Published online Dec 16, 2019. doi: 10.4253/wjge.v11.i12.548
Peer-review started: March 22, 2019
First decision: August 2, 2019
Revised: August 21, 2019
Accepted: September 11, 2019
Article in press: September 11, 2019
Published online: December 16, 2019
Processing time: 246 Days and 15.8 Hours
Endoscopic treatment of gastrointestinal diseases has developed rapidly in recent years, due to its minimally invasive nature. One of the main contributing factors for this progress is the improvement of endoscopic instruments, which are essential for facilitating safe and effective endoscopic interventions. However, the slow learning curve required in the implementation of many advanced endoscopic procedures using standard devices is associated with a high risk of complications. Other routine procedures may also be complicated by unexpected difficulties. Based on the ferromagnetic properties of many objects, both internal and external magnetic devices have been developed and applied for multiple endoscopic interventions. The applications of magnets, mainly including compression, anchoring and traction, facilitate many difficult procedures and make it feasible to operate procedures that were previously impossible. Other novel endoscopic applications, such as magnetic nanoparticles, are also under development. In this article, we reviewed published studies of endoscopic applications of magnets for the treatment of gastrointestinal diseases such as precancerous lesions and cancer, obstruction, stricture, congenital and acquired malformations, motility disorders, and ingestion of foreign bodies. Since several endoscopic applications of magnets may also be relevant to surgery, we included them in this review.
Core tip: Endoscopic applications of internal and external magnets can facilitate or even help develop multiple endoscopic interventions for treating gastrointestinal diseases, by providing compression, anchoring, and traction. This article aims to review therapeutic magnetic technologies, current applications and future developments.
- Citation: Hu B, Ye LS. Endoscopic applications of magnets for the treatment of gastrointestinal diseases. World J Gastrointest Endosc 2019; 11(12): 548-560
- URL: https://www.wjgnet.com/1948-5190/full/v11/i12/548.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i12.548
Due to the ferromagnetic properties, magnets have always been a focus of research in clinical practice. The initial application of magnets in the digestive tract can be traced back to the mid20th century[1,2], when magnets played a promising role in removing ingested foreign bodies. However, due to the widespread recognition of the perils of magnet ingestion[3,4], the therapeutic application of magnets has remained rare for a long time. In view of the safety associated with the extensive use of magnetic resonance imaging, many clinicians have reconsidered the roles that magnets could play in clinical medicine. Over the past 20 years, many innovative therapeutic uses of magnets have been reported, with early success, and the main applications of magnets include: compression anastomosis, compression without anastomosis, anchoring and traction. These applications, including endoscopic and surgical interventions for gastrointestinal diseases, have thus generated new attention. This article reviews the endoscopic applications of magnets in the treatment of gastrointestinal diseases. Surgical applications of magnets without endoscopes are excluded because they have been reviewed recently[5]. In addition, diagnostic applications including magnetic capsule manipulation[6] and magnetic navigation colonoscopy[7] are also beyond the scope of this review.
Applications of magnetic compression anastomosis in the esophagus include atresia[8-10] and diverticula[11-13].
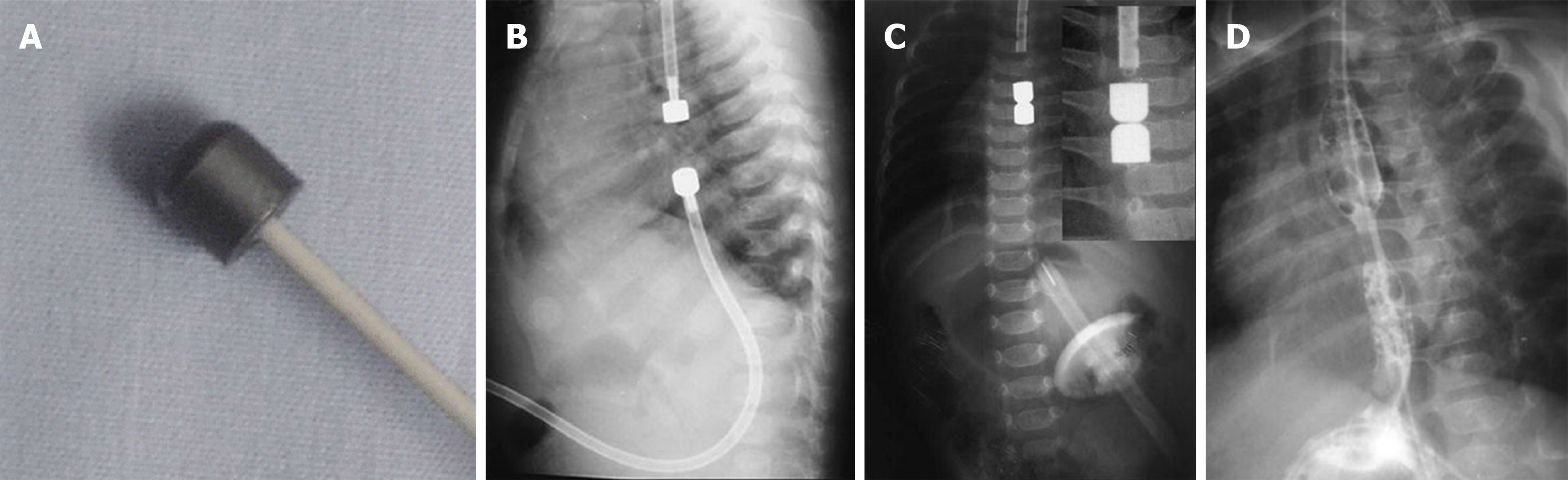
In 1975, Hendren et al[14] initially proposed the use of magnetic force for the treatment of esophageal atresia, and they used electromagnetic bougienage to lengthen esophageal segments to facilitate further surgical repair. The first application of magnets alone for esophageal atresia was reported by Zaritzky et al[8] in 2009, in which magnetic anastomosis was achieved by a mean of 4.8 days (range, 2-7 days) in all five children after placement of two catheter-mounted magnets to the proximal end (by mouth) and the distal end (by gastrostomy) of the atresia, respectively (Figure 1). The procedure was performed under fluoroscopic guidance with or without endoscopic assistance. Using a similar technique, both Dorman et al[9] and Ellebaek et al[10] achieved good results later in one case, respectively. Magnetic compression anastomosis for esophageal atresia helps to avoid adverse events of thoracotomy, including tracheal injury, devascularization and denervation of the esophagus[9]. Notably, esophageal stenosis could occur after magnetic compression anastomosis, and some of them may require repeated endoscopic dilation or even surgical intervention. The main cause of esophageal stenosis is the use of magnets with small diameters. Magnets with large diameters or self-assembling magnets may be applied to reduce stenosis. Preventative endoscopic dilation may also help to reduce the need for stenting or surgery[10].
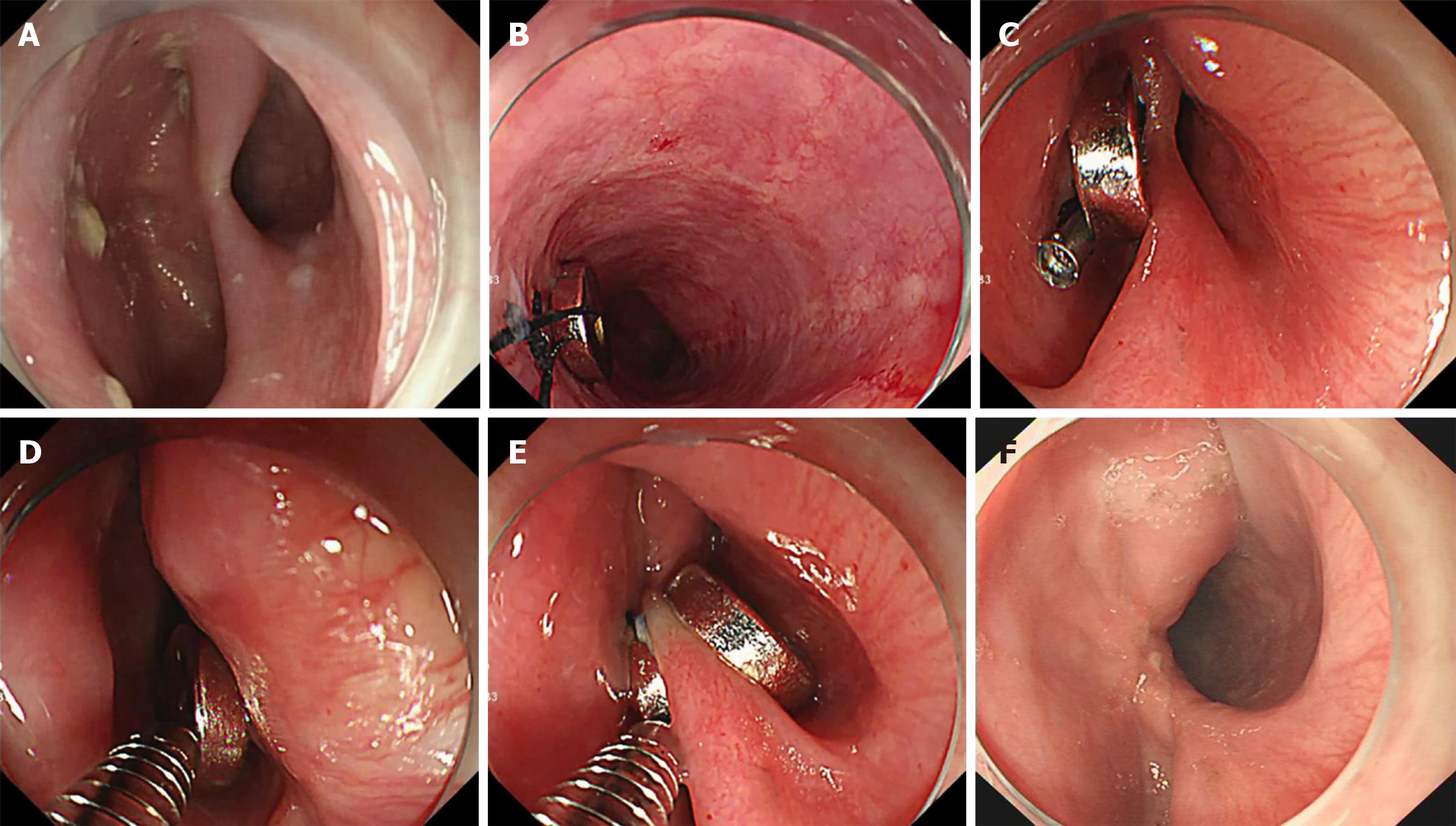
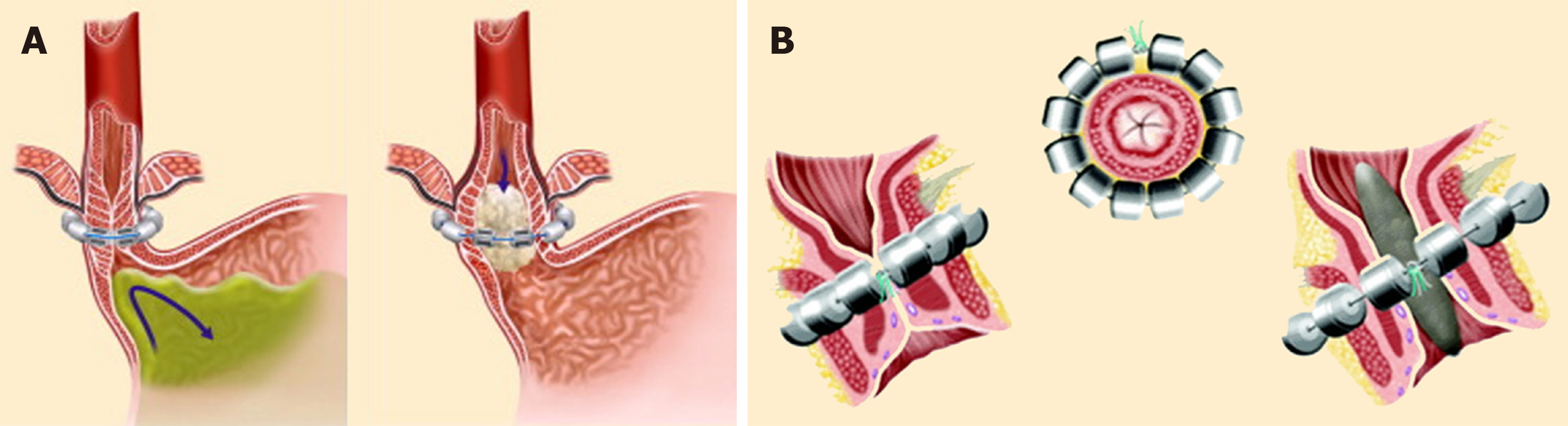
To date, there are only three reports including six cases of esophageal diverticulum (2 in the upper, 2 in the middle, and 2 in the distal esophagus) treated by magnetic compression anastomosis[11-13]. During the procedure, the first magnet can be introduced into the stomach or distal esophagus with the help of a catheter or a clip, and the second magnet can be placed at the base of the diverticulum. The binding of the two magnets can be achieved by pulling pack the first magnet under direct endoscopic visualization with or without fluoroscopic guidance (Figure 2). After 10-28 days, if a connecting hole is developed, diverticulotomy of the remaining part of the septum can be safely performed. Procedures can be repeated easily for better results if the diverticuloplasty is incomplete or if the diverticulum recurs. We first named this method “magnet-assisted diverticuloplasty (MAD)”[13]. MAD resolves the contradiction between complete transection of the septum and esophageal perforation when performing other endoscopic “clip and cut” diverticulotomy[15,16], as well as the need for endoscopic experts to perform the peroral endoscopic myotomy (POEM)[17-19]. Our limited experience suggests that this technique is easy, safe and effective, and that it would be especially suitable for high-risk patients with symptomatic esophageal diverticulum.
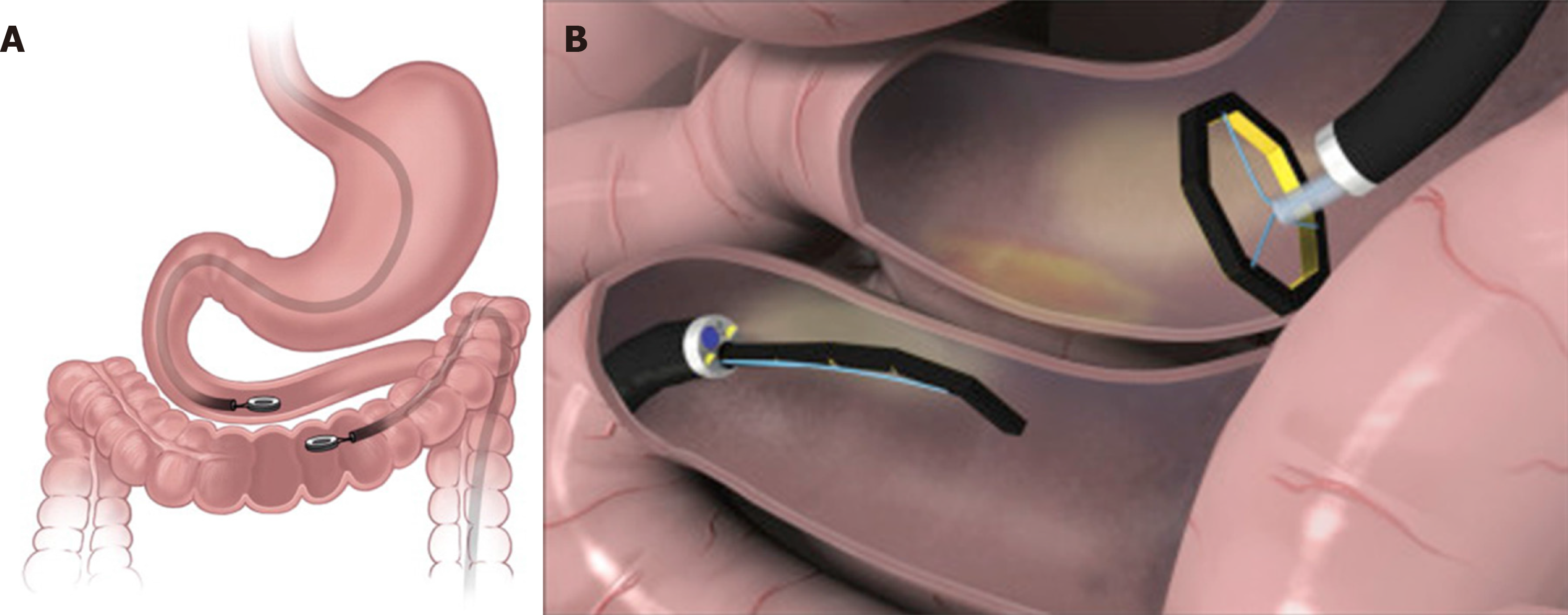
Magnetic compression anastomosis in the gastrointestinal tract has been assessed by multiple animal studies. According to its anatomical position, anastomosis can be divided into gastrojejunal anastomosis[20,21], gastrocolonic anastomosis[22], duodenocolonic anastomosis[22], jejunojejunal anastomosis[23], jejunoileal anastomosis[24], jejunocolonic anastomosis[22,25], and colorectal anastomosis[26]. Complete re-epithelization of the anastomosis rim can usually be achieved[22-25,27], but leaks may also occur before anastomosis maturation[23]. Endoscopic applications of these different types of anastomosis are for different clinical purposes, including treatment of gastric outlet obstruction[28,29], obesity and type 2 diabetes[30]. For gastric outlet obstruction, the distal magnet can be mounted on a catheter and advanced over a guidewire to the distal duodenum after balloon dilation of the stricture, and the proximal magnet can be inserted in the stomach along the introduction of the endoscope; the whole procedure should be performed under fluoroscopic guidance until the two magnets are coupled together. For obesity and type 2 diabetes, partial jejunal diversion can be selected so that the proximal magnet can be delivered to the proximal jejunum via enteroscopy, while the distal magnet can be delivered to the terminal ileum via colonoscopy simultaneously. Laparoscopy should also be performed to monitor or assist magnetic coupling. By using small disk or ring-shaped magnets, insertion of a stent may be needed to ensure the long-term patency of the anastomosis[20,28,29], but this may cause severe stent-related complications, such as bowel perforation[29]. Ryou et al[21,24,25,30] developed the through-the-scope smart self-assembling magnets in 2011, and these magnets provide a wide opening for the anastomosis (with a mean maximum diameter of 30-35 mm)[24,25]. Figure 3 shows two typical magnetic compression anastomosis systems for endoscopic gastrointestinal anastomosis.
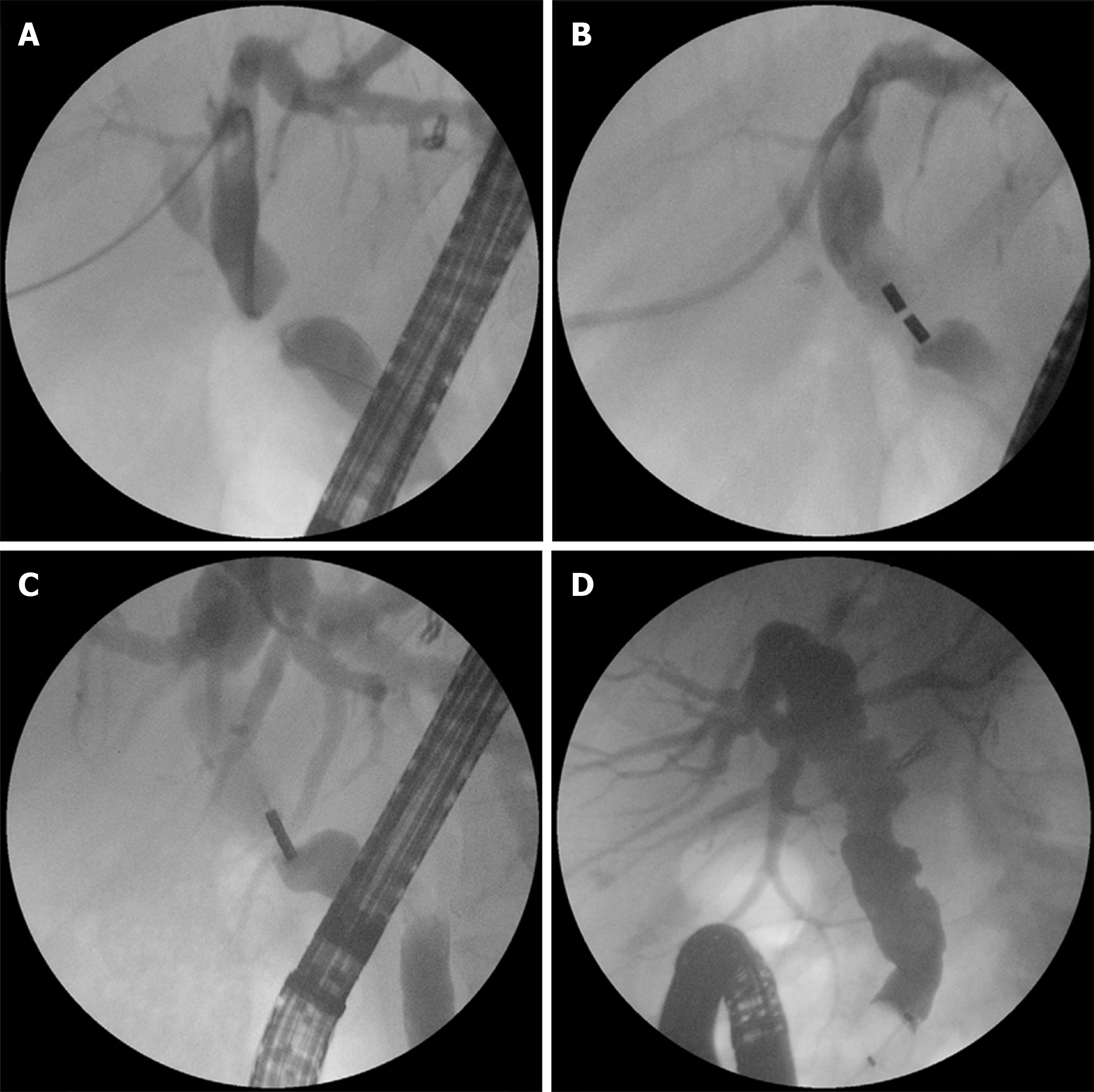
Magnetic compression anastomosis is usually used for severe biliary stenosis[31,32] and complete biliary obstruction[33-36] that are difficult to manage using conventional nonsurgical interventions. Based on the specific situation, either biliobiliary anastomosis[31,34,35] or bilioenteral anastomosis[33,37,38] can be conducted. The proximal magnet (mother magnet) is usually inserted through the percutaneous transhepatic biliary drainage (PTBD) tract, while the distal magnet (daughter magnet) can be delivered in three ways: endoscopically (Figure 4), through a second PTBD tract, or through a surgically formed fistula[39]. When inserting a magnet into the common bile duct (CBD), full sphincterotomy and/or sphincter balloon dilation is frequently required, and a metal stent may be inserted into the CBD to further facilitate magnet delivery[34,39,40]. After recanalization and magnets removal, biliary stents can also be placed to prevent restenosis[34,40]. In addition, an animal study showed the feasibility of a hinged metalloplastic anastomotic device for creation of a choledochoduo- denostomy above the papilla for large-diameter biliary drainage[38], in which all procedures were performed endoscopically, and sphincterotomy was not needed for system deployment.
Magnetic compression without anastomosis is mainly applied for improving gastroesophageal reflux[41-47] or fecal incontinence[48-50], but laparoscopic deployment of the Linx device [a system developed to augment the low esophageal sphincter (LES)] and surgical deployment of the Fenix device (a system developed to augment the anal sphincter) remain as the mainstream treatment (Figure 5). There are only two reports of endoscopic applications of magnets for preventing gastroesophageal reflux in vitro and/or in vivo in a porcine model[46,47]. In 2009, Bortolotti et al[46] deployed an endoesophageal magnetic device into the submucosal layer close to the LES to prevent gastroesophageal reflux. Although a high-pressure zone was achieved after insertion of the magnetic valve into the submucosal layer of the ex vivo porcine model (14.2 ± 1.27 mmHg vs 1.5 ± 0.26 mmHg, P < 0.001), mucosal breach could develop easily due to magnetic compression. After almost ten years, Dobashi et al[47] published their modified endoscopic method, that is, endoscopic magnet deployment in the subadventitial space to augment the LES. They performed the procedures in both in vitro and in vivo porcine models, in which the two subadventitial tunnels (one in the right side and one in the left side) were created with a biliary stone extraction balloon using the POEM technique, allowing subsequent endoscopic placement and fixation of the magnets[47]. Although this novel method by Dobashi et al[47] appears to be more reasonable than that by Bortolotti et al[46], erosion or fistula could also be developed. Fistula caused by magnetic compression after magnet ingestion has already been reported by many studies[3,51,52]. The anatomical structure of the human esophagus is different from that of porcine esophagus[53], with tight junctions to surrounding organs; thus, the feasibility of deploying magnets into the subadventitial space in the human body remains uncertain.
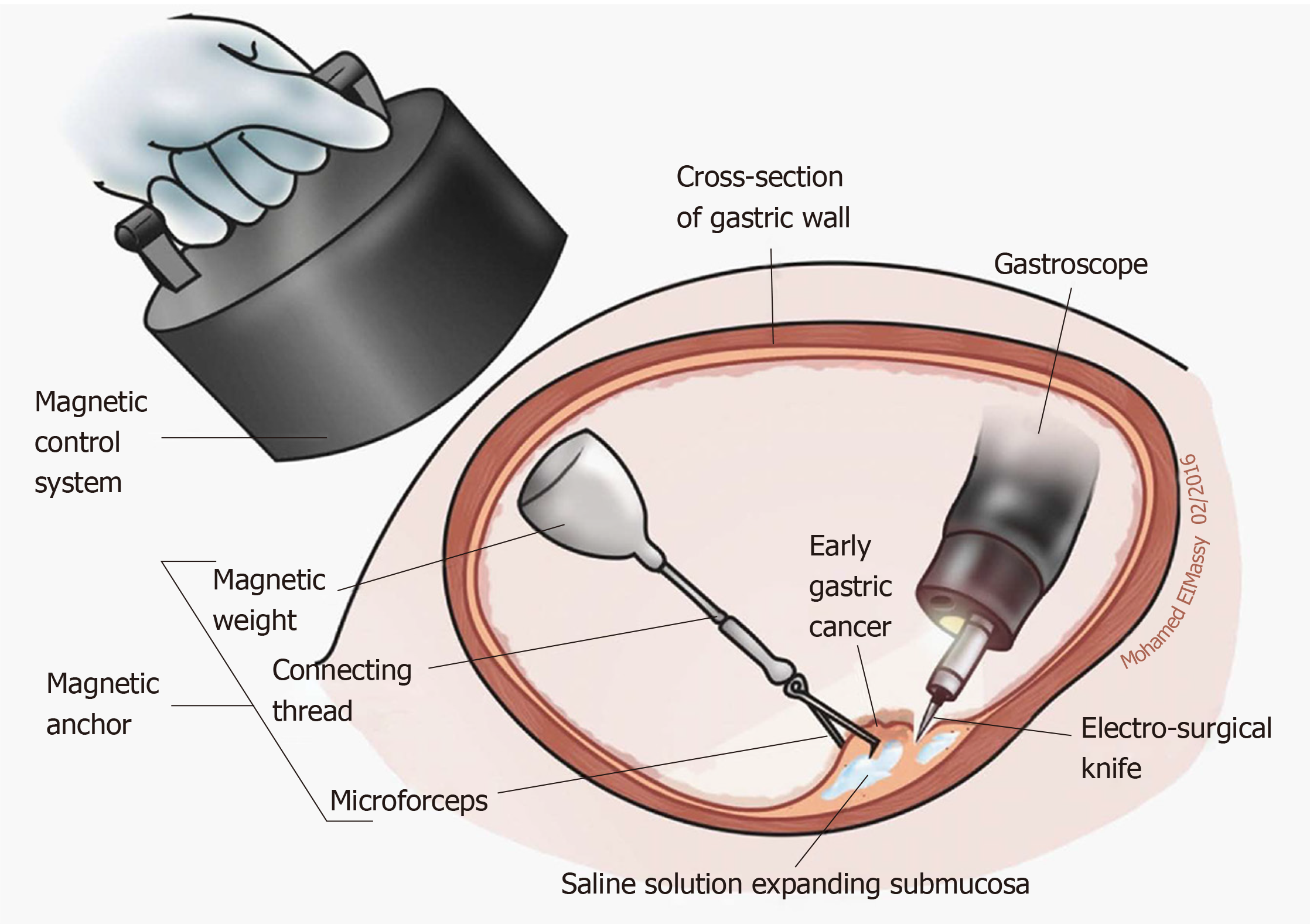
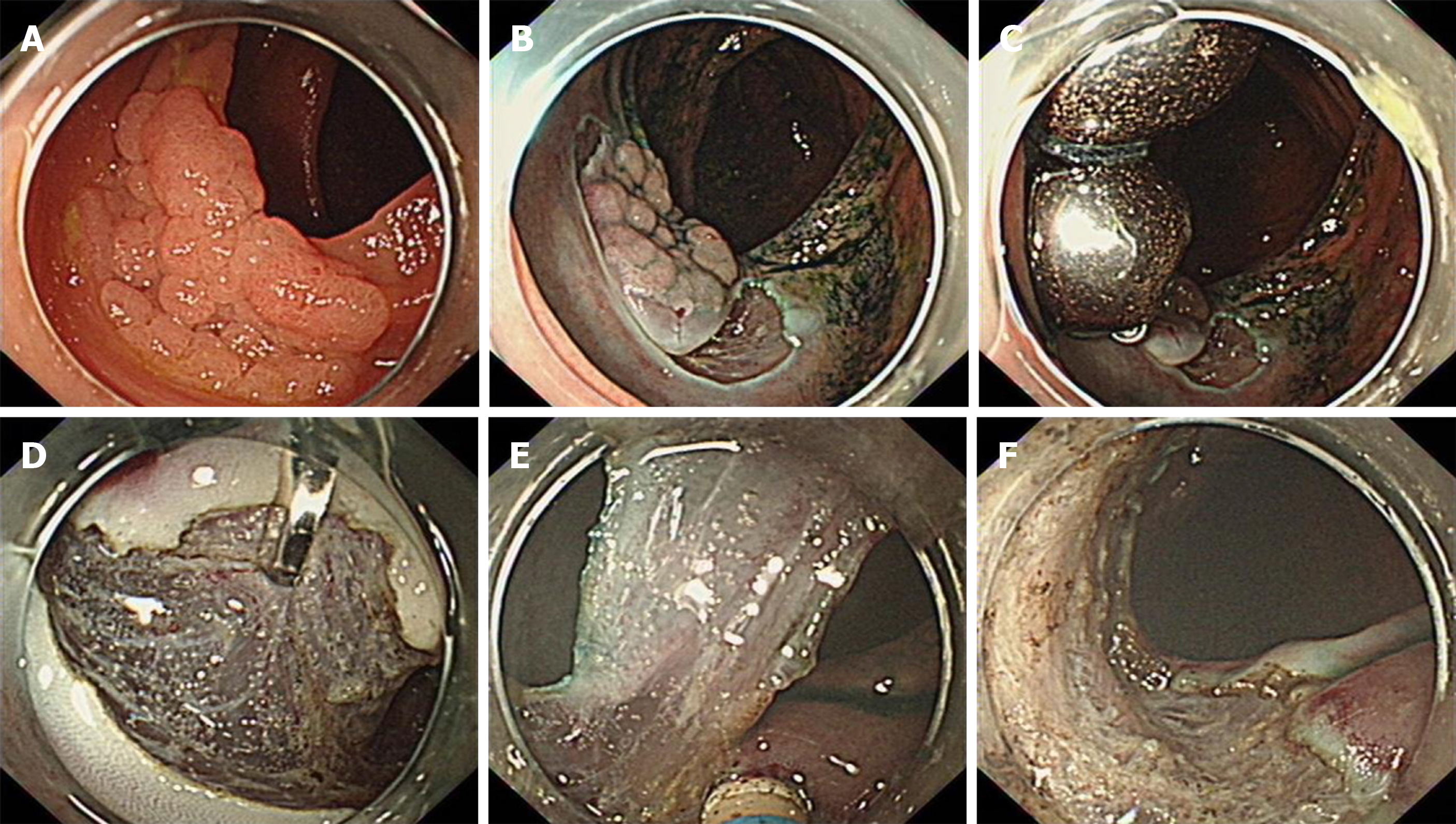
Currently, endoscopic submucosal dissection (ESD) is widely applied for en bloc resection of superficial gastrointestinal lesions[54], but the procedure can be technically difficult if the cutting line and submucosal layer cannot be adequately exposed. Tractions, like “the second hand” in surgery or laparoscopic operation, can facilitate safe and fast ESD by clearly exposing the field of vision[55]. As one of those traction methods, magnetic-anchor-guided ESD (MAG-ESD) is thought to be more attractive due to dynamic tissue retraction independent of the endoscope (Figure 6)[56]. In general, a small internal permanent magnet is applied to the edge of the lesion using an endoscopic clip, and a large external permanent magnet[57-60] or electromagnetic control system[61,62] is applied for retraction during MAG-ESD. The key point is that the external magnet can be moved to change the direction of traction as needed during the entire procedure. This technique has been reported for resecting both gastric[57,58,60-62] and colonic[59] lesions, helping to minimize technical difficulty and reduce the procedure time. Patient position changes can be replaced by using this technique, which is particularly valuable for obese patients under anesthesia. Despite its effectiveness, there are also some limitations for MAG-ESD[56], including the coupling strength of magnets, the distance between the internal and external magnets (abdominal wall thickness and air insufflation during endoscopy are two key influencing factors), and the high costs of large magnets. In addition, the strong external magnetic field can lead to detachment of the internal magnet from the lesion[60].
Based on the similar concept of MAG-ESD, Dobashi et al[63] developed an internal magnet traction device (MTD) with weaker magnetic force. Using the second MTD (deployed to the opposite wall) for traction of the first MTD (deployed to the edge of the lesion), endoscopists do not need to worry about tissue tearing. The strength and direction of traction can also be easily adjusted during the ESD procedure by increasing or decreasing distention of the lumen and by removing and repositioning the second MTD. Neither the thickness of the abdominal wall nor the location of the lesion influence the procedure. The study by Dobashi et al[63] used an in vitro porcine model and involved only gastric ESD; thus, its application in vivo and in other places with limited working space, such as the duodenum and colorectum, requires further investigation. In addition, as we reported previously[64-66], magnetic bead-assisted ESD (MBA-ESD) can also be used to facilitate difficult ESDs in the duodenum and colorectum. However, as we mentioned previously[64-66], the traction is mainly based on gravity. The magnetic force can play a role only when an additional magnetic bead is added to the same site to increase the weight and strength of the traction (Figure 7).
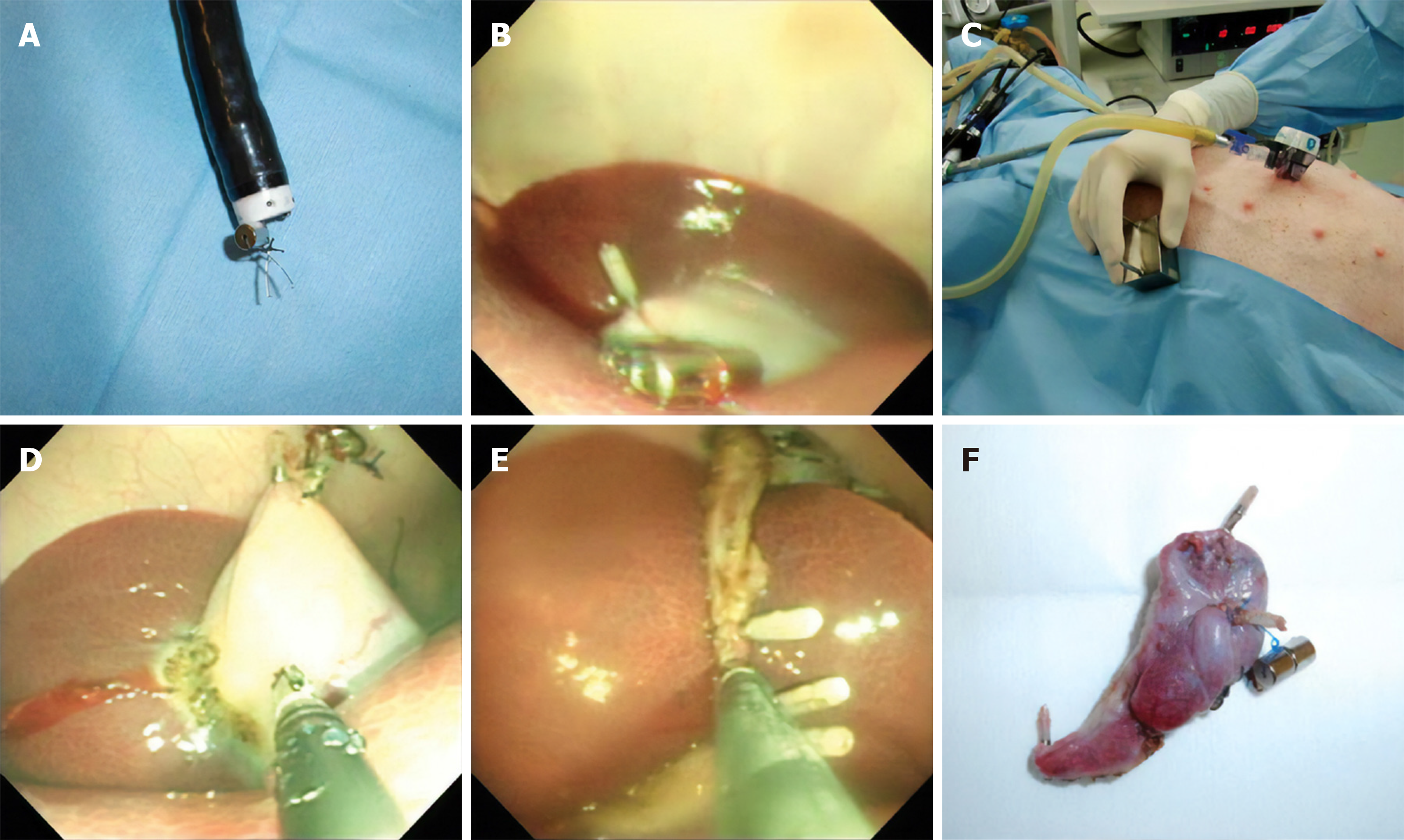
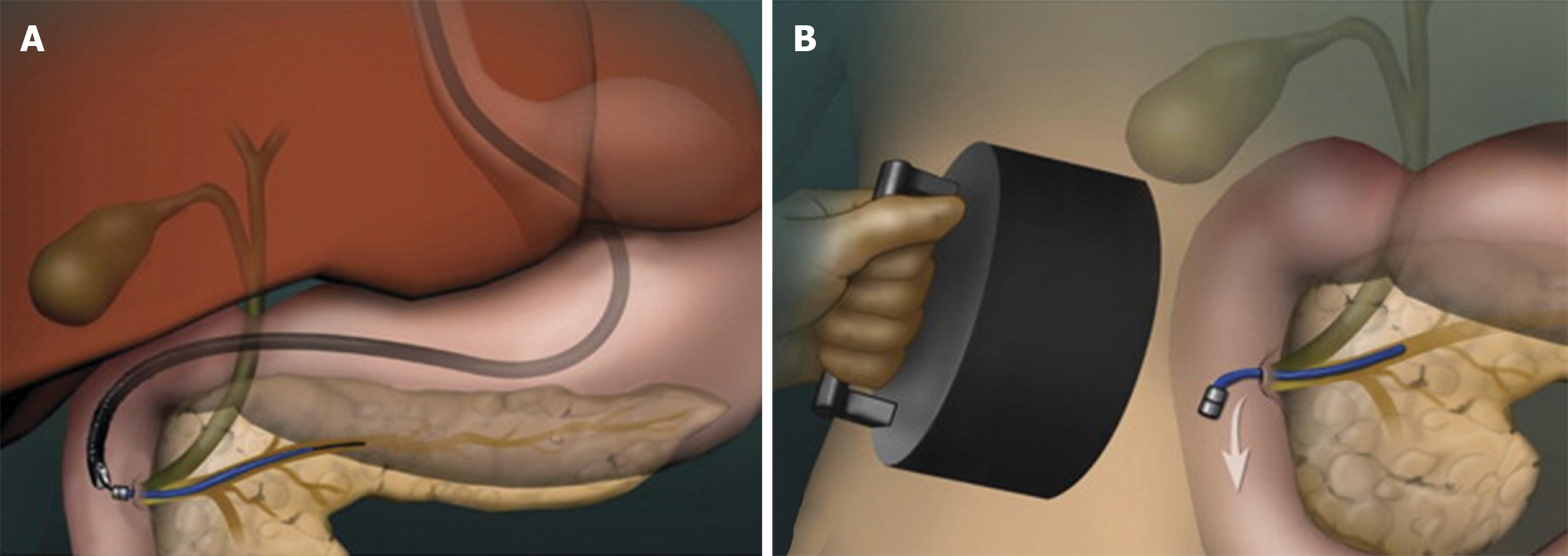
As the next surgical frontier with objective incision-free abdominal surgery, natural orifice transluminal endoscopic surgery (NOTES) has attracted increasing attention but has not been widely accepted because of technical difficulties[67]. The main limitation of NOTES is the loss of “the second hand” for tissue manipulation and visualization, where magnets may play a major role. According to reports involving in vitro and in vivo animal studies, NOTES that is facilitated with a magnetic anchor is feasible in different abdominal procedures such as cholecystectomy (Figure 8)[68-70] and sigmoidectomy[71,72]. Transgastric[71,72], Transcolonic[68], and transvaginal[69,70] approaches have been used for the access to the operation site. The internal magnet can be deployed to target organs or adjacent areas. However, there have been no reports of magnetic-anchor-assisted NOTES in humans thus far.
Other endoscopic applications include magnet-assisted foreign body and pancreaticobiliary stent removal, preoperative tumor marking, and magnetic-anchor-assisted direct percutaneous endoscopic jejunostomy.
Magnet-assisted foreign body removal may be regarded as the first application of magnet in the treatment of the gastrointestinal diseases. In the past[1,2], it was usually performed under fluoroscopic observation. A magnet inserted into a catheter was commonly used to remove ferromagnetic objects during the procedure. There is also a report on the blind removal of objects using such a device[73]. However, these methods were under indirect visualization and thus were always cumbersome and hazardous. With the widespread application of endoscopes, many other retrieval devices, such as graspers, forceps, snares, baskets, and nets, have been developed for endoscopic foreign body removal[74]. Despite their effectiveness, removal of foreign bodies in some cases remains difficult and time-consuming, especially when visualization of the objects is obscured[75,76], when the objects are too small or numerous[77], or when the objects are inaccessible[78]. Magnet-assisted foreign body removal performed under endoscopic observation is reported to be beneficial for extracting various objects, including coins[79,80], button batteries[81], impacted magnets[51], paperclips[75], needles[77], nails[76,78,82], pins[82] and safety pains[82]. Forceps[51], snares[75], Roth nets[76,77], and loop baskets[79] are commonly used for magnet insertion. Limited data suggest that the use of magnets for foreign body removal helps to shorten the operation time, avoid additional injuries, and ensure a higher success rate.
An internal magnet with string attached can also be clipped to a tumor or its periphery using an endoscopic clip at preoperative endoscopy, allowing fast and precise orientation of the tumor using ferromagnetic instruments during laparoscopic surgery. Ohdaira et al[83] selected a 4-mm cylindrical magnet and applied the magnet-string-clip system to gastric mucosa (20 mm away from the tumor periphery) in 15 patients with early gastric cancer; the tumor site was detected during laparoscopic gastrectomy in all cases. Warnick et al[84] reported the use of a ring-shaped magnet (mounted on the tip of the scope by a cap), but tumor localization failed in 1 of 28 patients with small colorectal tumors (23 in the colon and 5 in the rectum) owing to system migration.
An external magnet can be applied to remove endoscopically placed ferromagnetic pancreaticobiliary stents[85,86], which obviates the requirement for a second endoscopy for stent removal (Figure 9). This application involved only animal studies, but there are already reports of the use of a biodegradable stent[87] or spontaneous dislodgement spiral stent[88] in humans, in which additional endoscopy for stent removal is also not needed.
Applications of an internal magnet and an external magnet (i.e., magnetic anchors) also help to fix the jejunal wall to the abdominal wall, facilitating direct percutaneous endoscopic jejunostomy (D-PEJ)[89]. The D-PEJ is similar to conventional percutaneous endoscopic gastrostomy, except for the use of double-balloon enteroscopy (for access to the jejunum, insertion of an internal magnet, and placement of a tube) and magnetic anchors.
Magnetic nanoparticles are a class of nanoparticles that can be manipulated by an external magnetic field and functionalized with bioactive agents; thus, they can be used for hyperthermia cancer therapy, guided drug delivery, and other applications [90,91]. Currently, endoscopic application of nanotechnology and magnetic nanoparticles is in its infancy. Only a few in vitro and in vivo animal studies have primarily investigated their roles in the treatment of esophageal[92], liver[93], and pancreatic[93] tumors by local or systemic injection.
Endoscopic applications of magnetic devices represent a further advancement in the field of minimally invasive intervention. Their use expands the indications of therapeutic endoscopy and makes it easier and safer to perform difficult procedures. Notably, many novel techniques have only been performed in in vitro and in vivo animal studies, and thus, applications in humans require further detailed evaluations to ensure their safety. For those techniques that have been initially applied in clinical practice, effective measures should also be taken to detect, treat, or even prevent the well-recognized complications. In addition, specific commercially magnetic devices need to be developed in this promising filed.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: de Moura DTH, Gavriilidis P S-Editor: Wang JL L-Editor: Ma JY E-Editor: Li X
| 1. | Equen M. A New Magnet for Foreign Bodies in the Food and Air Passages. JAMA. 1945;127:87-89 [DOI 10.1001/jama.1945.92860020001009]. |
| 2. | Equen M, Roach G, Brown R, Bennett T. Magnetic removal of foreign bodies from the esophagus, stomach and duodenum. AMA Arch Otolaryngol. 1957;66:698-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Centers for Disease Control and Prevention (CDC). Gastrointestinal injuries from magnet ingestion in children--United States, 2003-2006. MMWR Morb Mortal Wkly Rep. 2006;55:1296-1300. [PubMed] |
| 4. | Kubota Y, Tokiwa K, Tanaka S, Iwai N. Intestinal obstruction in an infant due to magnet ingestion. Eur J Pediatr Surg. 1995;5:119-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Diaz R, Davalos G, Welsh LK, Portenier D, Guerron AD. Use of magnets in gastrointestinal surgery. Surg Endosc. 2019;33:1721-1730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Keller J, Fibbe C, Volke F, Gerber J, Mosse AC, Reimann-Zawadzki M, Rabinovitz E, Layer P, Swain P. Remote magnetic control of a wireless capsule endoscope in the esophagus is safe and feasible: results of a randomized, clinical trial in healthy volunteers. Gastrointest Endosc. 2010;72:941-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 54] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Dechêne A, Jochum C, Bechmann LP, Windeck S, Gerken G, Canbay A, Zöpf T. Magnetic endoscopic imaging saves abdominal compression and patient pain in routine colonoscopies. J Dig Dis. 2011;12:364-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Zaritzky M, Ben R, Zylberg GI, Yampolsky B. Magnetic compression anastomosis as a nonsurgical treatment for esophageal atresia. Pediatr Radiol. 2009;39:945-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Dorman RM, Vali K, Harmon CM, Zaritzky M, Bass KD. Repair of esophageal atresia with proximal fistula using endoscopic magnetic compression anastomosis (magnamosis) after staged lengthening. Pediatr Surg Int. 2016;32:525-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Ellebaek MBB, Qvist N, Rasmussen L. Magnetic Compression Anastomosis in Long-Gap Esophageal Atresia Gross Type A: A Case Report. European J Pediatr Surg Rep. 2018;6:e37-e39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Bouchard S, Huberty V, Blero D, Devière J. Magnetic compression for treatment of large oesophageal diverticula: a new endoscopic approach for a risky surgical disease? Gut. 2015;64:1678-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Disibeyaz S, Saygili F, Oztas E, Coskun O. Endoscopic septotomy of a magnet-induced neoseptum in a large mid-esophageal diverticulum. Endoscopy. 2016;48 Suppl 1:E244-E245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Ye L, Zeng H, Wang S, Jiang J, Tang H, Li C, Hu B. Magnet-assisted diverticuloplasty for treatment of Zenker's diverticulum. Endoscopy. 2018;50:E170-E171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Hendren WH, Hale JR. Electromagnetic bougienage to lengthen esophageal segments in congenital esophageal atresia. N Engl J Med. 1975;293:428-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 49] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Ishaq S, Hassan C, Antonello A, Tanner K, Bellisario C, Battaglia G, Anderloni A, Correale L, Sharma P, Baron TH, Repici A. Flexible endoscopic treatment for Zenker's diverticulum: a systematic review and meta-analysis. Gastrointest Endosc. 2016;83:1076-1089.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 119] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 16. | Bak YT, Kim HJ, Jo NY, Yeon JE, Park JJ, Kim JS, Byun KS, Choi YH, Lee CH. Endoscopic "clip and cut" diverticulotomy for a giant midesophageal diverticulum. Gastrointest Endosc. 2003;57:777-779. [PubMed] |
| 17. | Mou Y, Zeng H, Wang Q, Yi H, Liu W, Wen D, Tang C, Hu B. Giant mid-esophageal diverticula successfully treated by per-oral endoscopic myotomy. Surg Endosc. 2016;30:335-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Li QL, Chen WF, Zhang XC, Cai MY, Zhang YQ, Hu JW, He MJ, Yao LQ, Zhou PH, Xu MD. Submucosal Tunneling Endoscopic Septum Division: A Novel Technique for Treating Zenker's Diverticulum. Gastroenterology. 2016;151:1071-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 19. | Yang J, Zeng X, Yuan X, Chang K, Sanaei O, Fayad L, Kumbhari V, Singh V, Kalloo AN, Hu B, Khashab MA. An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: the first multicenter D-POEM experience. Endoscopy. 2019;51:346-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 20. | Cope C, Ginsberg GG. Long-term patency of experimental magnetic compression gastroenteric anastomoses achieved with covered stents. Gastrointest Endosc. 2001;53:780-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Ryou M, Cantillon-Murphy P, Azagury D, Shaikh SN, Ha G, Greenwalt I, Ryan MB, Lang JH, Thompson CC. Smart Self-Assembling MagnetS for ENdoscopy (SAMSEN) for transoral endoscopic creation of immediate gastrojejunostomy (with video). Gastrointest Endosc. 2011;73:353-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 22. | Gonzales KD, Douglas G, Pichakron KO, Kwiat DA, Gallardo SG, Encinas JL, Hirose S, Harrison MR. Magnamosis III: delivery of a magnetic compression anastomosis device using minimally invasive endoscopic techniques. J Pediatr Surg. 2012;47:1291-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 23. | Pichakron KO, Jelin EB, Hirose S, Curran PF, Jamshidi R, Stephenson JT, Fechter R, Strange M, Harrison MR. Magnamosis II: Magnetic compression anastomosis for minimally invasive gastrojejunostomy and jejunojejunostomy. J Am Coll Surg. 2011;212:42-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 24. | Ryou M, Aihara H, Thompson CC. Minimally invasive entero-enteral dual-path bypass using self-assembling magnets. Surg Endosc. 2016;30:4533-4538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 25. | Ryou M, Agoston AT, Thompson CC. Endoscopic intestinal bypass creation by using self-assembling magnets in a porcine model. Gastrointest Endosc. 2016;83:821-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Wall J, Diana M, Leroy J, Deruijter V, Gonzales KD, Lindner V, Harrison M, Marescaux J. MAGNAMOSIS IV: magnetic compression anastomosis for minimally invasive colorectal surgery. Endoscopy. 2013;45:643-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 27. | Jamshidi R, Stephenson JT, Clay JG, Pichakron KO, Harrison MR. Magnamosis: magnetic compression anastomosis with comparison to suture and staple techniques. J Pediatr Surg. 2009;44:222-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 93] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 28. | Chopita N, Vaillaverde A, Cope C, Bernedo A, Martinez H, Landoni N, Jmelnitzky A, Burgos H. Endoscopic gastroenteric anastomosis using magnets. Endoscopy. 2005;37:313-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 29. | van Hooft JE, Vleggaar FP, Le Moine O, Bizzotto A, Voermans RP, Costamagna G, Devière J, Siersema PD, Fockens P. Endoscopic magnetic gastroenteric anastomosis for palliation of malignant gastric outlet obstruction: a prospective multicenter study. Gastrointest Endosc. 2010;72:530-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 30. | Machytka E, Bužga M, Zonca P, Lautz DB, Ryou M, Simonson DC, Thompson CC. Partial jejunal diversion using an incisionless magnetic anastomosis system: 1-year interim results in patients with obesity and diabetes. Gastrointest Endosc. 2017;86:904-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 94] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 31. | Mimuro A, Tsuchida A, Yamanouchi E, Itoi T, Ozawa T, Ikeda T, Nakamura R, Koyanagi Y, Nakamura K. A novel technique of magnetic compression anastomosis for severe biliary stenosis. Gastrointest Endosc. 2003;58:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 32. | Itoi T, Yamanouchi E, Ikeda T, Sofuni A, Kurihara T, Tsuchiya T, Tsuchida A, Kasuya K, Moriyasu F. Magnetic compression anastomosis: a novel technique for canalization of severe hilar bile duct strictures. Endoscopy. 2005;37:1248-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Takao S, Matsuo Y, Shinchi H, Nakajima S, Aikou T, Iseji T, Yamanouchi E. Magnetic compression anastomosis for benign obstruction of the common bile duct. Endoscopy. 2001;33:988-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 34. | Parlak E, Koksal AS, Kucukay F, Eminler AT, Toka B, Uslan MI. A novel technique for the endoscopic treatment of complete biliary anastomosis obstructions after liver transplantation: through-the-scope magnetic compression anastomosis. Gastrointest Endosc. 2017;85:841-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 35. | Nakaseko Y, Shiba H, Yamanouchi E, Takano Y, Sakamoto T, Imazu H, Ashida H, Yanaga K. Successful Treatment of Stricture of Duct-to-Duct Biliary Anastomosis After Living-Donor Liver Transplantation of the Left Lobe: A Case Report. Transplant Proc. 2017;49:1644-1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | Ersoz G, Tekin F, Bozkaya H, Parildar M, Turan I, Karasu Z, Ozutemiz O, Tekesin O. Magnetic compression anastomosis for patients with a disconnected bile duct after living-donor related liver transplantation: a pilot study. Endoscopy. 2016;48:652-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 37. | Saito R, Tahara H, Shimizu S, Ohira M, Ide K, Ishiyama K, Kobayashi T, Ohdan H. Biliary-duodenal anastomosis using magnetic compression following massive resection of small intestine due to strangulated ileus after living donor liver transplantation: a case report. Surg Case Rep. 2017;3:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 38. | Jamidar P, Cadeddu M, Mosse A, Swain CP. A hinged metalloplastic anastomotic device: a novel method for choledochoduodenostomy. Gastrointest Endosc. 2009;69:1333-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Jang SI, Lee KH, Yoon HJ, Lee DK. Treatment of completely obstructed benign biliary strictures with magnetic compression anastomosis: follow-up results after recanalization. Gastrointest Endosc. 2017;85:1057-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 40. | Jang SI, Choi J, Lee DK. Magnetic compression anastomosis for treatment of benign biliary stricture. Dig Endosc. 2015;27:239-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 41. | Ganz RA, Gostout CJ, Grudem J, Swanson W, Berg T, DeMeester TR. Use of a magnetic sphincter for the treatment of GERD: a feasibility study. Gastrointest Endosc. 2008;67:287-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 76] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 42. | Bonavina L, Saino GI, Bona D, Lipham J, Ganz RA, Dunn D, DeMeester T. Magnetic augmentation of the lower esophageal sphincter: results of a feasibility clinical trial. J Gastrointest Surg. 2008;12:2133-2140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 106] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 43. | Bonavina L, Saino G, Lipham JC, Demeester TR. LINX(®) Reflux Management System in chronic gastroesophageal reflux: a novel effective technology for restoring the natural barrier to reflux. Therap Adv Gastroenterol. 2013;6:261-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 44. | Bonavina L, DeMeester T, Fockens P, Dunn D, Saino G, Bona D, Lipham J, Bemelman W, Ganz RA. Laparoscopic sphincter augmentation device eliminates reflux symptoms and normalizes esophageal acid exposure: one- and 2-year results of a feasibility trial. Ann Surg. 2010;252:857-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 126] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 45. | Ganz RA, Peters JH, Horgan S, Bemelman WA, Dunst CM, Edmundowicz SA, Lipham JC, Luketich JD, Melvin WS, Oelschlager BK, Schlack-Haerer SC, Smith CD, Smith CC, Dunn D, Taiganides PA. Esophageal sphincter device for gastroesophageal reflux disease. N Engl J Med. 2013;368:719-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 200] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 46. | Bortolotti M, Grandis A, Mazzero G. A novel endoesophageal magnetic device to prevent gastroesophageal reflux. Surg Endosc. 2009;23:885-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 47. | Dobashi A, Wu SW, Deters JL, Miller CA, Knipschield MA, Cameron GP, Lu L, Rajan E, Gostout CJ. Endoscopic magnet placement into subadventitial tunnels for augmenting the lower esophageal sphincter using submucosal endoscopy: ex vivo and in vivo study in a porcine model (with video). Gastrointest Endosc. 2019;89:422-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 48. | Lehur PA, McNevin S, Buntzen S, Mellgren AF, Laurberg S, Madoff RD. Magnetic anal sphincter augmentation for the treatment of fecal incontinence: a preliminary report from a feasibility study. Dis Colon Rectum. 2010;53:1604-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 49. | Pakravan F, Helmes C. Magnetic anal sphincter augmentation in patients with severe fecal incontinence. Dis Colon Rectum. 2015;58:109-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 50. | Sugrue J, Lehur PA, Madoff RD, McNevin S, Buntzen S, Laurberg S, Mellgren A. Long-term Experience of Magnetic Anal Sphincter Augmentation in Patients With Fecal Incontinence. Dis Colon Rectum. 2017;60:87-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 51. | Ye L, Yang Z, Du J, Zeng Q, Yuan X, Zhang Y, Hu B. Endoscopic removal of two magnets impacted in the lower esophagus and gastric fundus. Endoscopy. 2018;50:E124-E125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 52. | Sola R, Rosenfeld EH, Yu YR, St Peter SD, Shah SR. Magnet foreign body ingestion: rare occurrence but big consequences. J Pediatr Surg. 2018;53:1815-1819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 53. | Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Yoshida A, Hosoya T, Maselli R, Kudo SE. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag. 2012;8:329-342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 87] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 54. | Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 817] [Cited by in RCA: 925] [Article Influence: 92.5] [Reference Citation Analysis (0)] |
| 55. | Tsuji K, Yoshida N, Nakanishi H, Takemura K, Yamada S, Doyama H. Recent traction methods for endoscopic submucosal dissection. World J Gastroenterol. 2016;22:5917-5926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 50] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 56. | Mortagy M, Mehta N, Parsi MA, Abe S, Stevens T, Vargo JJ, Saito Y, Bhatt A. Magnetic anchor guidance for endoscopic submucosal dissection and other endoscopic procedures. World J Gastroenterol. 2017;23:2883-2890. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 57. | Aihara H, Ryou M, Kumar N, Ryan MB, Thompson CC. A novel magnetic countertraction device for endoscopic submucosal dissection significantly reduces procedure time and minimizes technical difficulty. Endoscopy. 2014;46:422-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 58. | Matsuzaki I, Miyahara R, Hirooka Y, Funasaka K, Furukawa K, Ohno E, Nakamura M, Kawashima H, Maeda O, Watanabe O, Ando T, Kobayashi M, Goto H. Simplified magnetic anchor-guided endoscopic submucosal dissection in dogs (with videos). Gastrointest Endosc. 2014;80:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 59. | Matsuzaki I, Isobe S, Hirose K, Marukawa T, Esaki M. Magnetic anchor-guided endoscopic submucosal dissection for colonic tumor. VideoGIE. 2017;2:74-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 60. | Matsuzaki I, Hattori M, Hirose K, Esaki M, Yoshikawa M, Yokoi T, Kobayashi M, Miyahara R, Hirooka Y, Goto H. Magnetic anchor-guided endoscopic submucosal dissection for gastric lesions (with video). Gastrointest Endosc. 2018;87:1576-1580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 61. | Kobayashi T, Gotohda T, Tamakawa K, Ueda H, Kakizoe T. Magnetic anchor for more effective endoscopic mucosal resection. Jpn J Clin Oncol. 2004;34:118-123. [PubMed] |
| 62. | Gotoda T, Oda I, Tamakawa K, Ueda H, Kobayashi T, Kakizoe T. Prospective clinical trial of magnetic-anchor-guided endoscopic submucosal dissection for large early gastric cancer (with videos). Gastrointest Endosc. 2009;69:10-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 117] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 63. | Dobashi A, Storm AC, Wong Kee Song LM, Gostout CJ, Deters JL, Miller CA, Knipschield MA, Rajan E. Efficacy and safety of an internal magnet traction device for endoscopic submucosal dissection: ex vivo study in a porcine model (with video). Surg Endosc. 2019;33:663-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 64. | Bethge J, Ye L, Ellrichmann M, Khan N, Feng Z, Schreiber S, Hu B. Advanced endoscopic submucosal dissection with magnetic bead-assisted traction based on gravity for a flat colorectal neoplasm with severe fibrosis. Endoscopy. 2018;50:824-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 65. | Guo LJ, Ye L, Huang ZY, Yin X, Hu B. Magnetic beads-assisted endoscopic submucosal dissection of duodenal heterotopic gastric mucosa with fibrosis. Endoscopy. 2019;51:E113-E115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 66. | Ye L, Yuan X, Pang M, Bethge J, Ellrichmann M, Du J, Zeng X, Tang C, Schreiber S, Hu B. Magnetic bead-assisted endoscopic submucosal dissection: a gravity-based traction method for treating large superficial colorectal tumors. Surg Endosc. 2019;33:2034-2041. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 67. | Dunkin BJ. Natural orifice transluminal endoscopic surgery: Educational challenge. World J Gastrointest Surg. 2010;2:224-230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 68. | Ryou M, Thompson CC. Magnetic retraction in natural-orifice transluminal endoscopic surgery (NOTES): addressing the problem of traction and countertraction. Endoscopy. 2009;41:143-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 69. | Scott DJ, Tang SJ, Fernandez R, Bergs R, Goova MT, Zeltser I, Kehdy FJ, Cadeddu JA. Completely transvaginal NOTES cholecystectomy using magnetically anchored instruments. Surg Endosc. 2007;21:2308-2316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 141] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 70. | Cho YB, Park CM, Chun HK, Yi LJ, Park JH, Yun SH, Kim HC, Lee WY. Transvaginal endoscopic cholecystectomy using a simple magnetic traction system. Minim Invasive Ther Allied Technol. 2011;20:174-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 71. | Cho YB, Park JH, Chun HK, Park CM, Kim HC, Yun SH, Lee WY. Multimedia article. Natural orifice transluminal endoscopic surgery applied to sigmoidectomy in survival animal models: using paired magnetic intra-luminal device. Surg Endosc. 2011;25:1319-1324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 72. | Leroy J, Perretta S, Diana M, Wall J, Lindner V, Harrison M, Marescaux J. An original endoluminal magnetic anastomotic device allowing pure NOTES transgastric and transrectal sigmoidectomy in a porcine model: proof of concept. Surg Innov. 2012;19:109-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 73. | McDermott VG, Taylor T, Wyatt JP, MacKenzie S, Hendry GM. Orogastric magnet removal of ingested disc batteries. J Pediatr Surg. 1995;30:29-32. [PubMed] |
| 74. | Birk M, Bauerfeind P, Deprez PH, Häfner M, Hartmann D, Hassan C, Hucl T, Lesur G, Aabakken L, Meining A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 382] [Article Influence: 42.4] [Reference Citation Analysis (0)] |
| 75. | Coash M, Wu GY. Endoscopic removal of a long sharp metallic foreign body by a snared magnet: an attractive solution. J Dig Dis. 2012;13:239-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 76. | Kwong WT, Chang JT. Endoscopic retrieval of ingested nails using a refrigerator magnet. Clin Gastroenterol Hepatol. 2013;11:A24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 77. | Aslinia FM, Flasar MH. Endoscopic ferromagnetic object retrieval by use of a simple magnet (with video). Gastrointest Endosc. 2012;76:667-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 78. | Nijhawan S, Kumpawat S, Ashdhir P, Behl N, Jha A, Rai RR. Impacted nail in duodenum: endoscopic removal with a novel magnetic foreign body retriever. Endoscopy. 2009;41 Suppl 2:E62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 79. | Nijhawan S, Rastogi M, Tandon M, Mallikarjun P, Singh V, Mathur A, Rai RR. Magnetic loop basket: a "two-in-one" instrument. Endoscopy. 2006;38:723-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 80. | Nijhawan S, Joshi A, Shende A, Agarwal N, Kumar D, Mathur A, Rai R. Endoscopy-assisted ferromagnetic foreign-body removal with a novel magnetic instrument. Endoscopy. 2004;36:1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 81. | Soong WJ, Yuh YS. Ingested button battery retrieved by a modified magnet endoscope. J Chin Med Assoc. 2007;70:132-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 82. | Nijhawan S, Singh V, Mallikaarjun P, Jain P, Tandon M, Rastogi M, Mathur A, Rai RR. Endoscopic removal of sharp metallic foreign bodies. Endoscopy. 2007;39 Suppl 1:E331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 83. | Ohdaira T, Nagai H. Intraoperative localization of early-stage upper gastrointestinal tumors using a magnetic marking clip-detecting system. Surg Endosc. 2007;21:810-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 84. | Warnick P, Chopra SS, Raubach M, Kneif S, Hünerbein M. Intraoperative localization of occult colorectal tumors during laparoscopic surgery by magnetic ring markers—a pilot study. Int J Colorectal Dis. 2012;28:795-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 85. | Cantillon-Murphy P, Ryou M, Shaikh SN, Azagury D, Ryan M, Thompson CC, Lang JH. A magnetic retrieval system for stents in the pancreaticobiliary tree. IEEE Trans Biomed Eng. 2010;57:2018-2025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 86. | Ryou M, Cantillon-Murphy P, Shaikh SN, Azagury D, Ryan MB, Lang JH, Thompson CC. Magnetic pancreaticobiliary stents and retrieval system: obviating the need for repeat endoscopy (with video). Gastrointest Endosc. 2012;75:888-892.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 87. | Siiki A, Rinta-Kiikka I, Sand J, Laukkarinen J. A pilot study of endoscopically inserted biodegradable biliary stents in the treatment of benign biliary strictures and cystic duct leaks. Gastrointest Endosc. 2018;87:1132-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 88. | Ye L, Hu B. Sa1366 Endoscopic placement of a plastic spiral stent for short-term biliary drainage in patients with cholelithiasis. Gastrointest Endosc. 2018;87:Ab232-Ab232. [DOI] [Full Text] |
| 89. | Yano T, Yamamoto H, Sunada K, Miura Y, Taguchi H, Arashiro M, Yoshizawa M, Hayashi Y, Miyata T, Tanaka H, Kobayashi E, Sugano K. New technique for direct percutaneous endoscopic jejunostomy using double-balloon endoscopy and magnetic anchors in a porcine model. Dig Endosc. 2011;23:206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 90. | Shubayev VI, Pisanic TR 2nd, Jin S. Magnetic nanoparticles for theragnostics. Adv Drug Deliv Rev. 2009;61:467-477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 843] [Cited by in RCA: 612] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 91. | Colombo M, Carregal-Romero S, Casula MF, Gutiérrez L, Morales MP, Böhm IB, Heverhagen JT, Prosperi D, Parak WJ. Biological applications of magnetic nanoparticles. Chem Soc Rev. 2012;41:4306-4334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 930] [Cited by in RCA: 727] [Article Influence: 55.9] [Reference Citation Analysis (0)] |
| 92. | Roeth AA, Slabu I, Baumann M, Alizai PH, Schmeding M, Guentherodt G, Schmitz-Rode T, Neumann UP. Establishment of a biophysical model to optimize endoscopic targeting of magnetic nanoparticles for cancer treatment. Int J Nanomedicine. 2017;12:5933-5940. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 93. | Ungureanu BS, Pirici D, Margaritescu C, Gheonea IA, Trincu FN, Fifere A, Saftoiu A. Endoscopic ultrasound guided injection of iron oxide magnetic nanoparticles for liver and pancreas: a feasibility study in pigs. Med Ultrason. 2016;18:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |