Willmann JK, Kim TK, Jang HJ, Vezeridis A, Westerway S. How to perform Contrast-Enhanced Ultrasound (CEUS). Ultrasound Int Open. 2018;4:E2-E15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 246] [Cited by in RCA: 222] [Article Influence: 31.7] [Reference Citation Analysis (33)] |
| 9. | Gulati M, King KG, Gill IS, Pham V, Grant E, Duddalwar VA. Contrast-enhanced ultrasound (CEUS) of cystic and solid renal lesions: a review. Abdom Imaging. 2015;40:1982-1996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 10. | McArthur C, Baxter GM. Current and potential renal applications of contrast-enhanced ultrasound. Clin Radiol. 2012;67:909-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Piscaglia F, Bolondi L; Italian Society for Ultrasound in Medicine and Biology (SIUMB) Study Group on Ultrasound Contrast Agents. The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol. 2006;32:1369-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 533] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 12. | Yusuf GT, Sellars ME, Deganello A, Cosgrove DO, Sidhu PS. Retrospective Analysis of the Safety and Cost Implications of Pediatric Contrast-Enhanced Ultrasound at a Single Center. AJR Am J Roentgenol. 2017;208:446-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 13. | Contrast Media Safety Committee ESUR. Guidelines on Contrast Media v10.0. CMSC, 2018. [accessed 17 March 2020]. Available from: http://www.esur.org/fileadmin/content/2019/ESUR_Guidelines_10.0_Final_Version.pdf. |
| 14. | Nilsson A, Lencioni R. Contrast-Enhanced Ultrasound of Focal Renal Lesions. In: Lencioni R. Enhancing the Role of Ultrasound with Contrast Agents. Lencioni R. Milano: Springer, 2006: 162-175. |
| 15. | Westwood M, Joore M, Grutters J, Redekop K, Armstrong N, Lee K, Gloy V, Raatz H, Misso K, Severens J, Kleijnen J. Contrast-enhanced ultrasound using SonoVue® (sulphur hexafluoride microbubbles) compared with contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging for the characterisation of focal liver lesions and detection of liver metastases: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2013;17:1-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 16. | Smajerova M, Petrasova H, Little J, Ovesna P, Andrasina T, Valek V, Nemcova E, Miklosova B. Contrast-enhanced ultrasonography in the evaluation of incidental focal liver lesions: A cost-effectiveness analysis. World J Gastroenterol. 2016;22:8605-8614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (2)] |
| 17. | Sidhu PS, Cantisani V, Dietrich CF, Gilja OH, Saftoiu A, Bartels E, Bertolotto M, Calliada F, Clevert DA, Cosgrove D, Deganello A, D'Onofrio M, Drudi FM, Freeman S, Harvey C, Jenssen C, Jung EM, Klauser AS, Lassau N, Meloni MF, Leen E, Nicolau C, Nolsoe C, Piscaglia F, Prada F, Prosch H, Radzina M, Savelli L, Weskott HP, Wijkstra H. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. 2018;39:e2-e44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 653] [Cited by in RCA: 589] [Article Influence: 84.1] [Reference Citation Analysis (1)] |
| 18. | Ammi M, Daligault M, Sayegh J, Abraham P, Papon X, Enon B, Picquet J. Evaluation of the Vascular Surgical Complications of Renal Transplantation. Ann Vasc Surg. 2016;33:23-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Bruno S, Remuzzi G, Ruggenenti P. Transplant renal artery stenosis. J Am Soc Nephrol. 2004;15:134-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 205] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 20. | Chen W, Kayler LK, Zand MS, Muttana R, Chernyak V, DeBoccardo GO. Transplant renal artery stenosis: clinical manifestations, diagnosis and therapy. Clin Kidney J. 2015;8:71-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 21. | Fananapazir G, McGahan JP, Corwin MT, Stewart SL, Vu CT, Wright L, Troppmann C. Screening for Transplant Renal Artery Stenosis: Ultrasound-Based Stenosis Probability Stratification. AJR Am J Roentgenol. 2017;209:1064-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Pan FS, Liu M, Luo J, Tian WS, Liang JY, Xu M, Zheng YL, Xie XY. Transplant renal artery stenosis: Evaluation with contrast-enhanced ultrasound. Eur J Radiol. 2017;90:42-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 23. | Ghazanfar A, Tavakoli A, Augustine T, Pararajasingam R, Riad H, Chalmers N. Management of transplant renal artery stenosis and its impact on long-term allograft survival: a single-centre experience. Nephrol Dial Transplant. 2011;26:336-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 24. | Mueller-Peltzer K, Rübenthaler J, Fischereder M, Habicht A, Reiser M, Clevert DA. The diagnostic value of contrast-enhanced ultrasound (CEUS) as a new technique for imaging of vascular complications in renal transplants compared to standard imaging modalities. Clin Hemorheol Microcirc. 2017;67:407-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Akbar SA, Jafri SZ, Amendola MA, Madrazo BL, Salem R, Bis KG. Complications of renal transplantation. Radiographics. 2005;25:1335-1356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 126] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 26. | Ayvazoglu Soy EH, Akdur A, Kirnap M, Boyvat F, Moray G, Haberal M. Vascular Complications After Renal Transplant: A Single-Center Experience. Exp Clin Transplant. 2017;15:79-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | García Roch C, Muñoz Cepeda MÁ, García García F, Ciampi Dopazo JJ, Pinto Varela JM, Díaz Crespo FJ. Contrast Enhanced Ultrasound (CEUS) efficiency in renal graft complications evaluation. Nefrologia. 2018;38:444-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Stenberg B, Wilkinson M, Elliott S, Caplan N. The prevalence and significance of renal perfusion defects in early kidney transplants quantified using 3D contrast enhanced ultrasound (CEUS). Eur Radiol. 2017;27:4525-4531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Keller AK, Jorgensen TM, Jespersen B. Identification of risk factors for vascular thrombosis may reduce early renal graft loss: a review of recent literature. J Transplant. 2012;2012:793461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 30. | El Zorkany K, Bridson JM, Sharma A, Halawa A. Transplant Renal Vein Thrombosis. Exp Clin Transplant. 2017;15:123-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 31. | Lockhart ME, Wells CG, Morgan DE, Fineberg NS, Robbin ML. Reversed diastolic flow in the renal transplant: perioperative implications versus transplants older than 1 month. AJR Am J Roentgenol. 2008;190:650-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 32. | Álvarez Rodríguez S, Hevia Palacios V, Sanz Mayayo E, Gómez Dos Santos V, Díez Nicolás V, Sánchez Gallego MD, Lorca Álvaro J, Burgos Revilla FJ. The Usefulness of Contrast-Enhanced Ultrasound in the Assessment of Early Kidney Transplant Function and Complications. Diagnostics (Basel). 2017;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 33. | Fernandez CP, Ripolles T, Martinez MJ, Blay J, Pallardó L, Gavela E. Diagnosis of acute cortical necrosis in renal transplantation by contrast-enhanced ultrasound: a preliminary experience. Ultraschall Med. 2013;34:340-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Quintana LF, Cofan F, Reverté JC, Oppenheimer F, Campistol JM. Renal cortical necrosis after kidney transplantation associated with the prothrombin 20210A mutation. Nephrol Dial Transplant. 2006;21:1455-1456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 35. | Dyer RB, Chen MY, Zagoria RJ. Classic signs in uroradiology. Radiographics. 2004;24 Suppl 1:S247-S280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 96] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 36. | Furness PN, Philpott CM, Chorbadjian MT, Nicholson ML, Bosmans JL, Corthouts BL, Bogers JJ, Schwarz A, Gwinner W, Haller H, Mengel M, Seron D, Moreso F, Cañas C. Protocol biopsy of the stable renal transplant: a multicenter study of methods and complication rates. Transplantation. 2003;76:969-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 162] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 37. | Grzelak P, Sapieha M, Kurnatowska I, Nowicki M, Strzelczyk J, Stefańczyk L. Contrast-enhanced sonography of postbiopsy arteriovenous fistulas in kidney grafts. J Clin Ultrasound. 2011;39:378-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Helck A, Sommer WH, Wessely M, Notohamiprodjo M, Reiser M, Clevert DA. Benefit of contrast enhanced ultrasound for detection of ischaemic lesions and arterio venous fistulas in renal transplants - a feasibility study. Clin Hemorheol Microcirc. 2011;48:149-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 39. | Fananapazir G, Rao R, Corwin MT, Naderi S, Santhanakrishnan C, Troppmann C. Sonographic Evaluation of Clinically Significant Perigraft Hematomas in Kidney Transplant Recipients. AJR Am J Roentgenol. 2015;205:802-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 40. | Grzelak P, Kurnatowska I, Nowicki M, Strzelczyk J, Durczyński A, Podgórski M, Stefańczyk L. The diagnostic value of contrast-enhanced ultrasonography in the assessment of perirenal hematomas in the early post-operative period after kidney transplantation. Clin Transplant. 2013;27:E619-E624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 41. | Karam G, Hétet JF, Maillet F, Rigaud J, Hourmant M, Soulillou JP, Giral M. Late ureteral stenosis following renal transplantation: risk factors and impact on patient and graft survival. Am J Transplant. 2006;6:352-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 64] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 42. | Kumar S, Ameli-Renani S, Hakim A, Jeon JH, Shrivastava S, Patel U. Ureteral obstruction following renal transplantation: causes, diagnosis and management. Br J Radiol. 2014;87:20140169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 43. | Daneshi M, Yusuf GT, Fang C, Sellars ME, Huang DY, Sidhu PS. Contrast-enhanced ultrasound (CEUS) nephrostogram: utility and accuracy as an alternative to fluoroscopic imaging of the urinary tract. Clin Radiol. 2019;74:167.e9-167.e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 44. | Chi T, Usawachintachit M, Weinstein S, Kohi MP, Taylor A, Tzou DT, Chang HC, Stoller M, Mongan J. Contrast Enhanced Ultrasound as a Radiation-Free Alternative to Fluoroscopic Nephrostogram for Evaluating Ureteral Patency. J Urol. 2017;198:1367-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Yusuf GT, Fang C, Huang DY, Sellars ME, Deganello A, Sidhu PS. Endocavitary contrast enhanced ultrasound (CEUS): a novel problem solving technique. Insights Imaging. 2018;9:303-311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 46. | Hamida FB, Barbouch S, Bardi R, Helal I, Kaaroud H, Fatma LB, Hedri H, Abderrahim E, Abdallah TB, Ayed K, Maiz HB, Kheder A. Acute rejection episodes after kidney transplantation. Saudi J Kidney Dis Transpl. 2009;20:370-374. [PubMed] |
| 47. | Haas M, Loupy A, Lefaucheur C, Roufosse C, Glotz D, Seron D, Nankivell BJ, Halloran PF, Colvin RB, Akalin E, Alachkar N, Bagnasco S, Bouatou Y, Becker JU, Cornell LD, Duong van Huyen JP, Gibson IW, Kraus ES, Mannon RB, Naesens M, Nickeleit V, Nickerson P, Segev DL, Singh HK, Stegall M, Randhawa P, Racusen L, Solez K, Mengel M. The Banff 2017 Kidney Meeting Report: Revised diagnostic criteria for chronic active T cell-mediated rejection, antibody-mediated rejection, and prospects for integrative endpoints for next-generation clinical trials. Am J Transplant. 2018;18:293-307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 663] [Cited by in RCA: 799] [Article Influence: 114.1] [Reference Citation Analysis (0)] |
| 48. | Bhowmik DM, Dinda AK, Mahanta P, Agarwal SK. The evolution of the Banff classification schema for diagnosing renal allograft rejection and its implications for clinicians. Indian J Nephrol. 2010;20:2-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 49. | Cai R, Tao L, Liang W, Lin M, Guo X, Huang XE. Application of Contrast-Enhanced Sonography on the Diagnosis of Acute and Chronic Rejection After Renal Transplantation. Ultrasound Q. 2020;36:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 50. | Jehn U, Schuette-Nuetgen K, Kentrup D, Hoerr V, Reuter S. Renal Allograft Rejection: Noninvasive Ultrasound- and MRI-Based Diagnostics. Contrast Media Mol Imaging. 2019;2019:3568067. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 51. | Yang C, Wu S, Yang P, Shang G, Qi R, Xu M, Rong R, Zhu T, He W. Prediction of renal allograft chronic rejection using a model based on contrast-enhanced ultrasonography. Microcirculation. 2019;26:e12544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 52. | Benozzi L, Cappelli G, Granito M, Davoli D, Favali D, Montecchi MG, Grossi A, Torricelli P, Albertazzi A. Contrast-enhanced sonography in early kidney graft dysfunction. Transplant Proc. 2009;41:1214-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 53. | Pellé G, Vimont S, Levy PP, Hertig A, Ouali N, Chassin C, Arlet G, Rondeau E, Vandewalle A. Acute pyelonephritis represents a risk factor impairing long-term kidney graft function. Am J Transplant. 2007;7:899-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 201] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 54. | Valera B, Gentil MA, Cabello V, Fijo J, Cordero E, Cisneros JM. Epidemiology of urinary infections in renal transplant recipients. Transplant Proc. 2006;38:2414-2415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 93] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 55. | Fiorante S, Fernández-Ruiz M, López-Medrano F, Lizasoain M, Lalueza A, Morales JM, San-Juan R, Andrés A, Otero JR, Aguado JM. Acute graft pyelonephritis in renal transplant recipients: incidence, risk factors and long-term outcome. Nephrol Dial Transplant. 2011;26:1065-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 56. | Kamath NS, John GT, Neelakantan N, Kirubakaran MG, Jacob CK. Acute graft pyelonephritis following renal transplantation. Transpl Infect Dis. 2006;8:140-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 117] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 57. | Gołębiewska J, Dębska-Ślizień A, Komarnicka J, Samet A, Rutkowski B. Urinary tract infections in renal transplant recipients. Transplant Proc. 2011;43:2985-2990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 58. | Craig WD, Wagner BJ, Travis MD. Pyelonephritis: radiologic-pathologic review. Radiographics. 2008;28:255-277; quiz 327-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 233] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 59. | Mitterberger M, Pinggera GM, Colleselli D, Bartsch G, Strasser H, Steppan I, Pallwein L, Friedrich A, Gradl J, Frauscher F. Acute pyelonephritis: comparison of diagnosis with computed tomography and contrast-enhanced ultrasonography. BJU Int. 2008;101:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 60. | Granata A, Andrulli S, Fiorini F, Basile A, Logias F, Figuera M, Sicurezza E, Gallieni M, Fiore CE. Diagnosis of acute pyelonephritis by contrast-enhanced ultrasonography in kidney transplant patients. Nephrol Dial Transplant. 2011;26:715-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 61. | Fontanilla T, Minaya J, Cortés C, Hernando CG, Arangüena RP, Arriaga J, Carmona MS, Alcolado A. Acute complicated pyelonephritis: contrast-enhanced ultrasound. Abdom Imaging. 2012;37:639-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 62. | Zeier M, Hartschuh W, Wiesel M, Lehnert T, Ritz E. Malignancy after renal transplantation. Am J Kidney Dis. 2002;39:E5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 63. | Chewcharat A, Thongprayoon C, Bathini T, Aeddula NR, Boonpheng B, Kaewput W, Watthanasuntorn K, Lertjitbanjong P, Sharma K, Torres-Ortiz A, Leeaphorn N, Mao MA, Khoury NJ, Cheungpasitporn W. Incidence and Mortality of Renal Cell Carcinoma after Kidney Transplantation: A Meta-Analysis. J Clin Med. 2019;8:530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 64. | Griffith JJ, Amin KA, Waingankar N, Lerner SM, Delaney V, Ames SA, Badani K, Palese MA, Mehrazin R. Solid Renal Masses in Transplanted Allograft Kidneys: A Closer Look at the Epidemiology and Management. Am J Transplant. 2017;17:2775-2781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 65. | Bertolotto M, Bucci S, Valentino M, Currò F, Sachs C, Cova MA. Contrast-enhanced ultrasound for characterizing renal masses. Eur J Radiol. 2018;105:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 66. | Schwenger V, Hankel V, Seckinger J, Macher-Göppinger S, Morath C, Zeisbrich M, Zeier M, Kihm LP. Contrast-enhanced ultrasonography in the early period after kidney transplantation predicts long-term allograft function. Transplant Proc. 2014;46:3352-3357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 67. | Nankivell BJ, PʼNg CH, OʼConnell PJ, Chapman JR. Calcineurin Inhibitor Nephrotoxicity Through the Lens of Longitudinal Histology: Comparison of Cyclosporine and Tacrolimus Eras. Transplantation. 2016;100:1723-1731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 136] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 68. | Kihm LP, Blume C, Seckinger J, Hankel V, Stoffler D, Morath C, Zeier M, Schwenger V. Acute effects of calcineurin inhibitors on kidney allograft microperfusion visualized by contrast-enhanced sonography. Transplantation. 2012;93:1125-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |