Copyright
©The Author(s) 2025.
World J Gastrointest Surg. Jun 27, 2025; 17(6): 107351
Published online Jun 27, 2025. doi: 10.4240/wjgs.v17.i6.107351
Published online Jun 27, 2025. doi: 10.4240/wjgs.v17.i6.107351
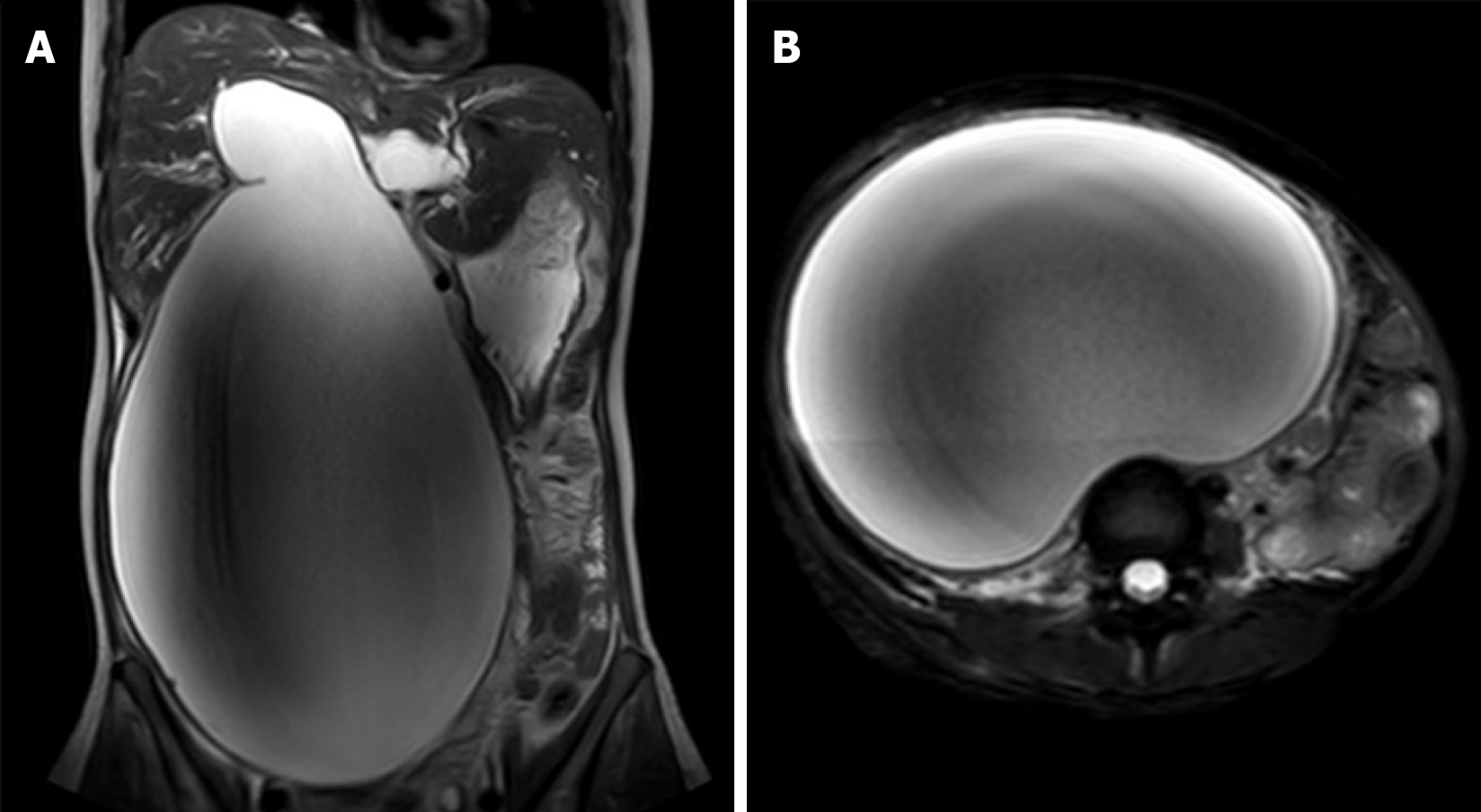
Figure 1 Abdominal magnetic resonance imaging scanning findings at first admission.
A: Representative magnetic resonance image of the upper abdomen (coronal view) reveals multiple cystic dilations of intrahepatic and extrahepatic bile ducts, suggesting type IV-A congenital biliary cystic dilation; B: The magnetic resonance image of the upper abdomen (axial view).
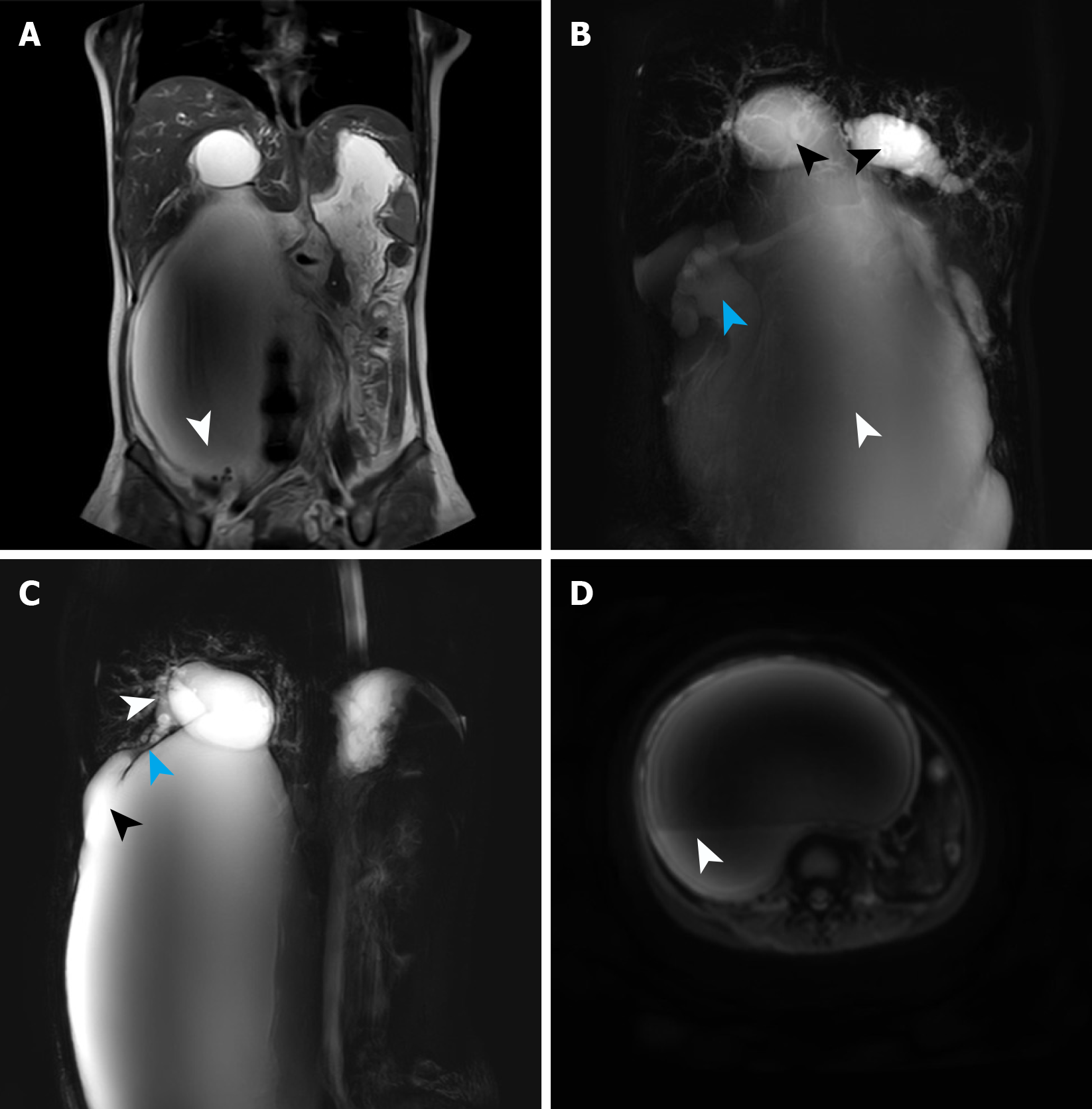
Figure 2 Magnetic resonance cholangiopancreatography findings at first admission.
A: A round filling defect was detected at the base of the dilated bile duct, suggesting the presence of a stone (white arrow); B: Magnetic resonance cholangiopancreatography revealed cystic dilation of the intrahepatic bile ducts (black arrow), accompanied with extreme dilation of the common hepatic duct and common bile duct (white arrows), presenting as a large cystic expansion. Hydronephrosis was also visualized (blue arrow); C: Magnetic resonance cholangiopancreatography demonstrated gallbladder atrophy (white arrow), narrowing of the cystic duct (blue arrow), and dilatation at the junction of the cystic duct and common hepatic duct (black arrow); D: Diffusion-weighted imaging identified a layered appearance within the cyst, with the lower layer suggesting bile sludge deposition based on its location and shape (white arrow).
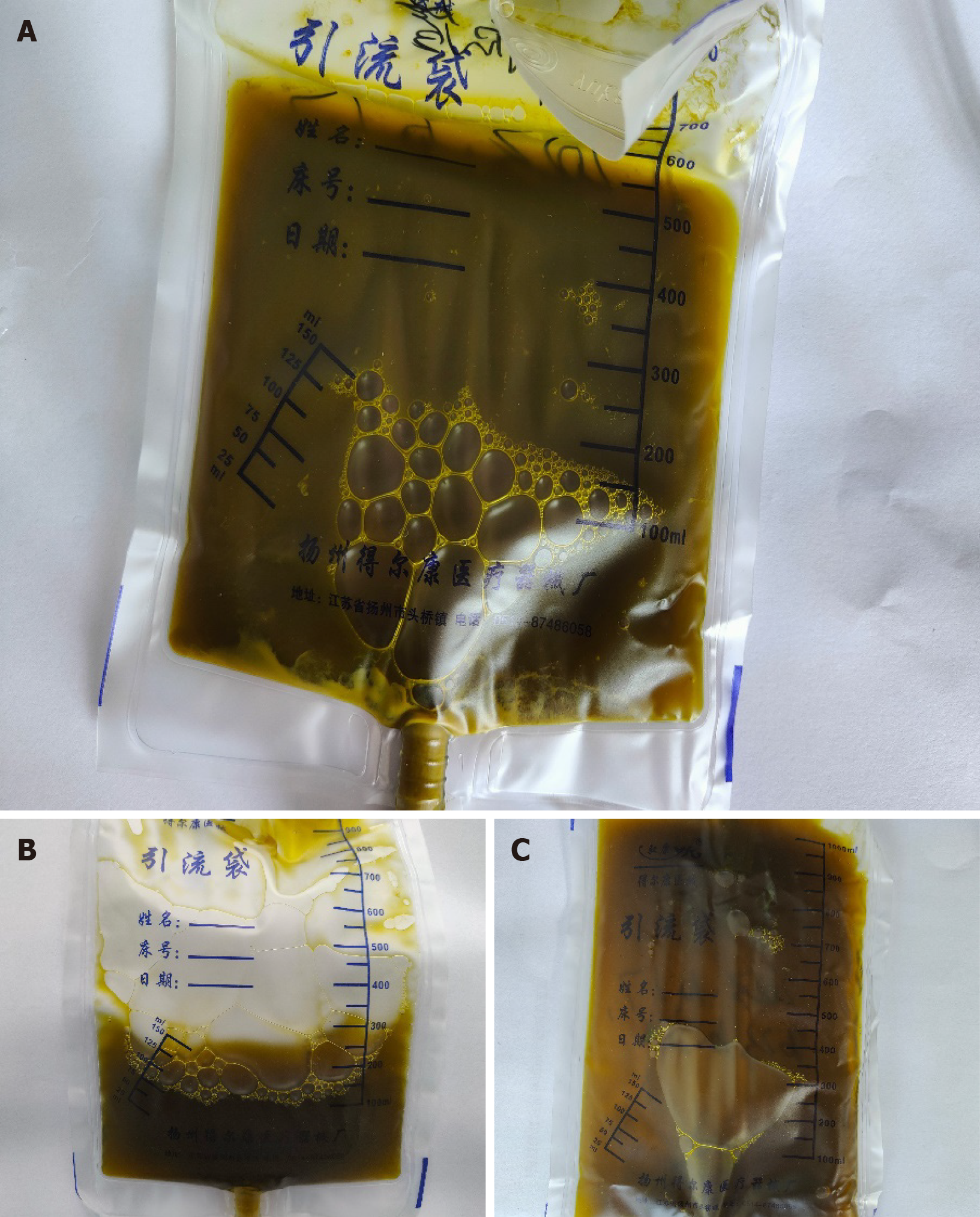
Figure 3 Changes in color and properties of percutaneous transhepatic cholangial drainage fluid.
A: The drainage fluid collected on the day of percutaneous transhepatic cholangial drainage surgery appearing dark and turbid; B: A clear drainage fluid was obtained on the first fast discharge, closely resembling normal bile; C: The drainage fluid collected during the second hospitalization for surgical treatment was clear, consistent with normal bile.
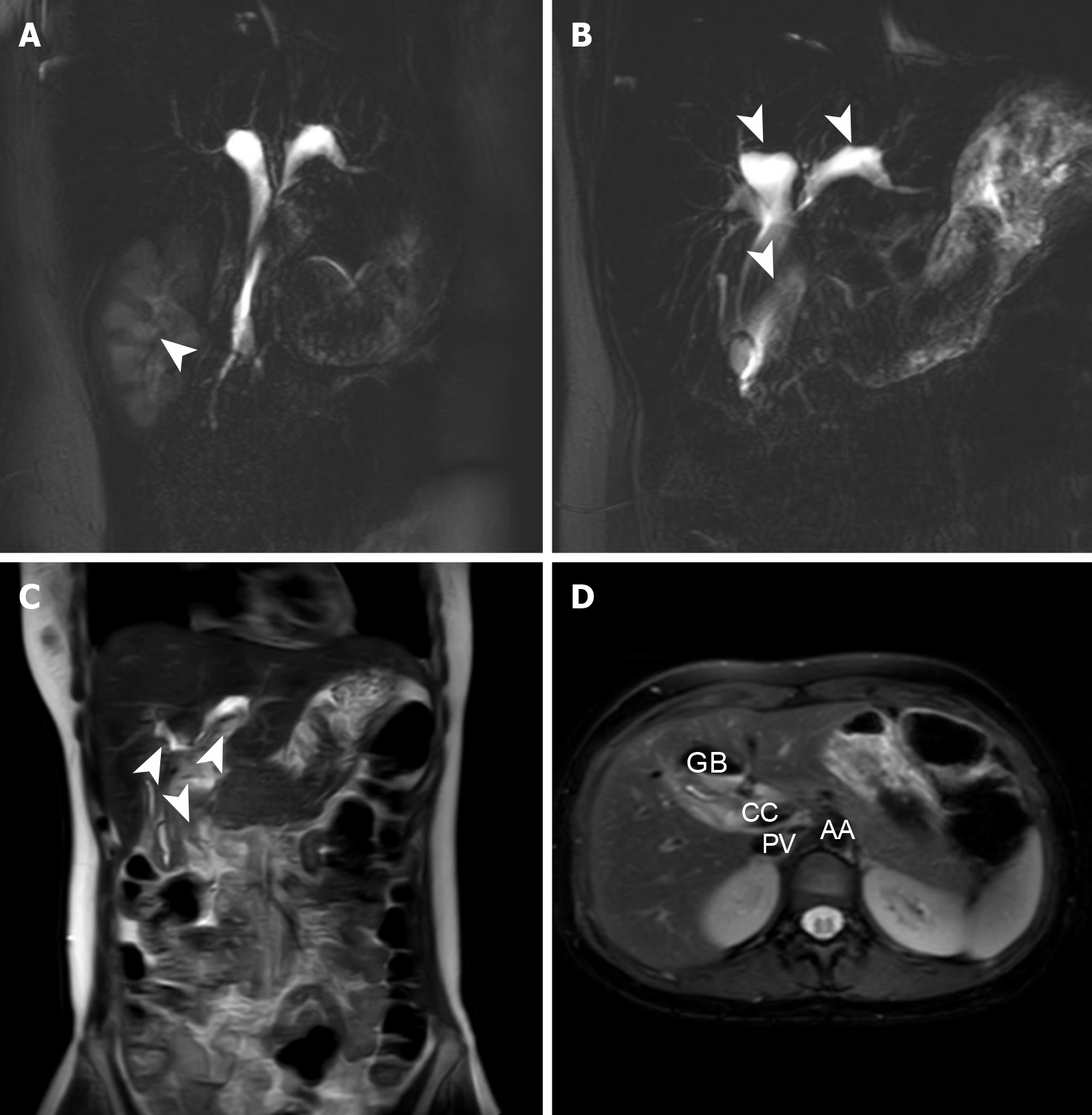
Figure 4 Abdominal magnetic resonance imaging findings at second admission.
A: Resolution of hydronephrosis (white arrow); B: Persistent dilatation of intra- and extrahepatic biliary ducts (white arrow); C: There was significant reduction in abdominal cyst size (white arrow); D: Key anatomical structures of the abdomen. GB: Gall bladder; CC: Choledochal cyst; PV: Portal vein; AA: Abdominal aorta.
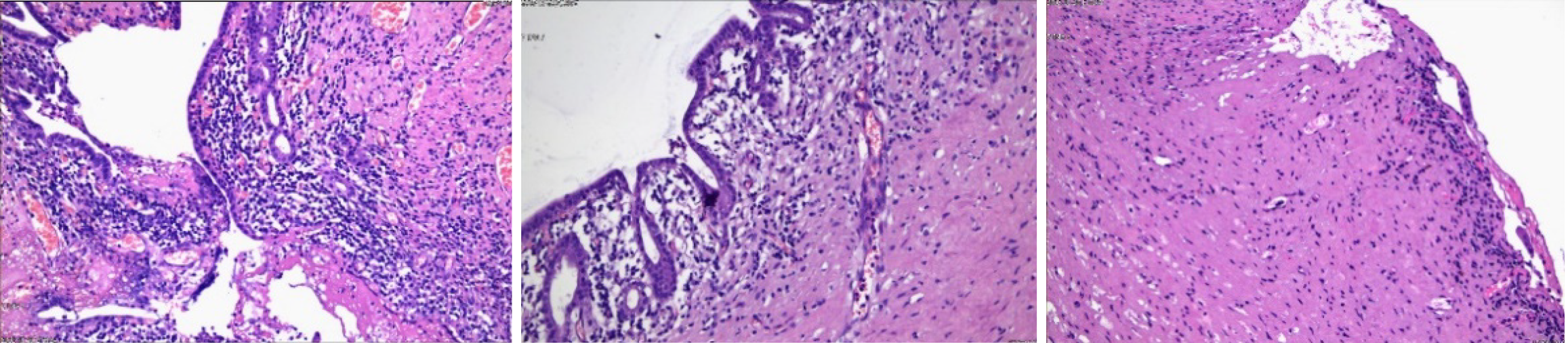
Figure 5 Postoperative pathological findings (dyeing method: Hematoxylin and eosin stain; magnifying power: 100 ×).
Examination of the surgical specimen: The submitted cyst wall presented with fibrous tissue hyperplasia, lined with a single layer of columnar epithelium, with some areas of epithelial detachment, and interstitial inflammatory cell infiltration, which suggested the presence of a choledochal cyst combined with acute and chronic inflammation.
- Citation: Wang DD, Du YY, Li YZ, Wang W, Ma TL, Xu XC, Mi C, Wang SY, Cui F, She YH, Wang MC, Yang HT. Treatment of giant choledochal cysts with combined surgery and percutaneous transhepatic cholangial drainage: A case report. World J Gastrointest Surg 2025; 17(6): 107351
- URL: https://www.wjgnet.com/1948-9366/full/v17/i6/107351.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i6.107351