Published online May 28, 2018. doi: 10.4329/wjr.v10.i5.46
Peer-review started: February 13, 2018
First decision: April 11, 2018
Revised: April 23, 2018
Accepted: May 23, 2018
Article in press: May 23, 2018
Published online: May 28, 2018
Processing time: 106 Days and 10.1 Hours
Tears of peroneus brevis tendon represent a cause of underdiagnosed lateral ankle pain and instability. The typical clinical presentation is retro-malleolar pain, in some cases associated with palpable swelling around the fibular malleolus, pain during activities and difficulty in walking. We present a case of peroneus brevis split lesion with superior peroneal retinaculum avulsion in a young athlete who referred to the emergency ward of our hospital for left ankle pain after an inversion injury. An early diagnosis allowed treating the injury and promptly resuming sport activity, after rehabilitation training. Surgical reconstruction key-points and post-surgical follow-up were also discussed. A late diagnosis would have caused a symptomatology worsening and an increased recovery time.
Core tip: The article is based on the findings observed in a patient who was followed in our institution for a split lesion of the peroneus brevis after an inversion ankle sprain. Split lesion of peroneus brevis is usually under diagnosed, therefore we want to highlight the importance of ancillary sign, as detachment of an osseous fragment seen on the X-ray, since an early diagnosis can allow the patient to reduce recovery time. In the manuscript, we also provide post-operative ultrasound imaging which can be helpful during follow-up for monitoring the patient and to help him to restart sport practices.
- Citation: Fischetti A, Zawaideh JP, Orlandi D, Belfiore S, SIlvestri E. Traumatic peroneal split lesion with retinaculum avulsion: Diagnosis and post-operative multymodality imaging. World J Radiol 2018; 10(5): 46-51
- URL: https://www.wjgnet.com/1949-8470/full/v10/i5/46.htm
- DOI: https://dx.doi.org/10.4329/wjr.v10.i5.46
The peroneus longus (PL) and brevis (PB) arise from the posterolateral surface of the fibula and the fascia of their homonymous muscle. Peroneal tendons share a common synovial sheath and pass posteriorly to the fibular malleolus, inside the retro-malleolar groove: At this level, they are stabilized by the superior peroneal retinaculum (SPR). Usually, the peroneus brevis tendon locates antero-medially to the peroneus longus. On the lateral surface of the calcaneus the tendons run superficial to the calcaneofibular ligament (CFL) and lateral to the talo-calcanear ligaments[1].
Distal to the CFL the tendons run superior (PB) and inferior (PL) to the peroneal trochlea on the lateral calcaneal wall, kept in place by the inferior peroneal retinaculum (IPR). The PB inserts on the base of the fifth metatarsal bone while the PL have a wide insertion on the lateral aspect of the base of the first metatarsal bone and the lateral side of the medial cuneiform. Both tendons are plantar flexors of the ankle and everters of the subtalar and mid-tarsal joints. Tears of peroneus brevis tendon are a frequent cause of underdiagnosed lateral ankle pain and instability. Several studies confirm that these lesions are more common than previously believed[2]. They represent frequently an overlooked clinical condition[3]. The typical clinical presentation is retro-malleolar pain, in some cases associated with palpable swelling around the fibular malleolus, pain during activities and difficulty in walking.
Patients usually do not remember a specific episode of trauma, however, in case of misdiagnosed peroneal lesion, they often mention chronic lateral ankle instability symptoms, which went on even for years[2]. We report a case of a young athlete with a traumatic SPR avulsion and associated PB split lesion, to highlight the crucial role of associated conditions such as a flat retro-malleolar groove in the development of such an injury also including imaging findings, clinical characteristics, and treatment options in order to reduce risk of recurrence or any further instability.
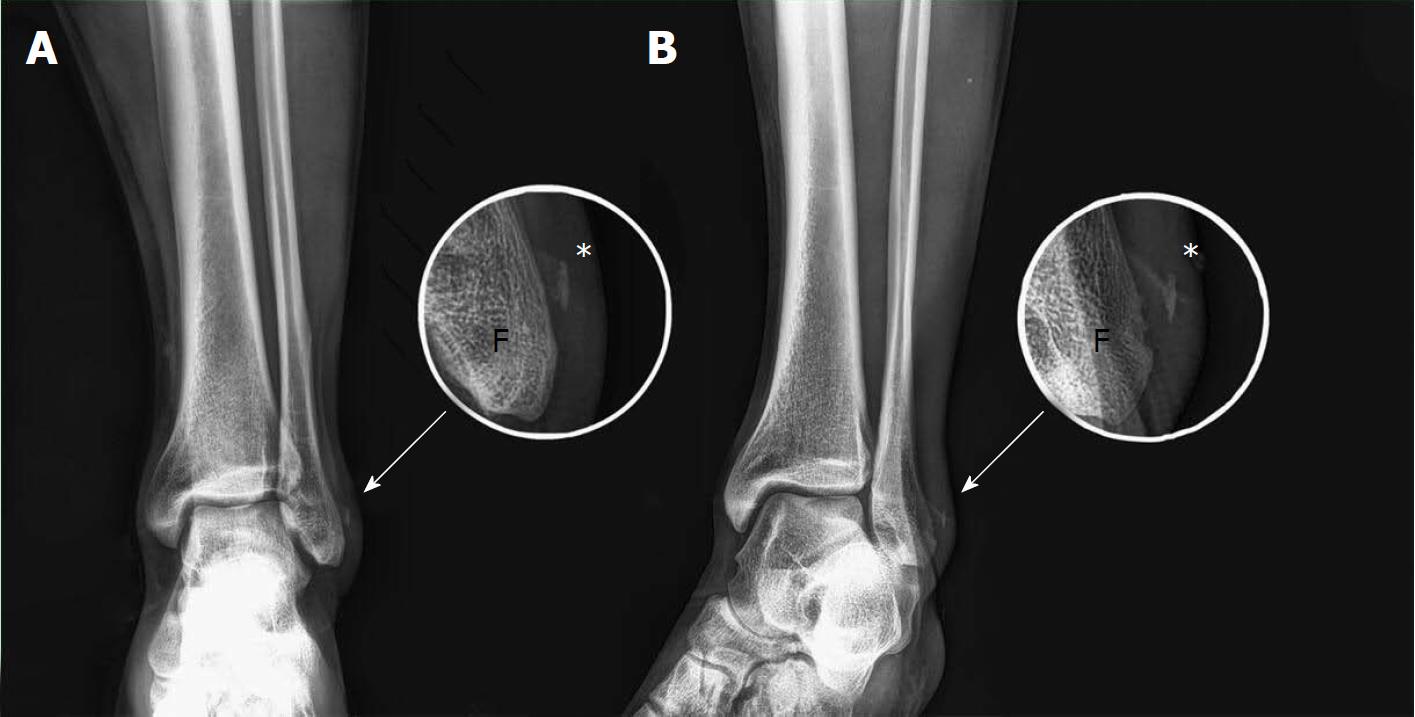
A 27 years old man presented at the emergency department with pain at the left ankle after an inversion injury; the lateral aspect of the ankle was swollen with only minor subcutaneous hematoma on the fibular malleolus. The patient reported no history of recent trauma. Plain films of the ankle were done to evaluate the bone status: The exam excluded fracture of the ankle, but revealed the detachment of an osseous fragment from the lateral aspect of the fibular malleolus (Figure 1). We suspected a traumatic lesion of the SPR and the lateral tendon compartment of the ankle. An ultrasound (US) examination was immediately performed by the on-call radiologist with a portable system (My Lab Alpha, Esaote Biomedica, Italy, equipped with a 3-13 Mhz linear probe), to evaluate the possible involvement of the lateral compartment ligaments and tendons of the ankle, usually damaged after an inversion ankle injury.
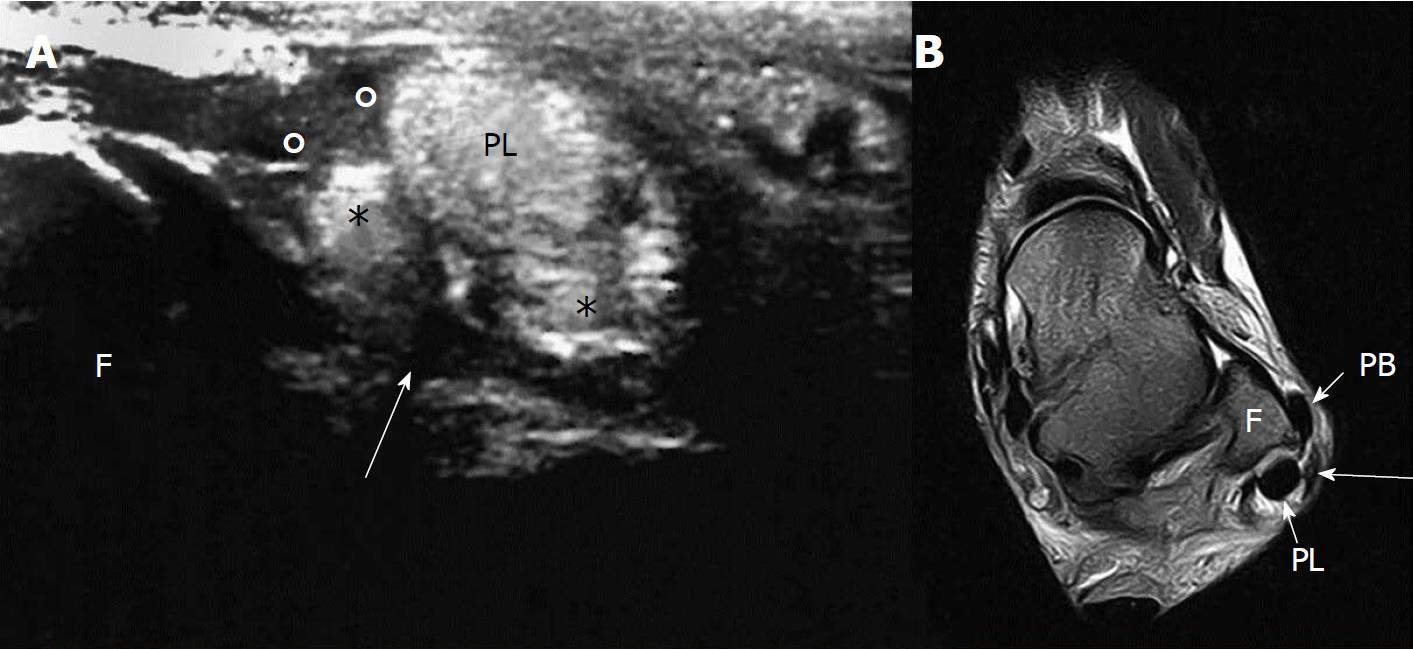
US examination demonstrated a diffuse swelling at the posterolateral aspect of the fibular malleolus with complete tear of the SPR and consequent instability of the PB (Figure 2A), which tended to the anterior subluxation at dynamic tests (flexion, extension and eversion of the foot). Moreover, US examination shows also a split lesion of the PB, which on axial US scan appears divided in two hemi-tendons at the level of deflection point on the fibular malleolus, with PL lying in the middle and separating them. The longitudinal tear of the PB had a distal extension of around 2 cm without involvement of the distal insertion on the base of the fifth metatarsal bone. Only minor anterior talofibular ligament (aTFL) sprain and no significant involvement of CFL or tibiofibular syndesmosis were found. The patient evaluation was completed with a magnetic resonance imaging (MRI) exam, performed after one week from the injury, in prevision of surgery (Figure 2B). Sequences T1-w, T2-w and with Short Tau Inversion Recovery in the three planes of the space were used. MRI examination confirmed the PB split lesion extended more distally than that showed by US examination (around 4 cm). No involvement of the distal PB insertion was found.
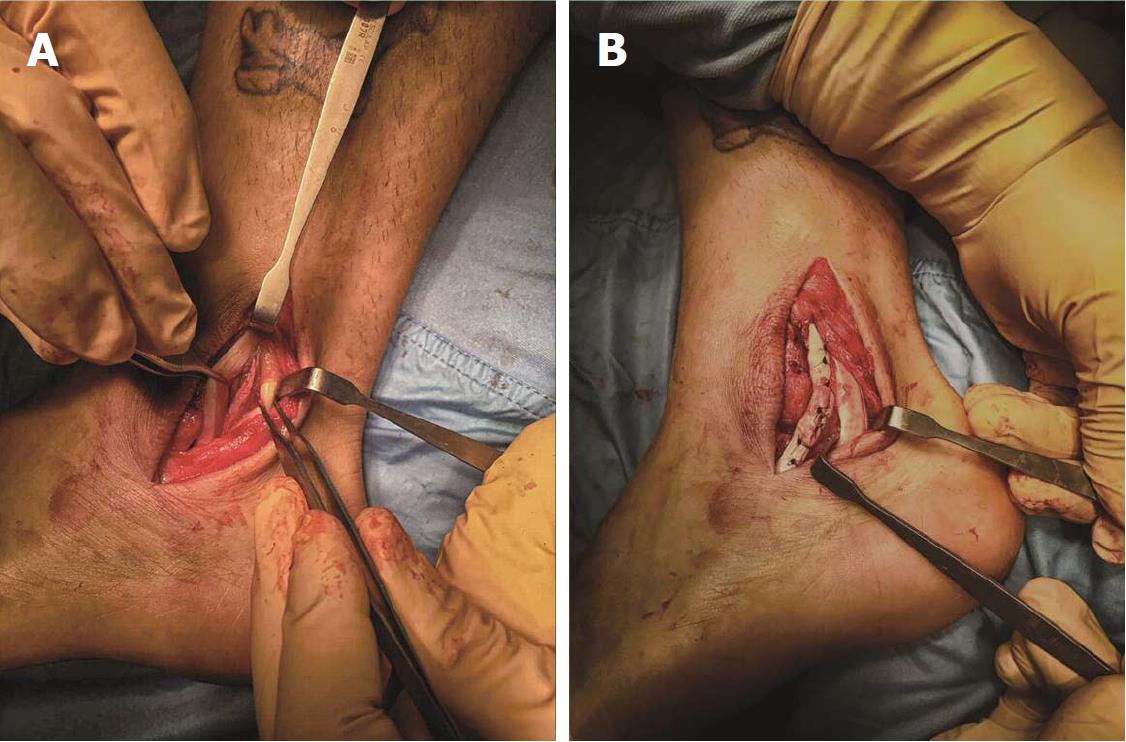
MRI also detects the avulsion of the fibular insertion of the SPR and a shallow retro-malleolar groove with associated anterior luxation of the peroneus brevis tendon. Furthermore, MRI showed a minor bone bruise of the distal tibial epiphysis and tibio-talar joint effusion. The anterior talo-fibular ligament was thickened but undamaged. The deltoid ligament presented fibro-scarring alterations, by previous trauma.No significant alterations affected the other tendons of the ankle. Surgery started with a curve incision of the posterolateral aspect of the ankle that revealed diffuse swelling of the SPR that was completely detached from its anterior insertion (Figure 3A). A wide longitudinal tear of the PB was also confirmed, with anterior luxation of the medial hemi-tendon, which represent about the 70% of the total PB.
Incision of the IPR was performed in order to expose the whole extension of the longitudinal tear, then, after curettage of the damaged edges of the peroneus brevis tendon, a lateral side-to-side suture of PB was done. IPR was also sutured (Figure 3B). Subsequent moderate milling of the retro-malleolar groove in order to restore physiological concavity and SPR reinsertion with a trans-osseous wiring was performed, using interrupted sutures are passed through the fibula and SPR in a horizontal fashion. The lowest 2 or 3 sutures were passed transosseously through the posterolateral aspect of the fibula and then through the posterior aspect of the SPR to wrap it over the peroneal tendons and minimize any chance for recurrent peroneal subluxation. A 0.054 K-wire was used for the repair holes through which No. 1.0 Vicryl suture (Polisorb, Covidien, Dublin, Ireland) can be passed[4]. The postoperative course was uneventful, the patient recovered promptly and was discharged on the same day. After surgery, a plaster cast was used for 2-6 wk; after 6-8 wk, the rehabilitation training was initiated. After approximately 12 wk, the patient could resume the sport activity.
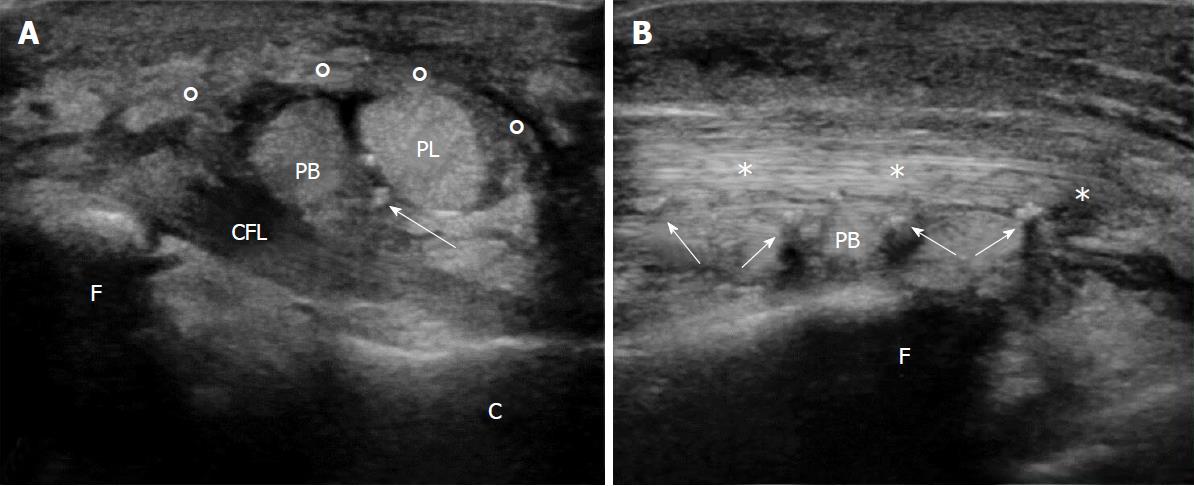
The patient was followed up with clinical and ultrasound examination after four weeks. The patient referred increased stability of the ankle, and no significant discomfort. Ultrasound evaluation, performed with a high-end US apparel (Samsung RS80 Prestige, Samsung Medical, South Korea; equipped with 8-15 Mhz linear probe) revealed a mild residual swelling at the level of the reconstructed SPR, which appear continuous, with correct localization of the peroneal tendons in the retro-malleolar groove, PB tendon was also continuous and showed several hyperechoic spots on its course due to the suture wires (Figure 4). US scan during dynamic maneuvers demonstrated an excellent peroneal tendons stability at the level of the restored retro-malleolar groove[5]. The clinical follow-up examination performed after 6 mo from surgery confirmed the stability of PB; the treatment allowed the patient to restart sport practices after the rehabilitation program. The patient referred no symptoms during sport activity and an optimal performance during the sport events.
PB resides in a vulnerable position, between the retro-malleolar groove and the peroneus longus tendon: during the dorsiflexion of the foot, it is compressed by the peroneus longus against the fibular malleolus. Moreover, the vascular supply to the tendon is reduced inside the fibular groove; finally the anatomic variants afore mentioned compromise the competence of SPR, reducing the stability of the peroneus brevis tendon[6]. When a tear occurs, the peroneus longus tendon migrates forward into the peroneus brevis, determining a split lesion. The association with SPR injury causes the dislocation of the tendon out of the fibular groove. There are many anatomic variants that predispose to PB disease: (1) Morphology of the retro-malleolar groove: In the 82% of the population it has a concave aspect; flat or convex aspects predispose to lateral dislocation and PB longitudinal tears. This condition could lead to peroneal instability and spontaneous dislocation, however, like in the presented case and in more than 60% of patient no symptoms or abnormalities could be detected at clinical evaluation[7]; (2) Peroneus Quartus Muscle: The most common accessory muscle of the ankle (12%-22% of the population), accessory muscle, that arises from the distal third of the lateral fibula, to insert on calcaneus or cuboid, passing posterior to peroneal tendons. It is usually asymptomatic, but it may produce impingement inside of the retro-malleolar groove and predispose to peroneus brevis tendon dislocation and tears; and (3) Low-lying PB muscle belly: Is an abnormally distal extension of the PB muscle at the level of the retro-malleolar groove and predispose to peroneal tendon diseases and SPR injuries.
PB split lesions are visible on US investigation and are lesions of continuity that affected the long axis of the tendon[8]. The exams should be performed with static and dynamic imaging (flexion, extension and eversion), along short and long axis, with the patient in supine decubitus and the ankle internally rotated[9]. Split lesion causes the formation of two hemi-tendons, usually different in size, that surround the peroneus longus tendon. Frequently, fluid distension of the synovial peroneal tendon sheath with increased vascularity at power Doppler are associated[8].
The diagnosis of peroneus brevis split lesion is typically formulated in the basis of clinical examination and US, but MRI is useful to evaluate the suffering of the subchondral bone and the extension of the tendon lesion, possible predisposing factors and helpful for planning the appropriate treatment[3,6]. MRI exam should be performed in the three planes axial, coronal and sagittal, with patient in supine decubitus and the ankle in neutral position[9]. Our protocol includes T1-w sequences in coronal and sagittal planes, T2-w sequences with and without fat suppression in the three planes and a PD sequence in coronal plane for their high contrast characteristic. On axial MRI images, the damaged PB assumes a characteristic “C shaped” or “chevron shaped”[5] configuration, that envelops the peroneus longus tendon, migrated anteriorly. The central portion of the tendon becomes very thinned and, in some case, it may be not well visualized.The longitudinal tear can be visualized also in the other planes, coronal and sagittal. The rupture of the SPR is associated with the dislocation of the tendon, laterally to the fibular malleolus. In our case, the rupture of the SPR, and, consequently, the peroneal tendon involvement, was suspected at the radiograph, suggesting a timely diagnosis and an early treatment.
Treatment of peroneus brevis tendon tears is initially conservative, with rest, ice, compression, and elevation (RICE), anti-inflammatory can also be prescribed to reduce inflammation and pain therapy and orthotics[6]. Refractory case, with associated lateral ankle pain and instability, or anatomic variants and SPR lesions need to undergo to surgical intervention, such as debridement, re-suturing and attachment of the tendon. If lateral ankle instability is present, the tendon lesion should be repaired at the same time of the ligament stabilization[2]. The longitudinal lesion is repaired with a side-to-side suture, combined with the reconstruction of SPR and the excision of the degenerative tissue.
The results of the surgical treatment are satisfactory in most patients[2], usually with a restored level of activity and without any further instability. Also different surgical techniques were proposed for peroneal tear and instability (e.g., bone block procedures, tissue transfer procedures, and rerouting procedures), however, the advantages of the proposed approach include better cosmesis, less soft tissue dissection, no wound retraction needed, detection of coexisting pathology, less postoperative pain, less peritendinous fibrosis, and less subjective tightness at peroneal tendons[10,11]. This case suggests that timely integrated imaging could be helpful not only in order to diagnose peroneal injuries but also to detect associated conditions that could be extremely relevant for surgical planning. This is extremely important in the management of the athletes, which have to rapidly resume sports activities after an accident. Split lesion of PB is usually underdiagnosed: In this case, radiograph findings were immediately suspected for a lateral compartment lesion, confirmed by second level exams. The early diagnosis allowed the patient to reduce recovery time and promptly restart sport practices. Moreover, ultrasound imaging, thanks to its dynamic capabilities, can be an effective practical option for evaluating lateral ankle instability, especially in cases of partial SPR tears and slight peroneal tendon subluxation.
Left ankle pain after an inversion injury, muscle functional impairment.
Swollen left ankle.
Differential diagnosis includes fibular malleolus fracture.
Unremarkable laboratory examination.
A radiography of the ankle excluded bone fracture but revealed the detachment of an osseous fragment; ultrasound demonstrated a diffuse swelling at the posterolateral aspect of the fibular malleolus and a split lesion of the peroneus (PB); MRI scan confirmed the PB split lesion and detects the avulsion of the fibular insertion of the superior peroneal retinaculum (SPR) and a shallow retro-malleolar groove with associated anterior luxation of the peroneus brevis tendon.
RICE treatment consists of rest, ice, compression, and elevation, anti-inflammatory can also be prescribed to reduce inflammation. Surgical treatment involves a side-to-side suture, combined with the reconstruction of SPR and the excision of the degenerative tissue.
This case suggests that integrated imaging is helpful for injury diagnosis and surgical planning. Unclear images, such as small bone detachment at plain films can be precious hints for the detection of underlying tendon pathology.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Ma DL, Robertson GA S- Editor: Ji FF L- Editor: A E- Editor: Tan WW
| 1. | Sconfienza LM, Orlandi D, Lacelli F, Serafini G, SIlvestri E. Dynamic high-resolution US of ankle and midfoot ligaments: normal anatomic structure and imaging technique. Radiographics. 2015;35:164-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Karlsson J, Wiger P. Longitudinal Split of the Peroneus Brevis Tendon and Lateral Ankle Instability: Treatment of Concomitant Lesions. J Athl Train. 2002;37:463-466. [PubMed] |
| 3. | Dombek MF, Lamm BM, Saltrick K, Mendicino RW, Catanzariti AR. Peroneal tendon tears: a retrospective review. J Foot Ankle Surg. 2003;42:250-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 129] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 4. | van Dijk PAD, Vopat BG, Guss D, Younger A, DiGiovanni CW. Retromalleolar Groove Deepening in Recurrent Peroneal Tendon Dislocation: Technique Tip. Orthop J Sports Med. 2017;5:2325967117706673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Neustadter J, Raikin SM, Nazarian LN. Dynamic sonographic evaluation of peroneal tendon subluxation. AJR Am J Roentgenol. 2004;183:985-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Major NM, Helms CA, Fritz RC, Speer KP. The MR imaging appearance of longitudinal split tears of the peroneus brevis tendon. Foot Ankle Int. 2000;21:514-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Molini L, Bianchi S. US in peroneal tendon tear. J Ultrasound. 2014;17:125-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Park HJ, Cha SD, Kim HS, Chung ST, Park NH, Yoo JH, Park JH, Kim JH, Lee TW, Lee CH. Reliability of MRI findings of peroneal tendinopathy in patients with lateral chronic ankle instability. Clin Orthop Surg. 2010;2:237-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Wang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics. 2005;25:587-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 143] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Taljanovic MS, Alcala JN, Gimber LH, Rieke JD, Chilvers MM, Latt LD. High-resolution US and MR imaging of peroneal tendon injuries. Radiographics. 2015;35:179-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (1)] |
| 11. | Hau WWS, Lui TH, Ngai WK. Endoscopic Superior Peroneal Retinaculum Reconstruction. Arthrosc Tech. 2017;7:e45-e51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |