Published online Jun 27, 2025. doi: 10.4240/wjgs.v17.i6.107351
Revised: April 18, 2025
Accepted: May 9, 2025
Published online: June 27, 2025
Processing time: 62 Days and 2.9 Hours
Choledochal cyst is a rare biliary tract disorder with five subtypes categorized based on the anatomical location of cystic dilatation. Type IV (which affects the intrahepatic and extrahepatic ducts) is the most common subtype in adults. Its clinical manifestations are diverse and the disease can potentially become malignant. Currently, the mainstay treatment is surgical excision which is used as a definitive treatment to prevent complications and avoid carcinogenesis. However, the surgical operation for giant choledochal cysts is technically chal
Here, we present a case of a giant choledochal cyst in an 18-year-old female. The diagnosis of patient was confirmed through magnetic resonance cholangiopancreatography. The patient developed acute cholangitis, and was treated with percutaneous transhepatic cholangial drainage to alleviate symptoms. The final treatment approach was cyst excision followed by Roux-en-Y hepaticojejunostomy, which successfully achieved excellent postoperative recovery.
Ultrasonography and magnetic resonance cholangiopancreatography can effe
Core Tip: Giant choledochal cysts are exceedingly rare in clinical practice. Here, we report a case of an 18-year-old female with a massive choledochal cyst complicated with acute cholangitis. Magnetic resonance cholangiopancreatography was performed, which facilitated the attainment of a confirmatory diagnosis, while percutaneous transhepatic cholangial drainage combined with definitive surgical intervention resulted in successful clinical outcomes. The present case highlights the critical significance of advanced imaging modalities in the diagnosis of giant choledochal cysts and highlights the efficacy of staged management (drainage followed by excision) for giant choledochal cysts. And the benefits of artificial intelligence systems for surgery are also discussed. These results provide crucial insights that can be used to optimize future diagnostic and therapeutic strategies for this rare biliary disorder.
- Citation: Wang DD, Du YY, Li YZ, Wang W, Ma TL, Xu XC, Mi C, Wang SY, Cui F, She YH, Wang MC, Yang HT. Treatment of giant choledochal cysts with combined surgery and percutaneous transhepatic cholangial drainage: A case report. World J Gastrointest Surg 2025; 17(6): 107351
- URL: https://www.wjgnet.com/1948-9366/full/v17/i6/107351.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i6.107351
Choledochal cyst, which has been renamed as biliary duct dilatation, is a congenital malformation that primarily affects female infants and children, characterized by cystic dilatation of the bile ducts[1]. Its incidence is higher among Asian populations (approximately 1:1000), with two-thirds of cases reported in Japan[2]. Patients with this condition present with an upper abdominal mass, abdominal pain, jaundice, and pancreatitis, predominantly in adults[2]. Although the exact etiology remains unclear, researchers have linked it to anomalous pancreaticobiliary ductal union, detected in 30%-70% of patients. Anomalous pancreaticobiliary ductal union refers to the fusion of the common bile duct and pancreatic duct outside the duodenal wall, allowing the reflux of pancreatic enzymes into the biliary tree. These enzymes, particularly alkaline digestive components, can degrade the biliary epithelium and stimulate hyperplasia, promoting cyst formation[3,4]. The disease is diagnosed through imaging and endoscopic modalities[5], including ultrasonography (US), computed tomography (CT), magnetic resonance imaging, and endoscopy. Although choledochal cysts are benign, they can potentially become malignant (3%-7.5%) and are considered precancerous lesions[5,6]. Patients with this condition are often treated through complete surgical excision, with Roux-en-Y hepaticojejunostomy being the recommended procedure[7].
A literature review demonstrated that most choledochal cysts are small, with diameters below 10 cm. Clinically, giant choledochal cysts are extremely uncommon. Here, we present a case of a giant choledochal cyst managed successfully with percutaneous transhepatic cholangial drainage (PTCD), cyst excision, and Roux-en-Y hepaticojejunostomy, achieving favorable postoperative outcomes. Therefore, our case provides valuable data that will guide further diagnosis, staged intervention, and surgical management of giant choledochal cysts. Importantly, this case demonstrates the efficacy of minimally invasive drainage combined with definitive anatomical reconstruction in the treatment of giant choledochal cysts.
An 18-year-old female visited our hospital with a three-month history of intermittent back pain, which worsened in the past five days. The patient had received treatment at another institution for the same symptoms but no definitive diagnosis was made, nor was appropriate treatment provided.
The patient had a three-month history of intermittent upper back pain, which aggravated for five days before hospital presentation. She was previously examined at an external clinical facility, that included US examination, which showed cholecystolithiasis with cholecystitis, biliary sludge, and cystic dilatation of the bile ducts. Thus, Xiaoyan Lidan Pian (anti-inflammatory and choleretic herbal tablets) and amoxicillin were prescribed to relieve symptoms, but this treatment was not effective. Upon admission to the hospital, further examination showed that her symptoms were similar to those of cholecystolithiasis with cholecystitis, characterized by intermittent dull pain in the right upper back, exacerbated by fatty food intake. She denied nausea, vomiting, fever, chills, jaundice, cough, or sputum production. Bowel and bladder habits were normal. Physical examination identified abdominal distension, and she reported to have experienced 5 kg weight loss during recent months.
The patient did not report a history of diabetes or hypertension.
The patient had no family history of genetic disease and none of her family members had a similar disease.
Physical examination revealed that the patient had a distended abdomen with tenderness, no rebound pain, and no yellowing of the skin, mucous membranes, or sclera.
Laboratory findings shown in (Table 1) revealed abnormal levels of liver function markers (elevated alanine aminotransferase, aspartate aminotransferase, and total bilirubin) and coagulation dysfunction (prolonged prothrombin time/international normalized ratio), but renal function markers were within normal limits.
| Parameters | |
| Hb%, 115-150 g/L | 100 g/L |
| WBC, 3500-9500/cumm | 9400/cumm |
| NE%, 40%-75% | 87.2% |
| PLT, 150000-407000/cumm | 719000/cumm |
| Serum creatinine, 39.0-76.0 μmol/L | 77.9 μmol/L |
| Serum bilirubin (total), < 21.0 μmol/L | 108.6 μmol/L |
| ALT, 6-29 U/L | 102 U/L |
| ALK phosphates, 43-130 U/L | 1083 U/L |
| PT, 9.4-12.5 seconds | 15.0 seconds |
| ALB, 42.0-56.0 g/L | 28.9 g/L |
| HBsAg, negative | Negative |
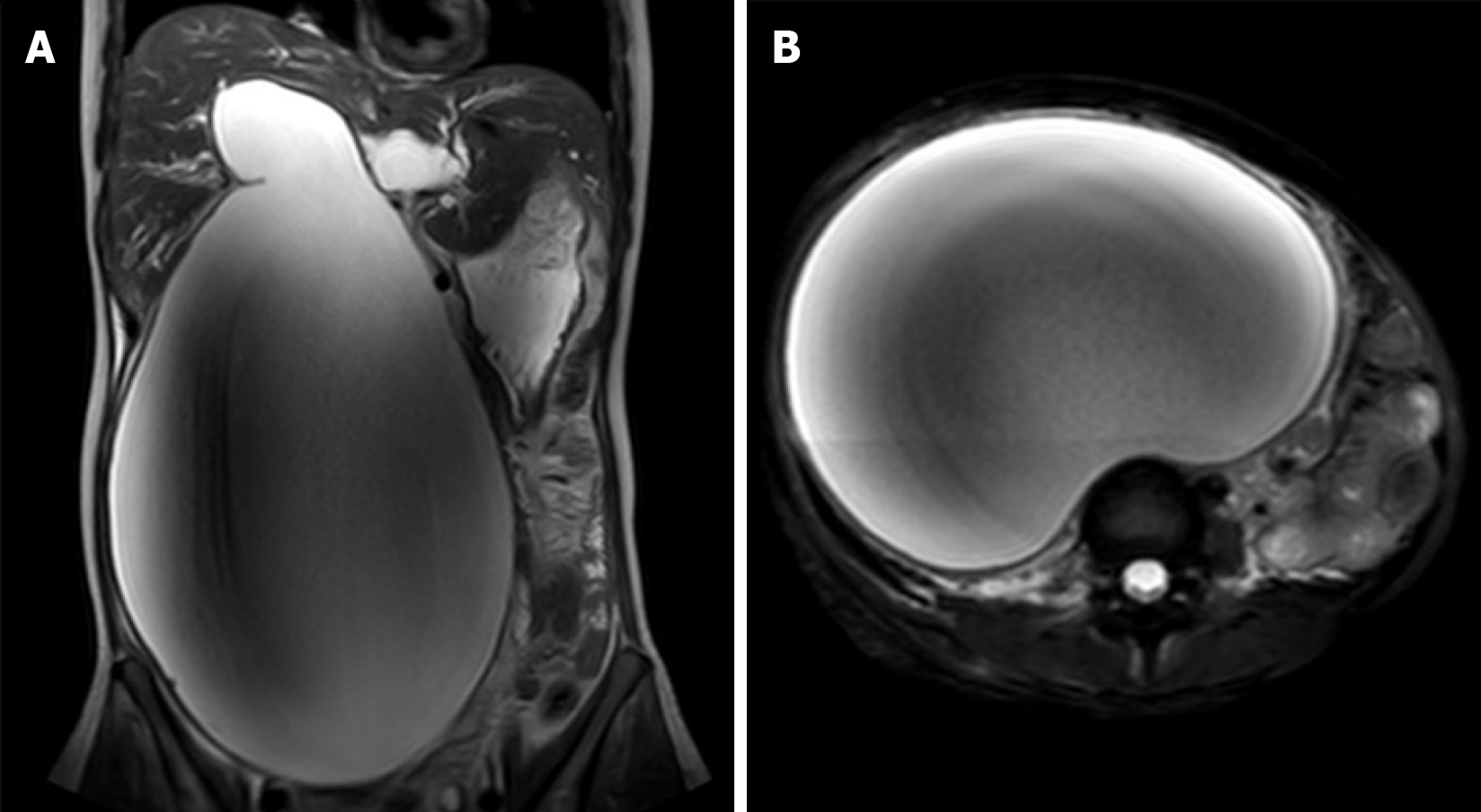
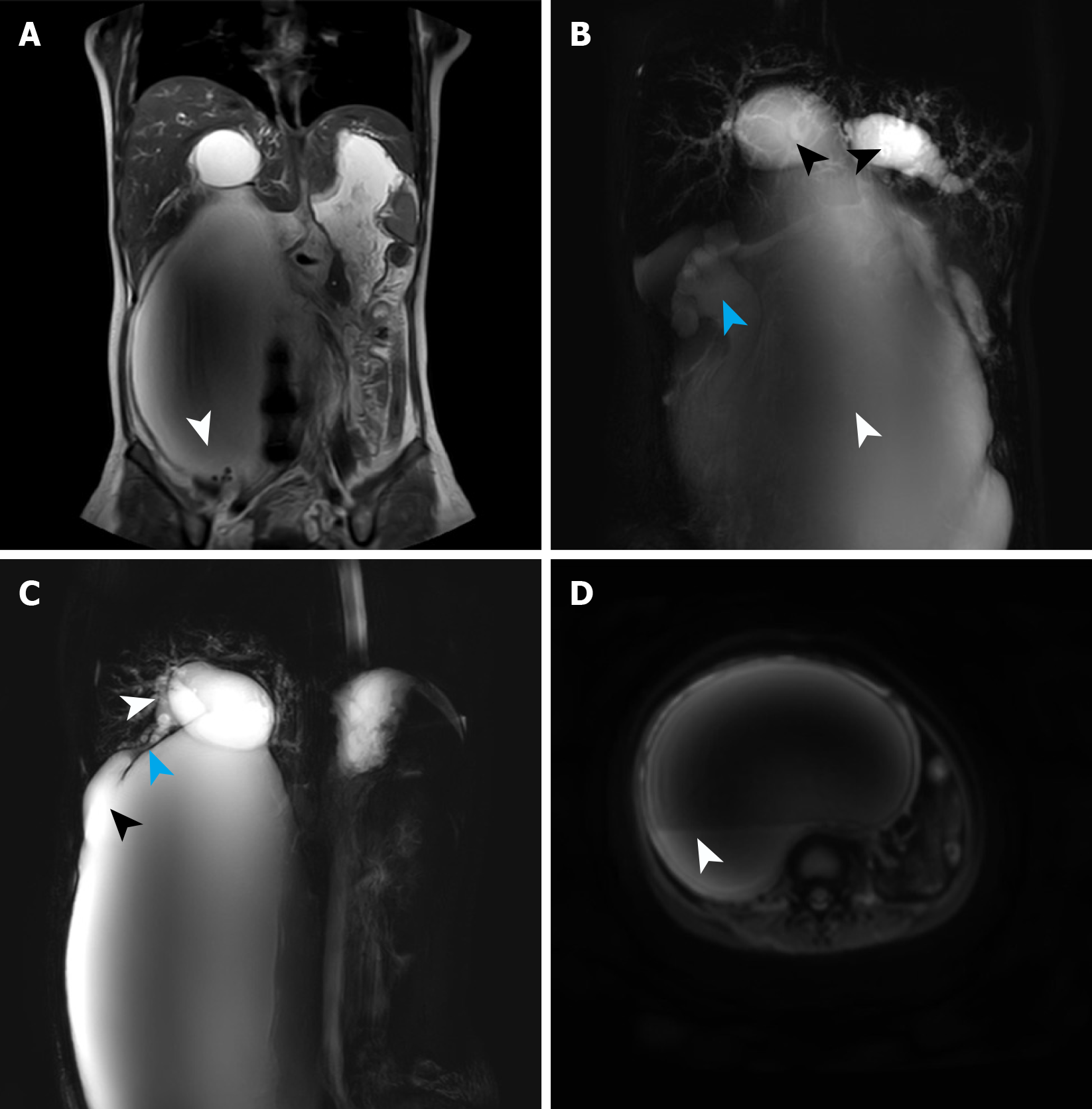
Upon admission, the patient underwent magnetic resonance imaging and magnetic resonance cholangiopancreatography (MRCP), which identified a giant cystic lesion in the abdominal cavity, measuring approximately 338.05 mm × 194.66 mm × 131.61 mm (Figure 1). Multiple calculi were observed at the cyst base (Figure 2A). Moreover, MRCP confirmed cystic dilatation of the common bile duct and intrahepatic biliary ducts, accompanied with hydronephrotic dilatation of the renal pelvis (Figure 2B), which was caused by ureteral compression by the cyst. The gallbladder was atrophic as a function of impaired bile storage and secretory function (Figure 2C). Diffusion-weighted imaging sequences (Figure 2D) revealed layering of the cystic contents, suggesting biliary sludge sedimentation. Following the classification guideline of Todani et al[8], the choledochal cysts were classified into five types. Type I is more prevalent in pediatric populations, whereas type IV (subclassified as IV-A in this case) is frequent among adults[9]. The patient in this case was diagnosed with a type IV-A choledochal cyst.
Comprehensive clinical evaluation was performed, which included patient symptoms, imaging findings, and physical examination, which led to the diagnosis of a choledochal cyst.
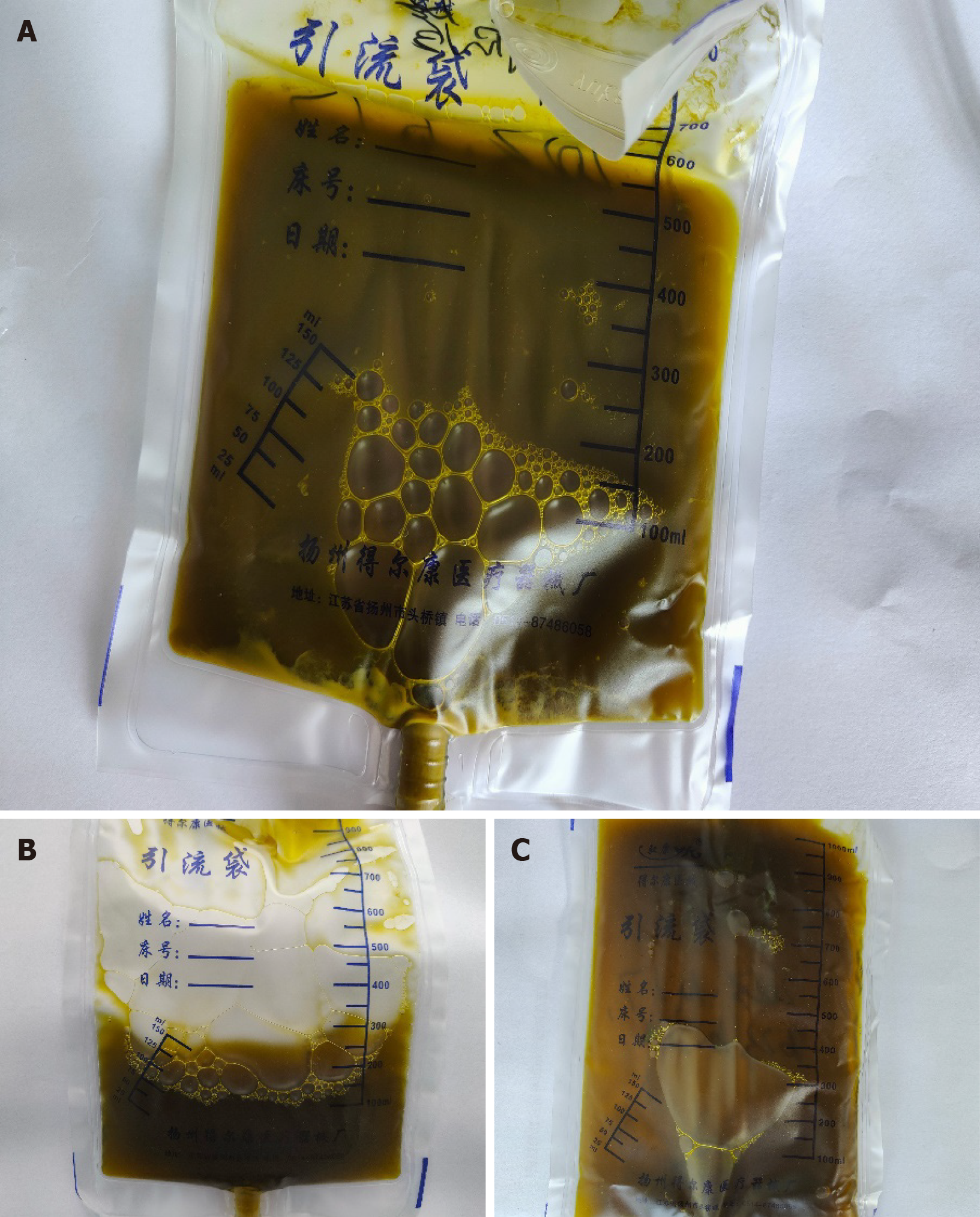
On the third day following admission, the patient developed high-grade fever (38.6 °C) presenting with chills. Consequently, cefoperazone sulbactam and dexamethasone were immediately administered to achieve fever control, and blood cultures were conducted. The culture confirmed bacteremia caused by Escherichia coli. Considering the diagnosis of acute cholangitis, PTCD was prioritized to decompress the biliary system and alleviate symptoms. During this procedure, we collected a yellow-green bile-stained fluid on the same day (Figure 3). Laboratory findings demonstrated elevated body temperature, abnormal complete blood count, and increased production of inflammatory markers (Table 2). The patient was put on empiric antibiotics therapy, which was later adjusted to imipenem and cilastatin sodium based on culture sensitivity. Once clinical stabilization was achieved, the patient was discharged with an indwelling drainage catheter for continued decompression.
| Parameters | |
| Bacterial + fungal culture | E. coli |
| PCT, 0.000-0.046 ng/mL | 0.854 ng/mL |
| IL-6, 0.00-7.00 pg/mL | 91.2 pg/mL |
| WBC, 3500-9500/cumm | 13040/cumm |
| NE%, 40%-75% | 81.37% |
| Hb%, 115-150 g/L | 68 g/L |
| PLT, 150000-407000/cumm | 334000/cumm |
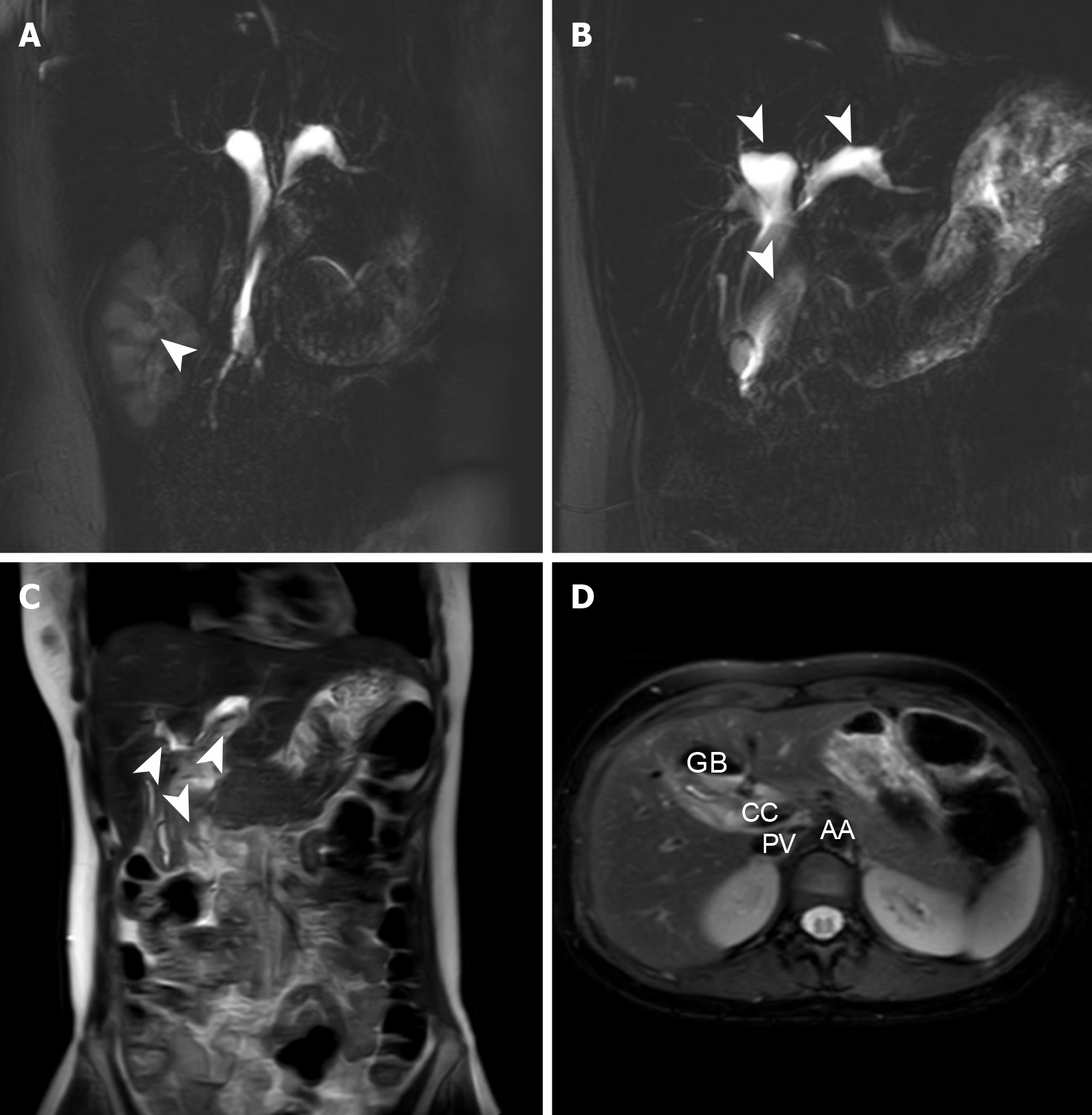
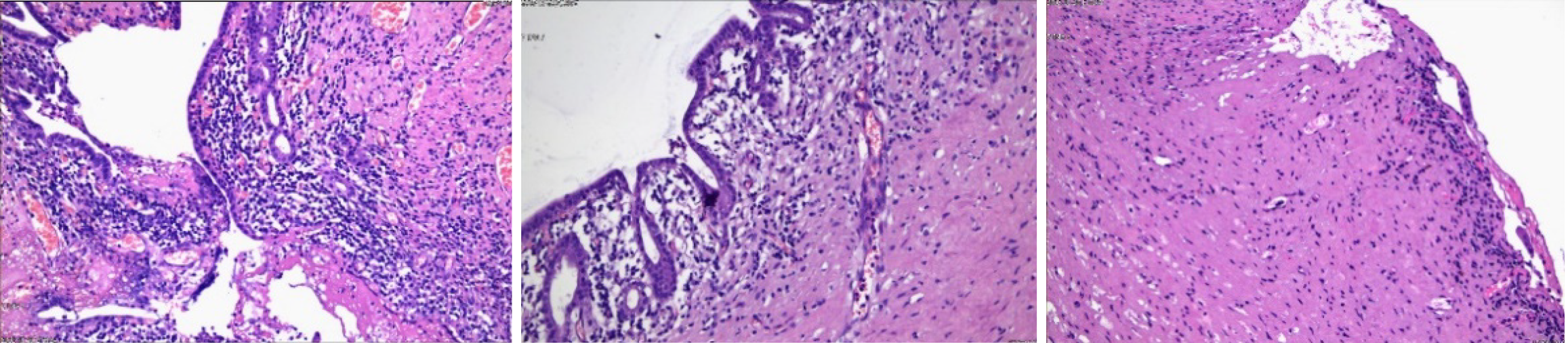
Six months later, the patient was readmitted for surgical treatment, and received a follow-up abdominal CT and MR abdominal scan + MRCP, which confirmed significant reduction in cyst expansion and hydronephrosis resolution (Figure 4). Laboratory parameters were within normal range (Table 3). Following a further clinical evaluation, the patient was deemed fit for surgery. Therefore, a comprehensive preoperative preparation was conducted, followed by cystectomy and Roux-en-Y hepaticojejunostomy through a laparoscopic approach. Postoperatively, the patient continued receiving antibiotics, fluid therapy, nutritional support, and treatment to maintain electrolyte and acid-base balance. On the first postoperative day, moderate ambulation was recommended to promote gastrointestinal function recovery. On the second day, the patient’s gastrointestinal tract became functional, and soft food was introduced. The patient did not report any discomforts. Postoperative pain was managed with opioid analgesics, which achieved good pain control. Details of the pathological findings on the surgical specimen are presented in the table below (Figure 5).
| Parameters | |
| Hb%, 115-150 g/L | 128 g/L |
| WBC, 3500-9500/cumm | 5740/cumm |
| NE%, 40%-75% | 84.10% |
| PLT, 150000-407000/cumm | 267000/cumm |
| Serum creatinine, 39.0-76.0 μmol/L | 43.9 μmol/L |
| Serum bilirubin (total), < 21.0 μmol/L | 16.4 μmol/L |
| ALT, 6-29 U/L | 59 U/L |
| ALK phosphates, 43-130 U/L | 233 U/L |
| PT, 9.4-12.5 seconds | 11.0 seconds |
| ALB, 42.0-56.0 g/L | 39.2 g/L |
| HBsAg, negative | Negative |
The patient showed satisfactory recovery and was discharged on the eighth postoperative day. Subsequently, the patient was followed up by phone 1 year after the surgery, and the patient reported no discomfort and could live a normal life.
The clinical manifestations of choledochal cyst include right upper quadrant mass, abdominal pain, high fever, chills, and jaundice. In children, the classic triad of right upper quadrant mass, abdominal pain, and jaundice is more prevalent in children than in adults (82% vs 25%)[6]. Considering the anomalous confluence of pancreatic and bile ducts, choledochal cysts can potentially induce pancreatitis, estimated to affect 20% of adults but rarely seen in children[6,10]. In addition, choledochal cysts can cause other complications, such as gallbladder stones, bile duct stones, cholangitis, liver abscess, cirrhosis, and spontaneous perforation[3,5]. Moreover, the compression caused by the cyst on the portal vein may induce portal hypertension[11]. In this case, the patient exhibited the classic triad of symptoms: Mass, abdominal pain, and jaundice, and developed cholangitis after admission. Notably, the patient’s cholangitis symptoms were resolved following percutaneous drainage and decompression, and subsequent surgical treatment achieved complete resolution of the patient’s symptoms.
The most common examination tool is abdominal US, because it is simple, quick, and harmless, making it an ideal screening method for this condition. Although US cannot visualize the entire biliary tract or its course, it can identify dilated bile ducts, facilitating diagnostic decisions[3]. CT can rapidly obtain images of the entire biliary system. Moreover, contrast-enhanced CT is highly sensitive as it visualizes bile duct wall conditions, regardless of whether bile duct obstruction is present or not, and the location of the obstruction. However, CT cannot effectively detect non-calcified stones within the biliary system[12]. To better assess the cyst and bile duct structure, imaging techniques such as endoscopic retrograde cholangiopancreatography and MRCP are recommended. These methods can display the cyst’s relationship with the bile duct, as well as its details, such as course, size, relative position, and relationship with surrounding structures. Given the non-invasive nature of MRCP, it is the preferred diagnostic method[13]. In addition, key serological markers, liver enzymes, bilirubin, and bile enzymes can facilitate the diagnosis and treatment of choledochal cysts. In the available studies, gamma-glutamyl transferase ≥ 346.5 U/L, accompanied with markedly elevated liver enzymes and bilirubin, can reflect the existence or risk of bile duct perforation[14].
The surgical treatment of choledochal cysts has two main objectives: (1) To relieve bile duct obstruction, promote smooth bile secretion, and treat recurrent cholangitis; and (2) To remove the affected bile ducts, reducing the risk of malignant bile duct tumors. Patients with choledochal cysts but normal bilirubin levels showed a significantly lower risk of malignancy (6% vs 86%), demonstrating the significance of bile enzymes in maintaining normal biliary function[12]. In cases where the gallbladder is also dilated, precipitating a positive Courvoisier’s sign, abnormal narrowing of the lower bile duct or the confluence of the pancreatic and bile ducts may occur, causing bile duct obstruction[15,16]. This phenomenon is most likely caused by a bile duct tumor, although bile duct sclerosis may be present in multiple areas of narrowing[17]. PTCD can satisfactorily relieve the symptoms of acute cholangitis. Choledochal cysts can potentially cause bile stasis and biliary calculi, accompanied with intermittent jaundice due to incomplete biliary obstruction being a hallmark feature[18]. PTCD can effectively manage acute cholangitis by decompressing the infected biliary system. Thus, early biliary drainage via PTCD is strongly recommended in choledochal cyst patients presenting with cholangitis, because it: (1) Drains infected bile, alleviating cholangitis symptoms; (2) Reduces cyst luminal pressure, facilitating cyst size reduction; and (3) Minimizes surgical complexity and perioperative complications. In clinical practice, the surgical treatment of giant choledochal cyst is technically challenging. Therefore, in all surgeries, predicting the surgical time and difficulty is crucial for providing adequate preoperative preparation and improving patient prognosis. In a retrospective study by Honda et al[19], it was observed that the maximum diameter of the cyst, the preoperative serum aspartate aminotransferase level and the diameter of the biliary anastomosis influenced the operative time. Another study demonstrated that the cyst size can prolong the operative time in pediatric patients undergoing choledochal cyst excision[20]. Other studies have shown that the size of the cyst in choledochal cysts is positively correlated with the severity of cholangitis[21]. Inflammatory changes in the bile ducts can induce extensive tissue adhesions, complicating the process of adhesion release, and increasing the risk of cyst wall damage and rupture during surgery. Additionally, cyst compression can cause displacement of the adjacent portal vein and hepatic artery, potentially leading to misjudgments of vascular positions by the surgeon, increasing the risk of vascular damage and significant blood loss during surgery[19]. It is estimated that the five-year overall survival rate after surgical resection of choledochal cysts is 95.5%[5], indicating that surgery may be the best treatment option for this condition. Recent studies have demonstrated that artificial intelligence (AI)-powered laparoscopic surgery can enhance visualization systems during operation. These systems enable surgeons to detect subtle metastatic lesions within the abdominal cavity with high precision[22], accurately identifying critical anatomical structures and laparoscopic instruments[23,24], and reliably localize vital blood vessels during minimally invasive procedures[25,26]. Therefore, integration of AI into biliary surgery can particularly reduce intraoperative collateral damage and mitigate bleeding risks. By enhancing real-time anatomical recognition and surgical navigation, AI-driven tools are expected to revolutionize complex biliary procedures, thereby improve safety and efficacy. In this patient, the coexistence of acute cholangitis and a giant choledochal cyst posed significant surgical risks, including potential intraoperative complications and poor outcomes. Thus, a staged approach combining PTCD with delayed cyst excision was adopted. Post-drainage imaging confirmed significant cyst shrinkage, enabling a safer and more efficient surgical procedure. The subsequent cyst excision and Roux-en-Y hepaticojejunostomy were completed in 3 hours and 20 minutes, with no major postoperative complications observed. The patient achieved rapid recovery and excellent long-term prognosis.
Gigantic choledochal cyst is a very rare biliary malformation, with the present case likely to be the largest ever documented choledochal cyst in literature. Multiple diagnostic methods for choledochal cysts are available, with US and MRCP deemed to be ideal for this condition. Surgical intervention is the most effective approach, as it can structurally restore the biliary malformation, prevent complications, and effectively lower the risk of cholangiocarcinoma. During the operation, surgeons should carefully release adhesions around the cyst and thoroughly dissect the cyst to achieve complete resection. AI systems are poised to improve the safety of such complex surgeries. This case demonstrates that PTCD is a safe and effective adjunct in managing giant choledochal cysts. It not only mitigates acute symptoms but also optimizes surgical conditions, ultimately enhancing operative success and patient outcomes.
We are grateful to the patient and his family for their cooperation during treatment. I am also grateful to my tutors Yang HT and Wang MC for their guidance. I appreciate the support from my colleagues in writing the manuscript.
| 1. | Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, Pawlik TM. Choledochal cysts: presentation, clinical differentiation, and management. J Am Coll Surg. 2014;219:1167-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 153] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 2. | Rahman MS, Rahman J. A choledochal cyst in an 18-year-old girl with diagnostic challenges, and outcome of surgery with a tailored procedure: A case report. Int J Surg Case Rep. 2023;110:108638. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Cazares J, Koga H, Yamataka A. Choledochal cyst. Pediatr Surg Int. 2023;39:209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 4. | Diao M, Li L, Cheng W. Timing of Choledochal Cyst Perforation. Hepatology. 2020;71:753-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Brown ZJ, Baghdadi A, Kamel I, Labiner HE, Hewitt DB, Pawlik TM. Diagnosis and management of choledochal cysts. HPB (Oxford). 2023;25:14-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 25] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 6. | Lipsett PA, Pitt HA, Colombani PM, Boitnott JK, Cameron JL. Choledochal cyst disease. A changing pattern of presentation. Ann Surg. 1994;220:644-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 222] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 7. | Eiamkulbutr S, Tubjareon C, Sanpavat A, Phewplung T, Srisan N, Sintusek P. Diseases of bile duct in children. World J Gastroenterol. 2024;30:1043-1072. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 8. | Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 934] [Cited by in RCA: 833] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 9. | Biswas J, Nath S, Ray S, Dhali A, Karpha K, Dhali GK. Giant choledochal cyst: The largest reported! Clin Case Rep. 2023;11:e6907. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 10. | Tresphory B, Calisti A. Successful Management of a Late Referred Giant Choledochal Cyst Type Ia in 8-Year-old Girl. Ann Afr Med. 2024;23:740-742. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Mrowiec S, Jabłońska B, Baron J, Gajda M, Stelmach A, Zemła P, Liszka Ł. A giant biliary cyst of Todani IA in a young woman: A case report. Medicine (Baltimore). 2021;100:e24022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 12. | Ludwig DR, Itani M, Childs DD, Revzin MV, Das KK, Anderson MA, Arif-Tiwari H, Lockhart ME, Fulcher AS. Biliary Duct Dilatation: AJR Expert Panel Narrative Review. AJR Am J Roentgenol. 2024;222:e2329671. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Jain R, Gupta A, Kandasamy D, Jana M. Imaging in Pediatric Obstructive Jaundice. Indian J Pediatr. 2022;89:899-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (1)] |
| 14. | Zhang S, Cai D, Chen Q, Zhang Y, Chen K, Jin Y, Luo W, Huang Z, Hu D, Gao Z. Value of serum GGT level in the timing of diagnosis of choledochal cyst perforation. Front Pediatr. 2022;10:921853. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Matcuk GR Jr, Grant EG, Ralls PW. Ultrasound measurements of the bile ducts and gallbladder: normal ranges and effects of age, sex, cholecystectomy, and pathologic states. Ultrasound Q. 2014;30:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Murphy K, McLaughlin P, O'Connor BR, Breen M, O'Súilleabháin C, Maceneaney P, Maher MM. Does Courvoisier's sign stand the test of time? Clin Radiol. 2012;67:e27-e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Ludwig DR, Anderson MA, Itani M, Sharbidre KG, Lalwani N, Paspulati RM. Secondary sclerosing cholangitis: mimics of primary sclerosing cholangitis. Abdom Radiol (NY). 2023;48:151-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 18. | Ciccioli C, Mazza S, Sorge A, Torello Viera F, Mauro A, Vanoli A, Bardone M, Scalvini D, Rovedatti L, Pozzi L, Strada E, Agazzi S, Veronese L, Barteselli C, Sgarlata C, Ravetta V, Anderloni A. Diagnosis and Treatment of Choledochal Cysts: A Comprehensive Review with a Focus on Choledochocele. Dig Dis Sci. 2025;70:39-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 19. | Honda M, Shimojima N, Maeda Y, Ito Y, Miyaguni K, Tsukizaki A, Abe K, Hashimoto M, Ishikawa M, Tomita H, Shimotakahara A, Hirobe S. Factors predicting surgical difficulties in congenital biliary dilatation in pediatric patients. Pediatr Surg Int. 2023;39:79. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Zhou Y, Zhang Y, Guo H, Zheng C, Guo C. Risk Factors Related to Operative Duration and Their Relationship With Clinical Outcomes in Pediatric Patients Undergoing Roux-en-Y Hepaticojejunostomy. Front Pediatr. 2020;8:590420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Jeong IH, Jung YS, Kim H, Kim BW, Kim JW, Hong J, Wang HJ, Kim MW, Yoo BM, Kim JH, Han JH, Kim WH. Amylase level in extrahepatic bile duct in adult patients with choledochal cyst plus anomalous pancreatico-biliary ductal union. World J Gastroenterol. 2005;11:1965-1970. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Chen H, Gou L, Fang Z, Dou Q, Chen H, Chen C, Qiu Y, Zhang J, Ning C, Hu Y, Deng H, Yu J, Li G. Artificial intelligence assisted real-time recognition of intra-abdominal metastasis during laparoscopic gastric cancer surgery. NPJ Digit Med. 2025;8:9. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Zygomalas A, Kalles D, Katsiakis N, Anastasopoulos A, Skroubis G. Artificial Intelligence Assisted Recognition of Anatomical Landmarks and Laparoscopic Instruments in Transabdominal Preperitoneal Inguinal Hernia Repair. Surg Innov. 2024;31:178-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 24. | Fujinaga A, Endo Y, Etoh T, Kawamura M, Nakanuma H, Kawasaki T, Masuda T, Hirashita T, Kimura M, Matsunobu Y, Shinozuka K, Tanaka Y, Kamiyama T, Sugita T, Morishima K, Ebe K, Tokuyasu T, Inomata M. Development of a cross-artificial intelligence system for identifying intraoperative anatomical landmarks and surgical phases during laparoscopic cholecystectomy. Surg Endosc. 2023;37:6118-6128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 25. | Une N, Kobayashi S, Kitaguchi D, Sunakawa T, Sasaki K, Ogane T, Hayashi K, Kosugi N, Kudo M, Sugimoto M, Hasegawa H, Takeshita N, Gotohda N, Ito M. Intraoperative artificial intelligence system identifying liver vessels in laparoscopic liver resection: a retrospective experimental study. Surg Endosc. 2024;38:1088-1095. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Ryu K, Kitaguchi D, Nakajima K, Ishikawa Y, Harai Y, Yamada A, Lee Y, Hayashi K, Kosugi N, Hasegawa H, Takeshita N, Kinugasa Y, Ito M. Deep learning-based vessel automatic recognition for laparoscopic right hemicolectomy. Surg Endosc. 2024;38:171-178. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |