Published online May 15, 2020. doi: 10.4251/wjgo.v12.i5.535
Peer-review started: December 13, 2019
First decision: January 14, 2020
Revised: January 30, 2020
Accepted: April 4, 2020
Article in press: April 4, 2020
Published online: May 15, 2020
Processing time: 152 Days and 17.8 Hours
Toll-like receptor-2 (TLR2) is responsible for recognizing Helicobacter pylori (H. pylori) and activating the immune response. Polymorphisms in TLR2 may modulate gastric carcinogenesis.
To evaluate whether the TLR2 19216T/C (rs3804099) and TLR2 -196 to -174 ins/del (rs111200466) polymorphisms contribute to gastric carcinogenesis in the Brazilian population, and to determine the influence of both polymorphisms and H. pylori infection on TLR2 mRNA expression.
DNA was extracted from 854 peripheral blood leukocyte or gastric tissue samples [202 gastric cancer (GC), 269 chronic gastritis (CG), and 383 control/healthy (C)] and genotyped by allele-specific PCR or restriction fragment length polymorphism (RFLP)-PCR. Quantitative polymerase chain reaction by TaqMan® assay was used to quantify TLR2 mRNA levels in fresh gastric tissues (48 GC, 36 CG, and 14 C).
Regarding the TLR2 -196 to -174 polymorphism, the ins/del and del/del genotypes were associated with a higher risk of GC by comparison with the C in all of the analyzed inheritance models (codominant, dominant, recessive, overdominant and log-additive; P < 0.0001). Similarly, an increased risk was observed when comparing the GC and CG groups [codominant (P < 0.0001), dominant (P < 0.0001), recessive (P = 0.0260), overdominant (P < 0.0001) and log-additive (P < 0.0001)]. In contrast, TLR2 19216T/C was associated with a protective effect in the GC group compared to the C group [dominant (P = 0.0420) and log-additive (P = 0.0300)]. Regarding the association of polymorphisms with H. pylori infection, individuals infected with H. pylori and harboring the TLR2 -196 to -174 ins/del polymorphism had an increased risk of gastric carcinogenesis [codominant (P = 0.0120), dominant (P = 0.0051), overdominant (P = 0.0240) and log-additive (P = 0.0030)], while TLR2 19216T/C was associated with a protective effect [codominant (P = 0.0039), dominant (P < 0.0001), overdominant (P = 0.0097) and log-additive (P = 0.0021)]. TLR2 mRNA levels were significantly increased in the GC group (median RQ = 6.95) compared to the CG group (RQ = 0.84, P < 0.0001) and to the normal mucosa group (RQ = 1.0). In addition, both H. pylori infection (P < 0.0001) and the presence of the polymorphic TLR2 -196 to -174del (P = 0.0010) and TLR2 19216 C (P = 0.0004) alleles influenced TLR2 mRNA expression.
The TLR2 -196 to -174 ins/del and TLR2 19216 T/C polymorphisms are strongly associated with GC. TLR2 mRNA expression levels are upregulated in neoplastic tissues and influenced by both the presence of H. pylori and variant genotypes.
Core tip: This study showed that two polymorphisms in toll-like receptor-2 (TLR2) are strongly associated with gastric cancer and Helicobacter pylori (H. pylori) infection in the Brazilian population. TLR2 mRNA expression was increased in gastric cancer tissue compared with chronic gastritis and normal tissues. Moreover, TLR2 mRNA expression levels were upregulated in gastric cancer in the presence of the TLR2 -196 to -174 del variant allele or the wild-type TLR2 19216 T allele and in the presence of H. pylori. Thus, gene polymorphisms that change expression levels, such as those in TLR2, may alter the immune response and, consequently, the development and clinical manifestations of cancer.
- Citation: Lourenço CM, Susi MD, Nascimento MCAD, Serafim Junior V, Vila APS, Rodrigues-Flemming GH, Goloni-Bertollo EM, Silva AE, Oliveira-Cucolo JG. Characterization and strong risk association of TLR2 del -196 to -174 polymorphism and Helicobacter pylori and their influence on mRNA expression in gastric cancer. World J Gastrointest Oncol 2020; 12(5): 535-548
- URL: https://www.wjgnet.com/1948-5204/full/v12/i5/535.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v12.i5.535
The cascade of gastric carcinogenesis described by Correa et al[1] describes the role of Helicobacter pylori (H. pylori) infection in the development of chronic gastritis (CG), considered the initial stage of tumor progression, and that ends with the development of gastric cancer (GC). Thus, H. pylori infection represents the main cause of CG, and infected patients have a 10-fold higher chance of developing GC[2]. Thus, this bacterium is widely known as a class I carcinogen in gastric diseases[3].
Pattern recognition receptors (PRRs), including toll-like receptors (TLRs) 2 and 4, recognize different pathogen-associated molecular patterns (PAMPs) shared by most microorganisms, including H. pylori[4]. TLR2 is involved in the recognition of bacterial lipopolysaccharide (LPS); TLR2 activation results in the activation of nuclear factor-κB (NF-κB) and functions as an innate immune response, but a Th1 adaptive immune response is also triggered by binding to H. pylori neutrophil-activating protein[5].
The presence of H. pylori disrupts gastric mucosa homeostasis and initiates an inflammatory response, stimulating the production and secretion of proinflammatory mediators, such as interleukin (IL)-1β, IL-2, IL-6, IL-8, IL-12, and reactive oxygen and nitrogen species that cause DNA damage[6]. This proinflammatory microenvironment may promote the development of precancerous lesions, such as chronic gastritis, gastric atrophy, intestinal metaplasia, and dysplasia, that eventually progress to gastric cancer[7].
TLR2 polymorphisms are associated with the pathogenesis of GC, vary among different populations and ethnic groups, and can modulate the immune response to H. pylori infection and its persistence. For example, TLR2 -196 to -174 ins/del, a 22-bp deletion in the promoter region, is associated with protection against GC in the Chinese population[8,9] but has no association with gastric diseases in the Japanese population[10,11]. However, studies in the Caucasian population demonstrated an increased risk for gastric cancer[12] and other types of cancer, such as breast[13], colorectal[14], and head and neck cancer[15].
For TLR2 19216T/C (rs3804099), a synonymous variant located on chromosome 4, it is not yet clear which allele (C or T) is associated with the susceptibility to disease. Some studies in the Asian population have indicated a protective association between the TC or CC genotype and different types of cancer, such as colorectal[16], breast[17], and hepatocellular carcinoma[18]. Conversely, in the Russian population, the CC genotype was closely associated with a risk of severe coronary atherosclerosis[19].
Thus, given the contradictory results and genetic heterogeneity of the Brazilian population, it is important to evaluate the role of these polymorphisms in the susceptibility to gastric carcinogenesis. In addition, we evaluated the influence of TLR2 polymorphisms and H. pylori infection on TLR2 mRNA expression. Our findings showed that the TLR2 -196 to -174 ins/del and TLR2 19216T/C polymorphisms are associated with an increased risk of and protection against gastric cancer development, respectively. TLR2 mRNA expression levels were upregulated in gastric cancer tissues and were influenced by both the presence of H. pylori and variant genotypes.
The Research Ethics Committee of Universidade do Sagrado Coração (USC) in Bauru, São Paulo, Brazil approved this study (Registration Number 382.514), and written informed consent for the collection of biological material (peripheral blood and gastric tissues) was obtained from all individuals.
This was a case-control study on CG and GC patients and healthy individuals. DNA was obtained from a total of 852 peripheral blood leukocyte or gastric tissue samples and genotyped for TLR2 polymorphisms [TLR2 del -196 to -174 (rs111200466) and TLR2 19216T/C (rs3804099)]. All samples included in this study were obtained from patients with gastric complaints who underwent an upper digestive endoscopy between January 2010 and March 2016 in the Gastroenterology Department, State Hospital of Bauru, São Paulo, Southeastern Region, Brazil. Patients treated with antibiotics, anti-inflammatory agents, chemotherapy drugs, radiotherapy or proton pump inhibitors within 30 days before endoscopy were not included in the study.
The case groups included 269 patients (123 men and 146 women; 147 H. pylori-positive and 122 H. pylori-negative; mean age, 50.89 ± 23.03 years) with a confirmed histopathological diagnosis of CG per the Sidney System[20] and 202 patients (152 men and 50 women; 86 H. pylori-positive and 116 H. pylori-negative; mean age, 66.26 ± 16.32 years) with a confirmed histopathological diagnosis of GC per Lauren’s classification[21]. The gastric disease-free control group (C) consisted of 381 patients (176 men and 205 women; mean age, 51.26 ± 16.77 years) who underwent endoscopy by medical indication, gave up gastric biopsy exclusively for this study, and were histopathologically confirmed to be negative for any gastric disease and for H. pylori infection by a trained professional of Sacred Heart University -Bauru-SP following the hospital standard (Table 1).
| Variables | Control, n = 381 | Chronic gastritis, n = 269 | Gastric cancer, n = 202 |
| Gender | |||
| Female | 205 (53.8) | 146 (54.3) | 50 (24.8) |
| Male | 176 (46.2) | 123 (45.7) | 152 (75.2) |
| Age in yr | |||
| mean ± SD | 51.26 ± 16.77 | 50.89 ± 23.03 | 66.26 ± 16.32 |
| Smoking | |||
| Yes | 79 (20.7) | 84 (31.2) | 142 (70.3) |
| No | 302 (79.3) | 185 (68.8) | 60 (29.7) |
| Drinking | |||
| Yes | 98 (25.7) | 115 (42.7) | 128 (63.3) |
| No | 281 (74.3) | 154 (57.3) | 74 (36.7) |
| Helicobacter pylori | |||
| Positive | 0 (0) | 122 (45.3) | 86 (42.6) |
| Negative | 381 (100) | 147 (54.7) | 116 (57.4) |
H. pylori infection was histologically established by Giemsa staining or the urease test performed by the Pathology Services of the State Hospital of Bauru, and the results were subsequently confirmed using PCR, as described in a previous study[22].
In addition, to quantify TLR2 mRNA levels, biopsies were collected during the endoscopic evaluation (gastric antrum and corpus regions) from 48 patients (29 men and 19 women; mean age, 53.10 ± 9.41 years; 16 H. pylori-positive and 32 H. pylori-negative) in the CG group, 36 patients (25 men and 11 women; mean age, 62.32 ± 14.66 years; 21 H. pylori-positive and 15 H. pylori-negative) in the GC group, and 14 individuals in the C group who were free of gastric cancer and H. pylori infection (9 men and 5 women; mean age, 49.58 ± 21.01 years).
DNA was extracted from peripheral blood following a previously published protocol[23] with modifications (using Ficoll-Paque™ PLUS to separate blood components), while total RNA and DNA were simultaneously extracted from tissue samples using the QIAamp® tissue kit (Qiagen, Germany) according to the reagent protocol and stored at -20 ºC.
The TLR2 -196 to -174 del polymorphism (rs111200466) was detected by allele-specific PCR, and restriction fragment length polymorphism (RFLP)-PCR was used to assess the TLR2 19216 T/C (rs3804099) polymorphism. For both PCR techniques, the reaction solution contained the following: 1 × buffer, 15.3 μL of ultrapure H2O, 2.0 μL (0.10 μmol/L) of dNTPs, 0.5 μL (25 mmol/L) of MgCl2, 1.25 μL of each primer (25 mmol/L), 0.2 μL (1 U) of Taq DNA polymerase, and 200 ng of genomic DNA. The amplification products of the TLR2 -196 to -174 del analysis and the digestion products of the TLR2 19216 T/C analysis were visualized on a 3% agarose-1000 gel (Invitrogen®) with ethidium bromide in the presence of a 100 bp molecular marker. To ensure greater genotyping reliability, a positive control (a heterozygous sample for the evaluated polymorphism) was included in all reactions. Approximately 10% of the samples were processed in duplicate for quality control purposes. Table 2 summarizes the location of both polymorphisms, minor allele frequency (MAF), PCR conditions, primer sets, and enzymes used in each assay.
| Genes | Location | MAF | Primers, 5’-3’ | Cycles | T° melting | Enzyme | Genotypes, bp |
| TLR2 -196 to -174 ins/del (rs111200466) | Chromosome 4:153684312-153684338 (intron variant) | 0.1952 (del) | F: CACGGAGGCAGCGAGAAA | 35 | 60 °C | - | ins/ins: 286 bp |
| R: CTGGGCCGTGCAAAGAAG | ins/del: 286 + 264 bp | ||||||
| del/del: 264 bp | |||||||
| TLR2 19216T/C (rs3804099) | Chromosome 4:153703504 (synonymous variant) | 0.4048(C) | F: TCCCTGGGCAGTCTTGAACATTTAG | 30 | 65 °C | TaiI | TT: 415 bp |
| TC: 415 + 109 + 306 bp | |||||||
| R: TGTCCAAATCAGTATCTCGCAGTTCC | CC: 306 + 109 bp |
Total RNA was extracted using an RNeasy Mini Kit (Qiagen, Germany) according to the manufacturer’s protocol. RNA concentration and quality were measured using a NanoDrop 2000 spectrophotometer (Thermo Fisher Scientific, United States) and a Bioanalyzer (Agilent, United States). A reverse transcription reaction was performed using a High Capacity cDNA kit (Applied Biosystems, Foster City, CA, United States) according to the protocol instructions.
Quantitative PCR was performed with a TaqMan® System (Life Technologies, United States) and the StepOne Plus Real-Time PCR system 2.2.3 (Applied Biosystems, United States) using a TaqMan probe specific for the TLR2 gene (Hs00610101_m1) and two reference genes, GUSB (Hs00187320_m1) and TBP (Hs00187332_m1). The reactions were performed in triplicate and included a negative control. Relative quantification (RQ) was performed using the 2-ΔΔCt method[24] after normalization to both reference genes, and 14 normal H. pylori-negative gastric tissue samples (C group) were used as a calibrator (RQ = 1.0). RQ was also performed for the samples stratified by polymorphism genotype (at least one polymorphic allele vs wild-type homozygote) and H. pylori infection (negative vs positive). The data were expressed as median values.
SNPStats software was used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) for the risk associations between polymorphisms and gastric diseases. The multiple logistic regression models were adjusted for age, gender, and H. pylori infection. The effect of the polymorphisms was evaluated in the models as (1) codominant (heterozygous vs wild-type homozygous, and polymorphic homozygous vs wild-type homozygous); (2) dominant (heterozygous + polymorphic homozygous vs wild-type homozygous); (3) recessive (polymorphic homozygous vs wild-type homozygous + heterozygous); (4) overdominant (heterozygous vs wild-type homozygous + polymorphic homozygous); or (5) log-additive (polymorphic homozygous with 2 + heterozygous vs wild-type homozygous).
The RQ values for TLR2 mRNA were statistically analyzed. The continuous data distribution was evaluated using the D’Agostino-Pearson omnibus test for normality. The Mann-Whitney test and Wilcoxon’s signed rank test were used for comparisons between groups (GC, CG and C) to analyze the influence of H. pylori infection and polymorphisms on TLR2 mRNA expression. Statistical analyses were performed using GraphPad Prism 5 software and SNPstats online tool (https://www. snpstats.net/start.htm). A probability level (P) of < 0.05 was considered to indicate statistical significance. MAF and Hardy-Weinberg equilibrium were evaluated using OEGE software[25].
The genotype and allele frequency distributions of the two polymorphisms complied with Hardy-Weinberg equilibrium in both the case and control groups (data not shown). The genotype frequencies of the TLR2 -196 to -174 ins/del and TLR2 19216 T/C polymorphisms in all three groups (GC vs C, CG vs C, and GC vs CG) are shown in Table 3.
| Polymorphisms | Models | Genotypes | C, n = 381 | Case | |||||||
| GC | CG | GC x CG | |||||||||
| n = 202 | OR (95%CI) | P value | n = 269 | OR (95%CI) | P value | OR (95%CI) | P value | ||||
| TLR2 -196 to -174 ins/del (rs111200466) | Codomi-nant | ins/ins | 316 (82.9) | 112 (55.5) | 1.00 | < 0.0001 | 212 (78.8) | 1.00 | 0.4100 | 1.00 | < 0.0001 |
| ins/del | 60 (15.8) | 79 (39.1) | 3.70 (2.41-5.70) | 53 (19.7) | 1.32 (0.88-1.98) | 2.68 (1.71-4.20) | |||||
| del/del | 5 (1.3) | 11 (5.5) | 5.73 (1.80-18.21) | 4 (1.5) | 1.19 (0.32-4.49) | 5.06 (1.45-17.70) | |||||
| Dominant | ins/ins | 316 (82.9) | 112 (55.5) | 1.00 | < 0.0001 | 212 (78.8) | 1.00 | 0.1900 | 1.00 | < 0.0001 | |
| ins/del | 65 (17.1) | 90 (44.5) | 3.87 (2.55-5.86) | 57 (21.2) | 1.31 (0.88-1.94) | 2.84 (1.84-4.39) | |||||
| del/del | |||||||||||
| Recessive | ins/ins | 376 (98.7) | 191 (94.5) | 1.00 | 0.0130 | 265 (98.5) | 1.00 | 0.8500 | 1.00 | 0.0260 | |
| ins/del | |||||||||||
| del/del | 5 (1.3) | 11 (5.5) | 4.00 (1.27-12.62) | 4 (1.5) | 1.13 (0.30-4.26) | 3.77 (1.08-13.12) | |||||
| Overdo-minant | ins/ins | 321 (84.2) | 123 (60.9) | 1.00 | < 0.0001 | 216 (80.3) | 1.00 | 0.1900 | 1.00 | < 0.0001 | |
| del/del | |||||||||||
| ins/del | 60 (15.8) | 79 (39.1) | 3.44 (2.24-5.27) | 53 (19.7) | 1.31 (0.87-1.97) | 2.49 (1.59-3.88) | |||||
| Log-additive | --- | --- | --- | 3.23 (2.23-4.69) | < 0.0001 | --- | 1.25 (0.88-1.79) | 0.2200 | 2.54 (1.72-3.74) | < 0.0001 | |
| TLR2 19216T/C (rs3804099) | Codomi-nant | T/T | 157 (41.2) | 101 (50.0) | 1.00 | 0.0920 | 131 (48.7) | 1.00 | 0.1600 | 1.00 | 0.8900 |
| T/C | 175 (45.9) | 83 (41.1) | 0.72 (0.49-1.06) | 106 (39.4) | 0.73 (0.52-1.01) | 0.95 (0.63-1.44) | |||||
| C/C | 49 (12.9) | 18 (8.9) | 0.56 (0.30-1.05) | 32 (11.9) | 0.78 (0.47-1.29) | 0.85 (0.43-1.69) | |||||
| Dominant | T/T | 157 (41.2) | 101 (50.0) | 1.00 | 0.0420 | 131 (48.7) | 1.00 | 0.0580 | 1.00 | 0.7100 | |
| T/T | 224 (58.8) | 101 (50.0) | 0.68 (0.45-0.99) | 138 (51.3) | 0.74 (0.54-1.01) | 0.93 (0.63-1.38) | |||||
| T/C | |||||||||||
| Recessive | T/T | 332 (87.1) | 184 (91.1) | 1.00 | 0.1600 | 237 (88.1) | 1.00 | 0.7100 | 1.00 | 0.6800 | |
| T/C | |||||||||||
| C/C | 49 (12.9) | 18 (8.9) | 0.65 (0.36-1.19) | 32 (11.9) | 0.91 (0.57-1.47) | 0.87 (0.45-1.68) | |||||
| Overdo-minant | T/T | 206 (54.1) | 119 (58.9) | 1.00 | 0.2500 | 163 (60.6) | 1.00 | 0.0970 | 1.00 | 0.9000 | |
| C/C | |||||||||||
| T/C | 175 (45.9) | 83 (41.1) | 0.81 (0.56-1.17) | 106 (39.4) | 0.77 (0.56-1.05) | 0.98 (0.65-1.46) | |||||
| Log-additive | --- | --- | --- | 0.74 (0.56-0.97) | 0.0300 | --- | 0.83 (0.66-1.05) | 0.1200 | 0.93 (0.69-1.26) | 0.6400 | |
TLR2 -196 to -174 del was associated with a higher risk of GC by comparison with the C group in the codominant [odds ratio (OR) = 3.70, 95%CI: 2.41-5.70 for TLR2 -196 to -174 ins/del; OR = 5.73, 95%CI: 1.80-18.21 for TLR2 -196 to -174 del/del; P < 0.0001], dominant (OR = 3.87, 95%CI: 2.55-5.86; P < 0.0001), recessive (OR = 4.00, 95%CI: 1.27-12.62; P = 0.0130), overdominant (OR = 3.44, 95%CI: 2.24-5.27; P < 0.0001), and log-additive models (OR = 3.23, 95%CI: 2.23-4.69; P < 0.0001). Similarly, this polymorphism was associated with an increased risk when comparing the GC and CG groups in the codominant (OR = 2.68, 95%CI: 1.71-4.20 for TLR2 -196 to -174 ins/del; OR = 5.06, 95%CI: 1.45-17.70 for TLR2 -196 to -174 del/del; P < 0.0001), dominant (OR = 2.84, 95%CI: 1.84-4.39; P < 0.0001), overdominant (OR = 2.49, 95%CI: 1.59-3.88; P < 0.0001), recessive (OR = 3.77, 95%CI: 1.08-13.12; P = 0.0260), and log-additive models (OR = 2.54, 95%CI: 1.72-3.74; P < 0.0001). However, no association was found with this polymorphism in the comparison of the CG and C groups (Table 3).
TLR2 19216T/C was associated with a protective effect against GC development compared to the C group by the dominant (OR = 0.68, 95%CI: 0.47-0.99; P = 0.0420) and log-additive models (OR = 0.74, 95%CI: 0.56-0.97; P = 0.0300). However, no association was found for the CG vs C and CG vs GC comparisons (Table 3).
Both polymorphisms were also investigated to evaluate their association with H. pylori infection. Thus, all the samples, including those in the case and control groups, were divided into H. pylori-negative cases (n = 619, 73%) and H. pylori-positive cases (n = 233, 27%). For the TLR2 -196 to -174 ins/del polymorphism, an association was observed with H. pylori-positive individuals in the codominant (OR = 1.55, 95%CI: 1.09-2.19 for TLR2 -196 to -174 ins/del; OR = 2.48, 95%CI: 1.01-6.08 for TLR2 -196 to -174 del/del; P = 0.0120), dominant (OR = 1.62, 95%CI: 1.16-2.27; P = 0.0051), overdominant (OR = 1.50, 95%CI: 1.06-2.12; P = 0.0240), and log-additive models (OR = 1.56, 95%CI: 1.17-2.08; P = 0.0030). In contrast, the TLR2 19216T/C polymorphism was associated with protection against H. pylori infection in the codominant (OR = 0.60, 95%CI: 0.44-0.83 for TLR2 19216T/C; OR = 0.58, 95%CI: 0.35-0.98 for TLR2 19216C/C; P = 0.0039), dominant (OR = 0.60, 95%CI: 0.44-0.81; P < 0.0001); overdominant (OR = 0.67, 95%CI: 0.49-0.91; P = 0.0097), and log-additive models (OR = 0.70, 95%CI: 0.55-0.88; P = 0.0021) (Table 4).
| Polymorphisms | Models | Genotypes/ alleles | Case | |||
| H. pylori-positive, n = 619 | H. pylori-negative, n = 233 | OR (95%CI) | P value | |||
| TLR2 -196 to -174 ins/del (rs111200466) | Codominant | ins/ins | 481 (77.7) | 159 (68.2) | 1.00 | 0.0120 |
| ins/del | 127 (20.5) | 65 (27.9) | 1.55 (1.09-2.19) | |||
| del/del | 11 (1.8) | 9 (3.9) | 2.48 (1.01-6.08) | |||
| Dominant | ins/ins | 481 (77.7) | 159 (68.2) | 1.00 | 0.0051 | |
| ins/del | 138 (22.3) | 74 (31.8) | 1.62 (1.16-2.27) | |||
| del/del | ||||||
| Recessive | ins/ins | 608 (98.2) | 224 (96.1) | 1.00 | 0.0880 | |
| ins/del | ||||||
| del/del | 11 (1.8) | 9 (3.9) | 2.22 (0.91-5.43) | |||
| Overdo-minant | ins/ins | 492 (79.5) | 168 (72.1) | 1.00 | 0.0240 | |
| del/del | ||||||
| ins/del | 127 (20.5) | 65 (27.9) | 1.50 (1.06-2.12) | |||
| Log-additive | --- | --- | --- | 1.56 (1.17-2.08) | 0.0030 | |
| TLR2 19216T/C (rs3804099) | Codominant | T/T | 261 (42.2) | 128 (54.9) | 1.00 | 0.0039 |
| T/C | 281 (45.4) | 83 (35.6) | 0.60 (0.44-0.83) | |||
| C/C | 77 (12.4) | 22 (9.4) | 0.58 (0.35-0.98) | |||
| Dominant | T/T | 261 (42.2) | 128 (54.9) | 1.00 | < 0.0001 | |
| T/C – C/C | 358 (57.8) | 105 (45.1) | 0.60 (0.44-0.81) | |||
| Recessive | T/T – T/C | 542 (87.6) | 211 (90.6) | 1.00 | 0.2200 | |
| C/C | 77 (12.4) | 22 (9.4) | 0.73 (0.45-1.21) | |||
| Overdo-minant | T/T – C/C | 338 (54.6) | 150 (64.4) | 1.00 | 0.0097 | |
| T/C | 281 (45.4) | 83 (35.6) | 0.67 (0.49-0.91) | |||
| Log-additive | --- | --- | --- | 0.70 (0.55-0.88) | 0.0021 | |
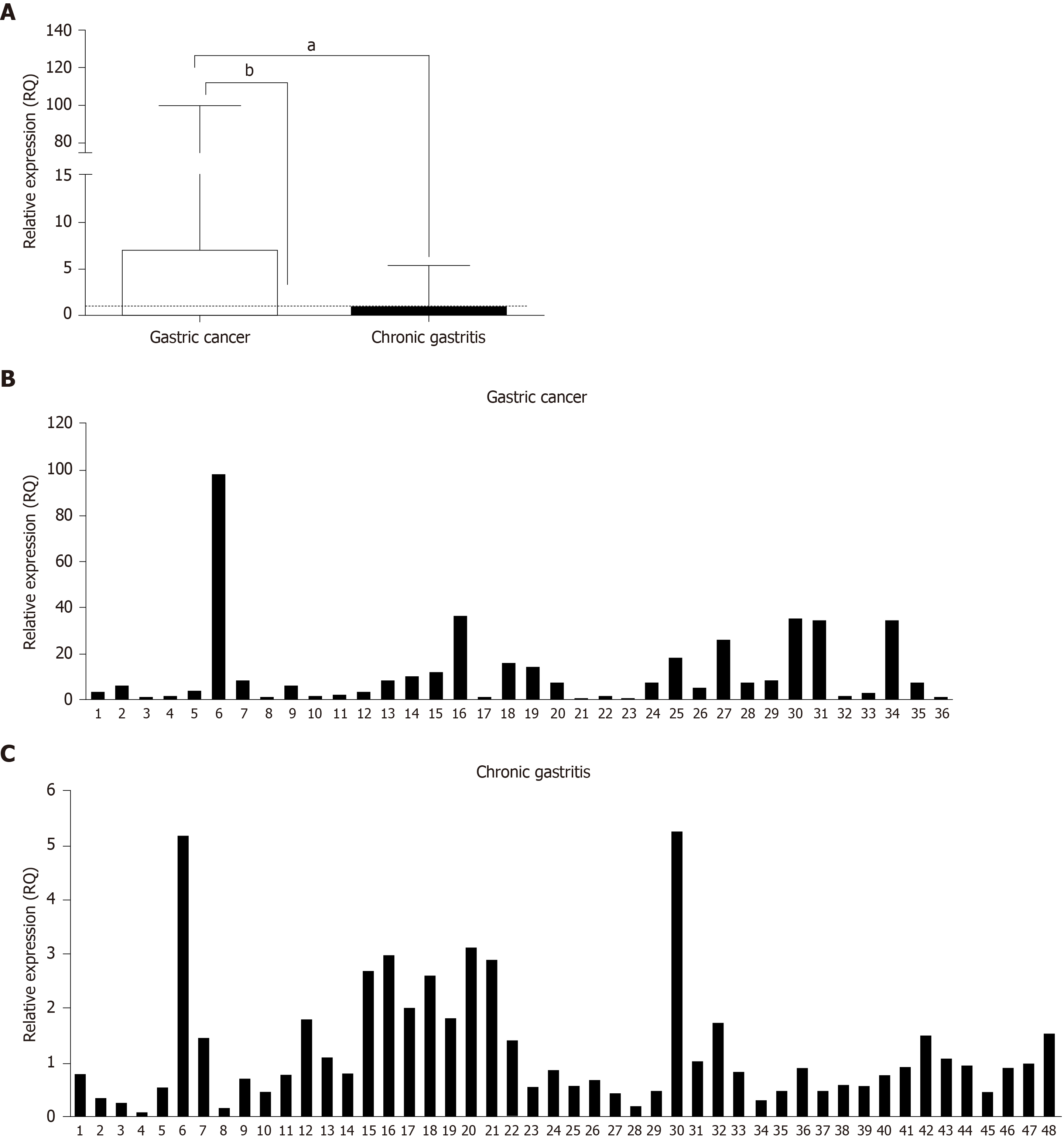
The relative expression of TLR2 mRNA in the GC and CG groups is shown in Figure 1. We observed significantly increased TLR2 mRNA expression in the GC group (median RQ = 6.95) compared to CG group (median RQ = 0.84, P < 0.0001) and C group (RQ = 1; P < 0.0001). However, we did not find a statistically significant difference between the CG and C groups (P = 0.9387).
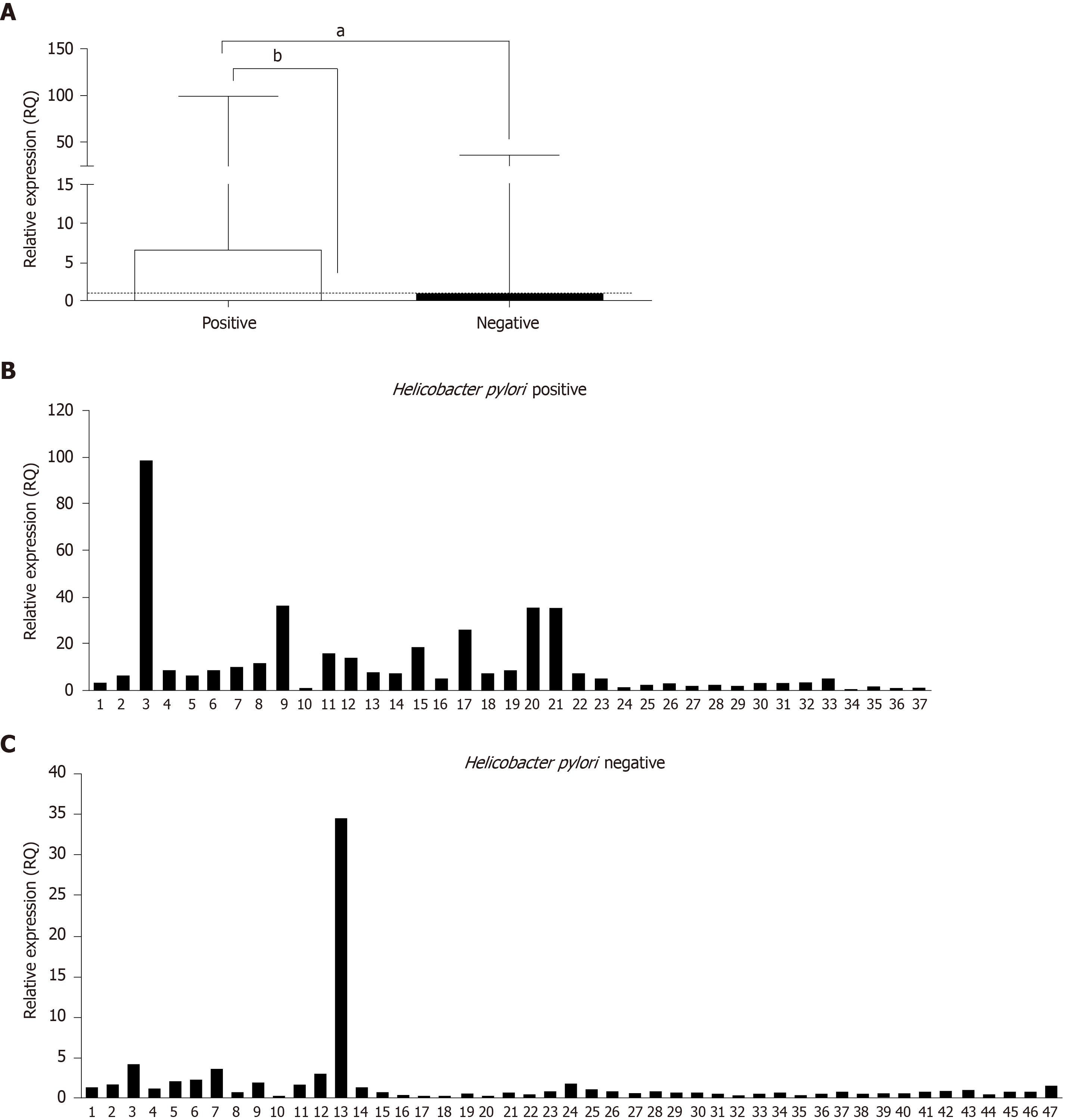
Another analysis was performed to determine whether H. pylori infection influences TLR2 mRNA levels. Samples from the GC and CG groups were separated according to the presence or absence of H. pylori infection and compared. The results showed significantly higher TLR2 mRNA expression in H. pylori-positive cases (median RQ = 6.38) than in H. pylori-negative cases (median RQ = 0.79; P < 0.0001; Figure 2). We observed significantly increased TLR2 mRNA expression in the H. pylori-positive cases group compared to C group (median RQ = 1, P < 0.0001), but not between H. pylori-negative cases vs C group (RQ = 1; P = 0.4305).
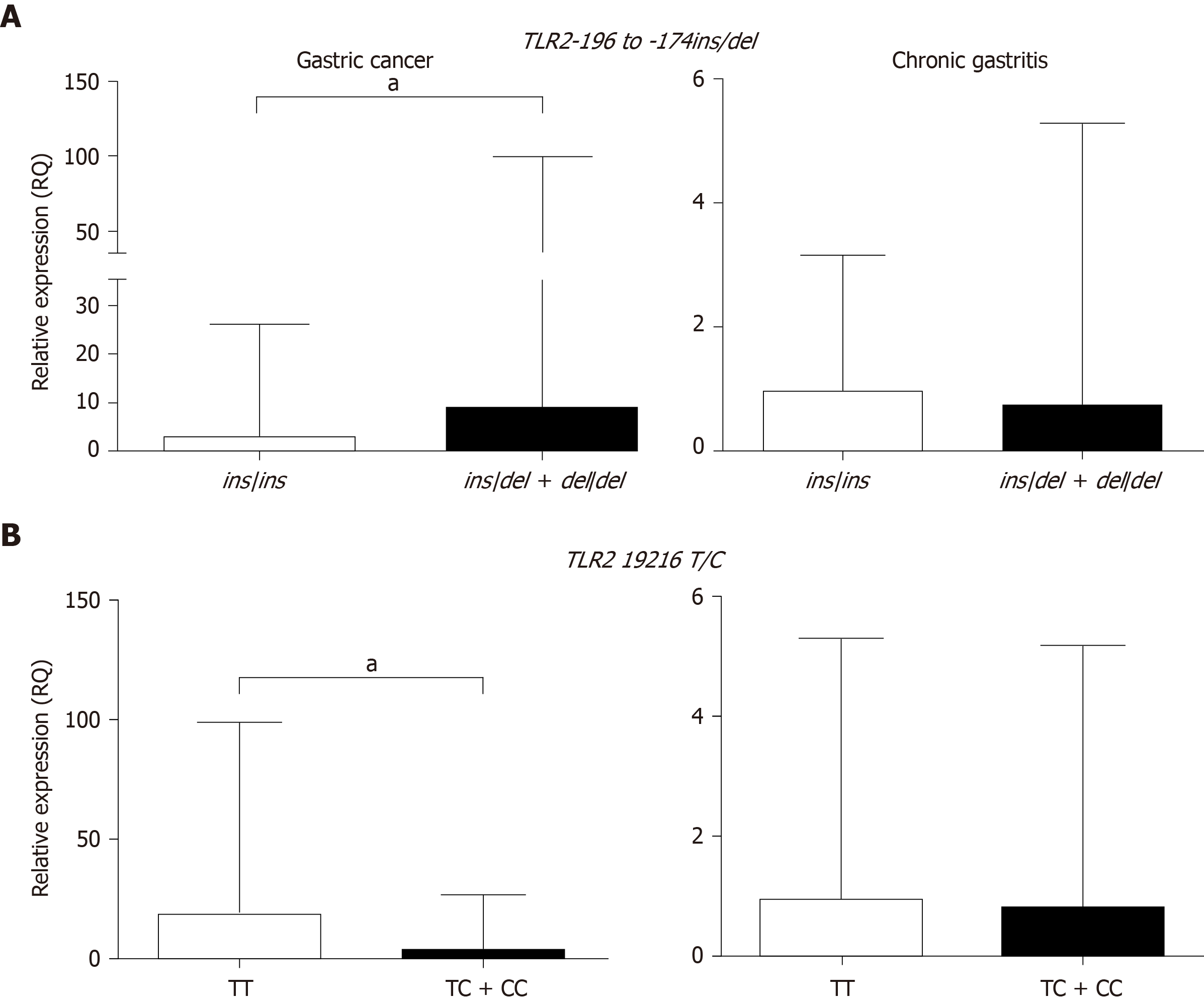
To evaluate the influence of the TLR2 -196 to -174 ins/del and TLR2 19216T/C polymorphisms on mRNA expression, the samples were grouped based on the presence of at least one polymorphic allele or a wild-type genotype (Table 5 and Figure 3).
In the GC group, individuals with at least one polymorphic TLR2 -196 to -174 del allele had greater than four-fold higher TLR2 mRNA expression in tumor tissue (median RQ = 8.74) than those with the wild-type genotype (median RQ = 2.58, P = 0.0010). In contrast, carriers of TLR2-19216 TC + CC polymorphic variants showed reduced expression (median RQ = 3.63) compared to those harboring the wild-type TLR2 -19216 TT allele (median RQ = 18.54, P = 0.0004). In the CG group, when the individuals were grouped as TLR2 -196 to -174 ins/del + del/del or TLR2-19216 TC + CC polymorphic allele carriers and homozygous wild-type allele carriers, the differences between the groups were not statistically significant (P = 0.5334 and P = 0.8827, respectively).
In our analyses, we demonstrated an association between the TLR2 -196 to -174 ins/del and TLR2 19216 T/C polymorphisms and gastric cancer (an increased risk and a protective effect, respectively), as well as greater susceptibility to H. pylori presence. Infection of the gastric mucosa by H. pylori leads to increased inflammation that contributes to cancer development, and factors that promote an exacerbated immune response may interfere with this process[26].
Regarding the TLR2 -196 to -174 ins/del (rs111200466) polymorphism, two meta-analyses have shown no association with gastric cancer risk, but in the Chinese population, an increased risk for gastric carcinogenesis was reported in H. pylori-infected individuals, reinforcing the importance of this microorganism in disease pathogenesis[27,28]. In contrast, a recent study in a southern Chinese population showed a risk association for gastric cancer; however, no association with H. pylori infection was observed[8].
Other studies have reported a risk association between the TLR2 -196 to -174 del variant and head and neck cancer[15,29], cervical cancer in the Tunisian population[30], breast cancer in the Greek population[13], and prostate[31] and bladder cancer in the Indian population[32]. In the Brazilian population, previous studies demonstrated a risk association for gastric and colorectal cancer [14,33].
For TLR2 19216T/C (rs3804099), our results demonstrated a protective association between the TC and CC genotypes and gastric cancer. This protective association has been previously reported for some types of cancer, such as colorectal, breast, gastric, and hepatocellular carcinoma, but all these studies were in the Asian population[16-18,34]. Two recent studies evaluated this polymorphism in the Thai population but failed to demonstrate any association with the development of gastric lesions or with H. pylori infection[35,36]. Thus, our study shows this protective association of TLR2 19216T/C with gastric cancer in the Brazilian population.
When we analyzed TLR2 mRNA expression, we found significantly higher levels of TLR2 mRNA in gastric cancer tissues than in chronic gastritis tissues. In the literature, a study in gastric cancer indicates that the TLR2 mRNA expression levels were significantly increased in tumor tissues compared to either adjacent non-tumor tissues or normal tissues from GC-free individuals, regardless of risk factors or H. pylori infection[37]. Similarly, a previous study from our research group also evaluated TLR2 receptor expression in different premalignant lesions (chronic gastritis, gastric atrophy, metaplasia) and observed a slight increase in TLR2 gene and protein expression in relation to normal gastric tissues[38].
Therefore, these studies showed that TLR2 mRNA expression levels are mainly increased in tumor tissue, and not in the chronic gastritis group, as this is a benign lesion that likely does not yet present significant alterations in genes associated with carcinogenesis.
Similar results were observed in colorectal cancer in the Brazilian population, where the relative mRNA expression in tumor tissues was 2.36-fold higher than that in adjacent normal tissues, and a strong immunostaining pattern was observed in the epithelium of tumor tissues[14]. In 2018, Semlali et al[16] analyzed TLR2 mRNA expression in the Saudi Arabian population and showed a decrease in TLR2 mRNA in colon cancer tissues compared to normal colon tissues, and this result was confirmed by immunohistochemistry.
This is the first study in gastric lesions to demonstrate the regulation of gene expression in the presence of variant genotypes (TLR2 -196 to -174 ins/del + del/del and TLR2 19216 T/C+C/C) and H. pylori infection, regardless of the type of lesion (cancer or gastritis). Thus, when we stratified gastric cancer tissue samples according to wild-type or variant genotypes, carriers of the TLR2 -196 to -174 ins/del + del/del genotypes had higher TLR2 mRNA expression levels than carriers of the ins/ins genotype. This finding supports the hypothesis that gene expression may be affected by allele variants in the promoter region and that H. pylori infection can influence the inflammatory profile mediated by TLRs. Proença et al[14] observed similar results in colorectal cancer, where TLR2 mRNA expression was 2.19-fold higher in TLR2 -196 to -174 del variant carriers than in wild-type genotype carriers[14].
Conversely, the opposite was observed for TLR2 19216 T/C+C/C variant carriers (this polymorphism has a protective effect in gastric cancer), who had reduced TLR2 expression levels with respect to TT wild-type genotype carriers. Thus, these data corroborate the results regarding the protective effect of the TLR2 19216 T/C+C/C genotype, which leads to the negative regulation of gene expression. An in silico analysis of the TLR2 nucleotide substitution in rs3804099 predicted a 70% probability that this SNP affects TLR2 mRNA splicing due to the creation of an additional splice site. Thus, this variant may alter protein expression, receptor conformation, and function[16].
Although the TLR2 19216T/C polymorphism results in a synonymous alteration (Asn199Asn), some genetic studies have shown a contribution of synonymous mutations to the risk of human diseases, including cancer[39]. A polymorphism in the epidermal growth factor receptor (EGFR) gene (rs2293347) has been identified as a potential predictor of the clinical outcome of treatment for advanced non-small-cell lung carcinoma[40]. Similarly, nonsynonymous SNPs in the Nijmegen breakage syndrome 1 (NBS1) gene (rs709816 and rs1061302) were associated with smoking-related cancers[41], and the tumor suppressor p53 (TP53) gene (rs111287251) was associated with overall tumor susceptibility[42].
The high expression of TLR2 results in the recruitment of MyD88 to the TLR/TIR domain and in the production of inflammatory response cytokines by a classic signaling pathway, the NF-κB pathway, that exacerbates inflammation and thus facilitates tumor progression[5].
In conclusion, our findings show that the TLR2 -196 to -174 ins/del and TLR2 19216 T/C polymorphisms are associated with gastric cancer (an increased risk and a protective effect, respectively) and H. pylori infection in the Brazilian population. Additionally, our results indicate that TLR2 mRNA levels are upregulated in gastric cancer tissue, mainly in the presence of the TLR2 -196 to -174 del variant allele, the TLR2 19216 T wild-type allele, and H. pylori infection. Thus, genetic polymorphisms may change gene expression, such as TLR2 polymorphisms, alter the immune response profile, and consequently increase the risk and clinical manifestations of gastric cancer.
Helicobacter pylori (H. pylori) infection is a carcinogen for gastric cancer (GC), and Toll-like receptors are involved in recognition and activation of the inflammatory response for this bacterium. The presence of single nucleotide polymorphism (SNP) genes responsible for activating the innate immunity may influence the risk of precancerous lesions and GC, among them of which include TLR2 polymorphisms. GC is the fifth most common cancer worldwide, mortality rates are still high. In Brazil, GC is the fourth most frequent type of cancer in men, and the sixth in women, with an estimated incidence of 21230 new cases in 2020.
Considering the inconsistent results in the literature, as well as the importance of these receptors in immune response and for the susceptibility to inflammatory diseases and cancer, new studies are needed. The Brazilian population is highly mixed; thus it becomes important to confirm the real role among the factors that influence changes in the recognition of H. pylori and gastric carcinogenesis.
The aim of this study was to evaluate whether the TLR2 19216T/C (rs3804099) and TLR2 -196 to -174 ins/del (rs111200466) polymorphisms contribute to gastric carcinogenesis in the Brazilian population. In addition, we also evaluate the influence of both polymorphisms and H. pylori infection on TLR2 mRNA expression. The results may highlight important polymorphisms that act on gastric carcinogenesis.
A case-control study was conducted to evaluate two TLR2 SNPs (TLR2 19216T/C -rs3804099 and TLR2 -196 to -174 ins/del - rs111200466) in CG and GC patients. A total of 854 DNA samples of peripheral blood [269 CG, 202 GC, and 383 samples from healthy individuals (C)] were genotyped by allele-specific PCR or restriction fragment length polymorphism (RFLP)-PCR. Quantitative polymerase chain reaction by TaqMan® assay was used to quantify TLR2 mRNA from fresh gastric tissues (48 GC, 26 CG, and 14 C).
The data showed that for the TLR2 -196 to -174 polymorphism, the ins/del and del/del genotypes were associated with a higher risk of GC compared with the C and CG groups. In contrast, TLR2 19216T/C was associated with a protective effect in the GC group compared to the C group. Regarding the association of polymorphisms with H. pylori infection, for the TLR2 -196 to -174 ins/del polymorphism, an association was observed with H. pylori-positive, while TLR2 19216T/C was associated with protection against H. pylori infection. TLR2 mRNA levels were significantly higher in the GC group compared to the CG group and normal mucosa. In addition, when the samples were grouped according to polymorphic genotypes and the presence of H. pylori, the two SNPs (TLR2 -196 to -174del and TLR2 19216 C alleles) and H. pylori infection influenced TLR2 mRNA expression.
Our findings highlight that the polymorphisms of the TLR2 -196 to -174 ins/del and TLR2 19216 T/C receptors are associated with gastric cancer (an increased risk and a protective effect, respectively) and H. pylori infection, and therefore may act as a potential factor in the progression of gastric carcinogenesis. TLR2 mRNA expression levels are upregulated in gastric cancer tissues and are influenced by the TLR2 -196 to -174 del variant allele, the TLR2 19216 T wild-type allele and H. pylori infection. Considering that most cases of GC have a good prognosis and are treatable when diagnosed at an early stage, it is of the utmost importance to establish molecular markers capable of identifying risk groups and providing early diagnosis in individuals with increased risk of developing this neoplasm. Thus, polymorphisms in genes that affect its expression, such as TLR2, could have an effect on the development and clinical manifestation of disease.
The pattern of the host’s immune response associated with genetic and environmental factors are essential for understanding the pathology of gastric cancer. Overall, our results indicate that the TLR2 gene plays an important role in gastric carcinogenesis, highlighting the importance of the TLR2 -196 to -174 del and TLR2 19216 T polymorphisms in increasing gene expression and H. pylori infection, possibly triggering a stronger inflammatory response, which in turn enhances the risk of tumor progression. In the future, it would be important to increase the biopsies collected during the endoscopic evaluation to quantify TLR2 mRNA levels, and investigate another polymorphism in the TLR2 gene (rs3804100, rs7696323, and rs10116253), described in the literature as associated with cancer, but not yet analyzed in our Brazilian population.
The authors are grateful to Lilian Castiglione for her support with the statistical analysis.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Hu X, Limpakan S, Nadatani Y, Park WS S-Editor: Gong ZM L-Editor: Filipodia E-Editor: Qi LL
| 1. | Correa P. A human model of gastric carcinogenesis. Cancer Res. 1988;48:3554-3560. [PubMed] |
| 2. | Koulis A, Buckle A, Boussioutas A. Premalignant lesions and gastric cancer: Current understanding. World J Gastrointest Oncol. 2019;11:665-678. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | (IARC) IAfRoC. Schistossomes, liver flukes and Helicobacter pylori. Lyon. 1994;. |
| 4. | Toor D, Wsson MK, Kumar P, Karthikeyan G, Kaushik NK, Goel C, Singh S, Kumar A, Prakash H. Dysbiosis Disrupts Gut Immune Homeostasis and Promotes Gastric Diseases. Int J Mol Sci. 2019;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 96] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 5. | Meliț LE, Mărginean CO, Mărginean CD, Mărginean MO. The Relationship between Toll-like Receptors and Helicobacter pylori-Related Gastropathies: Still a Controversial Topic. J Immunol Res. 2019;2019:8197048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 6. | Rudnicka K, Backert S, Chmiela M. Genetic Polymorphisms in Inflammatory and Other Regulators in Gastric Cancer: Risks and Clinical Consequences. Curr Top Microbiol Immunol. 2019;421:53-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Mommersteeg MC, Yu J, Peppelenbosch MP, Fuhler GM. Genetic host factors in Helicobacter pylori-induced carcinogenesis: Emerging new paradigms. Biochim Biophys Acta Rev Cancer. 2018;1869:42-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 8. | Huang J, Hang JJ, Qin XR, Huang J, Wang XY. Interaction of H. pylori with toll-like receptor 2-196 to -174 ins/del polymorphism is associated with gastric cancer susceptibility in southern China. Int J Clin Oncol. 2019;24:494-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Zeng HM, Pan KF, Zhang Y, Zhang L, Ma JL, Zhou T, Su HJ, Li WQ, Li JY, Gerhard M, Classen M, You WC. Genetic variants of toll-like receptor 2 and 5, helicobacter pylori infection, and risk of gastric cancer and its precursors in a chinese population. Cancer Epidemiol Biomarkers Prev. 2011;20:2594-2602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Hishida A, Matsuo K, Goto Y, Hamajima N. Genetic predisposition to Helicobacter pylori-induced gastric precancerous conditions. World J Gastrointest Oncol. 2010;2:369-379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 11. | Tahara T, Arisawa T, Wang F, Shibata T, Nakamura M, Sakata M, Hirata I, Nakano H. Toll-like receptor 2 (TLR) -196 to 174del polymorphism in gastro-duodenal diseases in Japanese population. Dig Dis Sci. 2008;53:919-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | de Oliveira JG, Rossi AF, Nizato DM, Miyasaki K, Silva AE. Profiles of gene polymorphisms in cytokines and Toll-like receptors with higher risk for gastric cancer. Dig Dis Sci. 2013;58:978-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Theodoropoulos GE, Saridakis V, Karantanos T, Michalopoulos NV, Zagouri F, Kontogianni P, Lymperi M, Gazouli M, Zografos GC. Toll-like receptors gene polymorphisms may confer increased susceptibility to breast cancer development. Breast. 2012;21:534-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Proença MA, de Oliveira JG, Cadamuro AC, Succi M, Netinho JG, Goloni-Bertolo EM, Pavarino ÉC, Silva AE. TLR2 and TLR4 polymorphisms influence mRNA and protein expression in colorectal cancer. World J Gastroenterol. 2015;21:7730-7741. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 15. | Makni L, Zidi S, Barbiroud M, Ahmed AB, Gazouani E, Mezlini A, Stayoussef M, Yacoubi-Loueslati B. Increased risks between TLR2 (-196 to -174 ins/del) and TLR3 1377C>T variants and head and neck cancers in Tunisia. Cent Eur J Immunol. 2019;44:144-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Semlali A, Parine NR, Al-Numair NS, Almutairi M, Hawsawi YM, Amri AA, Aljebreen AM, Arafah M, Almadi MA, Azzam NA, Alharbi O, Alanazi MS. Potential role of Toll-like receptor 2 expression and polymorphisms in colon cancer susceptibility in the Saudi Arabian population. Onco Targets Ther. 2018;11:8127-8141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Semlali A, Almutairi M, Parine NR, Al Amri A, Shaik JP, Al Naeem A, Abdulla Ajaj S, Rouabhia M, Alanazi MS. No genetic relationship between TLR2 rs4696480, rs3804100, and rs3804099 gene polymorphisms and female breast cancer in Saudi populations. Onco Targets Ther. 2017;10:2325-2333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Chen D, Xie W, Lu Y, Su S, Nong L, Jia Y, Liu Y, Zhou W, Wang H, Tan A. Gene polymorphisms of TLR2 and TLR3 in HBV clearance and HBV-related hepatocellular carcinoma in a Chinese male population. Int J Biol Markers. 2017;32:e195-e201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Kutikhin AG, Ponasenko AV, Khutornaya MV, Yuzhalin AE, Zhidkova II, Salakhov RR, Golovkin AS, Barbarash OL, Barbarash LS. Association of TLR and TREM-1 gene polymorphisms with atherosclerosis severity in a Russian population. Meta Gene. 2016;9:76-89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161-1181. [PubMed] |
| 21. | Lauren P. The Two Histological Main Types of Gastric Carcinoma: Diffuse and So-Called Intestinal-Type Carcinoma. An Attempt at a Histo-Clinical Classification. Acta Pathol Microbiol Scand. 1965;64:31-49. [PubMed] |
| 22. | Rasmussen LT, Labio RW, Gatti LL, Silva LC, Queiroz VF, Smith Mde A, Payão SL. Helicobacter pylori detection in gastric biopsies, saliva and dental plaque of Brazilian dyspeptic patients. Mem Inst Oswaldo Cruz. 2010;105:326-330. [PubMed] |
| 23. | Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16:1215. [PubMed] |
| 24. | Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149116] [Cited by in RCA: 133611] [Article Influence: 5567.1] [Reference Citation Analysis (1)] |
| 25. | Rodriguez S, Gaunt TR, Day IN. Hardy-Weinberg equilibrium testing of biological ascertainment for Mendelian randomization studies. Am J Epidemiol. 2009;169:505-514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 804] [Cited by in RCA: 790] [Article Influence: 49.4] [Reference Citation Analysis (0)] |
| 26. | Fischer S. Pattern Recognition Receptors and Control of Innate Immunity: Role of Nucleic Acids. Curr Pharm Biotechnol. 2018;19:1203-1209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 27. | Castaño-Rodríguez N, Kaakoush NO, Goh KL, Fock KM, Mitchell HM. The role of TLR2, TLR4 and CD14 genetic polymorphisms in gastric carcinogenesis: a case-control study and meta-analysis. PLoS One. 2013;8:e60327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 28. | Chen J, Hu S, Liang S, Chen Q, Yang Q, Zheng W, Ma W. Associations between the four toll-like receptor polymorphisms and the risk of gastric cancer: a meta-analysis. Cancer Biother Radiopharm. 2013;28:674-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Makni L, Messadi A, Zidi S, Gazouani E, Mezlini A, Yacoubi-Loueslati B. TLR2 (-196 to -174 Ins/Del) and TLR3 (1377C>T) as biomarkers for nasopharyngeal cancer in Tunisia. Turk J Med Sci. 2017;47:1216-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Zidi S, Sghaier I, Gazouani E, Mezlini A, Yacoubi-Loueslati B. Evaluation of Toll-Like Receptors 2/3/4/9 Gene Polymorphisms in Cervical Cancer Evolution. Pathol Oncol Res. 2016;22:323-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 31. | Mandal RK, George GP, Mittal RD. Association of Toll-like receptor (TLR) 2, 3 and 9 genes polymorphism with prostate cancer risk in North Indian population. Mol Biol Rep. 2012;39:7263-7269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 32. | Singh V, Srivastava N, Kapoor R, Mittal RD. Single-nucleotide polymorphisms in genes encoding toll-like receptor -2, -3, -4, and -9 in a case-control study with bladder cancer susceptibility in a North Indian population. Arch Med Res. 2013;44:54-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 33. | de Oliveira JG, Silva AE. Polymorphisms of the TLR2 and TLR4 genes are associated with risk of gastric cancer in a Brazilian population. World J Gastroenterol. 2012;18:1235-1242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 74] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 34. | Zeng HM, Pan KF, Zhang Y, Zhang L, Ma JL, Zhou T, Su HJ, Li WQ, Li JY, You WC. [The correlation between polymorphisms of Toll-like receptor 2 and Toll-like receptor 9 and susceptibility to gastric cancer]. Zhonghua Yu Fang Yi Xue Za Zhi. 2011;45:588-592. [PubMed] |
| 35. | Tongtawee T, Simawaranon T, Wattanawongdon W, Dechsukhum C, Leeanansaksiri W. Toll-like receptor 2 and 4 polymorphisms associated with Helicobacter pylori susceptibility and gastric cancer. Turk J Gastroenterol. 2019;30:15-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Tongtawee T, Bartpho T, Kaewpitoon S, Kaewpitoon N, Dechsukhum C, Leeanansaksiri W, Loyd RA, Talabnin K, Matrakool L, Panpimanmas S. Genetic polymorphisms in TLR1, TLR2, TLR4, and TLR10 of Helicobacter pylori-associated gastritis: a prospective cross-sectional study in Thailand. Eur J Cancer Prev. 2018;27:118-123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 37. | West AC, Tang K, Tye H, Yu L, Deng N, Najdovska M, Lin SJ, Balic JJ, Okochi-Takada E, McGuirk P, Keogh B, McCormack W, Bhathal PS, Reilly M, Oshima M, Ushijima T, Tan P, Jenkins BJ. Identification of a TLR2-regulated gene signature associated with tumor cell growth in gastric cancer. Oncogene. 2017;36:5134-5144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 38. | Cadamuro AC, Rossi AF, Matos Biselli-Périco J, Fucuta Pereira P, Do Vale EP, Acayaba R, Leite KR, Goloni-Bertollo EM, Silva AE. Effect of Helicobacter pylori eradication on TLR2 and TLR4 expression in patients with gastric lesions. Mediators Inflamm. 2015;2015:481972. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 39. | Sauna ZE, Kimchi-Sarfaty C. Understanding the contribution of synonymous mutations to human disease. Nat Rev Genet. 2011;12:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 658] [Cited by in RCA: 711] [Article Influence: 50.8] [Reference Citation Analysis (0)] |
| 40. | Alenius M, Wadelius M, Dahl ML, Hartvig P, Lindström L, Hammarlund-Udenaes M. Gene polymorphism influencing treatment response in psychotic patients in a naturalistic setting. J Psychiatr Res. 2008;42:884-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 41. | Park SL, Bastani D, Goldstein BY, Chang SC, Cozen W, Cai L, Cordon-Cardo C, Ding B, Greenland S, He N, Hussain SK, Jiang Q, Lee YC, Liu S, Lu ML, Mack TM, Mao JT, Morgenstern H, Mu LN, Oh SS, Pantuck A, Papp JC, Rao J, Reuter VE, Tashkin DP, Wang H, You NC, Yu SZ, Zhao JK, Zhang ZF. Associations between NBS1 polymorphisms, haplotypes and smoking-related cancers. Carcinogenesis. 2010;31:1264-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 42. | Hrstka R, Coates PJ, Vojtesek B. Polymorphisms in p53 and the p53 pathway: roles in cancer susceptibility and response to treatment. J Cell Mol Med. 2009;13:440-453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |