Published online Nov 28, 2020. doi: 10.3748/wjg.v26.i44.7022
Peer-review started: August 6, 2020
First decision: October 18, 2020
Revised: October 31, 2020
Accepted: November 13, 2020
Article in press: November 13, 2020
Published online: November 28, 2020
Preoperative chemoradiotherapy (CRT) is a standard treatment modality for locally advanced rectal cancer. However, CRT alone cannot improve overall survival. Approximately 20% of patients with CRT-resistant tumors show disease progression. Therefore, predictive factors for treatment response are needed to identify patients who will benefit from CRT. We theorized that the prognosis may vary if patients are classified according to pre- to post-CRT changes in carcinoembryonic antigen (CEA) levels.
To identify patients with locally advanced rectal cancer for preoperative chemoradiotherapy based on carcinoembryonic antigen levels.
We retrospectively included locally advanced rectal cancer patients who underwent preoperative CRT and curative resection between 2011 and 2017. Patients were assigned to groups A, B, and C based on pre- and post-CRT serum CEA levels: Both > 5; pre > 5 and post ≤ 5; and both ≤ 5 ng/mL, respectively. We compared the response to CRT based on changes in serum CEA levels. Receiver operating characteristic curve analysis was performed to determine optimal cutoff for neutrophil–lymphocyte ratio and platelet–lymphocyte ratio. Multivariate logistic regression analysis was used to evaluate the prognostic factors for pathologic complete response (pCR)/good response.
The cohort comprised 145 patients; of them, 27, 43, and 65 belonged to groups A, B, and C, respectively, according to changes in serum CEA levels before and after CRT. Pre- (P < 0.001) and post-CRT (P < 0.001) CEA levels and the ratio of down-staging (P = 0.013) were higher in Groups B and C than in Group A. The ratio of pathologic tumor regression grade 0/1 significantly differed among the groups (P = 0.003). Group C had the highest number of patients showing pCR (P < 0.001). Most patients with pCR showed pre- and post-CRT CEA levels < 5 ng/mL (P < 0.001, P = 0.008). Pre- and post-CRT CEA levels were important risk factors for pCR (OR = 18.71; 95%CI: 4.62–129.51, P < 0.001) and good response (OR = 5.07; 95%CI: 1.92–14.83, P = 0.002), respectively. Pre-CRT neutrophil–lymphocyte ratio and post-CRT T ≥ 3 stage were also prognostic factors for pCR or good response.
Pre- and post-CRT CEA levels, as well as change in CEA levels, were prognostic markers for treatment response to CRT and may facilitate treatment individualization for rectal cancer.
Core Tip: The response of preoperative chemoradiotherapy (CRT) for rectal cancer varies from pathologic complete response to disease progression. Pre- and post-CRT levels of carcinoembryonic antigen can indicate treatment response to CRT in patients with locally advanced rectal cancer. Carcinoembryonic antigen can be used as a prognostic marker to facilitate treatment individualization in rectal cancer.
- Citation: Cheong C, Shin JS, Suh KW. Prognostic value of changes in serum carcinoembryonic antigen levels for preoperative chemoradiotherapy response in locally advanced rectal cancer. World J Gastroenterol 2020; 26(44): 7022-7035
- URL: https://www.wjgnet.com/1007-9327/full/v26/i44/7022.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i44.7022
Preoperative chemoradiotherapy (CRT) is a standard treatment modality for locally advanced rectal cancer (LARC) based on findings from randomized controlled trials[1-3]. Advances in CRT and surgical modalities have resulted in better oncologic outcomes for rectal cancer, including a local recurrence rate of < 10%. However, CRT alone cannot improve overall survival[1] and treatment response to CRT can vary from pathologic complete response (pCR) to disease progression[4] Tumor sensitivity to CRT causes tumor regression after delayed surgery; approximately 40% of patients with CRT-sensitive tumors achieve partial response, and 8%–20% achieve pCR[4-6]. However, approximately 20% of patients with CRT-resistant tumors show disease progression[4]. Therefore, predictive factors for treatment response are needed to identify patients who will benefit from CRT.
Serum carcinoembryonic antigen (CEA) is an established biomarker for predicting prognosis and monitoring progression of colorectal cancer. Several studies have shown that the pretreatment serum level of CEA is associated with post-CRT pCR, down-staging, and survival (Table 1)[7-12]. However, previous studies focused on the fact that patients with higher pretreatment CEA (> 5 ng/mL) have poor prognosis and did not concentrate with the change of CEA levels.
| Ref. | Study design | pCR (%) | Related factor with response of preoperative CRT | Independent factor for pCR |
| Restivo et al[7], 2013 | Prospective (n = 260) | 16.5% | CEA < 5 ng/mL and distance from anal verge > 5 cm | |
| Huh et al[8], 2013 | Retrospective (n = 391) | 14.6% | Noncircumferential tumors, nonmacroscopic ulceration, WELL differentiation, Early T, N stage, low level of pretreatment CEA | Tumor circumferentiality, macroscopic ulceration, pretreatment CEA < 5 ng/mL |
| Wallin et al[9], 2013 | Retrospective (n = 469) | 20.0% | Pretreatment CEA ≤ 5 ng/mL | |
| Kleiman et al[10], 2015 | Prospective (n = 141) | 13.5% | Low post CRT CEA level, normalization of CEA from initial elevated; CEA level | |
| Hu et al[11], 2018 | Prospective (n = 146) | 15.0% | CEA exponential decrease group between pretreatment and during-CRT: Higher rates of downstaging and pCR | CEA clearance pattern |
| Yamamoto et al[12], 2019 | Prospective (n = 111) | Combination of lymphocyte to monocyte ratio (LMR) and ypN; status: poor prognosis | Low pretreatment LMR ypN(+) |
We theorized that variations in prognosis may be observed if patients are classified by pre- to post-CRT changes in CEA levels. Early identification of poor responders or patients with tumor resistance to CRT will allow clinicians to provide more aggressive treatment, such as intensified chemotherapy.
Therefore, in this study, we evaluated whether CEA levels change from before to after CRT and analyzed the relationship between serum CEA and treatment response to CRT. We investigated the effect of preoperative CEA level before and after CRT on treatment response to CRT in patients with LARC.
We retrospectively evaluated the medical data of 145 patients who were diagnosed with rectal adenocarcinoma and underwent preoperative CRT and curative resection at Ajou Hospital between January 2011 and December 2017. Based on the clinical stage, such as in the case of clinical T3 or T4 tumors, node-positive disease, and suspected diagnosis of invasion into the mesorectal fascia on preoperative imaging, some patients with advanced rectal cancer were offered concomitant CRT. We excluded patients with synchronous distant metastasis, clinical stage T2 disease, or without post-treatment magnetic resonance imaging (MRI). We included 135 patients in the final study sample. Long-course preoperative CRT was carried out with a total radiation dose of 5040 cGy delivered in 25 fractions over 5 wk; neoadjuvant chemotherapy with 5-fluorouracil and leucovorin was administered during the first and fifth weeks of radiotherapy. Patients were divided into three groups according to pre- and post-CRT serum CEA levels above/below 5 ng/mL. Groups A, B, and C comprised patients with pre- and post-CRT CEA levels > 5; > 5 and ≤ 5, and ≤ 5 ng/mL, respectively. This study was approved by the Institutional Review Board of Ajou Hospital (approval number: MED-MDB-18-329), and the need for informed consent was waived in view of the retrospective study design.
All patients were preoperatively evaluated by physical examination, colonoscopy, abdominopelvic computed tomography (APCT), chest CT, pelvic MRI, and routine laboratory tests, including serum CEA measurements. The tumor location was defined as the distance from the anal verge (AV) to the lowest margin of the tumor on MRI or sigmoidoscopy. Treatment response to CRT was assessed using APCT, pelvic MRI, sigmoidoscopy, and routine laboratory tests at 4–5 wk after CRT. Surgery was performed 6–8 wk after CRT and included low anterior resection with colorectal or coloanal anastomosis, abdominoperineal resection, Hartmann’s operation, and total proctocolectomy. Pathologic results were reported according to the Seventh American Joint Committee on Cancer TNM staging system. Treatment response to CRT and tumor regression grade (TRG) were evaluated by experienced pathologists at the study center in accordance with the American Joint Committee on Cancer TRG system[13,14].
Continuous variables were analyzed using the Student’s t-test and analysis of variance, and data are presented as mean ± SD or medians with ranges. Categorical variables were analyzed using the chi-square or Fisher’s exact test. The optimal cutoff values for neutrophil–lymphocyte ratio (NLR) and platelet–lymphocyte ratio (PLR) were calculated using receiver operating characteristic (ROC) analysis. The cutoff value was determined by the point on the ROC curve with the minimum distance from the 0% false-positive rate and 100% true-positive rate. Multivariate analyses for pCR or good response were undertaken using multiple logistic regression. The Kaplan–Meier method and log-rank test were used to analyze disease-free survival (DFS) and overall survival. All analyses were conducted in R package vs 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria). A P value < 0.05 was considered statistically significant.
Data from 135 patients [men, n = 99 (73.3%); age, 60.1 ± 10.9 (mean ± SD) years] were included in the final analysis; 34.1% (n = 46) of the patients were smokers. The mean (SD) pre-CRT tumor size was 4.6 (± 1.4) cm on MRI images, and tumor distance from AV was 6.4 (± 3.0) cm. The mean serum CEA level was significantly reduced from 18.1 to 4.8 ng/mL after CRT (Table 2).
| Characteristics | Distribution |
| Age (yr, mean ± SD) | 60.1 ± 10.9 |
| Sex | |
| Male | 99 (73.3%) |
| Female | 36 (26.7%) |
| BMI (kg/m2, mean ± SD) | 22.9 ± 3.1 |
| Smoker | 46 (34.1%) |
| ASA | |
| 1 | 80 (59.3%) |
| 2 | 40 (29.6%) |
| 3 | 14 (10.4%) |
| 4 | 1 (0.7%) |
| Distance of tumor from the anal verge (cm, mean ± SD) | 6.4 ± 3.0 |
| Pre-CRT CEA (ng/mL, mean ± SD) | 18.1 ± 45.0 |
| Pre-CRT tumor size (cm, mean ± SD) | 4.6 ± 1.4 |
| Pre-CRT TNM stage | |
| I | 1 (0.7%) |
| II | 13 (9.6%) |
| III | 121 (89.6%) |
| Curative resection after CRT | |
| Low anterior resection | 64 (47.4%) |
| Ultra-low anterior resection | 17 (12.6%) |
| Abdominoperineal resection | 46 (34.1%) |
| Hartmann operation | 7 (5.2%) |
| Total colectomy | 1 (0.7%) |
| Radiation dose, cGy | 5040 |
| Interval from preoperative CRT to operation (wk) | 7.8 ± 1.7 |
| Post-CRT CEA (ng/mL) | 4.8 ± 8.1 |
| Down-staging after preoperative CRT | 60 (44.4%) |
| Pathologic complete response | 27 (20.0%) |
| Adjuvant chemotherapy | 121 (89.6%) |
| Follow-up (mo) | 60.4 ± 24.3 |
Groups A, B, and C comprised 27, 43, and 65 patients, respectively. Intergroup comparisons of baseline parameters, such as age, sex, pre-CRT size of tumor, and clinical T stage, based on change in the CEA level from before to after CRT showed no significant differences. However, the analysis showed large intergroup differences in the pre-CRT CEA level [mean (range): Group A, 25.8 (10.6–70.7) vs Group B, 11.3 (6.8–21.3) vs Group C, 2.4 (1.8–3.3); P < 0.001]. Post-CRT CEA levels dramatically decreased in each group but was significantly different for Group A [A, 8.4 (6.0–13.7) vs B, 2.9 (2.0–4.0) vs C, 1.8 (1.2–2.9); P < 0.001]. The cutoff values of NLR and PLR for pCR were determined as 2.8 and 138.2, respectively, and there were no intergroup differences (P = 0.983, P = 0.132). Moreover, the ratio of post-CRT down-staging was lower in Group A than in groups B and C (A, 22.2% vs B, 41.9% vs C, 55.4%; P = 0.013; Table 3).
| Variables | Group A (n = 27) | Group B (n = 43) | Group C (n = 65) | P value |
| Age, yr | > 0.999 | |||
| < 65 | 17 (63.0%) | 27 (62.8%) | 41 (63.1%) | |
| ≥ 65 | 10 (37.0%) | 16 (37.2%) | 24 (36.9%) | |
| Sex | 0.358 | |||
| Male | 21 (77.8%) | 34 (79.1%) | 44 (67.7%) | |
| Female | 6 (22.2%) | 9 (20.9%) | 21 (32.3%) | |
| ASA | 0.734 | |||
| < 3 | 23 (85.2%) | 38 (88.4%) | 59 (90.8%) | |
| ≥ 3 | 4 (14.8%) | 5 (11.6%) | 6 (9.2%) | |
| Pre-CRT tumor size (cm) | 4.6 (3.7-5.0) | 4.5 (4.0-5.1) | 4.3 (3.8-5.0) | 0.515 |
| Pre-CRT CEA (ng/mL) | 25.8 (10.6-70.7) | 11.3 (6.8-21.3) | 2.4 (1.8-3.3) | < 0.001 |
| Pre-CRT NLR | 0.983 | |||
| < 2.8 | 17 (63.0%) | 28 (65.1%) | 42 (64.6%) | |
| ≥ 2.8 | 10 (37.0%) | 15 (34.9%) | 23 (35.4%) | |
| Pre-CRT PLR | 0.132 | |||
| < 138.2 | 11 (40.7%) | 19 (44.2%) | 39 (60.0%) | |
| ≥ 138.2 | 16 (59.3%) | 24 (55.8%) | 26 (40.0%) | |
| Pre-CRT T stage | 0.217 | |||
| T3 | 18 (66.7%) | 34 (79.1%) | 54 (83.1%) | |
| T4 | 9 (33.3%) | 9 (20.9%) | 11 (16.9%) | |
| Pre-CRT N stage | 0.021 | |||
| N0 | 1 (3.7%) | 1 (2.3%) | 11 (16.9%) | |
| N+ | 26 (96.3%) | 42 (97.7%) | 54 (83.1%) | |
| Pre-CRT TNM stage | 0.021 | |||
| I | 1 (3.7%) | 0 | 0 | |
| II | 1 (3.7%) | 1 (2.3%) | 11 (16.9%) | |
| III | 25 (92.6%) | 42 (97.7%) | 54 (83.1%) | |
| Post-CRT CEA (ng/dL) | 8.4 (6.0–13.7) | 2.9 (2.0–4.0) | 1.8 (1.2–2.9) | < 0.001 |
| Post-CRT T stage | 0.001 | |||
| 0–2 | 3 (11.1%) | 5 (11.6%) | 25 (38.5%) | |
| 3–4 | 24 (88.9%) | 38 (88.4%) | 40 (61.5%) | |
| Post-CRT N stage | 0.006 | |||
| N0 | 8 (29.6%) | 20 (46.5%) | 42 (64.6%) | |
| N+ | 19 (70.4%) | 23 (53.5%) | 23 (35.4%) | |
| Post-CRT M stage | 0.090 | |||
| 0 | 25 (92.6%) | 42 (97.7%) | 65 (100%) | |
| 1 | 2 (7.4%) | 1 (2.3%) | 0 | |
| Post-CRT TNM Stage | 0.008 | |||
| 0 | 0 | 0 | 2 (3.1%) | |
| I | 2 (7.4%) | 4 (9.3%) | 19 (29.2%) | |
| II | 5 (18.5%) | 15 (34.9%) | 21 (32.3%) | |
| III | 19 (66.7%) | 23 (53.5%) | 23 (35.4%) | |
| IV | 2 (7.4%) | 1 (2.3%) | 0 | |
| Down-staging on MRI after CRT | 0.013 | |||
| No | 21 (77.8%) | 25 (58.1%) | 29 (44.6%) | |
| Yes | 6 (22.2%) | 18 (41.9%) | 36 (55.4%) |
After preoperative CRT, three patients were clinically suspected to have distant metastasis on evaluation with APCT or chest CT (Table 3). One patient in Group B was confirmed to have no distant metastasis after curative resection. Intraoperatively, one patient in Group A was found to have liver metastasis, which was not detected on preoperative imaging (Table 4). TRG showed that the response of CRT was superior in groups B and C than in Group A [TRG, 0, 1: A, 8 (29.6%) vs B, 26 (60.5%) vs C, 44 (67.7%); P = 0.003]. Moreover, the ratio of pCR was significantly higher in Group C (A, 0% vs B, 4.7% vs C, 38.5%; P < 0.001; Table 4).
| Variables | Group A (n = 27) | Group B (n = 43) | Group C (n = 65) | P value |
| Name of surgery | 0.272 | |||
| Low anterior resection | 15 (55.6%) | 22 (51.2%) | 43 (66.2%) | |
| Others1 | 12 (44.4%) | 21 (48.8%) | 22 (33.8%) | |
| Differentiation | 0.781 | |||
| Well–Moderate | 8 (29.6%) | 13 (30.2%) | 16 (24.6%) | |
| Poorly + others2 | 19 (70.4%) | 30 (69.8%) | 49 (75.4%) | |
| Lymphovascular invasion | 0.444 | |||
| No | 22 (81.5%) | 35 (81.4%) | 58 (89.2%) | |
| Yes | 5 (18.5%) | 8 (18.6%) | 7 (10.8%) | |
| Perineural invasion | 0.005 | |||
| No | 21 (77.8%) | 38 (88.4%) | 64 (98.5%) | |
| Yes | 6 (22.2%) | 5 (11.6%) | 1 (1.5%) | |
| Postoperative T stage | < 0.001 | |||
| 0–2 | 2 (7.4%) | 11 (25.6%) | 38 (58.5%) | |
| 3–4 | 25 (92.6%) | 32 (74.4%) | 27 (41.5%) | |
| Postoperative N stage | 0.538 | |||
| N0 | 15 (55.6%) | 27 (62.8%) | 44 (67.7%) | |
| N+ | 12 (44.4%) | 16 (37.2%) | 21 (32.3%) | |
| Postoperative M stage | 0.002 | |||
| M0 | 24 (88.9%) | 43 (100%) | 65 (100%) | |
| M1 | 3 (11.1%) | 0 | 0 | |
| Postoperative TNM stage | < 0.001 | |||
| 0 | 0 | 3 (7.0%) | 25 (38.5%) | |
| I | 2 (7.4%) | 5 (11.6%) | 8 (12.3%) | |
| II | 13 (48.1%) | 19 (44.2%) | 11 (16.9%) | |
| III | 9 (33.3%) | 16 (37.2%) | 21 (32.3%) | |
| IV | 3 (11.1%) | 0 | 0 | |
| CEA on postoperative day 7 | 3.7 (2.8-5.2) | 1.6 (1.1-2.2) | 1.1 (0.7-1.7) | < 0.001 |
| Tumor regression grade | < 0.001 | |||
| 0 | 1 (3.7%) | 3 (7.0%) | 26 (40.0%) | |
| 1 | 7 (25.9%) | 23 (53.5%) | 18 (27.7%) | |
| 2 | 11 (40.7%) | 14 (32.6%) | 17 (26.2%) | |
| 3 | 8 (29.6%) | 3 (7.0%) | 4 (6.2%) | |
| Good response (TRG 0,1) | 0.003 | |||
| TRG 0, 1 | 8 (29.6%) | 26 (60.5%) | 44 (67.7%) | |
| TRG 2, 3 | 19 (70.4%) | 17 (39.5%) | 21 (32.3%) | |
| Pathologic complete response | < 0.001 | |||
| pCR (-) | 27 (100%) | 41 (95.3%) | 40 (61.5%) | |
| pCR (+) | 0 | 2 (4.7%) | 25 (38.5%) |
Comparisons between the non-pCR and pCR groups showed a lower ratio of pre-CRT CEA > 5 ng/mL in the pCR group than in the non-pCR group (P < 0.001). All patients with pCR did not show post-CRT CEA levels > 5 ng/mL (non-pCR: 25.7% vs pCR: 0%; P = 0.008). The pCR group had a higher ratio of down-staging after CRT, but the finding was not significant (P = 0.051). There were no patients with lymphovascular or perineural invasion in the pCR group, and the distribution of differentiation after operation was similar between the study groups (Table 5).
| Variables | Non-pCR (n = 108) | pCR (n = 27) | P value |
| Pre-CRT tumor size (cm, mean ± SD) | 4.7 ± 1.5 | 4.4 ± 1.3 | 0.246 |
| Pre-CRT CEA, ng/mL | < 0.001 | ||
| CEA ≤ 5 | 40 (37.0%) | 25 (92.6%) | |
| CEA > 5 | 68 (63.0%) | 2 (7.4%) | |
| Pre-CRT T stage | 0.875 | ||
| T3 | 84 (77.8%) | 22 (81.5%) | |
| T4 | 24 (22.2%) | 5 (18.5%) | |
| Pre-CRT N stage | 0.004 | ||
| N0 | 6 (5.6%) | 7 (25.9%) | |
| N+ | 102 (94.4%) | 20 (74.1%) | |
| Pre-CRT TNM stage | 0.005 | ||
| I | 1 (0.9%) | 0 | |
| II | 6 (5.6%) | 7 (25.9%) | |
| III | 101 (93.5%) | 20 (74.1%) | |
| Post-CRT CEA, ng/mL | 0.008 | ||
| ≤ 5 | 81 (75.0%) | 27 (100%) | |
| > 5 | 27 (25.0%) | 0 | |
| Downstaging after CRT | 0.051 | ||
| No | 65 (60.2%) | 10 (37.0%) | |
| Yes | 43 (39.8%) | 17 (63.0%) | |
| Differentiation | > 0.999 | ||
| Well–Moderate | 30 (27.8%) | 7 (25.9%) | |
| Poor + others1 | 78 (72.2%) | 20 (74.1%) | |
| Lymphovascular invasion | 0.034 | ||
| No | 88 (81.5%) | 27 (100%) | |
| Yes | 20 (18.5%) | 0 | |
| Perineural invasion | 0.151 | ||
| No | 96 (88.9%) | 27 (100%) | |
| Yes | 12 (11.1%) | 0 |
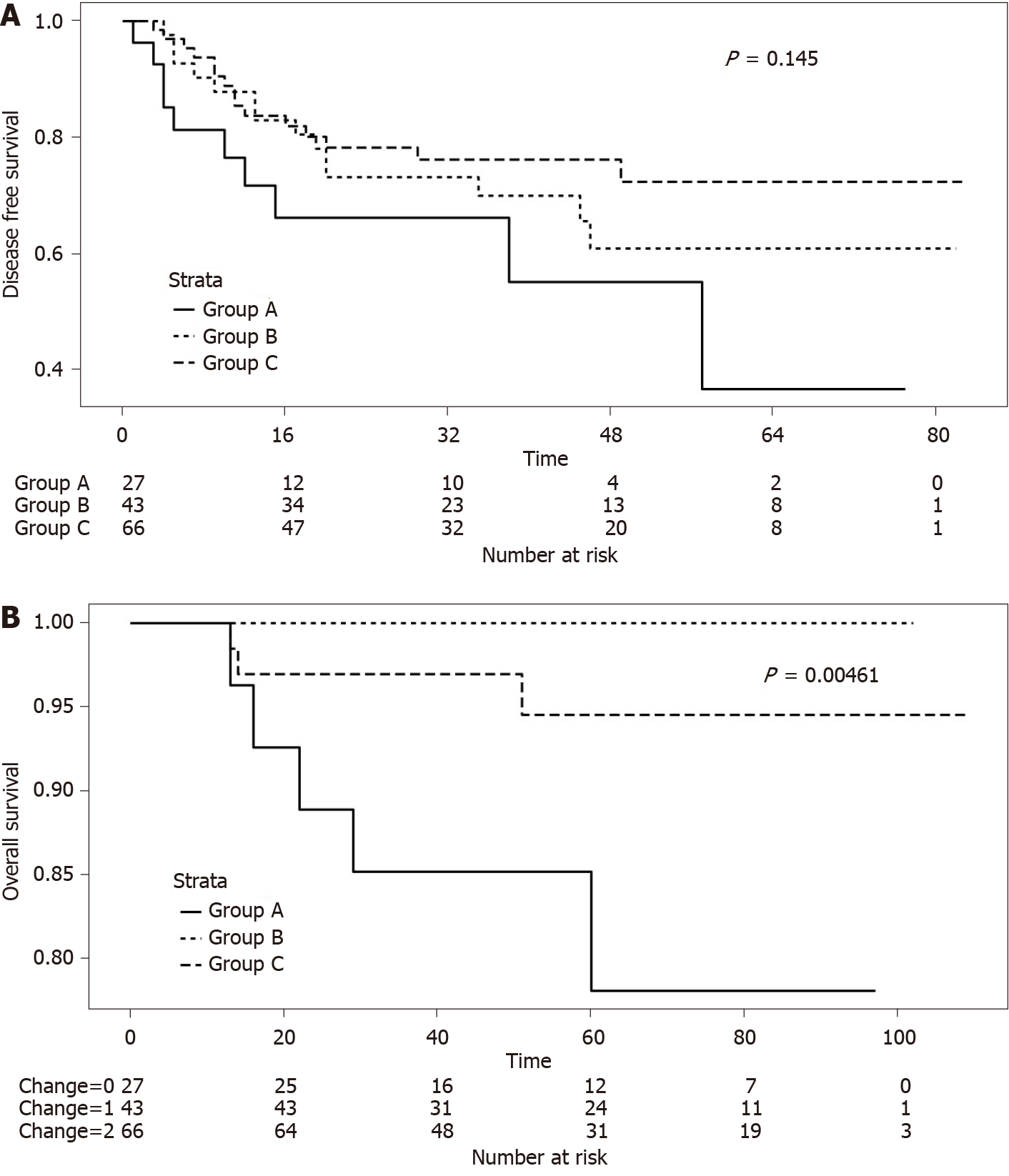
Multivariate analysis showed that sex (OR: 0.26, 95%CI: 0.08–0.80; P = 0.022), pre-CRT CEA levels ≤ 5 ng/mL (OR: 18.71, 95%CI: 4.62–129.51; P < 0.001), pre-CRT NLR < 2.8 (OR: 5.27, 95%CI: 1.55–22.55; P = 0.013), and post-CRT T stage < 3 (OR: 3.25, 95%CI: 1.09–9.97; P = 0.036) were prognostic markers for pCR. Meanwhile, post-CRT CEA levels ≤ 5 ng/mL (OR: 5.07, 95%CI: 1.92–14.83; P = 0.002) and well or moderate differentiation (OR: 3.41, 95%CI: 1.35–9.48; P = 0.013) were associated with good response. Pre-CRT NLR < 2.8 and post-CRT T stage < 3 were common prognostic factors in pCR and good response (Table 6). Despite no differences in the 5-year DFS between groups A, B, and C, we found that Group A showed a tendency of worse survival than the other study groups (Figure 1A; P = 0.145). Furthermore, the 5-year overall survival was significantly lower in Group A (Figure 1B; P = 0.005).
| Pathologic complete response | Good response (TRG 0,1) | |||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Sex (female vs male) | 0.26 (0.08–0.80) | 0.022 | ||
| Pre-CRT CEA (> 5 vs ≤ 5 ng/mL) | 18.71 (4.62–129.51) | < 0.001 | ||
| Pre-CRT NLR (≥ 2.8 vs < 2.8) | 5.27 (1.55–22.55) | 0.013 | 2.82 (1.27–6.48) | 0.013 |
| Post-CRT CEA (> 5 vs ≤ 5 ng/mL) | 5.07 (1.92–14.83) | 0.002 | ||
| Post-CRT T stage (≥ T3 vs < T3) | 3.25 (1.09–9.97) | 0.036 | 3.28 (1.23–9.90) | 0.023 |
| Postop differentiation (poorly1vs well-mod.) | 3.41 (1.35–9.48) | 0.013 | ||
This study aimed to identify the clinical factors associated with treatment response to CRT for rectal cancer. Our findings showed that pre-CRT CEA was a prognostic factor for pCR. Patients with preoperative serum CEA levels ≤ 5 ng/mL showed a good treatment response, with 20.0% of patients achieving pCR. Moreover, pre- and post-CRT CEA levels ≥ 5 ng/mL were independently associated with a good response. Patients without changes in CEA levels (pre- and post-CRT CEA > 5 ng/mL) after CRT showed a lower ratio of down-staging and poor results in terms of TRG.
Serum CEA is a well-known prognostic factor and has been used as a surveillance marker for colorectal cancer[15-17]. Several studies have shown that patients with rectal cancer with positive preoperative CEA levels (> 5 ng/mL) have poor outcomes, thereby indicating the prognostic significance of serum CEA for colorectal cancer[18-20]. Moreover, other studies have reported that the post-CRT serum CEA is related to and is a predictive factor for treatment response[17-19]. Preoperative CRT has been established as a standard treatment for LARC. However, treatment response to CRT varies from clinical complete response to resistance or progression. An individualized treatment strategy based on treatment response to CRT may be helpful to optimize outcomes for patients with LARC. Thus, prognostic factors to predict treatment response are needed.
Several studies have reported predictors of treatment response to preoperative CRT for LARC. Restivo et al[7] suggested that pretreatment CEA levels and tumor distance from the AV were predictors of treatment response to CRT for rectal cancer. Huh et al[8] reported that pretreatment CEA levels, tumor circumferentiality, and macroscopic ulceration on rigid sigmoidoscopy were clinical parameters for pCR, and they proposed a prediction model that used these three risk factors. However, evaluating the treatment response to CRT using sigmoidoscopy would be difficult and may yield inaccurate results, particularly with regard to post-radiation effects, because of the fibrosis and edema that develop after CRT. Habr-Gamma advocated a “watch and wait” policy for complete clinical response after CRT, but she also reported that follow-up for evaluating treatment for response is difficult[21]. Others showed the relationship between pretreatment systemic inflammation and pathologic response after CRT for rectal cancer[12,22]. Heo et al[23] reported that blood lymphocyte count was a useful predictive marker for pCR in LARC.
Our study identified clinical factors that were associated with pCR and good response after preoperative CRT for rectal cancer. Pre-CRT CEA levels were an apparent predictive marker for pCR, and this result is consistent with previous research that identified preoperative CEA as a prognostic factor associated with treatment response to CRT for rectal cancer[9,10,24]. In the multivariate analysis, the pretreatment CEA level was an important factor for pCR, and the post-treatment CEA level was a significant factor for good response. We focused on the difference in the pre- and post-CRT serum CEA levels, because a post-treatment CEA level ≤ 5 ng/mL could indicate good response among patients with a pretreatment CEA level > 5 ng/mL. Thus, we compared treatment response to CRT between those with pre- and post-treatment CEA > 5 ng/mL (Group A); pre- and post-treatment CEA > 5 and ≤ 5 ng/mL, respectively (Group B), and pre- and post-treatment CEA ≤ 5 ng/mL (Group C). Groups B and C showed good response. Although patients with pretreatment CEA > 5 ng/mL did not achieve pCR regardless of the post-CRT changes in CEA, our results showed that post-CRT CEA was associated with good response on multivariate analysis.
Furthermore, we identified other clinical factors, such as pretreatment tumor size, down-staging on MRI, and pre- and post-treatment NLR and PLR, that were associated with treatment response. The tumor distance from the AV did not show any correlation to treatment response. Only pretreatment NLR correlated with complete or good response to CRT on multivariate analysis.
As previously described, treatment response to CRT for LARC varies, with ≥ 40% of patients achieving partial response, 8%–20% of patients achieving pCR after surgery, and ≥ 20% of patients being resistant to treatment or developing progressive disease[5,6,25]. Achieving pCR is important because it is associated with DFS and distant metastasis[26]. Thus, several recent studies attempted to identify markers, including clinical factors, pathological features, imaging findings, and molecular biomarkers, associated with treatment response to CRT for rectal cancer. Moreover, gene expression profiles[27-29], proteins, microRNAs, and other biomarkers, such as tumor-infiltrating lymphocytes and immune checkpoint molecules, have been investigated. Kundel et al[27] reported the expression of EGFR in pretreatment biopsies between TRG groups (TRG 1 vs 3; P = 0.003, TRG 1 vs TRG 4; P = 0.033) were significantly different. Kamran et al[28] demonstrated KRAS/TP53 mutation was associated with non-response and Sendoya et al[29] also found similar result which RAS/TP53 were associated with poor outcome in prospective study. Akiyoshi et al[30] showed pretreatment neoantigen-specific CD8+ T cell is a key event in CRT response and immune check point can be useful target to enhance tumor regression. However, these studies were usually conducted in small cohorts and retrospective. Therefore, further investigation in a large cohort study is needed for validation. Molecular biomarkers are expected to have sufficient sensitivity and specificity, but none have yet been applied in clinical settings. In addition, cost-effectiveness is an important consideration.
An individualized treatment strategy based on sensitivity or resistance to preoperative CRT for LARC is needed. Understanding the relationship between each marker and treatment response can help achieve better patient outcomes. Serum CEA levels can be easily measured before and after CRT as part of the routine evaluation. However, a single assessment for CEA is insufficient to predict treatment response to CRT. Variations in prognosis may be observed if patients are classified according to changes in serum CEA levels from before to after CRT. The early identification of poor responders or patients with tumor resistance to CRT will allow clinicians to provide more aggressive treatment, such as intensified chemotherapy.
This study has several limitations. Our results were based on 135 patients from a single institution and need to be validated in larger cohorts and multicenter studies. Another limitation was the appropriate timing of pre- and post-CRT measurement of serum CEA levels. The pretreatment serum CEA levels were first measured at the time of the first patient visit to the study center. However, the interval between the measurement of CEA levels and time to CRT commencement can vary because some patients postpone the CRT schedule because of personal reasons. In addition, post-treatment CEA levels can be followed up differently, from 4 to 5 wk after CRT, depending on the clinician’s preference. Therefore, a clear standard interval needs to be defined between the measurement of serum CEA levels and CRT administration.
Pretreatment clinical factors such as lymphocyte counts and pre- and post-treatment CEA levels, are important markers in the prediction of treatment response to CRT for LARC. The change in serum CEA levels from before to after CRT, in addition with the pre- and post-treatment CEA levels, can be used to the predict treatment response to CRT for LARC. These clinical factors may facilitate individualized treatment strategies for LARC.
Preoperative chemoradiotherapy (CRT) is a standard treatment modality for locally advanced rectal cancer. Although advances in CRT and surgical treatment have helped achieve better outcomes for rectal cancer, the overall survival of patients remains an issue. Moreover, the response to CRT varies from pathologic complete response to disease progression. As preoperative CRT is a time-consuming modality, it is important to determine the predictive factors for treatment response to preoperative CRT.
Carcinoembryonic antigen (CEA) has been reported to be an important surveillance biomarker for colorectal cancer. Although various biomolecular or immune-molecular markers have been recently introduced, they are unable to show sufficiency for clinical application or cost-effectiveness. If we can prove the relationship between changes in CEA levels before and after chemoradiotherapy and the response to CRT for rectal cancer, we can provide personalized treatment for each patient with rectal cancer to ensure a better prognosis.
This study aimed to identify patients with locally advanced rectal cancer eligible for preoperative CRT according to changes in CEA levels before and after preoperative CRT.
We included 145 patients with locally advanced rectal cancer who underwent preoperative CRT and curative resection. Patients were assigned to three groups according to pre- and post-CRT serum CEA levels: both > 5; pre > 5 and post ≤ 5; and both ≤ 5 ng/mL, respectively. We compared the response to CRT depending on changes in serum CEA levels between the groups. Multivariate logistic regression analysis was used to evaluate the prognostic factors for pathologic complete response/good response.
There were 27, 43, and 65 patients in groups A, B, and C, respectively, according to changes in serum CEA levels before and after CRT. Pre-CRT (P < 0.001) and post-CRT (P < 0.001) CEA levels and the ratio of down-staging (P = 0.013) were higher in Groups B and C than in Group A. The ratio of pathologic tumor regression grade 0/1 significantly differed among the groups (P = 0.003). Group C had the highest number of patients showing pathologic complete response (pCR; P < 0.001). Most patients with pCR showed pre- and post-CRT CEA levels of < 5 ng/mL (P < 0.001, P = 0.008). Pre- and post-CRT CEA levels were important risk factors for pCR (odds ratio 18.71; 95% confidence interval 4.62–129.51, P < 0.001) and good response (odds ratio 5.07; 95% confidence interval 1.92–14.83, P = 0.002). Pre-CRT neutrophil-to-lymphocyte ratio and post-CRT T ≥ 3 stage were also prognostic factors for pCR or good response.
Pre- and post-CRT CEA levels as well as changes in CEA levels were prognostic markers for the response to CRT and may facilitate treatment individualization for rectal cancer.
Pretreatment clinical factors such as lymphocyte counts and pre- and post-treatment CEA levels are important markers that predict the response to CRT for locally advanced rectal cancer. These clinical factors may facilitate the development of individualized treatment strategies for advanced rectal cancer.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Watanabe T S-Editor: Zhang L L-Editor: A P-Editor: Liu JH
| 1. | Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF, Karstens JH, Liersch T, Schmidberger H, Raab R; German Rectal Cancer Study Group. Preoperative vs postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351:1731-1740. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4342] [Cited by in F6Publishing: 4238] [Article Influence: 211.9] [Reference Citation Analysis (1)] |
| 2. | Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, Daban A, Bardet E, Beny A, Ollier JC; EORTC Radiotherapy Group Trial 22921. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006;355:1114-1123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1993] [Cited by in F6Publishing: 1947] [Article Influence: 108.2] [Reference Citation Analysis (0)] |
| 3. | Gérard JP, Conroy T, Bonnetain F, Bouché O, Chapet O, Closon-Dejardin MT, Untereiner M, Leduc B, Francois E, Maurel J, Seitz JF, Buecher B, Mackiewicz R, Ducreux M, Bedenne L. Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3-4 rectal cancers: results of FFCD 9203. J Clin Oncol. 2006;24:4620-4625. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1251] [Cited by in F6Publishing: 1224] [Article Influence: 68.0] [Reference Citation Analysis (0)] |
| 4. | Dayde D, Tanaka I, Jain R, Tai MC, Taguchi A. Predictive and Prognostic Molecular Biomarkers for Response to Neoadjuvant Chemoradiation in Rectal Cancer. Int J Mol Sci. 2017;18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 5. | Collette L, Bosset JF, den Dulk M, Nguyen F, Mineur L, Maingon P, Radosevic-Jelic L, Piérart M, Calais G; European Organisation for Research and Treatment of Cancer Radiation Oncology Group. Patients with curative resection of cT3-4 rectal cancer after preoperative radiotherapy or radiochemotherapy: does anybody benefit from adjuvant fluorouracil-based chemotherapy? J Clin Oncol. 2007;25:4379-4386. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 330] [Cited by in F6Publishing: 322] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 6. | Park IJ, You YN, Agarwal A, Skibber JM, Rodriguez-Bigas MA, Eng C, Feig BW, Das P, Krishnan S, Crane CH, Hu CY, Chang GJ. Neoadjuvant treatment response as an early response indicator for patients with rectal cancer. J Clin Oncol. 2012;30:1770-1776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 325] [Cited by in F6Publishing: 360] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 7. | Restivo A, Zorcolo L, Cocco IM, Manunza R, Margiani C, Marongiu L, Casula G. Elevated CEA levels and low distance of the tumor from the anal verge are predictors of incomplete response to chemoradiation in patients with rectal cancer. Ann Surg Oncol. 2013;20:864-871. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Huh JW, Kim HR, Kim YJ. Clinical prediction of pathological complete response after preoperative chemoradiotherapy for rectal cancer. Dis Colon Rectum. 2013;56:698-703. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 9. | Wallin U, Rothenberger D, Lowry A, Luepker R, Mellgren A. CEA - a predictor for pathologic complete response after neoadjuvant therapy for rectal cancer. Dis Colon Rectum. 2013;56:859-868. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 82] [Article Influence: 7.5] [Reference Citation Analysis (1)] |
| 10. | Kleiman A, Al-Khamis A, Farsi A, Kezouh A, Vuong T, Gordon PH, Vasilevsky CA, Morin N, Faria J, Ghitulescu G, Boutros M. Normalization of CEA Levels Post-Neoadjuvant Therapy is a Strong Predictor of Pathologic Complete Response in Rectal Cancer. J Gastrointest Surg. 2015;19:1106-1112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Hu H, Huang J, Lan P, Wang L, Huang M, Wang J, Deng Y. CEA clearance pattern as a predictor of tumor response to neoadjuvant treatment in rectal cancer: a post-hoc analysis of FOWARC trial. BMC Cancer. 2018;18:1145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Yamamoto A, Toiyama Y, Okugawa Y, Oki S, Ide S, Saigusa S, Araki T, Kusunoki M. Clinical Implications of Pretreatment: Lymphocyte-to-Monocyte Ratio in Patients With Rectal Cancer Receiving Preoperative Chemoradiotherapy. Dis Colon Rectum. 2019;62:171-180. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Ryan R, Gibbons D, Hyland JM, Treanor D, White A, Mulcahy HE, O'Donoghue DP, Moriarty M, Fennelly D, Sheahan K. Pathological response following long-course neoadjuvant chemoradiotherapy for locally advanced rectal cancer. Histopathology. 2005;47:141-146. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 395] [Cited by in F6Publishing: 434] [Article Influence: 22.8] [Reference Citation Analysis (1)] |
| 14. | Kim SH, Chang HJ, Kim DY, Park JW, Baek JY, Kim SY, Park SC, Oh JH, Yu A, Nam BH. What Is the Ideal Tumor Regression Grading System in Rectal Cancer Patients after Preoperative Chemoradiotherapy? Cancer Res Treat. 2016;48:998-1009. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 15. | Gold P, Freedman SO. Specific carcinoembryonic antigens of the human digestive system. J Exp Med. 1965;122:467-481. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1291] [Cited by in F6Publishing: 1250] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 16. | Locker GY, Hamilton S, Harris J, Jessup JM, Kemeny N, Macdonald JS, Somerfield MR, Hayes DF, Bast RC Jr; ASCO. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol. 2006;24:5313-5327. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1057] [Cited by in F6Publishing: 1042] [Article Influence: 57.9] [Reference Citation Analysis (0)] |
| 17. | Labianca R, Nordlinger B, Beretta GD, Brouquet A, Cervantes A; ESMO Guidelines Working Group. Primary colon cancer: ESMO Clinical Practice Guidelines for diagnosis, adjuvant treatment and follow-up. Ann Oncol. 2010;21 Suppl 5:v70-v77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 217] [Cited by in F6Publishing: 235] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 18. | Park YA, Lee KY, Kim NK, Baik SH, Sohn SK, Cho CW. Prognostic effect of perioperative change of serum carcinoembryonic antigen level: a useful tool for detection of systemic recurrence in rectal cancer. Ann Surg Oncol. 2006;13:645-650. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 71] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Wang JY, Lu CY, Chu KS, Ma CJ, Wu DC, Tsai HL, Yu FJ, Hsieh JS. Prognostic significance of pre- and postoperative serum carcinoembryonic antigen levels in patients with colorectal cancer. Eur Surg Res. 2007;39:245-250. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Park IJ, Choi GS, Lim KH, Kang BM, Jun SH. Serum carcinoembryonic antigen monitoring after curative resection for colorectal cancer: clinical significance of the preoperative level. Ann Surg Oncol. 2009;16:3087-3093. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 100] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 21. | Habr-Gama A, Perez RO, Wynn G, Marks J, Kessler H, Gama-Rodrigues J. Complete clinical response after neoadjuvant chemoradiation therapy for distal rectal cancer: characterization of clinical and endoscopic findings for standardization. Dis Colon Rectum. 2010;53:1692-1698. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 274] [Cited by in F6Publishing: 285] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 22. | Dreyer SB, Powell AG, McSorley ST, Waterston A, Going JJ, Edwards J, McMillan DC, Horgan PG. The Pretreatment Systemic Inflammatory Response is an Important Determinant of Poor Pathologic Response for Patients Undergoing Neoadjuvant Therapy for Rectal Cancer. Ann Surg Oncol. 2017;24:1295-1303. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 23. | Heo J, Chun M, Noh OK, Oh YT, Suh KW, Park JE, Cho O. Sustaining Blood Lymphocyte Count during Preoperative Chemoradiotherapy as a Predictive Marker for Pathologic Complete Response in Locally Advanced Rectal Cancer. Cancer Res Treat. 2016;48:232-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Perez RO, São Julião GP, Habr-Gama A, Kiss D, Proscurshim I, Campos FG, Gama-Rodrigues JJ, Cecconello I. The role of carcinoembriogenic antigen in predicting response and survival to neoadjuvant chemoradiotherapy for distal rectal cancer. Dis Colon Rectum. 2009;52:1137-1143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 93] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 25. | Ryan JE, Warrier SK, Lynch AC, Heriot AG. Assessing pathological complete response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer: a systematic review. Colorectal Dis. 2015;17:849-861. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 73] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 26. | Fokas E, Liersch T, Fietkau R, Hohenberger W, Beissbarth T, Hess C, Becker H, Ghadimi M, Mrak K, Merkel S, Raab HR, Sauer R, Wittekind C, Rödel C. Tumor regression grading after preoperative chemoradiotherapy for locally advanced rectal carcinoma revisited: updated results of the CAO/ARO/AIO-94 trial. J Clin Oncol. 2014;32:1554-1562. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 256] [Cited by in F6Publishing: 284] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 27. | Kundel Y, Nasser NJ, Rath-Wolfson L, Purim O, Yanichkin N, Brenner R, Zehavi T, Nardi Y, Fenig E, Sulkes A, Brenner B. Molecular Predictors of Response to Neoadjuvant Chemoradiation for Rectal Cancer. Am J Clin Oncol. 2018;41:613-618. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Kamran SC, Lennerz JK, Margolis CA, Liu D, Reardon B, Wankowicz SA, Van Seventer EE, Tracy A, Wo JY, Carter SL, Willers H, Corcoran RB, Hong TS, Van Allen EM. Integrative Molecular Characterization of Resistance to Neoadjuvant Chemoradiation in Rectal Cancer. Clin Cancer Res. 2019;25:5561-5571. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 29. | Sendoya JM, Iseas S, Coraglio M, Golubicki M, Robbio J, Salanova R, Kujaruk M, Mikolaitis V, Rizzolo M, Ruiz G, Cabanne A, Gualdrini U, Mendez G, Hirmas S, Rotondaro C, Viglino J, Eleta M, Fernandez E, Abba M, Podhajcer O, Roca E, Llera AS. Pre-Existing Tumoral B cell Infiltration and Impaired Genome Maintenance Correlate with Response to Chemoradiotherapy in Locally Advanced Rectal Cancer. Cancers (Basel). 2020;12 . [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Akiyoshi T, Tanaka N, Kiyotani K, Gotoh O, Yamamoto N, Oba K, Fukunaga Y, Ueno M, Mori S. Immunogenomic profiles associated with response to neoadjuvant chemoradiotherapy in patients with rectal cancer. Br J Surg. 2019;106:1381-1392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |