Published online Jun 26, 2025. doi: 10.4330/wjc.v17.i6.107102
Revised: April 6, 2025
Accepted: May 27, 2025
Published online: June 26, 2025
Processing time: 96 Days and 0.1 Hours
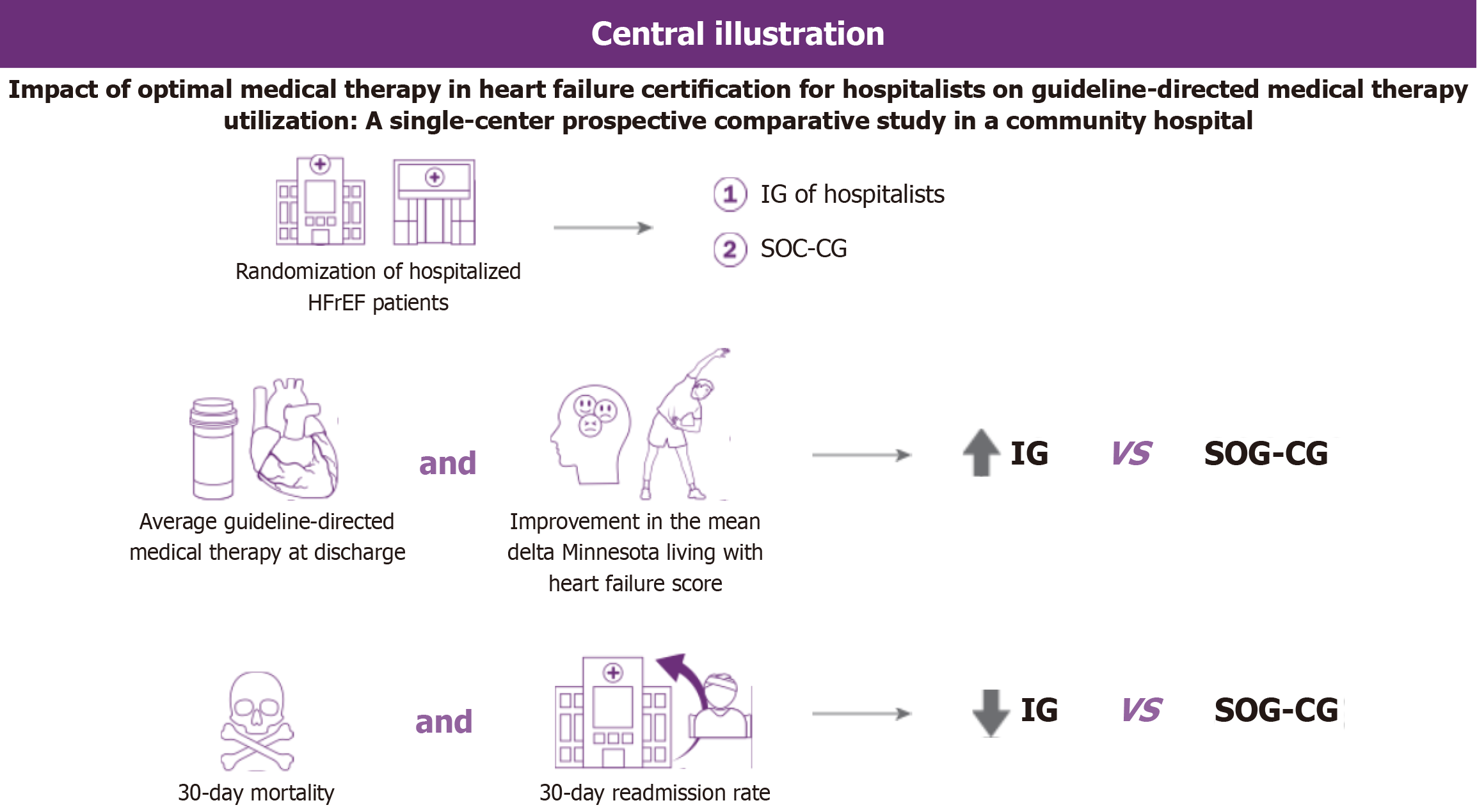
Significant gaps in guideline-directed medical therapy (GDMT) for heart failure (HF) stem from shortages of cardiologists and advanced HF providers, as well as a lack of optimal HF management knowledge among hospitalists. This study compared the impact of optimal medical therapy in HF (OMT-HF) certification on GDMT implementation and patient outcomes between an intervention group (IG) of hospitalists and a standard-of-care comparison group (SOC-CG).
To evaluate if OMT-HF has a difference in GDMT and patients in outcomes be
This study was implemented from November 2022 to May 2023. Hospitalized car
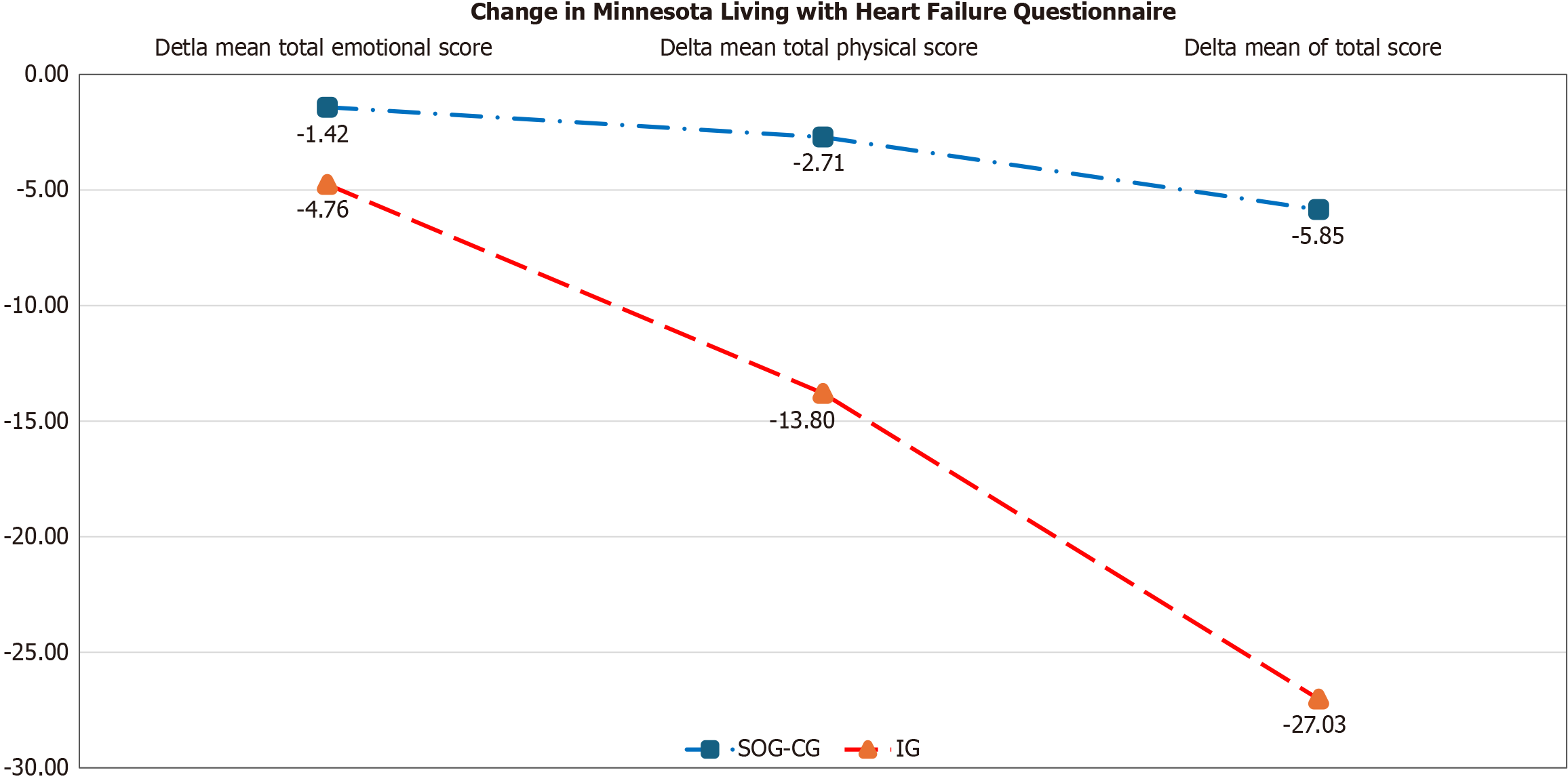
IG patients had lower readmission rates [(9 (42.85%) vs 11 (17.46%), P = 0.03] and a decreased trend in mortality 30-day post discharge. IG patients also showed greater mean improvements in total (-27.03 ± 24.59 vs -5.85 ± 23.52, P < 0.001), physical (-13.8 ± 12.3 vs -2.71 ± 11.16, P < 0.001) and emotional (-4.76 ± 8.10 vs -1.42 ± 5.98) dimensions on the MLWHFQ compared to SOC-CG, however, change in emotional dimension did not reach statistical significance.
Hospitalist OMT-HF certification may lead to better 30-day outcomes in hospitalized HF patients including quality of life, mortality and readmission rates. Larger prospective studies are warranted to validate these findings.
Core Tip: In patients with heart failure (HF) with reduced ejection fraction who are admitted to the hospital, seeing an optimal medical therapy in HF (OMT-HF) certified hospitalist can lead to improved guideline directed medical therapy scores, improved quality of life scores on the Milwaukee Living with Heart Failure Questionnaire 30 days post-discharge and lower 30-day readmission rates compared to those who did not see an OMT-HF certified hospitalist.
- Citation: Ishaq F, Nguyen DT, Graviss EA, Ebunlomo E, Bhimaraj A, Fida N. Impact of optimal medical therapy in heart failure certification for hospitalists on guideline-directed medical therapy utilization. World J Cardiol 2025; 17(6): 107102
- URL: https://www.wjgnet.com/1949-8462/full/v17/i6/107102.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i6.107102
Heart failure (HF) is a public health issue that significantly impacts morbidity, mortality, and healthcare costs in the United States, with HF with reduced ejection fraction (HFrEF) representing about 50% of cases. HF is a leading cause of hospitalization in the United States[1]. A significant portion of HF patients are readmitted to the hospital, with 25 percent readmission within 30 days after discharge[2,3]. The mortality rate for patients admitted with HF is between 10% and 15%[4]. There are significant gaps in implementing evidence-based therapies, with less than 25% of HFrEF patients re
This prospective, single-center study was implemented at Houston Methodist Baytown Hospital from November 2022 to May 2023. It is approximately a 320-bed multi-specialty hospital, sees approximately 800 HF admissions per year. The study was internally funded and approved by the Institutional Review Board (No. PRO00035436). The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the Institution's Human Research Committee.
A type-2 hybrid effectiveness-implementation study with a quasi-experimental design was used, including an inter
All patients were screened daily via electronic health record system [Epic (Epic Systems, Verona, WI)] and a database maintained in REDCap (Nashville, TN, United States). Adult patients with left ventricular ejection fraction ≤ 40% were included in the study. Patients who were in cardiogenic shock, unable to consent, at high risk per Acute Decompensated Heart Failure National Registry (systolic blood pressure < 115 mmHg, blood urea nitrogen ≥ 43 mg/dL, creatine ≥ 2.75 mg/dL) criteria[7], or being considered for advanced HF therapies were excluded. Informed consent was obtained according to institution guidelines.
Implementation science shows that contextual factors affect the adoption of programs such as guideline-directed medical therapy (GDMT) optimization during HF hospitalization. We conducted an implementation needs assessment[8], identi
Data was collected at three key time points: (1) At baseline for what GDMT patients are on at home; (2) Within 48 hours of hospital admission; and (3) At discharge. We compared difference in GDMT scores between the IG and SOC-CG groups at discharge (and change from baseline to discharge) and evaluated outcomes of length of stay (LOS), 30-day mortality, readmission, and changes in QoL from baselines to 30-days post discharge.
The GDMT scores at discharge were categorized as sub-optimal (< 3), acceptable (3–4), and optimal (≥ 5), as previously described[9,10]. Minnesota Living with Heart Failure Questionnaire (MLWHFQ) responses were used for physical and emotional dimension scores on admission and at 30 days post-discharge[11]. Continuous variables were assessed for nor
A total of 84 patients with complete data and follow-up were included (63 IG, 21 SOC-CG). There was no statistical difference in the baseline demographics of the patients between the two groups. These include a median age of 62.5 years (IQR: 53.0–71.0 years), BMI of 30.44 kg/m2 ± 8.120 kg/m2, 55% male, 25% Black, and 24% Hispanic. Comorbidities included coronary artery disease (39%), atrial fibrillation (30%), diabetes (41%), hypertension (79%), hyperlipidemia (47%), sleep-disordered breathing (16%), chronic kidney disease (60%) and chronic obstructive airway disease (21%). A total of 16% had prior implantable cardioverter-defibrillator placement. Most patients were identified as New York Heart Association class 3. A total of 66% of the patients had Medicare/Medicaid, while 14% were uninsured.
Acute on chronic HFrEF was the most common diagnosis, with atrial fibrillation and non-ST-segment elevation myo
The GDMT mean total score at admission was not significantly different between the two groups. IG patients were prescribed a higher average number of core medications at discharge than were SOC-CG patients (2.26 ± 1.2 vs 2 ± 0.95, P ≤ 0.01). At discharge, more IG patients (36, 57.1%) were prescribed mineralocorticoid receptor antagonist compared to SOC-CG patients (6, 28.57%) (P = 0.042). The differences in the prescription of other core GDMT medication groups were not significant. There was no statistically significant difference in the GDMT scores between the two groups (SOC-CG: 2.8 ± 1.7 vs IG: 3.4 ± 2.0, P = 0.19) (Table 1).
| Did patient see an optimal medical therapy in heart failure certified provider | |||
| No (n = 21) | Yes (n = 63) | P value | |
| GDMT score at discharge | |||
| Number of core medications at discharge (mean ± SD) | 2 ± 0.95 | 2.26 ± 1.2 | < 0.001 |
| Number of core medications at discharge | 0.43 | ||
| 0 | 1 (4.76) | 6 (9.52) | |
| 1 | 5 (23.81) | 10 (15.87) | |
| 2 | 9 (42.86) | 16 (25.39) | |
| 3 | 5 (23.81) | 23 (36.50) | |
| 4 | 1 (4.76) | 8 (12.7) | |
| On at least one core medication at discharge | 20 (95.7) | 57 (88.5) | 0.67 |
| GDMT total score, mean at admission (mean ± SD) | 1.29 ± 1.8 | 1.32 ± 1.7 | 0.65 |
| GDMT total score, mean at discharge (mean ± SD) | 2.8 ± 1.7 | 3.44 ± 2.0 | 0.18 |
| Optimal dosing of core medications at discharge | 0.11 | ||
| Sub-optimal (GDMT total score < 3) | 13 (56.5) | 19 (31.1) | |
| Acceptable (GDMT total score 3–4) | 5 (21.7) | 25 (41.0) | |
| Optimal (GDMT total score ≥ 5) | 5 (21.7) | 17 (27.9) | |
| Individual core medication used at discharge | |||
| Beta-blocker | 20 (95.2) | 55 (87.3) | 0.44 |
| Mineralocorticoid receptor antagonist | 6 (28.57) | 36 (57.1) | 0.04 |
| Ace inhibitor, angiotensin receptor blocker or angiotensin receptor/neprilysin inhibitor | 14 (66.6) | 41(65.07) | 1.00 |
| Sodium-glucose cotransporter-2 inhibitor | 2 (9.52) | 11 (17.46) | 0.50 |
| Ivabradine | 0 (0.0) | 0 (0.0) | -- |
| Vericiguat | 0 (0.0) | 0 (0.0) | -- |
| Hydralazine/nitrates | 4 (15.87) | 10 (15.87) | 0.74 |
| Minnesota Living with Heart Failure Questionnaire | |||
| Mean scores at admission | |||
| Total score (mean ± SD) | 53.09 ± 27.3 | 55.80 ± 26.5 | 0.69 |
| Physical dimension score (items 2, 3, 4, 5, 6, 7, 12, 13) (mean ± SD) | 25 ± 11.22 | 26.35 ± 12.11 | 0.65 |
| Emotional dimension score (items 17, 18, 19, 20, 21) (mean ± SD) | 12.76 ± 9.0 | 12.71 ± 7.4 | 0.98 |
| Mean scores at 30 days after discharge | |||
| Total score (mean ± SD) | 47.23 ± 27.5 | 28.7 ± 25.93 | < 0.001 |
| Physical dimension score (items 2, 3, 4, 5, 6, 7, 12, 13) (mean ± SD) | 22.28 ± 15.15 | 12.4 ± 12.3 | < 0.01 |
| Emotional dimension score (items 17, 18, 19, 20, 21) (mean ± SD) | 11.33 ± 7.08 | 7.9 ± 7.8 | 0.08 |
| Mean delta change from admission to 30 days after discharge | |||
| Total score delta (mean ± SD) | -5.85 ± 23.52 | -27.03 ± 24.59 | < 0.001 |
| Physical dimension score delta (items 2, 3, 4, 5, 6, 7, 12, 13) (mean ± SD) | -2.71 ± 11.16 | -13.8 ± 12.3 | < 0.001 |
| Emotional dimension score delta (items 17, 18, 19, 20, 21) (mean ± SD) | -1.42 ± 5.98 | -4.76 ± 8.10 | 0.09 |
At admission, MLWHFQ scores were similar between SOC-CG and IG groups for total (53.09 ± 27.3 vs 55.80 ± 26.5, P = 0.69), physical (25 ± 11.22 vs 26.35 ± 12.11, P = 0.65), and emotional dimensions (12.76 ± 9.0 vs 12.71 ± 7.4, P = 0.98). At 30 days post-discharge, the IG group showed greater reductions in total (-27.03 ± 24.59 vs -5.85 ± 23.52, P < 0.001) (Figure 2) and physical scores (-13.8 ± 12.3 vs -2.71 ± 11.16, P < 0.001), while emotional score changes were not significant (-4.76 ± 8.10 vs -1.42 ± 5.98, P = 0.09). As lower MLWHFQ scores reflect better QoL, these results highlight significant improve
Compared with SOC-CG patients, IG patients showed a greater improvement in the mean delta of their total (27.03 ± 24.59 vs -5.85 ± 23.52, P < 0.001), physical dimension (-13.8 ± 12.3 vs -2.71 ± 11.6, P < 0.001) and emotional dimension scores (-4.76 ± 8.10 vs -1.42 ± 5.98, P = 0.09) (Table 1).
Twelve physicians and seven mid-level providers completed the post OMT-HF course module feedback survey. Ten providers were early-career (0–5 years), three mid-career (6–15 years), and six senior-career (≥ 15 years). Provider demo
In the total cohort, the LOS was longer for patients who saw the IG group compared to those who did not [median (IQR): 6.0 (3.0–8.0) vs 5.0 (3.0–6.0), P ≤ 0.01] however, the 30-day readmission rate was lower for patients in the IG group [9 (42.85%) vs 11 (17.46%), P = 0.03].
We observed a trend toward higher 30-day all-cause mortality in SOC-CG patients compared to IG patients [1 (4.8%) vs 0 (0%), P = 0.25], though this difference was not statistically significant due to the low number of events.
Our study leverages hospitalists to optimize GDMT in HF patients during hospitalization which affords a critical opportunity to implement GDMT while the patient is being decongested and allows monitoring.
Cardiologists, given their focused expertise, often provide higher-quality HF care compared to internists, who may face challenges staying current with evolving management strategies across multiple chronic conditions[12,13]. Barriers to GDMT include clinician knowledge, patient and caregiver awareness, medication costs, and trials not fully representing real-world HF patients[14]. To address provider knowledge and workforce challenges, we equipped hospitalists with an OMT-HF certification focusing on GDMT fundamentals.
Participants responded positively to the program, with HFSA leadership, hospital administration and hospitalists collaborating to identify barriers and shaping implementation. Our study demonstrated improved trends in GDMT use, higher core medication prescriptions, and better QoL scores for patients treated by the IG. The IG also had a significantly lower 30-day readmission rate (P = 0.035), suggesting the OMT-HF course as a cost-effective method to bridge GDMT knowledge gaps, leading to improved outcomes. Prior studies have shown complex relationship between LOS and both readmission rate and mortality[15,16]. Extended LOS in IG patients may reflect the severity of illness or more mindful treatment, leading to improved decongestion[17,18], though this was difficult to evaluate[19]. A short LOS may lead to missed opportunities for up-titration of GDMT, patient education and post discharge planning, including early follow-up and care coordination[5,20]. Studies have shown that 57% of patients remain congested at 5 days of hospitalization, and premature discharge corelate with increased risk of cardiovascular death or rehospitalization within 180 days[19]. As mortality and readmission rates were lower in the IG group, it may reflect that a longer LOS with mindful treatment, in conjunction with optimal care across the continuum of care post discharge, can improve outcomes[20-23]. The mean delta in the emotional score on MLWHFQ did not reach statistical significance. This may be due to variance in resources avai
The MLHFQ is a widely used tool that assesses the physical and emotional dimensions of health-related QoL in HF patients. Higher scores indicate poorer QoL, and several studies have linked elevated scores to worse clinical outcomes[10]. Our results suggest that empowering hospitalists through focused programs such as OMT-HF can expedite patient care without the need to wait for a specialist; its application should be explored through other providers and settings. We did not exclude real-life conditions, such as consultation with cardiology, for external validity.
The study faced several limitations: (1) A delayed start due to the severe acute respiratory syndrome coronavirus 2 pan
Additionally, data contamination would have been difficult to prevent had natural randomization between groups not occurred. Second, data on sodium-glucose cotransporter 2 inhibitors were not available, as these therapies were incor
Audits and feedback were delivered through a single virtual seminar, which potentially may not have fully captured participant engagement or reception. While both hospitalist groups were well-established, we cannot exclude inherent differences in clinical practice that may have influenced outcomes.
Lastly, although the MLWHFQ is a widely validated tool, it remains a qualitative assessment. Improvements in per
Despite these limitations, we believe our initiative is replicable across other institutions and hope it inspires implemen
This study suggests that OMT-HF certification may contribute to improved GDMT adherence and QoL. Although the findings are encouraging, they are limited by the small sample size. Larger studies are needed to confirm these results, assess long-term outcomes, and explore strategies such as electronic health record alerts and structured feedback to optimize implementation. The results support the potential of hospitalist HF certification programs to help bridge gaps in care.
We extend our heartfelt thanks to John Barnes, CEO of Heart Failure Society of America, and the education staff for faci
| 1. | Agarwal MA, Fonarow GC, Ziaeian B. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017. JAMA Cardiol. 2021;6:952-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 138] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 2. | Foroutan F, Rayner DG, Ross HJ, Ehler T, Srivastava A, Shin S, Malik A, Benipal H, Yu C, Alexander Lau TH, Lee JG, Rocha R, Austin PC, Levy D, Ho JE, McMurray JJV, Zannad F, Tomlinson G, Spertus JA, Lee DS. Global Comparison of Readmission Rates for Patients With Heart Failure. J Am Coll Cardiol. 2023;82:430-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 29] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 3. | Khan MS, Sreenivasan J, Lateef N, Abougergi MS, Greene SJ, Ahmad T, Anker SD, Fonarow GC, Butler J. Trends in 30- and 90-Day Readmission Rates for Heart Failure. Circ Heart Fail. 2021;14:e008335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 164] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 4. | Alnomasy N, Still CH. Nonpharmacological Interventions for Preventing Rehospitalization Among Patients with Heart Failure: A Systematic Review and Meta-Analysis. SAGE Open Nurs. 2023;9:23779608231209220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Greene SJ, Butler J, Albert NM, DeVore AD, Sharma PP, Duffy CI, Hill CL, McCague K, Mi X, Patterson JH, Spertus JA, Thomas L, Williams FB, Hernandez AF, Fonarow GC. Medical Therapy for Heart Failure With Reduced Ejection Fraction: The CHAMP-HF Registry. J Am Coll Cardiol. 2018;72:351-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 471] [Cited by in RCA: 909] [Article Influence: 129.9] [Reference Citation Analysis (0)] |
| 6. | Yamaguchi T, Kitai T, Miyamoto T, Kagiyama N, Okumura T, Kida K, Oishi S, Akiyama E, Suzuki S, Yamamoto M, Yamaguchi J, Iwai T, Hijikata S, Masuda R, Miyazaki R, Hara N, Nagata Y, Nozato T, Matsue Y. Effect of Optimizing Guideline-Directed Medical Therapy Before Discharge on Mortality and Heart Failure Readmission in Patients Hospitalized With Heart Failure With Reduced Ejection Fraction. Am J Cardiol. 2018;121:969-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 7. | Fonarow GC; ADHERE Scientific Advisory Committee. The Acute Decompensated Heart Failure National Registry (ADHERE): opportunities to improve care of patients hospitalized with acute decompensated heart failure. Rev Cardiovasc Med. 2003;4 Suppl 7:S21-S30. [PubMed] |
| 8. | Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, Ruiter RAC, Markham CM, Kok G. Implementation Mapping: Using Intervention Mapping to Develop Implementation Strategies. Front Public Health. 2019;7:158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 354] [Cited by in RCA: 405] [Article Influence: 67.5] [Reference Citation Analysis (0)] |
| 9. | Fiuzat M, Hamo CE, Butler J, Abraham WT, DeFilippis EM, Fonarow GC, Lindenfeld J, Mentz RJ, Psotka MA, Solomon SD, Teerlink JR, Vaduganathan M, Vardeny O, McMurray JJV, O'Connor CM. Optimal Background Pharmacological Therapy for Heart Failure Patients in Clinical Trials: JACC Review Topic of the Week. J Am Coll Cardiol. 2022;79:504-510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 47] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 10. | Abraham WT, Psotka MA, Fiuzat M, Filippatos G, Lindenfeld J, Mehran R, Ambardekar AV, Carson PE, Jacob R, Januzzi JL Jr, Konstam MA, Krucoff MW, Lewis EF, Piccini JP, Solomon SD, Stockbridge N, Teerlink JR, Unger EF, Zeitler EP, Anker SD, O'Connor CM. Standardized definitions for evaluation of heart failure therapies: scientific expert panel from the Heart Failure Collaboratory and Academic Research Consortium. Eur J Heart Fail. 2020;22:2175-2186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Bilbao A, Escobar A, García-Perez L, Navarro G, Quirós R. The Minnesota living with heart failure questionnaire: comparison of different factor structures. Health Qual Life Outcomes. 2016;14:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 109] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 12. | Bazmpani MA, Papanastasiou CA, Giampatzis V, Kamperidis V, Zegkos T, Zebekakis P, Savopoulos C, Karvounis H, Efthimiadis GK, Ziakas A, Karamitsos TD. Differences in Demographics, in-Hospital Management and Short-Term Prognosis in Admissions for Acutely Decompensated Heart Failure to Cardiology vs. Internal Medicine Departments: A Prospective Study. J Cardiovasc Dev Dis. 2023;10:315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Edep ME, Shah NB, Tateo IM, Massie BM. Differences between primary care physicians and cardiologists in management of congestive heart failure: relation to practice guidelines. J Am Coll Cardiol. 1997;30:518-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 148] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | DeVore AD, Bosworth HB, Granger BB. Improving implementation of evidence-based therapies for heart failure. Clin Cardiol. 2022;45 Suppl 1:S52-S59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Sud M, Yu B, Wijeysundera HC, Austin PC, Ko DT, Braga J, Cram P, Spertus JA, Domanski M, Lee DS. Associations Between Short or Long Length of Stay and 30-Day Readmission and Mortality in Hospitalized Patients With Heart Failure. JACC Heart Fail. 2017;5:578-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 16. | Arundel C, Lam PH, Faselis C, Sheriff HM, Dooley DJ, Morgan C, Fonarow GC, Aronow WS, Allman RM, Ahmed A. Length of stay and readmission in older adults hospitalized for heart failure. Arch Med Sci. 2021;17:891-899. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Mebazaa A, Davison B, Chioncel O, Cohen-Solal A, Diaz R, Filippatos G, Metra M, Ponikowski P, Sliwa K, Voors AA, Edwards C, Novosadova M, Takagi K, Damasceno A, Saidu H, Gayat E, Pang PS, Celutkiene J, Cotter G. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial. Lancet. 2022;400:1938-1952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 457] [Article Influence: 152.3] [Reference Citation Analysis (0)] |
| 18. | Mocan D, Lala RI, Puschita M, Pilat L, Darabantiu DA, Pop-Moldovan A. The Congestion "Pandemic" in Acute Heart Failure Patients. Biomedicines. 2024;12:951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Pagnesi M, Staal L, Ter Maaten JM, Beldhuis IE, Cotter G, Davison BA, Jongs N, Felker GM, Filippatos G, Greenberg BH, Pang PS, Ponikowski P, Lombardi CM, Adamo M, Severin T, Gimpelewicz C, Voors AA, Teerlink JR, Metra M. Decongestion and Outcomes in Patients Hospitalized for Acute Heart Failure: Insights From the RELAX-AHF-2 Trial. JACC Heart Fail. 2025;13:414-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 20. | Chang GM, Tung YC. Impact of care coordination on 30-day readmission, mortality, and costs for heart failure. Am J Manag Care. 2024;30:e116-e123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 21. | Metra M, Adamo M, Tomasoni D, Mebazaa A, Bayes-Genis A, Abdelhamid M, Adamopoulos S, Anker SD, Bauersachs J, Belenkov Y, Böhm M, Gal TB, Butler J, Cohen-Solal A, Filippatos G, Gustafsson F, Hill L, Jaarsma T, Jankowska EA, Lainscak M, Lopatin Y, Lund LH, McDonagh T, Milicic D, Moura B, Mullens W, Piepoli M, Polovina M, Ponikowski P, Rakisheva A, Ristic A, Savarese G, Seferovic P, Sharma R, Thum T, Tocchetti CG, Van Linthout S, Vitale C, Von Haehling S, Volterrani M, Coats AJS, Chioncel O, Rosano G. Pre-discharge and early post-discharge management of patients hospitalized for acute heart failure: A scientific statement by the Heart Failure Association of the ESC. Eur J Heart Fail. 2023;25:1115-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 48] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 22. | Krishna P. Assuring a Continuum of Care for Heart Failure Patients Through Postacute Care Collaboration: An Integrative Review. Prof Case Manag. 2022;28:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 23. | Chang GM, Chen JY, Kuo WY, Tung YC. Associations of continuity and coordination of care with outcomes and costs after discharge among patients with heart failure: A nationwide population-based study. Int J Cardiol. 2022;353:54-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 24. | Celano CM, Villegas AC, Albanese AM, Gaggin HK, Huffman JC. Depression and Anxiety in Heart Failure: A Review. Harv Rev Psychiatry. 2018;26:175-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 317] [Article Influence: 52.8] [Reference Citation Analysis (0)] |