Copyright
©2013 Baishideng Publishing Group Co.
World J Radiol. May 28, 2013; 5(5): 193-201
Published online May 28, 2013. doi: 10.4329/wjr.v5.i5.193
Published online May 28, 2013. doi: 10.4329/wjr.v5.i5.193
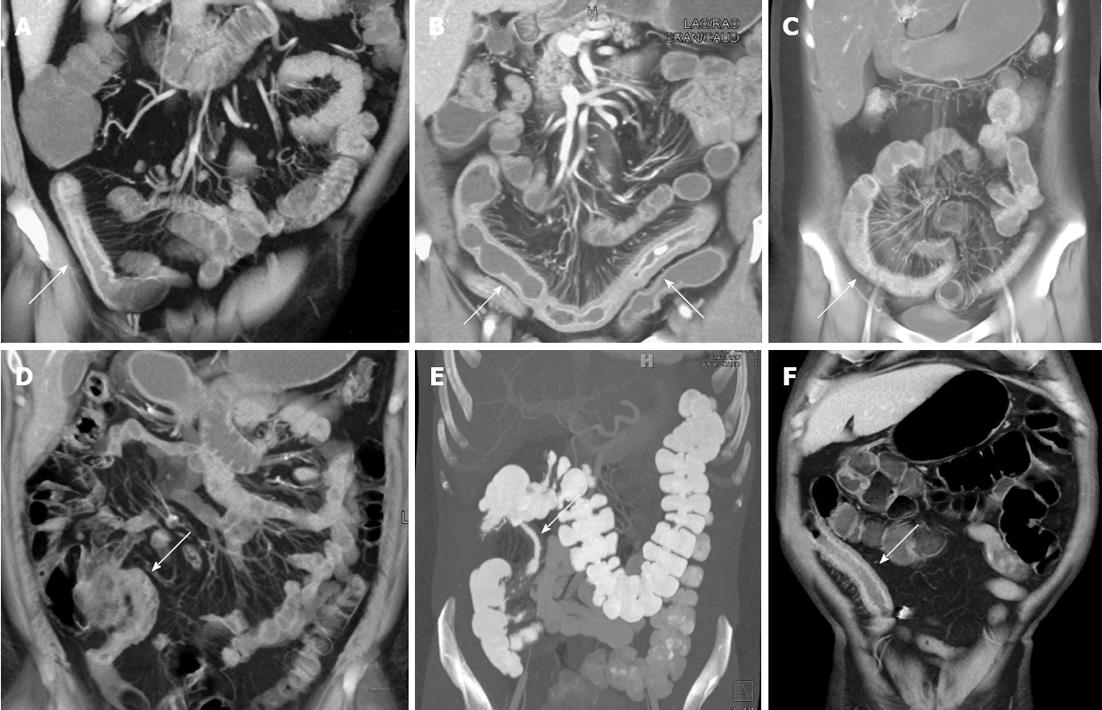
Figure 1 Active Crohn’s disease.
A: Fifty-four-year-old male with Crohn’s disease. Coronal volume rendered image demonstrates prominent wall thickening and mucosal hyperemia encompassing a 10 cm segment of ileum (arrow). The volume rendered three dimensional (3-D) image nicely accentuates the marked mesenteric hyperemia and vasa recta engorgement adjacent to the inflamed loop of bowel; B: Sixty-two-year-old male with Crohn’s disease. Coronal volume rendered images demonstrate a long segment of markedly thickened, inflamed bowel in the pelvis (arrows). Notably, the 3-D images accentuate the marked engorgement of the vasa recta (“comb sign”) adjacent to the inflamed loop of bowel; C: Twenty-two-year-old with Crohn’s disease. Coronal volume rendered image demonstrates an acutely inflamed loop of colon (arrow) with mucosal hyperemia and wall thickening, as well as adjacent engorgement of the vasa recta; D: Thirty-eight-year-old male with Crohn’s disease. Coronal volume rendered image demonstrates thickening and mucosal hyperemia of the terminal ileum, a classic appearance and location for acute Crohn’s related inflammation; E: Thirty-four-year-old male with Crohn’s disease. Coronal volume rendered image demonstrates thickening of an intermediate length segment of terminal ileum (arrow); F: Sixty-year-old male with Crohn’s disease and history of prior ileal resection and reanastomosis. Coronal volume rendered image demonstrates marked thickening, mucosal hyperemia, and adjacent vasa recta engorgement of the neo-terminal ileum (arrow).
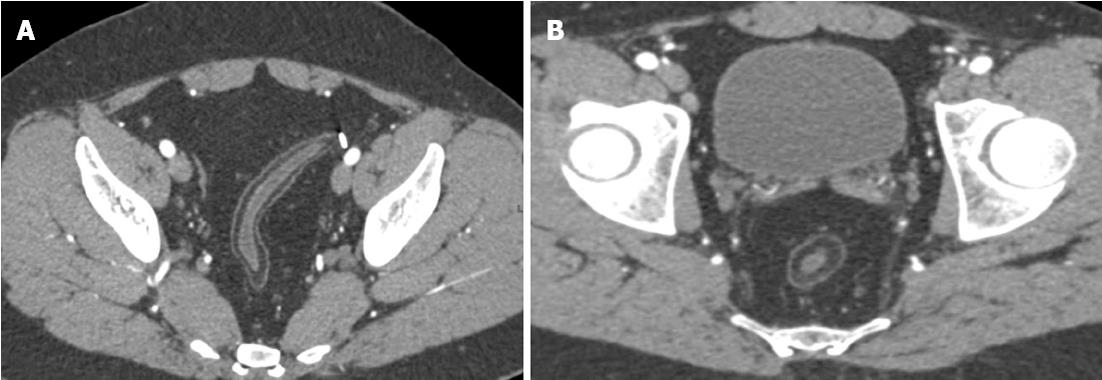
Figure 2 Sequela of chronic Crohn’s related bowel inflammation.
Twenty-seven year-old male with Crohn’s disease. Axial images demonstrate diffuse fat deposition in the wall of the rectosigmoid colon (A, B), as well as marked fibrofatty proliferation (“creeping fat”) (B) surrounding the rectum.
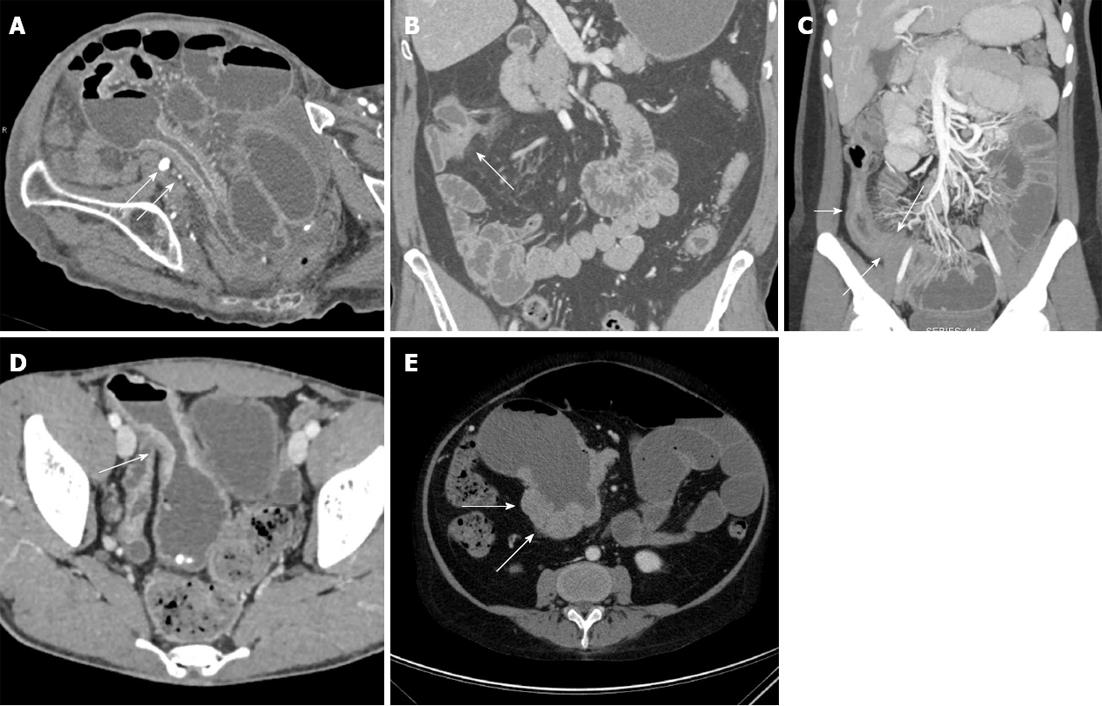
Figure 3 Bowel-related complications of Crohn’s disease.
A: Eighty-four-year-old who presented with abdominal pain. Axial contrast-enhanced image demonstrates multiple dilated loops of small bowel, in keeping with a small bowel obstruction. This image also demonstrates a long segment of bowel wall thickening and mucosal hyperemia with luminal narrowing (arrows). Given the patient’s age, this was originally thought to represent a neoplastic or ischemic stricture, but was found to represent late-onset Crohn’s disease after surgery; B: Forty-nine-year-old male with Crohn’s disease. Coronal volume rendered computed tomography image demonstrates a short segment stricture and focal thickening of the hepatic flexure of the colon, with minimal adjacent induration, but no significant mesenteric hyperemia. This was thought to be a chronic-appearing stricture. Colonoscopy was performed to exclude an underlying neoplasm, and the patient was found to have a chronic stricture in this location without acute inflammation or evidence of tumor; C: Twenty-four-year-old female with Crohn’s disease. Coronal volume rendered image demonstrates several dilated loops of small bowel in the left abdomen, with a discrete transition point (long arrows) in the distal ileum, at the site of a long segment of narrowed, hyperemic, thickened, inflamed small bowel (short arrow); D: Twenty-five-year-old male with Crohn’s disease. Axial contrast enhanced image demonstrates thickening of a loop of small bowel in the pelvis, with dilatation proximal to the site of stricturing. Given the irregular thickening (arrow) at this site, the possibility of a malignancy could not be excluded. As a result, the patient underwent surgical resection and was found to have a small bowel adenocarcinoma; E: Fifty-one-year-old female with a history of Crohn’s disease. Axial image demonstrates nodular soft tissue thickening (arrows) surrounding an aneurysmally dilated loop of bowel in the right abdomen. This was found to represent B-cell lymphoma following surgical resection.
Figure 4 Identification of early Crohn’s disease using maximum intensity projection images.
Forty-seven-year-old male with abdominal pain. While no significant abnormality was appreciated on the axial source images or multiplanar reformats, coronal maximum intensity projection images raised the possibility of mild mesenteric hyperemia and vasa recta engorgement (circle) adjacent to the cecum. The patient underwent colonoscopy, and was found to have Crohn’s colitis.
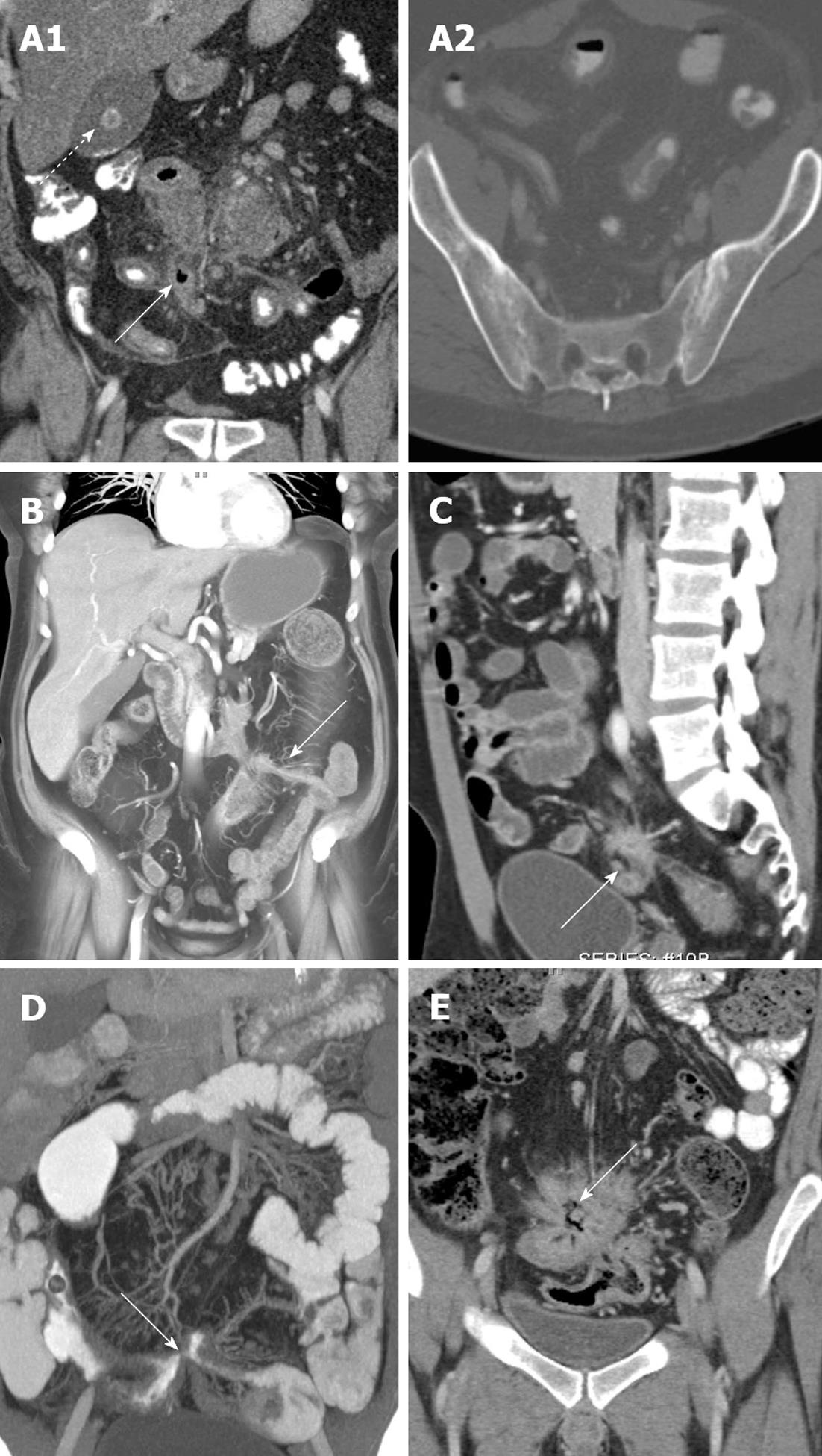
Figure 5 Fistulas and sinus tracts related to Crohn’s disease.
A: Thirty-nine-year-old male with Crohn’s disease. Coronal image demonstrates several thick-walled, inflamed loops of small bowel tethered and matted together in the right lower abdomen, with ectopic gas (solid arrow), fluid, and phlegmonous change at the center of this collection of bowel loops. While discrete fistulous tracts could not be visualized, this constellation of findings is highly suggestive of complex fistulizing Crohn’s disease. A gallstone (dashed arrow) is incidentally visualized in the gallbladder, a commonly associated finding in Crohn’s disease (A1). Image of the bony pelvis demonstrates bilateral narrowing, sclerosis, and partial ankylosis of the sacroiliac joints (A2); B: Sixty-nine-year-old male with Crohn’s disease. Coronal volume rendered (VR) image demonstrates several thickened, inflamed bowel loops in the mid and left abdomen with mucosal hyperemia and adjacent vasa recta engorgement. A clear enhancing fistulous tract (arrow) is identified connecting adjacent tethered bowel loops; C: Twenty-four-year-old male with Crohn’s disease. Sagittal contrast-enhanced image demonstrates clumping (arrow) and matting of two immediately adjacent, inflamed loops of ileum and sigmoid colon. This appearance persisted on follow-up examination, and was highly concerning for an enterocolonic fistula; D: Twenty-eight-year-old female with Crohn’s disease. Coronal volume rendered image demonstrates an enteroenteric fistulae (arrow) connecting adjacent loops of small bowel; E: Twenty-six-year-old female with Crohn’s disease. Coronal multiplanar reformatted image demonstrates multiple loops of bowel tethered together and matted in the central abdomen. Especially given the linear gas (arrow) at the center of these bowel loops, this appearance is strongly suggestive of multiple enteroenteric and enterocolic fistulae.
Figure 6 Abscesses related to Crohn’s disease.
A: Forty-three-year-old female with Crohn’s disease. Coronal and sagittal computed tomography images with contrast demonstrate a right-sided perianal rim-enhancing fluid collection/abscess (A1 and A2, arrows) with a direct tract extending from the abscess to the rectum; B: Thirty-six-year-old male with Crohn’s disease. Coronal contrast-enhanced image demonstrates a thickened loop of ileum in the right lower quadrant with marked adjacent phlegmonous change and inflammation, as well as an abscess (arrow) along the mesenteric border of the inflamed loop of bowel.
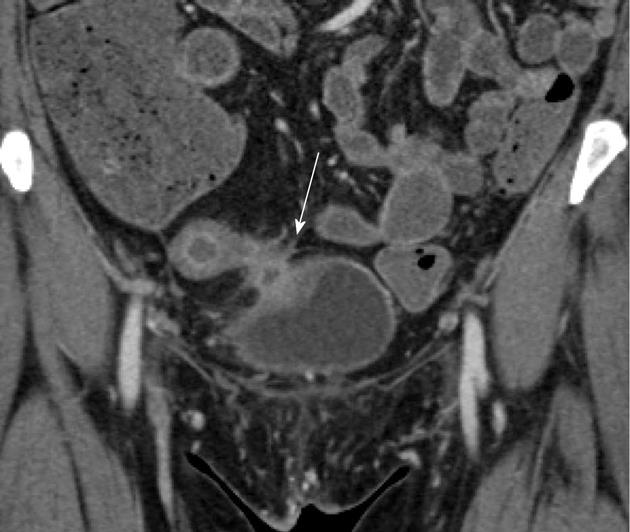
Figure 7 Enterovesicular fistula.
Fifty-two-year-old female with Crohn’s disease. Coronal contrast-enhanced computed tomography image demonstrates a markedly thickened, hyperemic loop of bowel in the pelvis, in keeping with acute Crohn’s related inflammation. The bowel loop directly abuts the bladder, which is focally thickened (arrow) at the site of contact, although no gas was identified in the bladder. The patient was ultimately proven to have an enterovesicular fistula.
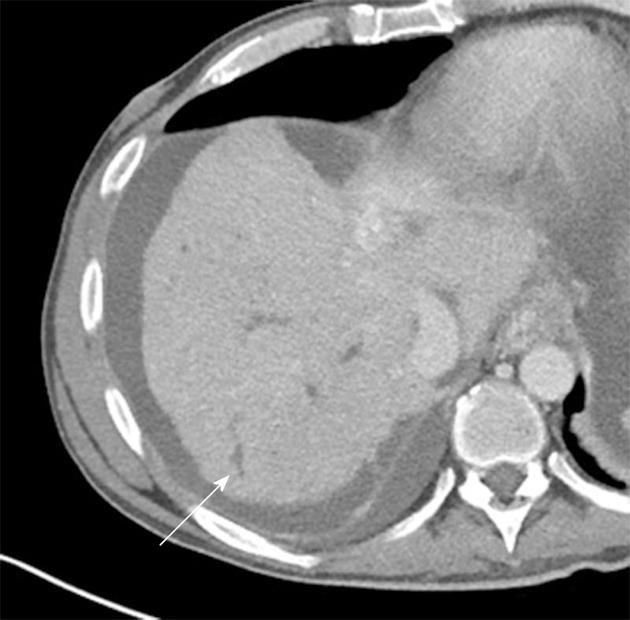
Figure 8 Primary sclerosing cholangitis and Crohn’s disease.
Twenty-four-year-old female with inflammatory bowel disease and primary sclerosing cholangitis. Axial contrast enhanced image demonstrates beading and irregular dilatation of the peripheral intrahepatic biliary tree (arrow). Massive enlargement of the caudate lobe with nodularity of the liver capsule was also noted (not shown).
- Citation: Raman SP, Horton KM, Fishman EK. Computed tomography of Crohn’s disease: The role of three dimensional technique. World J Radiol 2013; 5(5): 193-201
- URL: https://www.wjgnet.com/1949-8470/full/v5/i5/193.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i5.193