Published online May 28, 2019. doi: 10.4329/wjr.v11.i5.74
Peer-review started: February 22, 2019
First decision: March 14, 2019
Revised: April 4, 2019
Accepted: May 14, 2019
Article in press: May 15, 2019
Published online: May 28, 2019
Processing time: 97 Days and 2.5 Hours
Third epidermoid tumors are a rare finding. The appearance of these tumors often makes them difficult to diagnose, and thus they require multimodality imaging.
A 48-year-old male patient reported to our hospital with complaints of vomiting and severe headache. The patient also complained of involuntary micturition for the past five days. We used a combination of computed tomography (CT) and magnetic resonance imaging (MRI) imaging modalities to confirm the presence of a malignant epidermoid cyst arising from the third ventricle. A contrast-enhanced CT of the head demonstrated minimal perilesional enhancement while an MRI revealed a large, lobulated and septated T2 hyperintense mass arising from the third ventricle. The maximum size of the lesion measured 73 mm × 65 mm × 64 mm in size.
Malignant epidermoid arising from the third ventricle in an adult male was reported using a combination of CT, MRI, and MR spectroscopy.
Core tip: The use of multi-modality imaging can help radiologist diagnose uncommon tumors in unusual sites. The combination of computed tomography, magnetic resonance imaging, and MR spectroscopy was useful in confirming the diagnosis of malignant epidermoid arising from the third ventricle, an unusual site in routine practice.
- Citation: Pawar S, Borde C, Patil A, Nagarkar R. Malignant epidermoid arising from the third ventricle: A case report. World J Radiol 2019; 11(5): 74-80
- URL: https://www.wjgnet.com/1949-8470/full/v11/i5/74.htm
- DOI: https://dx.doi.org/10.4329/wjr.v11.i5.74
Epidermoid cysts are an uncommon finding in routine clinical settings. They are slow-growing, benign tumors that grow in the extra-axial areas. Epidermoid cysts account for less than 1% of all intracranial tumors[1]. Intracranial dermoid cysts are often observed in the cranial midline, sub-frontal areas, posterior fossa, and suprasellar cistern[2]. Intraventricular dermoid cysts are extremely rare and have been reported in the fourth ventricle[2]. Current imaging modalities have made it possible to recognize intracranial tumors[3]. The use of radiologic diagnosis for third ventricle epidermoid cysts is almost always possible.
We present a case of epidermoid cysts in the third ventricle in an adult male.
A 48-year-old male presented to our outpatient department with vomiting, headache, and involuntary micturition.
The above-mentioned symptoms had been present for five days.
The patient had no history of major illness.
The patient had no relevant family history.
The patient had no pallor. General condition of the patient was normal.
The patient’s routine laboratory investigations were within normal limits.
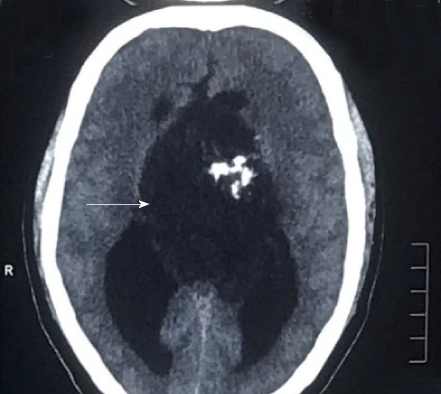
A non-contrast computed tomography scan of the head revealed a mass arising from the third ventricle appearing hypodense and showing coarse nodular as well as curvilinear calcifications (Figure 1).
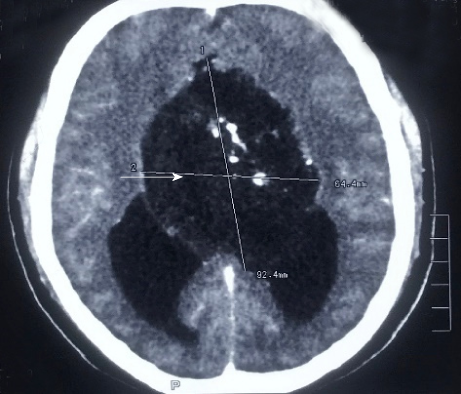
A contrast-enhanced computed tomography (CT) of the head demonstrated minimal perilesional enhancement. The lesion obstructed the hydrocephalus of the lateral ventricles (Figure 2). No dilatation of the fourth ventricle was observed. The lesion measured 8-10 Hounsfield units. The maximum size of the lesion measured 77x57 mm on CT scan.
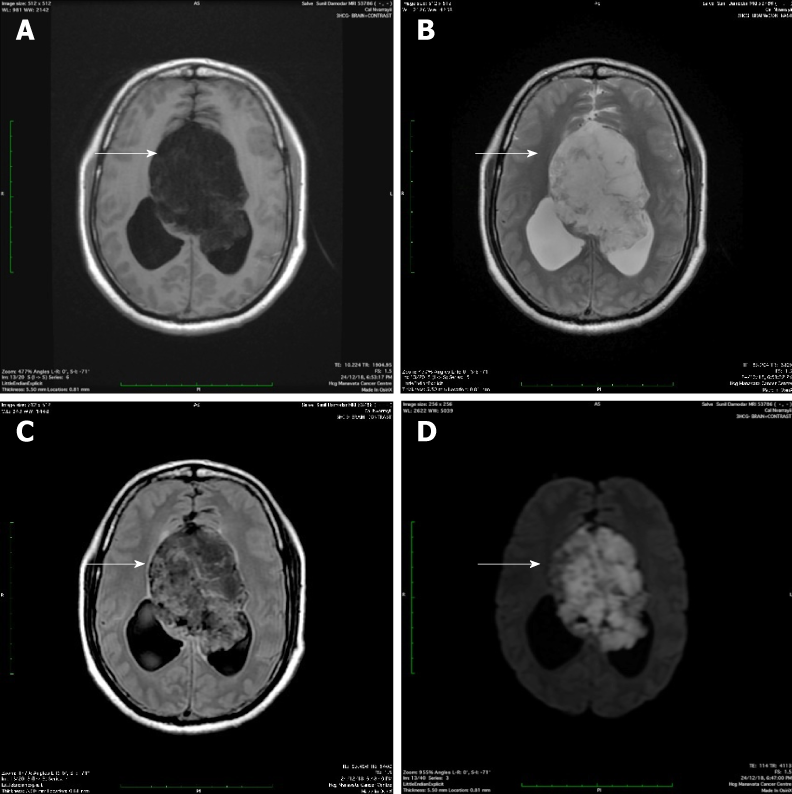
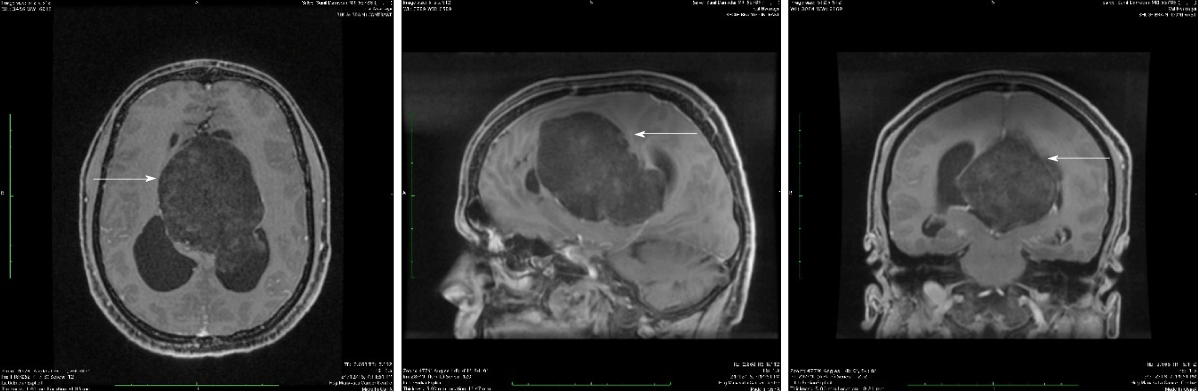
Magnetic resonance imaging (MRI) of the lesion revealed a large, lobulated, septated T2 hyperintense mass arising from the third ventricle (Figure 3B). It was hypointense on T1-weighted imaging with few cystic areas (Figure 3A). Few calcifications were observed within the cystic areas. On diffusion-weighted magnetic resonance imaging, the lesion showed increased restricted diffusion (Figure 3D). The lesion obstructed the hydrocephalus and caused moderate dilatation of the bilateral lateral ventricles. No dilation of the fourth ventricle was observed. On contrast-enhanced CT scan, the lesion showed minimal peripheral enhancement without any demonstrable solid enhancing component. The maximum size of the lesion measured 73 mm × 65 mm × 64 mm in size (Figure 4).
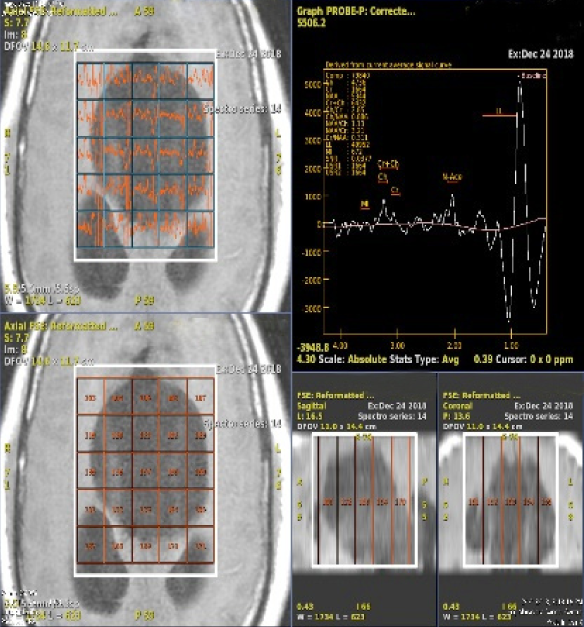
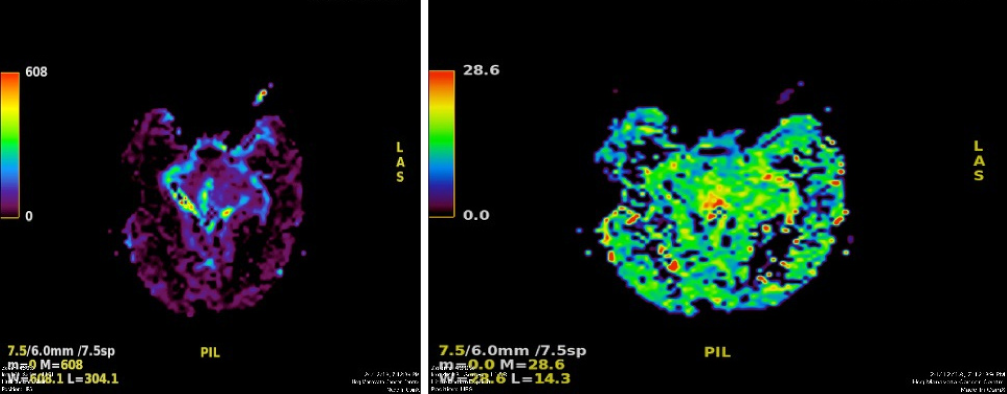
On MR spectroscopy, there was high lipid/lactate peak with comparatively lower N-acetylaspartate (NAA) and choline levels. The maximum choline (Cho)/creatine ratio was 2.85 within the lesion and CHO/NAA ratio was 0.766 (Figure 5). MR perfusion derived relative cerebral blood volume (rCBV) maps demonstrating heterogeneous perfusion abnormalities. Mild higher normalized rCBV ratios in comparison with white matter were noted in the peripheral region of the cyst, which corresponded to malignant transformation (Figure 6).
Considering the imaging findings, we suspected the lesion to be an epidermoid, dermoid, or an arachnoid cyst. However, we ruled out the diagnosis of a dermoid or arachnoid cyst considering the presence of a restricted diffusion on diffusion-weighted imaging (DWI). A combination of T1WI, T2WI, T2 axial FLAIR, and DW imaging techniques helped us diagnose an epidermoid cyst. However, the use of MR spectroscopy helped in making the probable diagnosis of a malignant epidermoid cyst arising from the third ventricle.
The patient underwent craniotomy coupled with intra-hemisphere excision of the tumor. The patient was given levetiracetam 500 mg twice a day.
The patient is stable and currently doing well.
Epidermoid cysts are slow-growing and often benign congenital tumors that comprise 0.2%-1.8% of primary intracranial neoplasms[4]. The first epidermoid cysts were described by an artist in 1807 in a French medical school[5]. The French pathologist Cruveilhier gave the first full description of epidermoid cysts[6]. From a histological point of view, epidermoid cysts often resemble the linear growth rate of the skin[5]. They are made up of a thin epithelium lining that appears pearly white and smooth macroscopically. Epidermoid tumors often have a high content of cholesterol and an internal core composed of desquamated epithelial keratin that is distinctive on MR imaging and allied radiological modalities[5].
To the best of our knowledge, intracranial epidermoid cysts are located off the midline. The most common location of epidermoids includes the region within the cerebellopontine angle (CPA)[7]. Intracranial epidermoids account for the third most common tumor in the CPA region followed by vestibular schwannoma and meningioma[7].
There have been more than 100 cases of epidermoids reported in the fourth ventricle, followed by the parasellar and sellar regions[8]. However, epidermoids may also be found in the lobes of the cerebral hemisphere, spine, and brainstem[8].
To the best of our knowledge, third ventricular epidermoid tumors are extremely rare. Patients with epidermoid tumors often present with signs and symptoms such as headache, seizures, cranial nerve defects, raised intracranial pressure, and cerebral signs[8]. Our patient presented with headache and vomiting.
Epidermoids appear as well-defined lobulated, round hypoattenuated masses on CT imaging. However, there have been reports where uniformly hyperdense epidermoids have been reported on CT imaging, which are associated with a calcium constitution or high protein content[9,10]. Epidermoids appear hyperintense on T2 weighted and hypointense on T1 weighted MRI imaging[7]. In our case, we observed a hyperintense T2 weighted mass on MRI imaging. Lastly, MR spectroscopy showed an increase in the lactate peak, which was indicative of anaerobic metabolism. There was an increase in the Cho/NAA ratio, which is generally observed in neoplasms. The Cho/Cr ratio increased to 2.85.
As per current evidence, the major differential diagnosis for a third ventricle includes arachnoid cyst, cystic neoplasm, and dermoid cyst. The differential diagnosis of different third ventricle masses based on different sequences has been mentioned in Table 1. Arachnoid cysts often appear less lobulated and follow a signal intensity patterns similar to those of cerebrospinal fluid with all MR pulse sequences including DWI and FLAIR[11]. Cystic neoplasms, such as cystic ependymoma and cystic medulloblastoma, have a varied appearance on imaging due to the varying degrees of necrosis, calcification, and hemorrhage. The solid component of these lesions often shows heterogeneous contrast enhancement and restriction on DWI[11]. Dermoid cysts are similar to epidermoid cysts, as both are lined by stratified squamous epithelium. In the context of imaging, dermoid cysts show a hyperintense signal on T1-weighted images while they appear as well-defined low attenuating (fat density) lobulated masses on CT scan[11].
| Sequences | Epidermoid | Dermoid | Arachnoid cyst | Cystic lesions medulloblastoma | Cystic lesions ependymoma |
| T1WI | Hypointense | Hyperintense | Hypointense | Hypointense | Hypointense (Solid part) |
| T2WI | Iso-hyperintense | Hypo-hyperintense | Hyperintense | Heterogenous due to calcification, necrosis, and cyst formation | Foci of blooming (hemorrhage/calcification) |
| FLAIR | Heterogenous signal higher than CSF | Hyperintense | Hypointense | Heterogeneous signal higher than CSF | Heterogeneous signal higher than CSF |
| DWI | Restricted diffusion | No restriction | No restriction | Restricted diffusion | Restricted diffusion (Solid part) |
| Contrast | Non enhancement (in malignant transformation it enhances) | Non-enhancement | Non-enhancement | Heterogeneous enhancement | Heterogeneous enhancement |
| MR spectroscopy | Choline: + NAA: - Cho/Crt: + | Choline: + NAA: - Cho/Crt: + | Choline: + NAA: - Cho/Crt: + | Choline: ++ NAA: - Cho/Crt: ++ Lipid: + Lactate: + | Choline: ++ NAA: - Cho/Crt ++ Lipid: + Lactate: + |
| MR perfusion | - | - | - | +++ (solid part) | +++ |
The patient underwent craniotomy coupled with intra-hemisphere excision of the tumor. The procedure was uneventful. The patient was administered levetiracetam 500 mg twice a day. The patient is currently doing well. The diagnosis of malignant transformation of an epidermoid cyst arising from the third ventricle is challenging. Our key strengths involved our multidisciplinary approach in diagnosing, treating, and managing the patient. Non-invasive imaging modalities such as MR spectroscopy helped us confirm the diagnosis of a malignant epidermoid cyst from the third ventricle.
We have presented a rare case of a third ventricular lesion presumed to be an epidermoid tumor as seen on MRI. The use of multimodality imaging can help radiologists diagnose uncommon tumors in unusual sites. The combination of CT, MRI, and MR spectroscopy was useful in confirming the diagnosis of a malignant epidermoid cyst arising from the third ventricle, an unusual site in routine practice.
We would like to thank Mr. Lyndon Fernandes for his medical writing assistance.
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tang GH, Wasnik AP S-Editor: Ji FF L-Editor: A E-Editor: Xing YX
| 1. | Law EK, Lee RK, Ng AW, Siu DY, Ng HK. Atypical intracranial epidermoid cysts: rare anomalies with unique radiological features. Case Rep Radiol. 2015;2015:528632. [PubMed] [DOI] [Full Text] |
| 2. | Iyer VR, Sanghvi DA. Third ventricular dermoid: an unusual tumor at an unusual site. Neurol India. 2008;56:209-210. [PubMed] [DOI] [Full Text] |
| 3. | Ozutemiz C, Ada E, Ersen A, Ozer E. Imaging Findings of an Epidermoid Cyst with Malignant Transformation to Squamous Cell Carcinoma. Turk Neurosurg. 2017;27:312-315. [PubMed] [DOI] [Full Text] |
| 4. | Patil A, Kulkarni V, Singh G, Sehrawat P. Fourth ventricle epidermoid tumor: Radiologic findings. Med J DY Patil Univ. 2016;9:136-139. [DOI] [Full Text] |
| 5. | Kaido T, Okazaki A, Kurokawa S, Tsukamoto M. Pathogenesis of intraparenchymal epidermoid cyst in the brain: a case report and review of the literature. Surg Neurol. 2003;59:211-216. [PubMed] [DOI] [Full Text] |
| 6. | Kachhara R, Bhattacharya RN, Radhakrishnan VV. Epidermoid cyst involving the brain stem. Acta Neurochir (Wien). 2000;142:97-100. [PubMed] [DOI] [Full Text] |
| 7. | Kallmes DF, Provenzale JM, Cloft HJ, McClendon RE. Typical and atypical MR imaging features of intracranial epidermoid tumors. AJR Am J Roentgenol. 1997;169:883-887. [PubMed] [DOI] [Full Text] |
| 8. | Man XR, Kanodia A, Nicholas R, Main G. A rare case of third ventricular epidermoid cyst as seen by newer MRI sequences. Int Neuropsychiatr Dis J. 2014;2:68-77. [DOI] [Full Text] |
| 9. | Giannotta SL, Pauli F, Farhat SM. Epidermoid cyst of the third ventricle. Surg Neurol. 1976;5:164-166. [PubMed] [DOI] [Full Text] |
| 10. | Aribandi M, Wilson NJ. CT and MR imaging features of intracerebral epidermoid--a rare lesion. Br J Radiol. 2008;81:e97-e99. [PubMed] [DOI] [Full Text] |