Published online Dec 14, 2020. doi: 10.3748/wjg.v26.i46.7425
Peer-review started: July 28, 2020
First decision: September 30, 2020
Revised: October 11, 2020
Accepted: November 4, 2020
Article in press: November 4, 2020
Published online: December 14, 2020
Processing time: 138 Days and 23 Hours
Joint, skin, oral cavity, and eye lesions are the most common extraintestinal manifestations of ulcerative colitis that can occur before or after its onset. The cases of ulcerative colitis with dermatomyositis (DM) are rare. In this study, we report a rare case of ulcerative colitis with DM that was effectively treated with infliximab.
The patient was a 57-year-old female with a 2-year history of DM. The patient was admitted to hospital with abdominal pain, diarrhea, and blood in stool lasting for more than 2 mo. Colonoscopy revealed multiple erosions and ulcers in the entire colon and rectum. Pathological sections showed chronic inflammatory cell infiltration, especially neutrophil infiltration, in the colonic mucosa; therefore, the patient was diagnosed with ulcerative colitis. Preparations of 5-aminosalicylic acid was added to her treatment based on the original treatment for DM, but its effect was unsatisfactory. The patient’s discomfort was relieved after infliximab treatment.
Infliximab can improve DM in the treatment of ulcerative colitis. Specialists need to raise awareness about patients with inflammatory bowel disease who have rare extraintestinal manifestations.
Core Tip: Few cases of ulcerative colitis have dermatomyositis (DM) as complication. DM may be a less frequent extraintestinal manifestation of ulcerative colitis. Infliximab is effective in the treatment of ulcerative colitis in patients with autoimmune disease or poor hormone response.
- Citation: Huang BB, Han LC, Liu GF, Lv XD, Gu GL, Li SQ, Chen L, Wang HQ, Zhan LL, Lv XP. Infliximab is effective in the treatment of ulcerative colitis with dermatomyositis: A case report. World J Gastroenterol 2020; 26(46): 7425-7435
- URL: https://www.wjgnet.com/1007-9327/full/v26/i46/7425.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i46.7425
Ulcerative colitis (UC) is a type of inflammatory bowel disease (IBD) characterized by abdominal pain, diarrhea, and bloody mucus defecation and usually occurs in the rectum and colonic mucosa[1]. UC, as a systemic inflammatory disease, can have a variety of extraintestinal manifestations (EIMs) with an incidence of more than 20% in some countries[2,3]. The EIMs of IBD have two types. The first type is associated with the severity of IBD and includes oral aphthous ulcers and erythema nodosum. The second type, which includes ankylosing spondylitis and uveitis, is independent from the intestinal inflammation of IBD and is associated with autoimmune diseases[4]. IBD also has rare myopathy-type EIMs, such as orbital myositis[5]. Only a few cases of IBD with dermatomyositis (DM) are reported on PubMed[6,7].
DM is an inflammatory disease of the skin and muscle that is characterized by the presence of specific antibodies and elevated creatine kinase[8]. Muscle biopsy reveals atrophy of the muscle tract[9]. This paper reports a case of UC with DM treated by infliximab and reviews its pathogenesis and treatment. We hope this report will provide recommendations for the treatment of IBD with rare EIMs.
The patient was a 57-year-old woman whose chief complaint was abdominal pain, diarrhea, and bloody mucus stool for more than 2 mo.
Diarrhea with bloody mucus stool occurred suddenly more than ten times a day since early August 2018. The patient also had periumbilical pain, which can be relieved after defecation. She did not have fever, cough, chest tightness, or other discomfort.
The patient was hospitalized in early June 2016 for eyelid edema, limb weakness, and swallowing difficulties. She had a series of typical clinical symptoms of DM, such as Gottron’s papules in the extensor surfaces of the metacarpophalangeal joints, V-neck sign, facial erythema, and periorbital edema (Figure 1). Electromyography showed myogenic damage. Muscle biopsy pathology (Figure 2) and magnetic resonance imaging (Figure 3) supported myositis. The patient was initially given prednisone [50 mg every day (qd) orally (po)] and methotrexate (15 mg once a week po). She did not stop taking the glucocorticoid and methotrexate for a long time after discharge, during which she added immunosuppressive drugs, such as cyclosporine and hydroxychloroquine, in combination and adjusted the dosage of hormones because of her unstable condition. The patient continued to suffer from limb weakness and dysphagia in early August 2018, but no new rash or edema appeared throughout the body when she was taking prednisone (10 mg qd po), methotrexate (10 mg once a week po), and cyclosporine [50 mg twice a day (bid) po]. She had a history of hypertension and depression and had undergone appendectomy.
The patient did not have a history of smoking or drinking.
The patient was 160 cm tall, weighed 45 kg, and had a body mass index of 17.58. Blotchy pigmentation was present on the neck, both legs, and hips. She had abdominal tenderness but not rebound pain. Her limbs and neck muscles also had tenderness. Her distal muscle strength was level 4, her proximal muscle strength was level 3, and her muscle tone was normal.
The result of routine blood examination was as follows: White blood cell count, 5.03 × 109/L; red blood cell count, 2.42 × 1012/L; and hemoglobin, 70.70 g/L. Routine stool examination showed positive occult blood with red and white blood cells in the stool. Liver function showed that her albumin decreased to 32.60 g/L. D-dimer was 742 ng/mL. The autoantibody test results were as follows: antinuclear antibody (+), anticentromere antibody (+), anti-Ro52 antibody (+), and anticentromere protein B antibody (+). Immunofluorescence staining indicated a centromeric-type disease (1:320). Parasites and bacteria were not found in the feces. Cardiac enzymes, tuberculosis antibody, T-spot test, cytomegalovirus DNA and antibodies, Epstein-Barr virus antibodies, and tumor markers were normal.
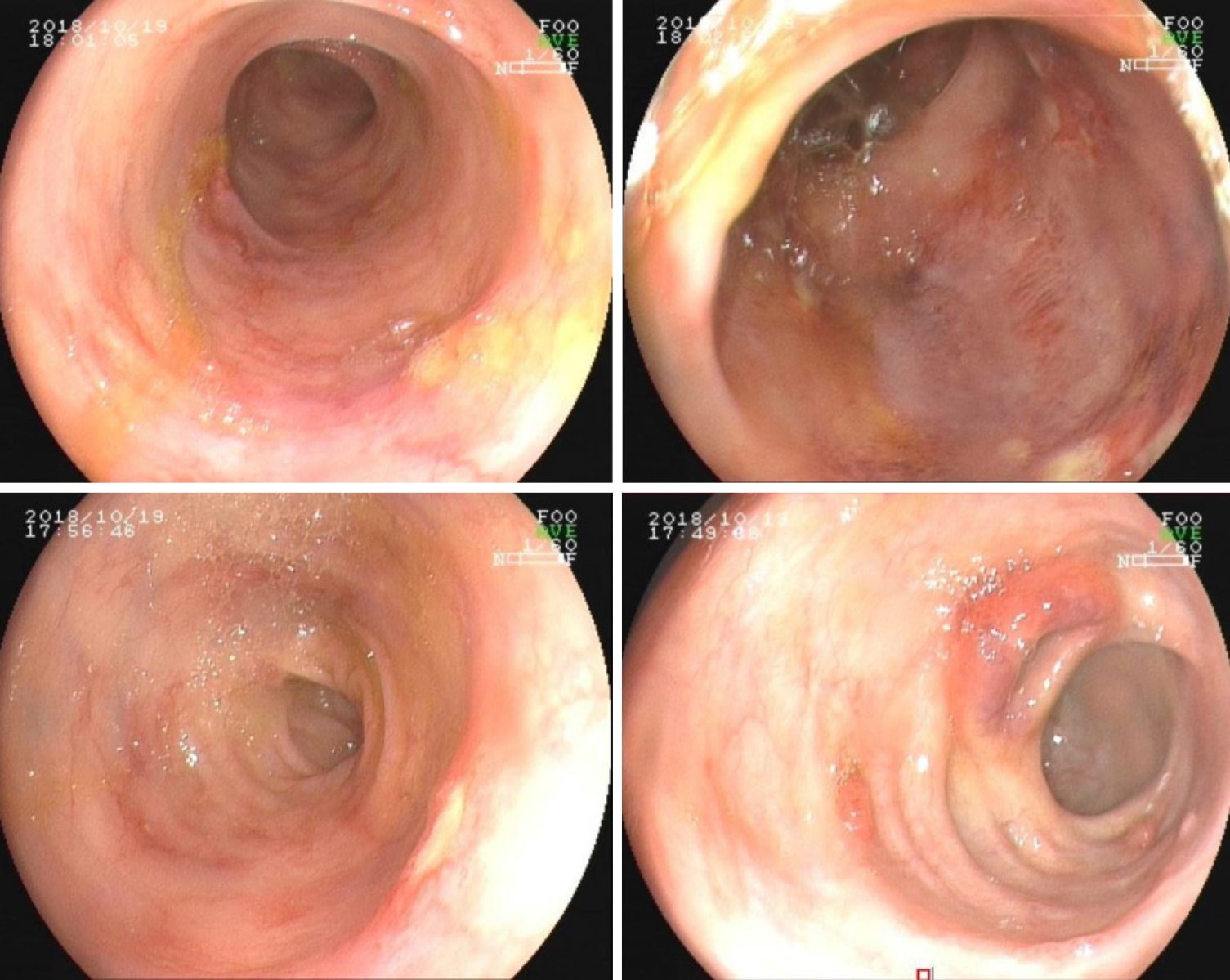
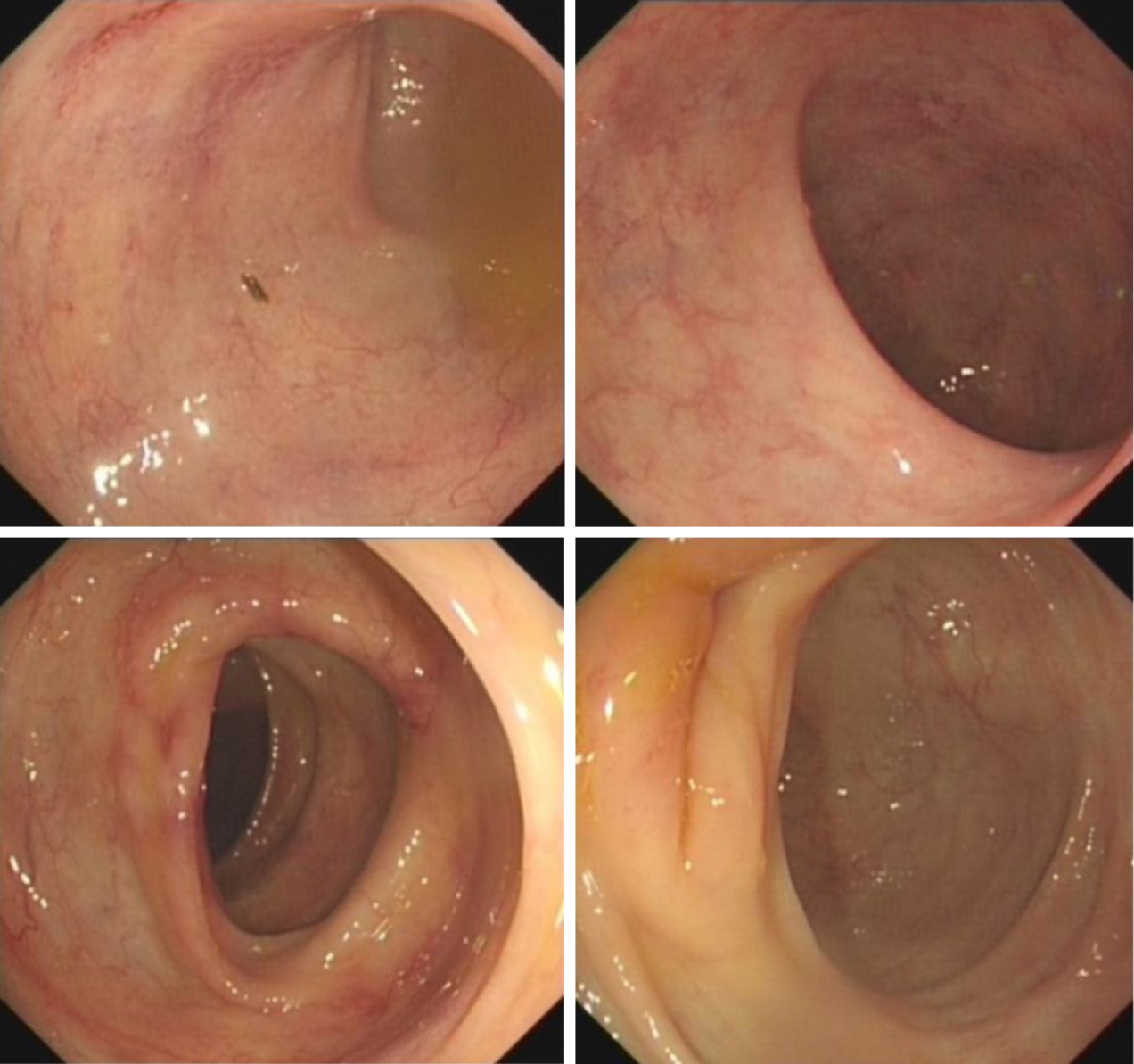
Colonoscopy showed multiple hyperemia, erosion, and ulcers in the whole colon and rectum. The ulcer was approximately 0.3-0.6 cm and was accompanied by yellow and white moss-like structures and edema of the surrounding mucosa. Part of the ileum had hyperemia and erosion. Multiple broad basal and pedicled polyps with a red surface and a size of 0.3-0.7 cm was found in the ileocecal region (Figure 4).
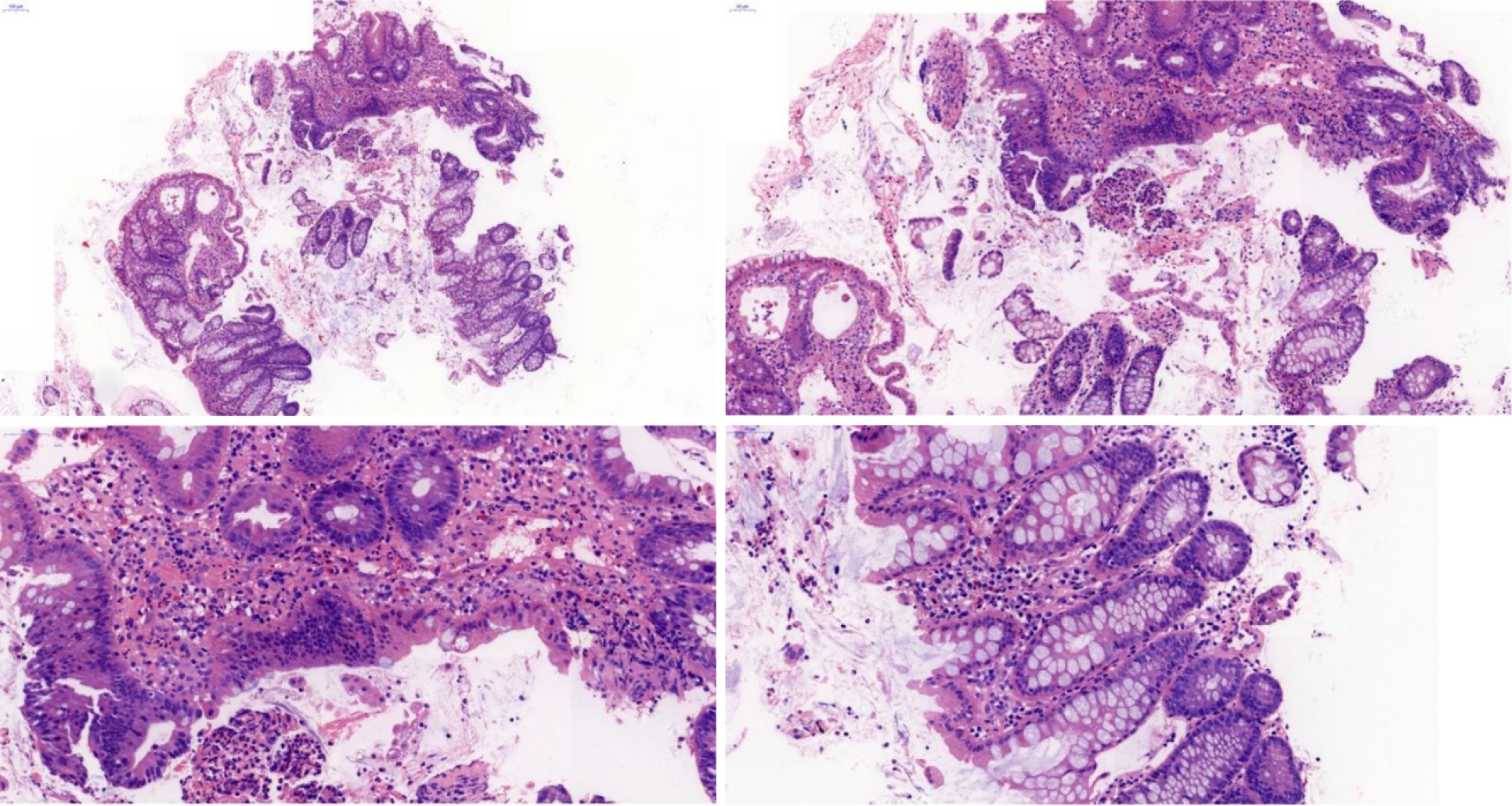
Pathological results showed a moderate chronic inflammation of the transverse colon mucosa accompanied by neutrophil infiltration and appendage as the ulcer changed (Figure 5).
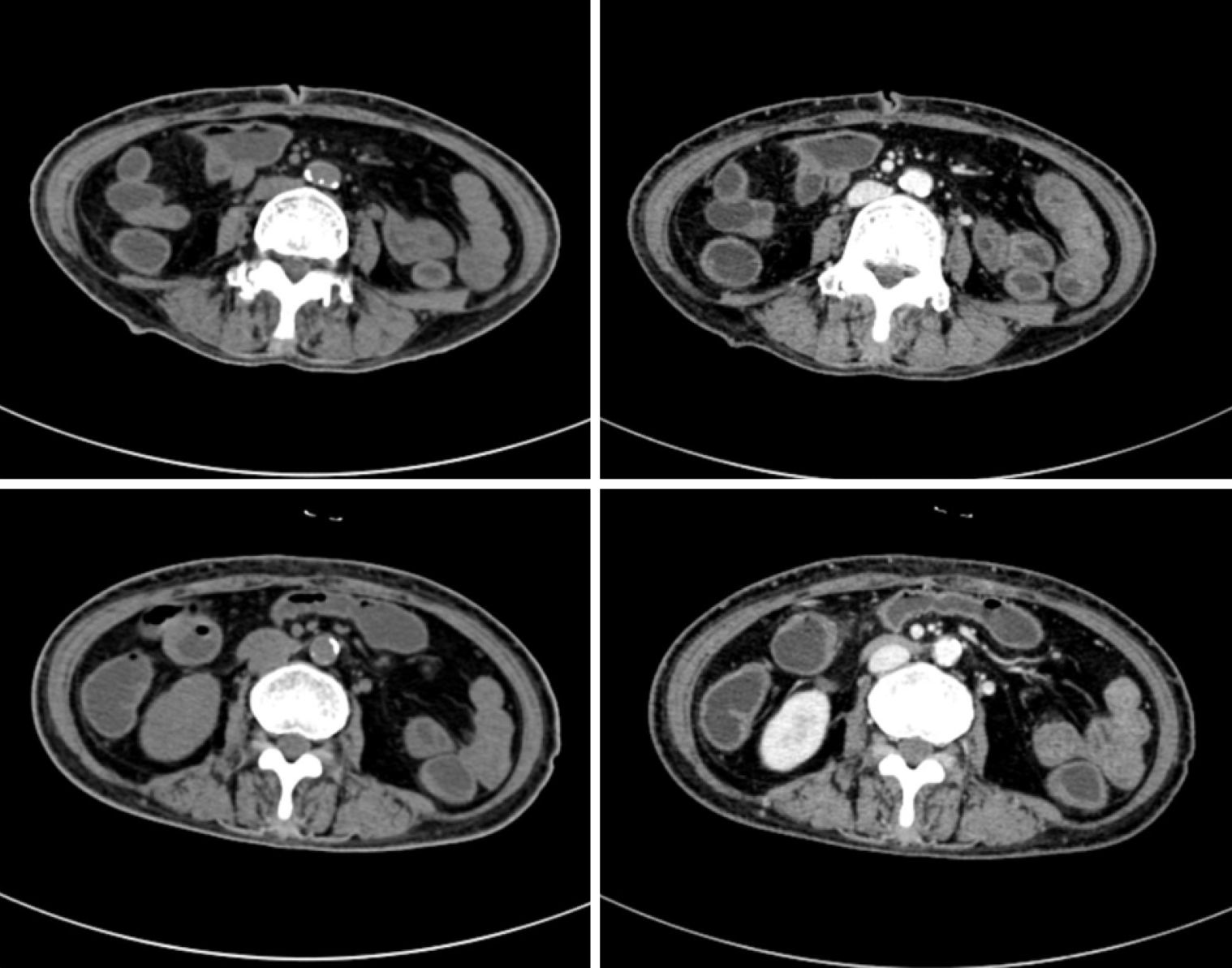
Computed tomography enterography showed that the wall of the splenic curvature, descending colon, sigmoid colon, and rectum were slightly thickened and the colonic pouch became shallow, part of which was like sausage. These characteristics turned out to be UC (Figure 6).
Zhan-Rui Chen, BM, Associate Chief Physician of Rheumatology and Immunology.
Yun Pei, BM, Associate Chief Physician of Radiology.
Zu-Yun Li, Master of Pathology and Pathophysiology, Associate Chief Physician, and Associate Professor of Pathology.
Jun-Lin Liang, MD, Chief Physician, and Professor of Colorectal and Anal Surgery.
Yong-Sheng Zhang, MM, Associate Chief Physician of Nutrition.
Xiao-Ping Lv, MM, Chief Physician, and Professor of Gastroenterology.
After multidisciplinary consultation in our hospital, the patient was diagnosed with: (1) UC (type of first episode, extensive colonic type, moderate, active stage) with a Mayo score of 9[10-12]; (2) DM; (3) Multiple colon polyps; (4) Coronary atherosclerotic heart disease; and (5) Hypertension.
Mesalazine was temporarily added to treat intestinal symptoms because the patient was already taking glucocorticoids and immunosuppressants. We gave the patient prednisone (10 mg qd po), methotrexate (10 mg once a week po), cyclosporine (50 mg bid po), mesalazine (2 g bid po), and pivionium bromide (50 mg thrice a day po) as well as early symptomatic treatment, such as albumin supplementation and the regulation of intestinal flora, from October 18, 2018 to November 1, 2018. However, the digestive tract symptoms did not improve. We consulted the expert opinions of the rheumatology department and finally gave the patient gamma globulin [5 g qd for 3 d via intravenous (IV) drip] combined with prednisone acetate (5 mg qd for 10 d po). On November 6, 2018, we gave infliximab (5 mg/kg via IV drip) treatment supplemented by mesalazine (2 g bid po). The patient occasionally experienced abdominal pain, did not have diarrhea, and was able to defecate formed stool once a day after the first injection of infliximab. Thus, the patient was discharged. The patient was instructed to take a daily dose of mesalazine (2 g bid po) at home, and she returned to the hospital regularly for infliximab treatment at weeks 2 and 6 and then every 8 wk after the fourth treatment.
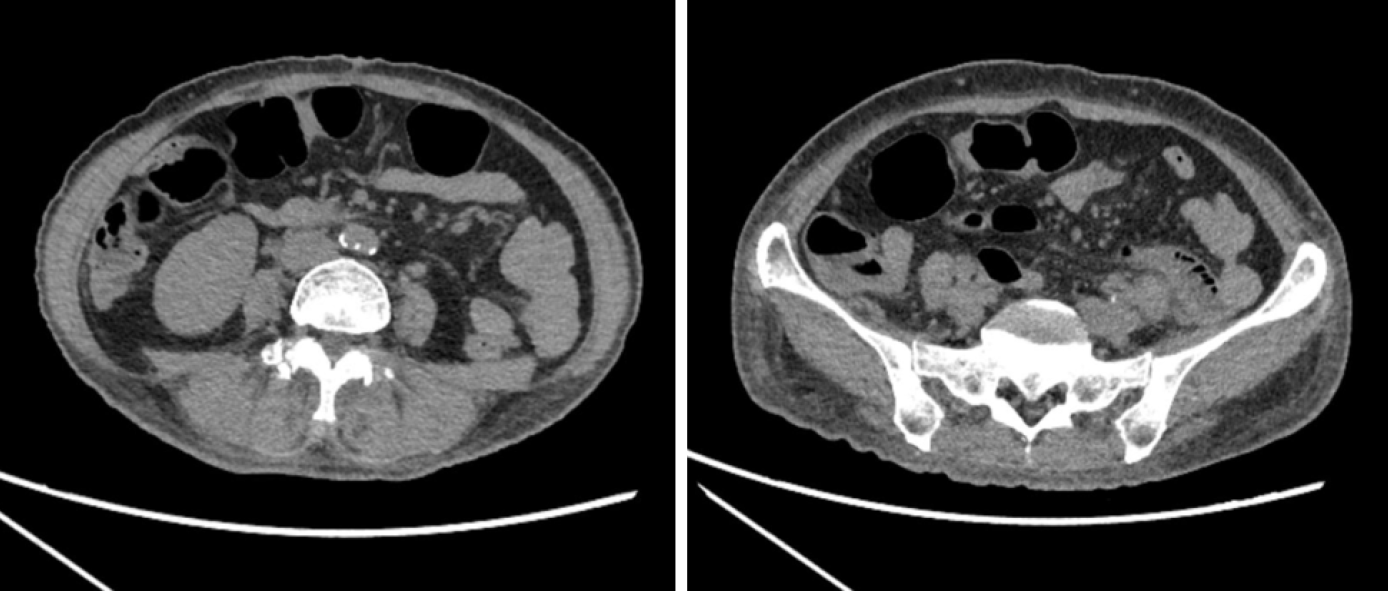
At home, the patient occasionally experienced abdominal pain but did not have diarrhea and was able to excrete formed stool once a day. Muscle pain and weakness in the extremities were remarkably relieved, and the skin rash around the eyes and the back of the hand darkened in color and reduced in size day by day. She gained 15 kg with an increase in body mass index and could walk independently by the fourth injection of infliximab. She also had a good control of depression (Figure 7). Her symptoms disappeared during the fourth treatment with infliximab. Abdominal computed tomography showed that the wall of the colon and rectum was slightly thickened compared to before (Figure 8). Colonoscopy re-examination showed that the mucosa of the whole colon and rectum were slightly edematous and less smooth with the formation of scattered ulcer scars and the presence of a little patchy mucosal erosion. Vascular texture was coarse and messy. The ulcer also improved and disappeared (Figure 9). The updated diagnosis was UC (extensive colonic type, mild, remission) with a Mayo score of 2[11,12].
The most common digestive tract discomfort in adult DM is dysphagia, whereas gastrointestinal involvement is relatively rare[13,14]. Gastrointestinal symptoms in patients with DM may be caused by mild gastrointestinal vasculitis and the involvement of the smooth muscles of the intestines[15]. Kidambi et al[14] found that 79.1% of patients with DM who underwent colonoscopy because of abdominal pain and diarrhea had no organic lesions in the gastrointestinal tract, whereas the rest were mostly complicated by rare intestinal adenomas. Therefore, the possibility of DM-associated enteritis is very small.
About a quarter of patients will develop EIMs prior to IBD onset, and the rest will develop parenteral manifestations after IBD diagnosis[4]. IBD can be associated with DM[6,7]. The results of Tseng et al[16] showed that the cumulative incidence of DM in patients with UC is higher than that of the control group, and UC is positively correlated with DM. We suspect that their correlation is caused by their similar mechanisms. Autoimmune diseases, such as DM, and autoinflammatory disease, such as IBD, are at the opposite ends of the same disease spectrum[17]. DM and UC have imbalances of Th17 and Treg cytokines, in which Th17 is increased and Treg is decreased[18,19]. A large-scale retrospective study on the combination of IBD and DM locally or abroad has not been conducted yet because of the low incidence of these diseases. Thus, the connection and mechanism of the two diseases remain unexplored.
The diagnosis of DM in this patient was definite. The patient still had skin pigmentation after long-term treatment with prednisone, methotrexate, and cyclosporine, but the rash and muscle strength were remarkably improved; therefore, the patient’s DM was stable. Vasculitis can cause gastrointestinal diseases, but the patient had no other symptoms of vasculitis. The result of vasculitis-related immunological examination was normal. Small intestinal computed tomography enterography showed no characteristic manifestations of ischemic enterocolitis, such as comb sign or the target sign of mesenteric vessels[20]. The rheumatology expert thought that the evidence of vasculitis was insufficient. We diagnosed the patient with UC rather than other DM-related intestinal disease based on the results of the colonoscopy and pathological biopsy. DM and IBD have similar but different drug treatments. Therefore, we considered whether to use DM-based or UC-based treatments. The symptoms of patients with DM and IBD are remarkably improved by hormones and 5-aminosalicylic acid[6,7]. However, the patient’s condition was not improved by mesalazine, which is a DM-based treatment. The patient’s condition 2 years prior to the onset of intestinal symptoms was poorly controlled by multiple hormonal and immunosuppressive drugs. Therefore, we presumed that the patient had a negative reaction to hormones. In addition, this patient had extensive intestinal lesions, low albumin, and anemia, which indicate severe ulcerative colitis[21]. Therefore, we gave the patient an early conversion treatment of infliximab to control intestinal inflammation.
Infliximab is a chimeric monoclonal antibody against tumor necrosis factor-α. It is a combination of human and mouse proteins. It can induce the production of regulatory macrophages and the apoptosis of proinflammatory T helper cells, inhibit growth factors, and downregulate the proinflammatory activity of neutrophils[22,23]. Several studies have reported the efficacy of infliximab in IBD, which is used for patients with moderate to severe IBD who are unresponsive to hormones and immunosuppressive agents or have serious adverse reactions to these drugs[24]; therefore, infliximab can benefit patients with the EIMs of IBD, such as erythema nodosum, ankylosing spondylitis, and pyoderma[25]. Common adverse reactions caused by infliximab include acute infusion reactions, such as skin rashes, headaches, flushing, hypotension, and other allergic reactions. Given that infliximab also increases the risk of malignant tumors, neurological diseases, and infections and exerts other adverse effects, such as liver, blood system, heart, and other system damage, patients need to be screened for tuberculosis and hepatitis B virus infection, advanced heart failure (New York Heart Association III or IV Grade), and neurological diseases before treatment with this drug[26,27].
Patients with IBD receive intravenous injections of infliximab every 8 wk at 0, 2, 6, and thereafter at a dose of 5 mg/kg in accordance with drug safety, effectiveness, and economy[12]. Although researchers believe that anti-tumor necrosis factor-α can also be used for DM, few have studied the effects of infliximab on DM. Some case reports indicated that infliximab is beneficial for the treatment of DM with interstitial lung diseases[28]. A randomized double-blind controlled study showed that infliximab can improve muscle strength in patients with polymyositis and DM[29]. We gave the patient an IV injection of gamma globulin as an adjuvant therapy before the first infliximab treatment to control disease progression. Gamma globulin can be used in patients with IBD[30] and refractory DM who cannot respond to hormones and immunosuppressive drugs effectively[31]. The patient remained stable in the follow-up treatment with infliximab and mesalazine alone. The effective control of UC is conducive to the improvement of EIMs, such as DM.
Immune-mediated diseases can involve multiple organs and cause many difficulties for specialists in differential diagnosis. Rare systemic association should be considered in the diagnosis and treatment of such diseases when symptoms are not related or the condition cannot be improved under conventional treatment. The use of biological agents is a new approach in the treatment of these rare diseases.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ekmektzoglou K, Tabll AA S-Editor: Chen XF L-Editor: Filipodia P-Editor: Liu JH
| 1. | Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017;389:1756-1770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2199] [Cited by in RCA: 2486] [Article Influence: 310.8] [Reference Citation Analysis (2)] |
| 2. | Yang BR, Choi NK, Kim MS, Chun J, Joo SH, Kim H, Lee J. Prevalence of extraintestinal manifestations in Korean inflammatory bowel disease patients. PLoS One. 2018;13:e0200363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Zippi M, Corrado C, Pica R, Avallone EV, Cassieri C, De Nitto D, Paoluzi P, Vernia P. Extraintestinal manifestations in a large series of Italian inflammatory bowel disease patients. World J Gastroenterol. 2014;20:17463-17467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 100] [Cited by in RCA: 98] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 4. | Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:1982-1992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 546] [Cited by in RCA: 472] [Article Influence: 47.2] [Reference Citation Analysis (0)] |
| 5. | Bourikas LA, Papadakis KA. Musculoskeletal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:1915-1924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Szabo N, Lukacs S, Kulcsar I, Gunasekera W, Nagy-Toldi A, Dezso B, Danko K. Association of idiopathic inflammatory myopathy and Crohn's disease. Clin Rheumatol. 2009;28:99-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Chugh S, Dilawari JB, Sawhney IM, Dang N, Radotra BD, Chawla YK. Polymyositis associated with ulcerative colitis. Gut. 1993;34:567-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Troyanov Y, Targoff IN, Payette MP, Raynauld JP, Chartier S, Goulet JR, Bourré-Tessier J, Rich E, Grodzicky T, Fritzler MJ, Joyal F, Koenig M, Senécal JL. Redefining dermatomyositis: a description of new diagnostic criteria that differentiate pure dermatomyositis from overlap myositis with dermatomyositis features. Medicine (Baltimore). 2014;93:318-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 9. | Karri SB, Kannan MA, Rajashekhar L, Uppin MS, Challa S. Clinico pathological study of adult dermatomyositis: Importance of muscle histology in the diagnosis. Ann Indian Acad Neurol. 2015;18:194-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Harbord M, Eliakim R, Bettenworth D, Karmiris K, Katsanos K, Kopylov U, Kucharzik T, Molnár T, Raine T, Sebastian S, de Sousa HT, Dignass A, Carbonnel F; European Crohn’s and Colitis Organisation [ECCO]. Corrigendum: Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 2: Current Management. J Crohns Colitis. 2017;11:1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55:749-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1970] [Cited by in RCA: 2352] [Article Influence: 123.8] [Reference Citation Analysis (2)] |
| 12. | Rutgeerts P, Sandborn WJ, Feagan BG, Reinisch W, Olson A, Johanns J, Travers S, Rachmilewitz D, Hanauer SB, Lichtenstein GR, de Villiers WJ, Present D, Sands BE, Colombel JF. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462-2476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2744] [Cited by in RCA: 2886] [Article Influence: 144.3] [Reference Citation Analysis (2)] |
| 13. | Ebert EC. Review article: the gastrointestinal complications of myositis. Aliment Pharmacol Ther. 2010;31:359-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 14. | Kidambi TD, Schmajuk G, Gross AJ, Ostroff JW, Terdiman JP, Lee JK. Endoscopy is of low yield in the identification of gastrointestinal neoplasia in patients with dermatomyositis: A cross-sectional study. World J Gastroenterol. 2017;23:4788-4795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Tweezer-Zaks N, Ben-Horin S, Schiby G, Bank I, Levi Y, Livneh A, Langevitz P. Severe gastrointestinal inflammation in adult dermatomyositis: characterization of a novel clinical association. Am J Med Sci. 2006;332:308-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Tseng CC, Chang SJ, Liao WT, Chan YT, Tsai WC, Ou TT, Wu CC, Sung WY, Hsieh MC, Yen JH. Increased Cumulative Incidence of Dermatomyositis in Ulcerative Colitis: a Nationwide Cohort Study. Sci Rep. 2016;6:28175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | McGonagle D, McDermott MF. A proposed classification of the immunological diseases. PLoS Med. 2006;3:e297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 672] [Cited by in RCA: 577] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 18. | Gong Y, Lin Y, Zhao N, He X, Lu A, Wei W, Jiang M. The Th17/Treg Immune Imbalance in Ulcerative Colitis Disease in a Chinese Han Population. Mediators Inflamm. 2016;2016:7089137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 19. | Espinosa-Ortega F, Gómez-Martin D, Santana-De Anda K, Romo-Tena J, Villaseñor-Ovies P, Alcocer-Varela J. Quantitative T cell subsets profile in peripheral blood from patients with idiopathic inflammatory myopathies: tilting the balance towards proinflammatory and pro-apoptotic subsets. Clin Exp Immunol. 2015;179:520-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Hokama A, Kishimoto K, Ihama Y, Kobashigawa C, Nakamoto M, Hirata T, Kinjo N, Higa F, Tateyama M, Kinjo F, Iseki K, Kato S, Fujita J. Endoscopic and radiographic features of gastrointestinal involvement in vasculitis. World J Gastrointest Endosc. 2012;4:50-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Siegel CA, Whitman CB, Spiegel BMR, Feagan B, Sands B, Loftus EV Jr, Panaccione R, D'Haens G, Bernstein CN, Gearry R, Ng SC, Mantzaris GJ, Sartor B, Silverberg MS, Riddell R, Koutroubakis IE, O'Morain C, Lakatos PL, McGovern DPB, Halfvarson J, Reinisch W, Rogler G, Kruis W, Tysk C, Schreiber S, Danese S, Sandborn W, Griffiths A, Moum B, Gasche C, Pallone F, Travis S, Panes J, Colombel JF, Hanauer S, Peyrin-Biroulet L. Development of an index to define overall disease severity in IBD. Gut. 2018;67:244-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 108] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 22. | Zhang C, Shu W, Zhou G, Lin J, Chu F, Wu H, Liu Z. Anti-TNF-α Therapy Suppresses Proinflammatory Activities of Mucosal Neutrophils in Inflammatory Bowel Disease. Mediators Inflamm. 2018;2018:3021863. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 23. | Vos AC, Wildenberg ME, Arijs I, Duijvestein M, Verhaar AP, de Hertogh G, Vermeire S, Rutgeerts P, van den Brink GR, Hommes DW. Regulatory macrophages induced by infliximab are involved in healing in vivo and in vitro. Inflamm Bowel Dis. 2012;18:401-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 148] [Article Influence: 11.4] [Reference Citation Analysis (1)] |
| 24. | Järnerot G, Hertervig E, Friis-Liby I, Blomquist L, Karlén P, Grännö C, Vilien M, Ström M, Danielsson A, Verbaan H, Hellström PM, Magnuson A, Curman B. Infliximab as rescue therapy in severe to moderately severe ulcerative colitis: a randomized, placebo-controlled study. Gastroenterology. 2005;128:1805-1811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 774] [Cited by in RCA: 768] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 25. | Harbord M, Annese V, Vavricka SR, Allez M, Barreiro-de Acosta M, Boberg KM, Burisch J, De Vos M, De Vries AM, Dick AD, Juillerat P, Karlsen TH, Koutroubakis I, Lakatos PL, Orchard T, Papay P, Raine T, Reinshagen M, Thaci D, Tilg H, Carbonnel F; European Crohn’s and Colitis Organisation. The First European Evidence-based Consensus on Extra-intestinal Manifestations in Inflammatory Bowel Disease. J Crohns Colitis. 2016;10:239-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 619] [Cited by in RCA: 546] [Article Influence: 60.7] [Reference Citation Analysis (0)] |
| 26. | Nielsen OH, Ainsworth MA. Tumor necrosis factor inhibitors for inflammatory bowel disease. N Engl J Med. 2013;369:754-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 251] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 27. | Subedi S, Gong Y, Chen Y, Shi Y. Infliximab and biosimilar infliximab in psoriasis: efficacy, loss of efficacy, and adverse events. Drug Des Devel Ther. 2019;13:2491-2502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 61] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 28. | Chen D, Wang XB, Zhou Y, Zhu XC. Efficacy of infliximab in the treatment for dermatomyositis with acute interstitial pneumonia: a study of fourteen cases and literature review. Rheumatol Int. 2013;33:2455-2458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Schiffenbauer A, Garg M, Castro C, Pokrovnichka A, Joe G, Shrader J, Cabalar IV, Faghihi-Kashani S, Harris-Love MO, Plotz PH, Miller FW, Gourley M. A randomized, double-blind, placebo-controlled trial of infliximab in refractory polymyositis and dermatomyositis. Semin Arthritis Rheum. 2018;47:858-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 30. | Shah S, Terdiman J, Gundling K, Mahadevan U. Immunoglobulin therapy for refractory Crohn's disease. Therap Adv Gastroenterol. 2014;7:99-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Patel SY, Kumararatne DS. From black magic to science: understanding the rationale for the use of intravenous immunoglobulin to treat inflammatory myopathies. Clin Exp Immunol. 2001;124:169-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |