Published online Aug 15, 2025. doi: 10.4251/wjgo.v17.i8.109245
Revised: May 30, 2025
Accepted: July 14, 2025
Published online: August 15, 2025
Processing time: 101 Days and 15.6 Hours
Gallbladder and biliary tract cancer (GBTC) is a highly aggressive malignant tumor with a high fatality rate. The global incidence and mortality of GBTC continue to increase, presenting a significant challenge to public health. Strategies for preventing and controlling GBTC in Brazil, Russian Federation, India, China and South Africa (BRICS) countries offer valuable lessons for other developing nations.
To investigate GBTC burden trends in BRICS countries and perform an age-period-cohort (APC) analysis of Global Burden of Disease (GBD) from 1990-2021.
Data on the incidences and crude incidence rates, the number of deaths and crude mortality rates, and the age-standardized incidence rate (ASIR) and age-standardized mortality rate (ASMR) of GBTC were obtained for BRICS countries from the GBD study 2021. Joinpoint regression analysis was employed to examine the trends in disease burden from 1990 to 2021. The APC model was utilized to assess the age, period, and birth cohort effects on the changes in GBTC disease burden worldwide and in the BRICS countries during the same time frame. Bayesian APC analysis was used to estimate the future burden.
The increases in incidence and deaths were 101.09% and 74.26%, respectively, compared with 1990. The ASMRs in Brazil, Russia, and China decreased, while those in India and South Africa increased. Among the BRICS countries, in most age groups in Brazil, Russia, India, and South Africa, the crude incidence and mortality rates in women were higher than those in men, whereas in China, the situation was the opposite. Joinpoint regression analysis revealed that from 1990 to 2021, the overall ASIR of gallbladder and bile duct cancer exhibited a declining trend. Although the incidence rate in China showed an increasing trend, the mortality rate exhibited a declining trend, which became more pronounced over time.
In BRICS countries, the number of incident cases and deaths from GBTC increased between 1990 and 2021, primarily due to rapid population growth. Nevertheless, the ASIR and ASMR declined during the same period.
Core Tip: The global burden of gallbladder and biliary tract cancer (GBTC) continues to rise, with marked heterogeneity across Brazil, Russian Federation, India, China, and South Africa (BRICS) nations. Using global burden of disease 2021 data, age-period-cohort modeling revealed a 101% increase in global GBTC incidence and 74% mortality growth from 1990-2021. Declining age-standardized mortality rates were observed in Brazil, Russia, and China, contrasting with increases in India and South Africa. Male predominance in China vs female predominance in other BRICS countries was noted. Trend analysis highlighted China's unique initial decline followed by a rebound in incidence, underscoring the urgent need for targeted prevention strategies.
- Citation: Cui YL, Bao X, Liu DM, Mu H, Yu G. Gallbladder and biliary tract cancer burden trends in Brazil, Russian Federation, India, China, and South Africa in 1990-2021. World J Gastrointest Oncol 2025; 17(8): 109245
- URL: https://www.wjgnet.com/1948-5204/full/v17/i8/109245.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i8.109245
Gallbladder and biliary tract cancer (GBTC) is a highly aggressive malignant tumor associated with a high fatality rate. The global incidence and mortality of GBTC continue to increase, presenting a significant challenge to public health. Due to the insidious nature of its early symptoms, most patients are diagnosed at an advanced stage, leading to a notably poor prognosis, with a 5-year survival rate of less than 20%[1-3]. GBTC includes gallbladder cancer (GBC), intrahepatic cholangiocarcinoma, and extrahepatic cholangiocarcinoma, including perihilar cholangiocarcinoma and distal cholangiocarcinoma[4]. GBC is the most common malignancy of the gallbladder and biliary tract, accounting for 80% to 95% of all biliary tract carcinomas[5]. The incidence of GBC varies significantly by geographical region, being highest in central and eastern Asia as well as South America. For instance, it is notably elevated in countries such as China and Thailand[6,7].
The Brazil, Russian Federation, India, China, and South Africa (BRICS) nations are part of the developing world and are characterized by their rapid economic growth. These countries are increasingly dedicating a substantial portion of their economic resources to healthcare expenditure[8]. Nevertheless, they continue to encounter significant challenges in balancing the diverse needs of promoting public health, controlling non-communicable diseases, and enhancing population health.
There are significant global disparities in the burden of GBTC, with higher incidence rates observed in high-income countries, where mortality rates are declining, while middle-income and low-income countries face higher mortality rates due to limited medical resources and the burden of infectious diseases. Gender, age, race, and socio-economic status are key factors influencing the incidence and prognosis of the disease[9,10]. In the BRICS countries, there are notable differences in the incidence and mortality of GBTC, which are influenced by demographic characteristics, economic development, and healthcare infrastructure. China reports the highest incidence of GBC globally, driven primarily by risk factors such as gallstones and chronic typhoid infection[11]. India shows a moderate incidence of GBTC, with a similar incidence rate in both genders, and major risk factors include gallstones and chronic infections[12]. In Russia, the incidence of GBC is higher in males, with lifestyle factors such as smoking and alcohol consumption being significant contributors. In South Africa and Brazil, GBTC incidence rates are lower, but obesity and diabetes in South Africa, and a higher female incidence rate in Brazil, contribute to increased risk. Chronic infections and gallstones are also prevalent risk factors in Brazil. The socio-demographic index (SDI) of each country plays a significant role in disease management and treatment; higher SDI countries generally offer better healthcare services and early diagnosis, while low-SDI countries face challenges with inadequate medical resources and delayed health interventions[13]. Therefore, studying the BRICS nations is crucial for comprehending the effects of diseases on a significant portion of the global population and for crafting specific strategies to enhance public health and manage diseases within these countries[14].
In order to provide a scientific basis for the development of public health policies and prevention and treatment programs, this study utilized data from the 2021 Global Burden of Disease (GBD) study to systematically analyze the current status and changing trends of GBTC disease burden in the BRICS countries over the past 32 years. Additionally, it predicted the short-term future development trends. Through the estimation and prediction of the burden of disease in the BRICS countries, we can better understand the impact of GBTC in the BRICS countries, and provide information on disease progression, public health prevention and treatment strategies for other developing countries.
The GBD study is a comprehensive research program designed to systematically assess the health status and burden of disease of the global population. The data used in this study were extracted from GBD 2021[15], a data collection that involved multiple sources, including epidemiological surveys, hospital records, vital registration systems, disease surveillance systems, and additional sources such as academic papers and policy reports (https://ghdx.healthdata.org/gbd-2021/sources), and recorded by age and sex. The incidence, prevalence, and mortality of more than 300 diseases and injuries in 204 countries and territories were examined. In this study, by using the Global Health Data Exchange query tool (http://ghdx.healthdata.org/gbd-results-tool), GBTC data were collected from 1990 to 2021, including the number of incidence cases and crude incidence rate, the number of deaths cases and crude mortality rate and the corresponding age-standardized rates. The population was divided into seven age groups every five years: 20-24, 25-29, 30-34, 35-39, 40-44, 45-49, 50-54, 55-59, 60-64, 65-69, 70-74, 75-79, 80-84, 85-89, 90-94 and 95+ years of age.
This study used data from the GBD study, which was approved by the Washington University School of Medicine Institutional Review Board, and had already been de-identified by the original data provider. No personal identifiable information was involved in this research. As this was a secondary analysis of existing data, no additional human participant research ethics review or informed consent was required. Our analysis conformed to guidelines for accurate and transparent health assessment reporting.
Gallbladder and bile duct cancers were identified according to International Classification of Diseases, 10th Revision (ICD-10) C23, C24-C24.9, and the 9th Revision (ICD-9) 156-156.9[16].
In this analysis of the GBD, injuries, and risk factors study (GBD) 2021, we screened the number of GBTC incidences and crude incidence rates, the number of deaths and crude mortality rates, as well as the age-standardized incidence rate (ASIR) and age-standardized mortality rate (ASMR) globally and in the BRICS countries. Percentage changes (PCs) were calculated to describe the long-term trends of the GBTC burden in these regions. Through software analysis, the crude incidence and crude mortality rates of GBTC were visually displayed and descriptively analyzed for different age groups of men and women globally and in the BRICS countries in 2021. Joinpoint regression analysis was employed to examine the trends in disease burden from 1990 to 2021. The age-period-cohort (APC) model was utilized to assess the age, period, and birth cohort effects on the changes in GBTC disease burden worldwide and in the BRICS countries during the same time frame. Decomposition analysis was conducted to quantify the relative contributions of age structure, population size, and epidemiological changes to the overall disease burden of GBTC from 1990 to 2021. Finally, the Bayesian APC (BAPC) model was applied to forecast the disease burden trends of GBTC among men and women globally and in the BRICS countries from 2022 to 2040.
The statistical analysis and visualization presented in this article were performed using the R statistical software (version 4.3.2) and Joinpoint software (version 5.1.0).
The Joinpoint regression model is a set of linear statistical models designed to evaluate the temporal trend of disease burden caused by GBTC[17]. This model estimates the variation pattern of mortality rates using the least squares method, thereby addressing the potential non-objectivity of conventional trend analyses based solely on linear trends. Specifically, it calculates the sum of squared residuals between estimated and actual values to identify turning points in the trend. The Joinpoint software (version 5.1.0; National Cancer Institute, Rockville, Maryland, United States) was utilized to construct this model. Additionally, we calculated the average annual PC (AAPC) and assessed whether the fluctuation trends across different periods were statistically significant by comparing the AAPC to 0. A P value less than 0.05 was considered statistically significant. This model avoids the bias of subjective segmentation and objectively identifies turning points in trends. However, the model is sensitive to short-term data fluctuations, which may lead to overestimation of the clinical significance of minor changes. Furthermore, the requirement to predefine the maximum number of joinpoints may result in missing potential change points.
This study employs the APC model to investigate the effects of age, period, and cohort on the incidence and mortality of GBTC[18]. In this model, net drift captures the overall temporal trend of disease incidence and mortality, similar to the AAPC. However, unlike AAPC, which focuses solely on time-based trends, net drift integrates both period and cohort effects simultaneously. Local drift is utilized to estimate the AAPC in GBTC incidence and mortality within specific age groups. The age effect refers to the variation in incidence and mortality with advancing age, as characterized by the longitudinal age curve, which depicts the natural progression of the disease in terms of age-related incidence and mortality. The period effect reflects the influence of social, economic, and cultural changes across different time periods on disease incidence and mortality. The cohort effect quantifies variations in incidence and mortality due to differing exposures to risk factors among individuals born in distinct time periods. Relative risk (RR) is employed to evaluate the period and cohort effects. To address multi-collinearity among age, period, and cohort, the intrinsic estimator based on Poisson distribution is used to derive disease parameters. To prevent information overlap between adjacent cohorts, equal intervals must be maintained for age, period, and cohort definitions. APC analysis is performed using the online APC tool (https://analysistools.cancer.gov/apc/). The APC model can simultaneously decompose three types of effects, revealing the underlying driving mechanisms of disease burden. Additionally, local drift can identify age-specific trends. However, this method requires constraints to address the 'age = period - cohort' linear non-identifiability issue. Furthermore, the interpretation of results should be contextualized within the epidemiological framework to avoid over-interpretation.
Decomposition analysis is a method used to elucidate how differences in contributing factors result in variations in overall values[19]. This approach is instrumental in uncovering significant heterogeneity in demographic and epidemiological trends. To quantify the relative contributions of age structure, population size, and epidemiological dynamics to the overall burden of GBTC from 1990 to 2021, this paper employs the Das Gupta decomposition method. This method algebraically isolates the standardized effects of each multiplicative factor, thereby summarizing their respective contributions to the observed changes. Changes in age structure primarily reflect population aging, fluctuations in population size are associated with variations in population quantity, and epidemiological changes are linked to crude incidence and mortality rates. This method quantifies the independent contributions of population aging, size growth, and epidemiological changes. Additionally, the Das Gupta method has relaxed assumptions regarding data distribution, making it suitable for non-normal data. However, this method does not allow for the analysis of interactions between factors.
The BAPC model leverages integrated nested Laplace approximations to estimate the marginal posterior distribution, effectively addressing some of the mixing and convergence challenges associated with Markov Chain Monte Carlo sampling in traditional Bayesian approaches. This model has been shown to achieve the highest coverage rate [95% confidence interval (95%CI)], making it particularly well-suited for analyzing age-stratified disease burden predictions. Using age-specific population data from 1990 to 2021, projected population data from 2022 to 2040, and disease and weight data for each age group from the GBD 2021 study, this paper applies the BAPC model to forecast the future 19-year ASIRs and ASMRs for gallbladder and extrahepatic bile duct cancers among men and women globally and in the BRICS countries. The BAPC model was implemented using the R packages INLA (www.r-inla.org) and BAPC (http://r-forge.r-project.org/). The advantage of this model lies in its ability to integrate historical data with population forecasts, providing robust trend estimates. However, its limitations are also evident: The accuracy of predictions depends on the quality of baseline data and does not account for potential future policy interventions or unforeseen factors.
The global number of incident cases increased from 107798 in 1990 [95% uncertainty interval (95%UI): 96890-117512] to 216768 in 2021 (95%UI: 181888-245238), with an increase of approximately 101.09%. The ASIR decreased from 2.89 per 100000 people in 1990 (95%UI: 2.59-3.15) to 2.56 per 100000 people in 2021 (95%UI: 2.16-2.89), with a decrease of approximately 11.46%. The number of deaths increased from 98683 in 1990 (95%UI: 88941-109189) to 171961 in 2021 (95%UI: 142352-194238), with an increase of approximately 74.26%, whereas the ASMR decreased from 2.69 per 100000 people in 1990 (95%UI: 2.39-2.97) to 2.04 per 100000 people in 2021 (95%UI: 1.7-2.29), with a decrease of approximately 24.09%. Among the BRICS countries, the number of incident and death cases in 2021 increased compared to 1990, with the PC in the number of incident and death cases in India being the largest. In addition, in 2021, except for Brazil, the ASIRs in the other four countries increased; the ASMRs in Brazil, Russia, and China decreased, while those in India and South Africa increased (Table 1).
| Countries | 1990 | 2021 | Percentage changes, 1990-2021 | Population | ||||
| n (95%UI) | ASR (95%UI) | n (95%UI) | ASR (95%UI) | n (95%UI) | ASR (95%UI) | 1990, n (million, 95%UI) | 2021, n (million, 95%UI) | |
| Incidence | ||||||||
| Global | 107798 (96890, 117512) | 2.89 (2.59, 3.15) | 216768 (181888, 245238) | 2.56 (2.16, 2.89) | 101.09 (77.14, 120.21) | -11.46 (-21.91, -3.35) | 5334 (5231, 5445) | 7891 (7667, 8131) |
| Brazil | 2692 (2549, 2789) | 3.17 (2.97, 3.3) | 5728 (5286, 6005) | 2.29 (2.11, 2.4) | 112.8 (103.07, 122.23) | -27.87 (-30.98, -24.91) | 149 (138, 159) | 220 (188, 251) |
| Russia | 3369 (3240, 3467) | 1.87 (1.8, 1.93) | 5119 (4701, 5524) | 2.13 (1.96, 2.3) | 51.97 (40.64, 63.13) | 13.62 (5.34, 22.01) | 151 (139, 163) | 145 (125, 164) |
| India | 6890 (5510, 9956) | 1.52 (1.24, 2.22) | 26105 (17885, 30789) | 2.24 (1.54, 2.64) | 278.87 (170.19, 356.12) | 47.5 (4.73, 77.25) | 853 (789, 915) | 1414 (1240, 1602) |
| China | 17077 (13003, 21744) | 2.19 (1.68, 2.79) | 51720 (35618, 66848) | 2.49 (1.71, 3.21) | 202.86 (124.42, 294.71) | 13.62 (-14.39, 45.88) | 1176 (1097, 1264) | 1423 (1319, 1530) |
| South Africa | 129 (91, 177) | 0.64 (0.44, 0.88) | 358 (236, 422) | 0.8 (0.53, 0.95) | 178.08 (113.25, 226.95) | 26.04 (-4.94, 49.21) | 37 (33, 41) | 57 (50, 64) |
| Deaths | ||||||||
| Global | 98683 (88941, 109189) | 2.69 (2.39, 2.97) | 171961 (142352, 194238) | 2.04 (1.7, 2.29) | 74.26 (54.2, 91.45) | -24.09 (-33.19, -16.88) | 5334 (5231, 5445) | 7891 (7667, 8131) |
| Brazil | 2801 (2648, 2905) | 3.41 (3.18, 3.56) | 5758 (5283, 6056) | 2.32 (2.12, 2.44) | 105.53 (95.66, 114.75) | -32.04 (-35.06, -29.23) | 149 (138, 159) | 220 (188, 251) |
| Russia | 2978 (2864, 3065) | 1.67 (1.61, 1.72) | 3440 (3157, 3721) | 1.42 (1.31, 1.54) | 15.51 (6.38, 24.61) | -15.14 (-21.77, -8.61) | 151 (139, 163) | 145 (125, 164) |
| India | 7090 (5709, 10396) | 1.63 (1.33, 2.41) | 26744 (18241, 31538) | 2.35 (1.61, 2.77) | 277.18 (167.1, 353.9) | 44.57 (1.75, 73.66) | 853 (789, 915) | 1414 (1240, 1602) |
| China | 17251 (13213, 22143) | 2.32 (1.78, 2.97) | 37833 (26653, 49262) | 1.85 (1.29, 2.4) | 119.31 (64.03, 185.61) | -20.24 (-39.19, 2.21) | 1176 (1097, 1264) | 1423 (1319, 1530) |
| South Africa | 134 (94, 186) | 0.68 (0.47, 0.95) | 366 (242, 431) | 0.85 (0.56, 1) | 172.76 (108.14, 221.86) | 23.97 (-6.45, 47.46) | 37 (33, 41) | 57 (50, 64) |
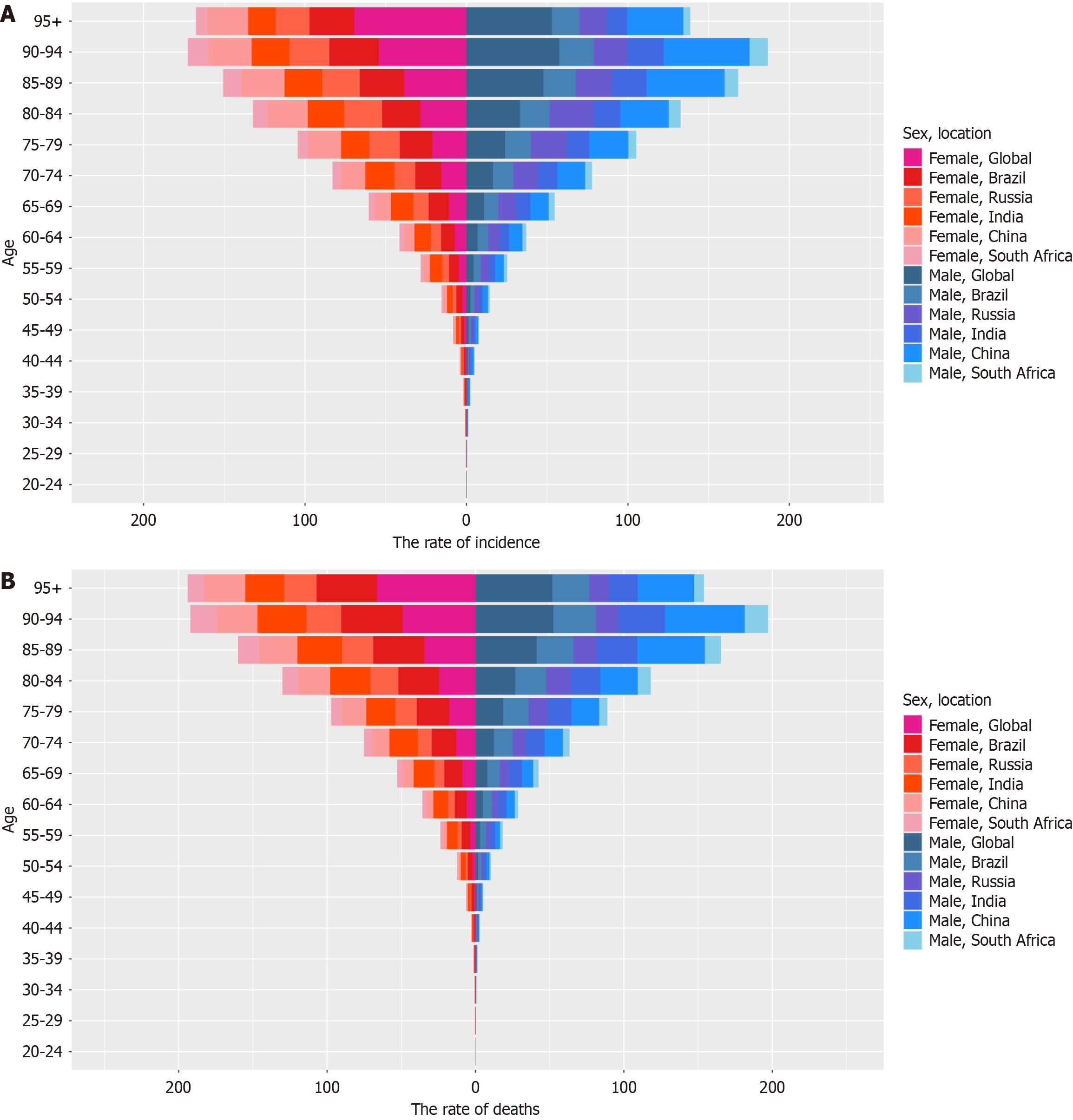
In 2021, the crude incidence and mortality rates of gallbladder and bile duct cancer in both men and women showed a gradually increasing trend with age. In global data, women aged ≥ 95 years had the highest crude incidence and mortality rates, while men had the highest crude incidence and mortality rates at the age of 90-94 years. In Brazil, India, and South Africa, the crude incidence and crude mortality rates were 1.4 times higher in women compared to men. In Russia, the crude incidence rate was identical for both sexes, while the crude mortality rate was 1.3 times higher in women than in men. In contrast, in China, the crude incidence and crude mortality rates for women were 70% of those observed in men (Figure 1).
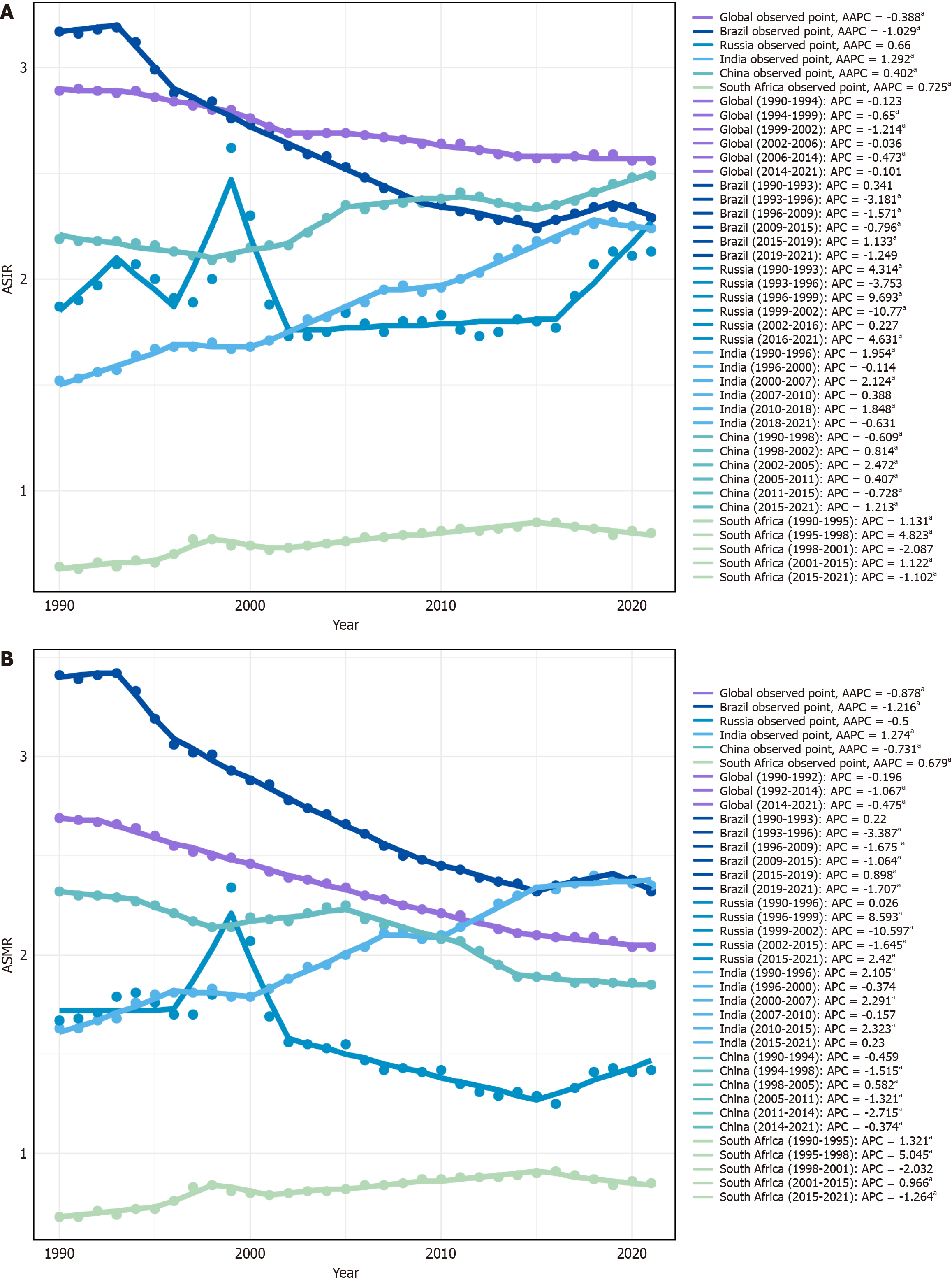
Joinpoint regression analysis revealed that from 1990 to 2021, the overall ASIR of gallbladder and bile duct cancer exhibited a declining trend (95%CI = -0.495% to 0.282%; P < 0.001). In Brazil, the overall ASIR for gallbladder and bile duct cancer also showed a downward trend (AAPC = -1.029%, 95%CI = -1.244% to -0.813%; P < 0.001). Conversely, the overall ASIR in India, China, and South Africa demonstrated an increasing trend (India: AAPC = 1.292%, 95%CI = 0.951%-1.634%; P < 0.001; China: AAPC = 0.402%, 95%CI = 0.216%-0.588%; P < 0.001; South Africa: AAPC = 0.725%, 95%CI = 0.175%-1.279%; P = 0.01; Figure 2A). Notably, except for China, where the overall ASMR of gallbladder and bile duct cancer decreased (AAPC = -0.731%, 95%CI = -0.942% to -0.520%; P < 0.001), the global trends and those of other BRICS countries in terms of ASMR were consistent with the ASIR patterns (Figure 2B).
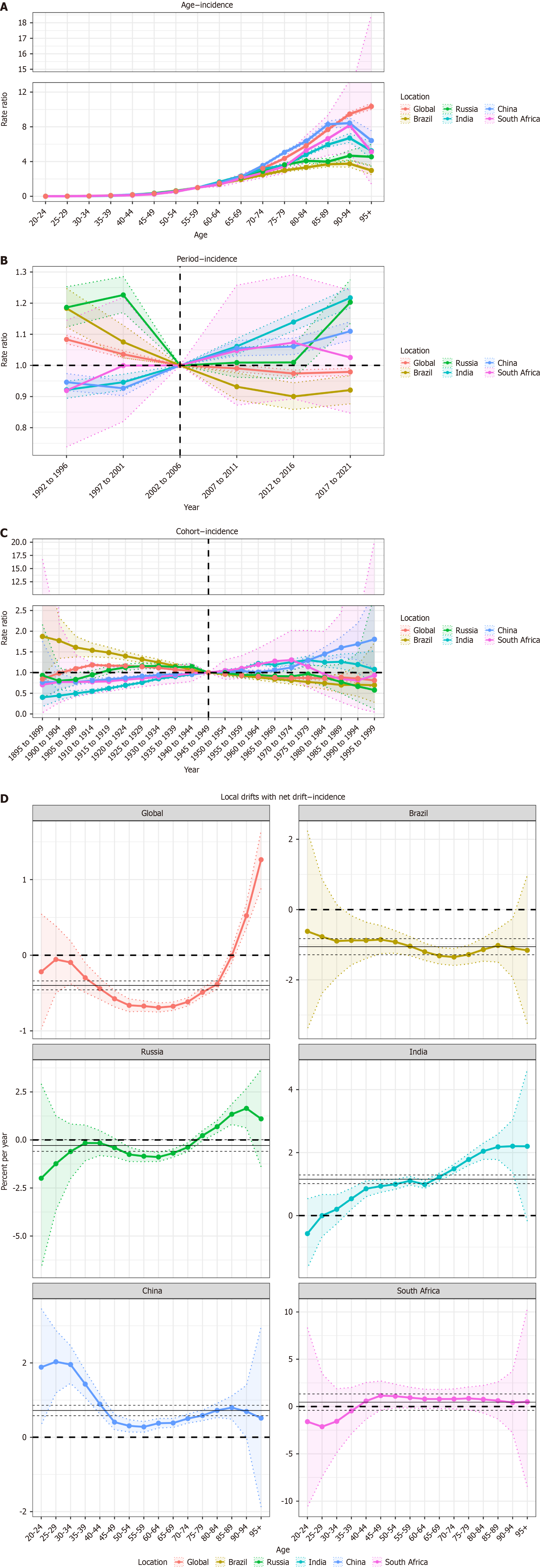
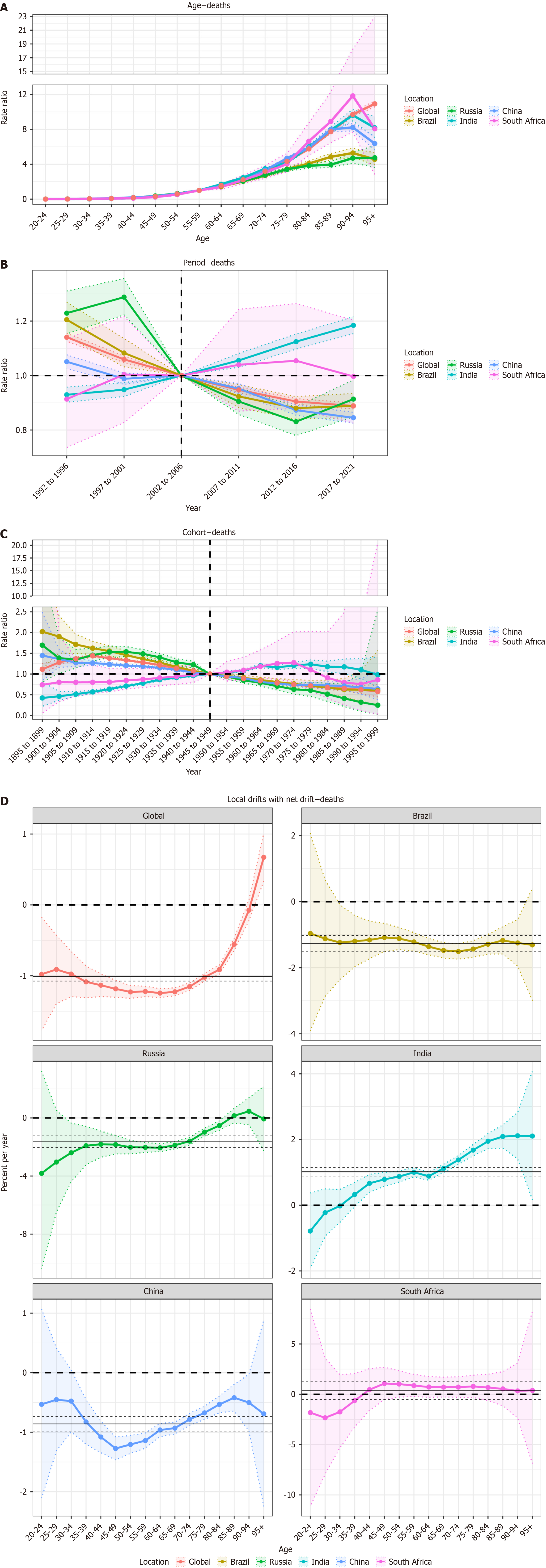
While maintaining the period and cohort effects constant, the age effect on the incidence and mortality rates of gallbladder and bile duct cancer in the BRICS countries exhibited a trend of gradually increasing and then decreasing. This suggests that as age increases, the incidence and mortality rates first rise and subsequently decline. Specifically, in Brazil, India, China, and South Africa, the incidence and mortality rates of GBTC exhibit an overall increasing trend with age, peaking in the 90-94 age group, followed by a subsequent decline. In contrast, in Russia, both the incidence and mortality rates showed a continuous increase from ages 20 to 79 years, while fluctuating patterns were observed beyond the age of 80 years. In contrast, the effect of age on the incidence and mortality rates of gallbladder and bile duct cancer globally demonstrated a consistently increasing trend, indicating that with advancing age, the incidence and mortality rates progressively increased (Figures 3A and 4A).
While maintaining the age and cohort effects constant, the reference period for this study was set from 2002 to 2006. Globally and in Brazil, the incidence and mortality rates of gallbladder and bile duct cancers have gradually decreased over time. In contrast, the incidence of gallbladder and bile duct cancers in India, China, and South Africa progressively increased over time. Additionally, the mortality rates of gallbladder and bile duct cancer in India and South Africa gradually increased over time, whereas the mortality rate in China gradually decreased during the same period. Compared with the reference period (2002-2006), an RR > 1 indicates that the RR of incidence or mortality in a given period is higher than that of the reference period, whereas an RR < 1 suggests that the RR is lower than that of the reference period (Figures 3B and 4B).
While maintaining the age and period effects constant, the reference cohort in this study was defined as individuals born between 1945 and 1949. Globally, the incidence and mortality risks of gallbladder and bile duct cancer among consecutive birth cohorts initially increased and then gradually declined. In Brazil, both incidence and mortality risks consistently decreased over time. In Russia and India, the incidence and mortality risks initially increased, followed by a gradual decrease. In China, the incidence risk exhibited a steady upward trend, whereas the mortality risk demonstrated a gradual decline. In South Africa, both incidence and mortality risks followed a pattern of initial increase and subsequent gradual decline (Figures 3C and 4C).
Overall, the local drift of incidence for gallbladder and bile duct cancer in China was greater than 0, showing a trend of initially decreasing followed by increasing, indicating that the disease burden is worsening. Furthermore, the increasing trend becomes more pronounced after an initial decrease. In contrast, the local drift of mortality was less than 0, showing a trend of initially decreasing followed by increasing, indicating that the disease burden is alleviating, with the rate of alleviation gradually slowing down and the trend of increase becoming larger. In Brazil, the local drift of both incidence and mortality for gallbladder and bile duct cancer was less than 0, gradually decreasing, suggesting that the disease burden is decreasing, with the rate of decrease gradually slowing down (Figures 3D and 4D).
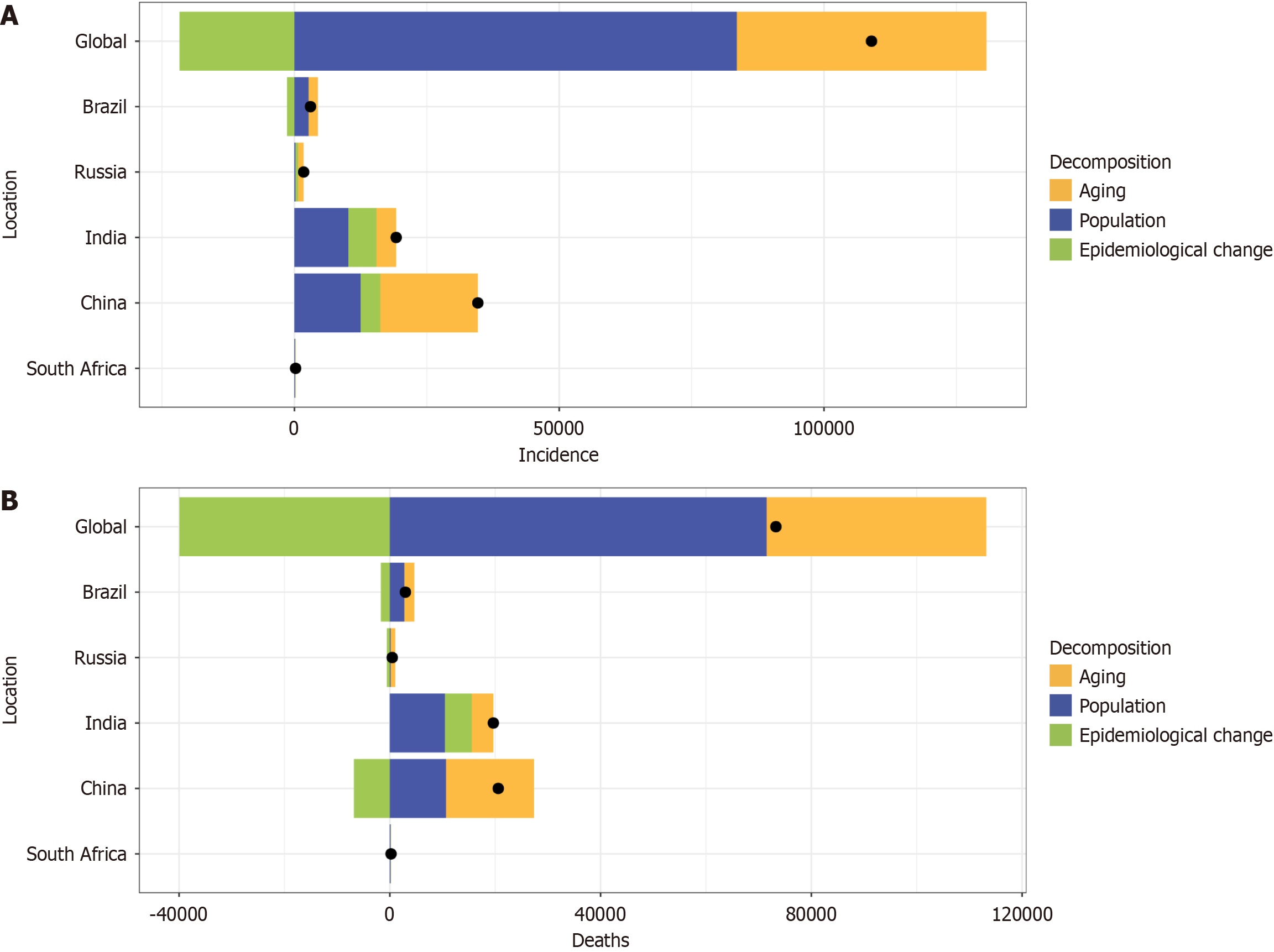
Decomposition analysis was used to quantify the relative contributions of changes in age structure, population size, and epidemiology to the overall burden of gallbladder and bile duct cancer.
Between 1990 and 2021, the global increase in the number of gallbladder and bile duct cancer cases, as well as the increase in Brazil, was primarily attributed to epidemiological transitions and population aging. Conversely, population growth contributed significantly to the stabilization or reduction of patient numbers in some regions. In Russia, India, China, and South Africa, the increase in gallbladder and bile duct cancer cases was mainly driven by population growth, aging, and epidemiological changes. Similarly, the increase in mortality due to gallbladder and bile duct cancer globally, as well as in Brazil, Russia, and China, was predominantly due to epidemiological transitions and population aging. In contrast, population growth has played a critical role in mitigating the increase in mortality in certain areas. In India and South Africa, the increase in deaths due to gallbladder and bile duct cancer was largely attributable to population growth, aging populations, and epidemiological changes (Figure 5).
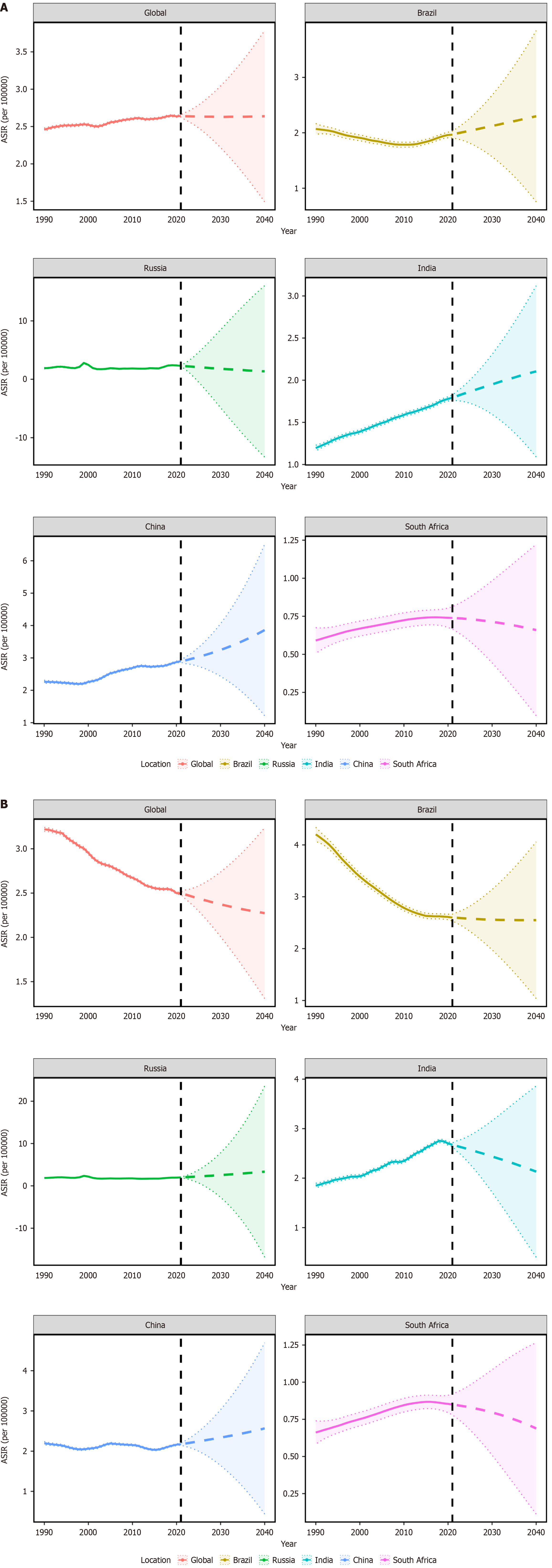
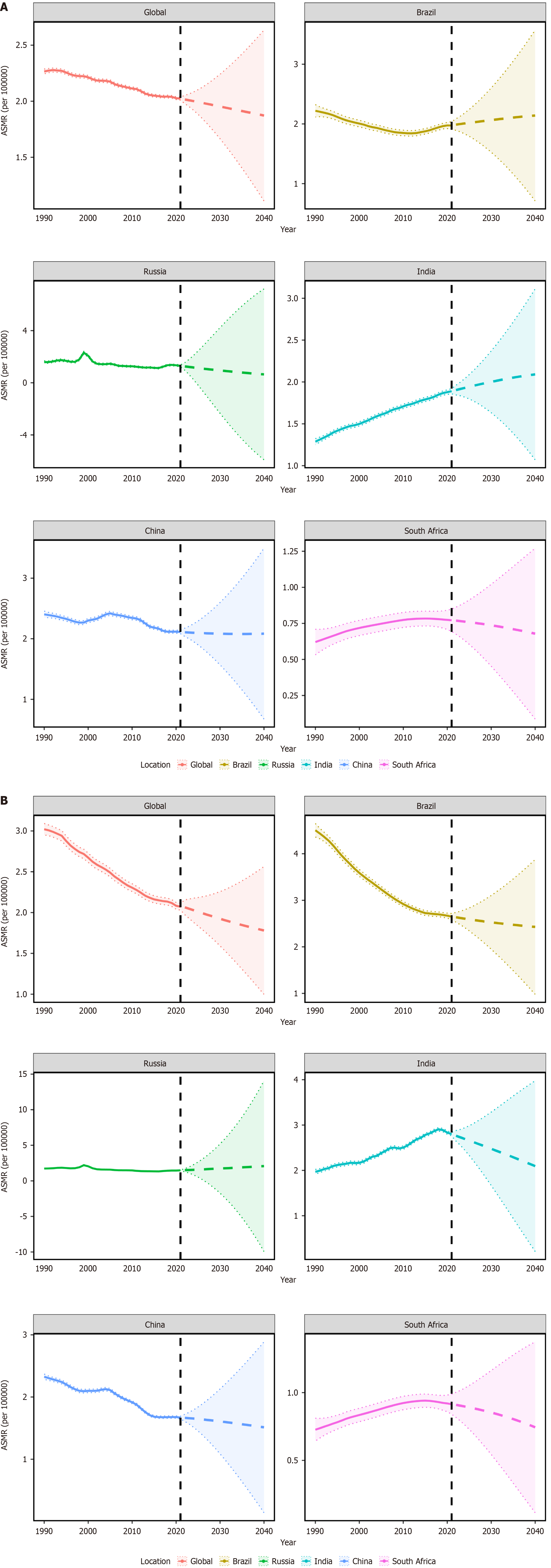
This study conducted a BAPC analysis and predicted the burden trends of ASIRs and ASMRs for GBTC among both males and females globally, as well as in the BRICS countries, from 2022 to 2040.
The ASIR of GBTC in females is projected to exhibit a decreasing trend annually over the next 19 years, whereas the ASIR trend in males is expected to remain relatively stable. In Brazil, the ASIR of GBTC in males is anticipated to increase annually over the same period, whereas the trend in females is likely to remain relatively stable. Notably, in India, the ASIR of GBTC in males is predicted to rise annually over the next 19 years, in contrast to the declining trend observed in females. Both males and females in China are expected to experience an annual increase in the ASIR of gallbladder and bile duct cancer over the next 19 years. Conversely, in South Africa, the ASIR for both sexes is projected to decrease annually during this timeframe (Figure 6).
The ASMR of gallbladder and bile duct cancer is projected to decline globally in both men and women over the next 19 years. In contrast, the ASMR for men in Brazil and India is expected to increase annually during this period, whereas the trend for women in these countries shows an opposite pattern. Additionally, the ASMR of gallbladder and bile duct cancer in both men and women in South Africa is anticipated to decrease annually over the next 19 years (Figure 7).
To the best of our knowledge, this is the first study to examine GBTC incidence and mortality using the APC model, facilitating comparisons between global data and BRICS nations. Our study's primary contribution, in contrast to earlier GBD 2021 publications, offers a more thorough insight into disease trends by employing age, period, and cohort effects to differentiate various sources of mortality risk both globally and within BRICS countries. Another notable advancement is the assessment of localized drift in the global and BRICS age distributions of mortality and age at onset from 1990 to 2021, which enables us to identify temporal trends in incidence for each age group and account for period effects.
From 1990 to 2021, the number of cases associated with GBTC increased by 101.09% (95%UI = 77.14-120.21), while the number of related deaths rose by 74.26% (95%UI = 54.20-91.45), likely driven by rapid population growth. After eliminating inconsistencies in age composition, global age-standardized GBTC mortality declined over this 32-year period. This is largely attributed to the introduction of Gemcitabine-based chemotherapy in the 2010s. However, with the prevalence of a number of potential risk factors for GBTC, such as gallstones, obesity, diabetes, consuming sweetened and sucrose beverages, and numerous pathogens (e.g., mycotoxins, hepatitis B and hepatitis C viruses, etc.)[20-22]. These factors should be considered as crucial matters when aiming to reduce the burden of GTBC, and thus require further attention.
Over the past 32 years, there has been a marked increase (exceeding 70%) in both the number of cases and deaths attributed to GBTC[23]. This rise correlates with shifts in population structure, such as aging and population growth, as well as changes in the global geographical distribution of GBTC risk factors. Disparities in disease burden persist across different regions and genders. For instance, both the ASIR and ASMR in Brazil are trending downward, whereas in India and South Africa, they are increasing. In China and Russia, the ASIR is on the rise, but the ASMR is declining. Consequently, despite the overall downward trend in age-standardized rates, this should not lead to complacency regarding further prevention or reduction efforts for GBTC. The rising incidence rates observed in South Africa and India may be linked to their relatively low SDI, underscoring the need for targeted interventions. In regions with varying SDI, the ASIR, ASMR, and age-standardized disability-adjusted life years rate of GBC have exhibited distinct trends. In high SDI and upper-middle SDI regions, these metrics have shown a consistent downward trend. Conversely, in lower-middle SDI and low SDI regions, an upward trend has been observed[24]. These findings underscore the complex influence of socio-demographic changes on the disease burden across different countries. While individuals residing in economically developed areas tend to benefit from better education, prioritize health more effectively, and enjoy greater access to healthcare services, the onset and progression of tumors result from the intricate interplay of multiple potential carcinogenic factors[25]. Consequently, despite significant advancements in disease prevention, there remains substantial room for improvement in medical preventive strategies.
A variety of malignant tumors show obvious gender tendencies due to different gender-specific carcinogenic mechanisms[26]. Among the BRICS countries, in most age groups across Brazil, Russia, India, and South Africa, the crude incidence and mortality rates for females are higher than those for males. In contrast, the situation in China is reversed. The burden of GBTC is notably higher among Chinese males compared to females. Chinese males may be more likely than females to consume a diet high in fats and low in fiber, which could contribute to a higher incidence of GBTC. Similarly, exposure risks in certain occupations, such as those in the petrochemical industry, may further increase the risk of developing the disease. The gender disparity in GBTC incidence is influenced by a combination of socio-economic, environmental, dietary, and public health policy factors. Additionally, our findings indicate an increasing burden of GBTC among older adults[27]. In the BRICS countries, the disease burden of GBTC escalates with advancing age. Moreover, obesity serves as a critical influencing factor. Particularly in developed countries and regions, individuals are more susceptible to obesity due to high-calorie diets, sedentary lifestyles, and physical stress. Globally, the prevalence of obesity is higher among females than males, which may be attributed to gender-specific factors such as hormonal differences, gut microbiota composition, and genetic predispositions. This increased prevalence of obesity in women contributes to a higher incidence of GBC, thereby intensifying the disease burden. The primary risk factor for GBC is the presence of gallbladder disease, and it is strongly associated with advanced age, as well as other factors including obesity, physical activity, and hormonal influences. Given the characteristics of GBC, it is imperative that primary prevention, medical treatment, and diagnostic care be tailored to address gender and aging considerations.
Biological events, demographic shifts, and socio-economic factors have led to variations in cohort effects across different generations. Early generations, in addition to experiencing population aging, faced medical resource shortages and socio-economic instability, which impeded timely interventions for GBC risk factors, such as gallstones and non-alcoholic fatty liver disease. The diminishing cohort effect for those born post-1917 reflects the success of cancer prevention initiatives and improvements in healthcare infrastructure. With the increasing adoption of cholecystectomy and global advancements in preventive medicine, both the global incidence and mortality rates for GBC have declined. However, in low-SDI BRICS nations, such as India and South Africa, incidence and mortality rates continue to rise.
Rapid population growth in developing countries has been a major driver of the rising global burden of GBC[28]. Specifically, in low-SDI regions, the positive effects of epidemiological changes have been somewhat counteracted by population growth, which has slowed the aging process, yielding contrasting effects. These findings underscore the challenges presented by shifting demographic and epidemiological dynamics. Demographic trends suggest that most countries are experiencing accelerated population aging, with the impact of aging on disease burden becoming more pronounced as socio-economic development progresses. The results also highlight the increasing significance of aging on cerebrovascular disease burden in regions with lower SDI, stressing the need for greater attention to the aging population in underdeveloped areas.
Given the poor prognosis of GBC patients, it is essential to develop and implement preventive strategies. Current research emphasizes the critical role of controlling gallstones as a significant means of alleviating the global burden of GBC, given its direct association with the disease's incidence and mortality[29]. There is a pressing need for health policy and management measures to address modifiable risk factors for gallstones and GBC, including smoking, poor diet, obesity, physical inactivity, and diabetes. However, substantial disparities in the burden of GBC across different countries and regions, particularly in China, Russia, and India, suggest that urban-rural differences and regional economic imbalances may influence disease screening and early diagnosis rates. Research on preventable risk factors in these countries could contribute to the development of targeted health strategies and clinical guidelines.
The present study had several limitations. First, all BRICS members are developing countries, which may face challenges in providing comprehensive and accurate disease and health data due to constraints in resources and infrastructure. Second, significant regional and urban-rural disparities exist within developing countries such as China, India, and Russia; however, the data available in the GBD database may not fully capture these differences. Additionally, the economic growth and health data of developing countries such as Russia are highly susceptible to external economic and political influences, potentially introducing bias in BAPC predictions. Third, the parameter estimates generated by the APC model lack intuitive interpretation, complicating the explanation of their practical significance. This analysis is also prone to ecological fallacies, which may affect the accuracy of causal inferences. Finally, period and cohort effects were examined using cross-sectional data from the most recent GBD 2021 estimates, covering the period from 1990 to 2021. Future cohort studies conducted in various countries are necessary to assess RRs at specific locations and times and to evaluate differential risks among susceptible populations.
Our research sheds light on the variations in gender and age concerning the impact of GBTC across the BRICS nations and globally over the last 32 years. In BRICS countries, the number of incident cases and deaths due to GBTC increased between 1990 and 2021, primarily due to rapid population growth. Nevertheless, the age-standardized incidence and mortality rates declined during the same period. Notably, the prevention and control strategies adopted by BRICS nations provide valuable insights that could benefit other developing countries.
patient ethics approval nor animal ethics review.
| 1. | Danpanichkul P, Suparan K, Tothanarungroj P, Dejvajara D, Rakwong K, Pang Y, Barba R, Thongpiya J, Fallon MB, Harnois D, Lui RN, Wallace MB, Yang JD, Roberts LR, Wijarnpreecha K. Epidemiology of gastrointestinal cancers: a systematic analysis from the Global Burden of Disease Study 2021. Gut. 2024;74:26-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 2. | Shahin RK, Elkady MA, Abulsoud AI, Abdelmaksoud NM, Abdel Mageed SS, El-Dakroury WA, Zewail MB, Elazazy M, Sobhy MH, Nomier Y, Elazazy O, Elballal MS, Mohammed OA, Midan HM, Elrebehy MA, Ziada BO, Doghish AS. miRNAs orchestration of gallbladder cancer - Particular emphasis on diagnosis, progression and drug resistance. Pathol Res Pract. 2023;248:154684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 3. | Rodas F, Vidal-Vidal JA, Herrera D, Brown-Brown DA, Vera D, Veliz J, Püschel P, Erices JI, Sánchez Hinojosa V, Tapia JC, Silva-Pavez E, Quezada-Monrás C, Mendoza-Soto P, Salazar-Onfray F, Carrasco C, Niechi I. Targeting the Endothelin-1 pathway to reduce invasion and chemoresistance in gallbladder cancer cells. Cancer Cell Int. 2023;23:318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 4. | Ye C, Dong C, Lin Y, Shi H, Zhou W. Interplay between the Human Microbiome and Biliary Tract Cancer: Implications for Pathogenesis and Therapy. Microorganisms. 2023;11:2598. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Dutta A, Mungle T, Chowdhury N, Banerjee P, Gehani A, Sen S, Mallath M, Roy P, Krishnan S, Ganguly S, Banerjee S, Roy M, Saha V. Characteristics and outcomes of gallbladder cancer patients at the Tata Medical Center, Kolkata 2017-2019. Cancer Med. 2023;12:9293-9302. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Zhang X, Xu C, Zhang H, Du X, Zhang Q, Lu M, Ma Y, Ma W. Gallbladder cancer incidence and mortality rate trends in China: analysis of data from the population-based cancer registry. BMC Public Health. 2024;24:3122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Zhao Z, Wu H, Han J, Jiang K. Global trends and disparities in gallbladder and biliary tract cancers: insights from the global burden of disease study 2021. Eur J Gastroenterol Hepatol. 2025;37:573-584. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Sahoo PM, Rout HS, Jakovljevic M. Future health expenditure in the BRICS countries: a forecasting analysis for 2035. Global Health. 2023;19:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 9. | Dutta P, Danpanichkul P, Suparan K, Pang Y, Rakwong K, Fine MR, Wijarnpreecha K. Sex disparities in global burden of gallbladder and biliary tract cancer: analysis of Global Burden of Disease study from 2010 to 2019. J Gastroenterol Hepatol. 2024;39:2863-2871. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Nelson SM, Gao YT, Nogueira LM, Shen MC, Wang B, Rashid A, Hsing AW, Koshiol J. Diet and biliary tract cancer risk in Shanghai, China. PLoS One. 2017;12:e0173935. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Khan SA, Tavolari S, Brandi G. Cholangiocarcinoma: Epidemiology and risk factors. Liver Int. 2019;39 Suppl 1:19-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 494] [Article Influence: 82.3] [Reference Citation Analysis (0)] |
| 12. | Larsson SC, Giovannucci EL, Wolk A. Sweetened Beverage Consumption and Risk of Biliary Tract and Gallbladder Cancer in a Prospective Study. J Natl Cancer Inst. 2016;108:djw125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Ouyang G, Liu Q, Wu Y, Liu Z, Lu W, Li S, Pan G, Chen X. The global, regional, and national burden of gallbladder and biliary tract cancer and its attributable risk factors in 195 countries and territories, 1990 to 2017: A systematic analysis for the Global Burden of Disease Study 2017. Cancer. 2021;127:2238-2250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 92] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 14. | Liu Z, Wang Z, Xu M, Ma J, Sun Y, Huang Y. The priority areas and possible pathways for health cooperation in BRICS countries. Glob Health Res Policy. 2023;8:36. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2133-2161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1073] [Cited by in RCA: 1410] [Article Influence: 1410.0] [Reference Citation Analysis (0)] |
| 16. | World Health Organization. International Statistical Classification of Diseases and Related Health Problems (ICD). [cited 30 May 2025]. Available from: https://www.who.int/standards/classifications/classification-of-diseases. |
| 17. | Li HZ, Du LB. [Application of Joinpoint regression model in cancer epidemiological time trend analysis]. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54:908-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 18. | Rosenberg PS, Check DP, Anderson WF. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2014;23:2296-2302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 460] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 19. | Das Gupta P. Standardization and decomposition of rates from cross-classified data. Genus. 1994;50:171-196. [PubMed] |
| 20. | Liu Z, Shi O, Zhang T, Jin L, Chen X. Disease burden of viral hepatitis A, B, C and E: A systematic analysis. J Viral Hepat. 2020;27:1284-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Zhan Z, Chen X, Xu S, Li Q, Yu J, Guo Z, Chen B. Impact of high body mass index on gallbladder and biliary tract cancer burden in China: a comprehensive analysis of trends from 1990 to 2021. World J Surg Oncol. 2024;22:296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 22. | Vega EA, Mellado S, Salehi O, Freeman R, Conrad C. Treatment of Resectable Gallbladder Cancer. Cancers (Basel). 2022;14:1413. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 23. | Liu C, Du S, Liu X, Niu W, Song K, Yu J. Global, regional, and national burden of gallbladder and biliary tract cancer, 1990 to 2021 and predictions to 2045: an analysis of the Global Burden of Disease study 2021. J Gastrointest Surg. 2025;29:101968. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Lei S, Huang G, Li X, Xi P, Yao Z, Lin X. Global Burden, Trends, and Inequalities of Gallbladder and Biliary Tract Cancer, 1990-2021: A Decomposition and Age-Period-Cohort Analysis. Liver Int. 2025;45:e16199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 25. | Vuthaluru S, Sharma P, Chowdhury S, Are C. Global epidemiological trends and variations in the burden of gallbladder cancer. J Surg Oncol. 2023;128:980-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (1)] |
| 26. | Bernardez B, Higuera O, Martinez-Callejo V, Cardeña-Gutiérrez A, Marcos Rodríguez JA, Santaballa Bertrán A, Majem M, Moreno-Martínez ME. Sex and gender differences in cancer pathogenesis and pharmacology. Clin Transl Oncol. 2025;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Reimann P, Mavroeidi IA, Burghofer J, Taghizadeh H, Webersinke G, Kasper S, Schreil G, Morariu D, Reichinger A, Baba HA, Kirchweger P, Schuler M, Djanani A, Prager GW, Rumpold H, Benda M, Schneider EM, Mink S, Winder T, Doleschal B. Exploring the impact of durvalumab on biliary tract cancer: insights from real-world clinical data. Cancer Immunol Immunother. 2024;73:251. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Zhou Y, Chen ZQ. Research on the prognostic value of adjusting intraperitoneal three-dimensional quality evaluation mode in laparoscopic cholecystectomy patients. World J Gastrointest Surg. 2024;16:1078-1086. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 29. | Baruah C, Jorvekar SB, Sarma A, Gogoi G, Roy N, Dutta U, Khanna S, Borkar RM, Kumar A, Barah P. Gallstone Physicochemical Properties and Heavy Metal Concentrations Associated with Gallbladder Carcinogenesis in Assam, India. Chem Res Toxicol. 2025;38:598-608. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |