Published online Sep 21, 2017. doi: 10.3748/wjg.v23.i35.6534
First decision: February 21, 2017
Revised: June 1, 2017
Accepted: July 12, 2017
Article in press: July 12, 2017
Published online: September 21, 2017
Processing time: 213 Days and 14.2 Hours
A 27-year-old man with recurrent right lower quadrant pain was admitted to our hospital. Ultrasonography and computed tomography examination of the abdomen revealed a target sign in the ascending colon, which was compatible with the diagnosis of cecal intussusception. The intussusception was spontaneously resolved at that time, but it relapsed 6 mo later. The patient underwent a successful colonoscopic disinvagination; there was no evidence of neoplastic or inflammatory lesions in the colon and terminal ileum. The patient underwent laparoscopic surgery for recurring cecal intussusception. During laparoscopy, we observed an unfixed cecum on the posterior peritoneum (i.e. a mobile cecum). Thus, we performed laparoscopic appendectomy and cecopexy with a lateral peritoneal flap using a barbed wound suture device. The patient’s post-operative course was uneventful, and he continued to do well without recurrence at 10 mo after surgery. Laparoscopic cecopexy using a barbed wound suture device is a simple and reliable procedure that can be the treatment of choice for recurrent cecal intussusception associated with a mobile cecum.
Core tip: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
- Citation: Yamamoto T, Tajima Y, Hyakudomi R, Hirayama T, Taniura T, Ishitobi K, Hirahara N. Case of colonic intussusception secondary to mobile cecum syndrome repaired by laparoscopic cecopexy using a barbed wound suture device. World J Gastroenterol 2017; 23(35): 6534-6539
- URL: https://www.wjgnet.com/1007-9327/full/v23/i35/6534.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i35.6534
Mobile cecum syndrome is characterized by chronic right lower quadrant pain without evidence of appendicitis or other etiological factors. Although abnormal mobility of the cecum and ascending colon has been estimated to occur in 10%-20% of the population, intussusception or volvulus of the cecum secondary to a mobile cecum is uncommon[1,2]. Approximately one-third of the intussusceptions of the intestinal tract occur as a result of surgery-induced changes, such as adhesion, submucosal edema, and intestinal motility disorders; colonic intussusceptions in adults are usually caused by malignant or benign tumors[3]. Therefore, surgical interventions, such as intestinal resection through either an open or laparoscopic approach, have been performed for the majority of adult patients with colonic intussusception[4]. We describe herein a rare case of colonic intussusception secondary to mobile cecum syndrome, which was successfully treated with laparoscopic cecopexy using a barbed wound suture device.
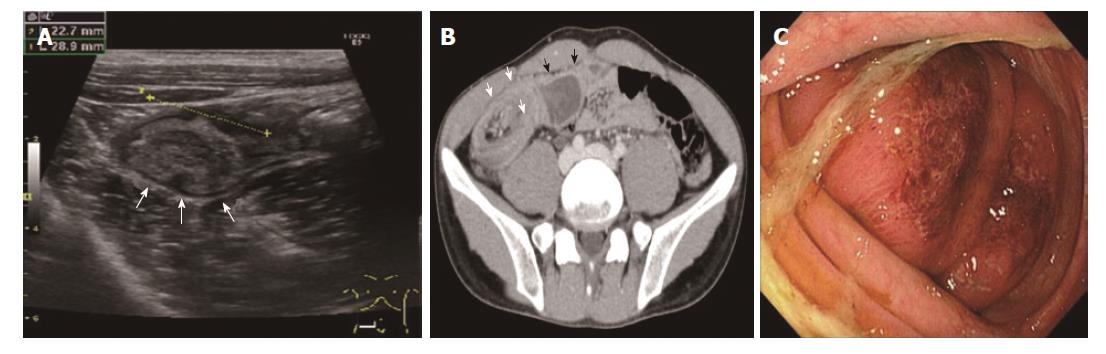
A 27-year-old man with recurring abdominal pain in the right lower quadrant was re-admitted to our hospital. The patient had a 3-year history of mild ulcerative colitis, but he had been free from abdominal symptoms and continued to do well without medications. On admission, abdominal ultrasonography (Figure 1A) and contrast-enhanced computed tomography (CT) (Figure 1B) showed a target sign in the ascending colon with dilatation of the cecum and ileum, which was compatible with the diagnosis of cecal intussusception. The patient had no previous surgical history, and there was no evidence of intraabdominal tumors or inflammatory conditions in these imaging evaluations. Thereafter, the intussusception spontaneously resolved.
The patient was discharged a few days after admission, but the abdominal pain recurred 6 mo later. Abdominal CT scan again revealed cecal intussusception. An emergency colonoscopy was performed to reduce the intussusception, in which the cecum had advanced into the ascending colon. An edematous colonic mucosa restricted to the lead point of intussusception was identified (Figure 1C). No other inflammatory changes or neoplastic lesions were detected in the colon and terminal ileum, even after reduction of the intussusception. The patient was thus diagnosed with recurrent cecal intussusception that was likely due to a mobile cecum, and underwent an elective laparoscopic surgery.
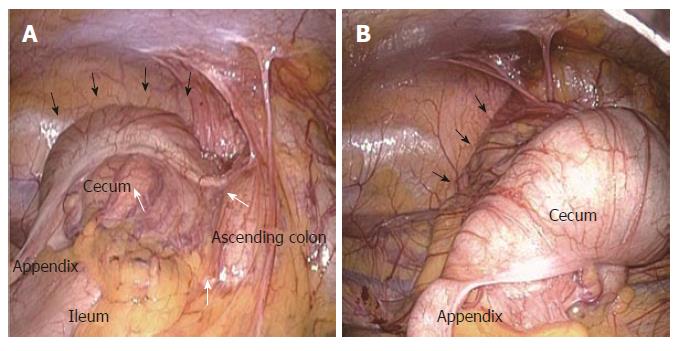
The patient was placed in the supine position under general anesthesia. A 20-mm long skin incision was made on the umbilicus, and a 12-mm trocar was inserted. After creating a pneumoperitoneum with carbon dioxide at an intra-abdominal pressure of 10 mmHg, additional 5-mm and 12-mm trocars were placed at the left upper quadrant and the middle of the lower abdomen, respectively. Upon laparoscopy, no evidence of ischemia, inflammation, or caliber change in the gastrointestinal tract, including the cecum, appendix and terminal ileum, was found. A linear indentation running along the minor axis of the large bowel was identified in the middle portion of the ascending colon, which left a trace of intussusception (Figure 2A). The cecum was easily mobilized from the right lower quadrant to the upper abdominal cavity, as it was not fixed to the posterior parietal peritoneum (Figure 2B).
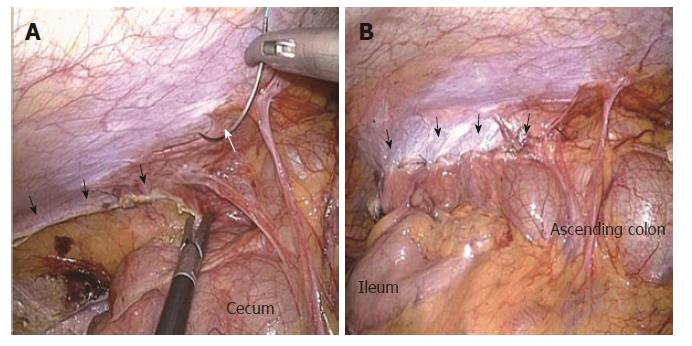
The findings confirmed that the recurrent cecal intussusception was associated with an abnormal fixation of the cecum and ascending colon to the parietal peritoneum (i.e. a mobile cecum). Laparoscopic appendectomy and cecopexy were performed. After the appendectomy, an approximately 10-cm long incision was made in the right parietal peritoneum along the ascending colon for the cecopexy (Figure 3A); then, the cecum and ascending colon were fixed to the incision line of the parietal peritoneum with a continuous suture technique, using an absorbable barbed wound suture device (V-Loc™ 180; Medtronic, Tokyo, Japan) (Figure 3B). The operation time was 87 min, with less than 10 g of blood loss. The patient’s postoperative course was uneventful, and he was discharged 4 d after surgery. The patient continued to do well without recurrence at 10 mo after surgery.
Intestinal intussusception is the leading cause of gastrointestinal obstruction in children. However, it is rarely encountered in adults, accounting for 1%-5% of all cases of intestinal obstruction[5]. Although the exact mechanism of bowel intussusception remains unclear, one leading theory is that intestinal motility disorder due to intraluminal lesions or inflammation induces invagination[6,7]. The common site of intussusception is the junction between the free intestine and the portion fixed to the retroperitoneum or at postoperative adhesions[7,8]. Non-malignant lesions, such as benign or inflammatory neoplasms, Meckel’s diverticulum and appendix, are the most common cause of intussusception in the small bowel, with only 30% of cases due to malignant neoplasms[6,9]. In contrast, malignant lesions are responsible for most cases of colonic intussusceptions[7,10].
In the present case, neither malignant or benign tumors nor inflammatory conditions were identified upon colonoscopic, ultrasonographic and CT examinations. Laparoscopically, other than the unfixed cecum and ascending colon on the posterior peritoneum, no notable finding (e.g., abdominal adhesions or mesenteric lymph node swelling) was observed, thereby indicating that the cecal intussusception occurred secondary to the mobile cecum in our patient.
Mobile cecum is not uncommon, with up to 25% to 64% of cadavers exhibiting a mobile cecum. Nevertheless, colonic intussusception related to mobile cecum is rare in adults[11,12]. We performed a review of the literature from 1995 to 2016 using the PubMed database with the search terms “intussusception,” “mobile cecum” and “adult,” which yielded only 4 cases of colonic intussusception associated with mobile cecum[13-16]. Moreover, all of these cases had some lead lesions as a cause of intussusception, such as villous adenoma and submucosal lipoma in the cecum or ileocecal valve (Table 1).
| Ref. | Age | Sex | Clinical symptoms | Repeated symptoms | Episode duration | Diagnostic modalities | Characteristic finding | Etiology of intussusception/ location | Operative procedure |
| Hamdi et al[16] | 85 | F | Abdominal pain, diarrhea | Yes | 3 mo | Barium enema, CT | Target mass | Tumor /cecum | Resection |
| Drnovsek et al[15] | 65 | M | Abdominal pain, rectal bleeding | No | 12 h | CT | Target sign | Tubulovillous adenoma /cecum | Right hemicolectomy |
| Kuzmich et al[14] | 62 | M | Abdominal pain, weight loss | Yes | 2 mo | US | Target sign | Submucosal lipoma /ileocecal valve | Right hemicolectomy |
| Frydman et al[13] | 22 | F | Rectal prolapse | No | 1 d | CT | Target sign | Villous adenoma /cecum | Right hemicolectomy |
| Present case | 27 | M | Right lower quadrant pain | Yes | 7 mo | US, CT | Target sign | None | Laparoscopic cecopexy |
Meanwhile, our case showed no evidence of neoplastic lesions or inflammatory conditions in the colon and terminal ileum, except edematous colonic mucosa identified at the lead point of intussusception. In terms of the cause of intussusception, our patient represented a rare case of colonic intussusception associated with a mobile cecum. The mucosal edema identified on the lead point of intussusception might be a cause or an effect of the intussusception in our patient. It is undeniable that the mucosal edema might have been induced by ulcerative colitis because the patient had a history of mild ulcerative colitis; however, he had been free from ulcerative colitis-related specific symptoms and required no medications for the treatment.
The presenting symptoms of colonic intussusception are nonspecific, such as abdominal pain, nausea and emesis, and a definitive diagnosis can be made only in 33% of patients prior to surgery[17]. The typical target sign or a sausage-shaped mass on a CT scan is used to confirm the diagnosis of intussusception[17,18]. In our patient, cecal intussusception was diagnosed on the basis of the target sign on abdominal ultrasonography and CT examination. Ultrasonography is a noninvasive and readily available imaging modality and easy to perform in routine clinical practice, thus, it was useful in the diagnostic workup of colonic intussusception in our patient.
In the treatment of colonic intussusception, co-lonoscopic reduction is worth considering because it is less invasive than surgery, although its efficacy remains controversial[9]. In adult patients, surgical resection is generally required because most cases have intraluminal neoplasms as a cause of intussusception[3,7,19]. In the present case, we performed an elective laparoscopic cecopexy after endoscopic reduction of cecal in-tussusception because the patient had neither intraluminal lesions nor mesenteric lymphadenopathy.
Cecopexy or right hemicolectomy can be performed to treat mobile cecum syndrome with abdominal symptoms. Some studies have recommended only colectomy because there is a possibility of recurrence of the abdominal pain due to volvulus or intussusception after performing a cecopexy[20,21]. Meanwhile, other reports have described cecopexy as a good treatment option for patients with a mobile cecum, which is associated with a low rate of disease and symptom recurrence[22,23]. Given the absence of any recurrence in our case, laparoscopic cecopexy seems to be a useful treatment of choice for cecal intussusception secondary to mobile cecum without neoplastic lesions.
Open and laparoscopic surgery can be performed for mobile cecum syndrome, and the benefits of laparoscopic surgery, in terms of cosmetic outcomes and less invasiveness, have been reported[24,25]. In the present case, we performed an elective laparoscopic cecopexy after colonoscopic reduction of cecal intussusception because the patient was generally stable and had no neoplastic lesions that could have possibly caused cecal intussusception. In addition, a barbed wound suture device was used to fix the cecum to the posterior peritoneum. Previous studies have reported various benefits of using barbed sutures, including knotless suturing, shorter stitching time and increased convenience for the surgeon[26,27]. In our case, a barbed suture device was useful for laparoscopic cecopexy, as it was easy to handle and resulted in a shorter operation time.
Laparoscopic cecopexy is a useful strategy to treat colonic intussusception secondary to a mobile cecum without any other pathologic disorders. A barbed suture device is also useful in performing a laparoscopic cecopexy in terms of its ease in handling and shorter stitching time.
A 27-year-old man with recurring abdominal pain in the right lower quadrant.
The patient’s abdomen was slightly distended and hard. Tenderness of the right lower quadrant was detected with a palpable mass when intussusception occurred.
Cecal volvulus or intra-abdominal tumors.
Laboratory data were within normal limits.
Abdominal ultrasonography and computed tomography scan showed a target sign in the ascending colon with dilatation of the cecum and ileum, which was compatible with the diagnosis of cecal intussusception.
There was no evidence of malignancy or any other inflammatory disease.
Laparoscopic cecopexy using a barbed wound suture device.
Past studies have recommended only colectomy to treat the mobile cecum, given the high rate of recurrence after cecopexy. Recently, some case reports have described a cosmetic benefit and reduced invasiveness of cecopexy without recurrence of cecal intussusception.
A mobile cecum, which is defined as the unfixed cecum and ascending colon on the posterior peritoneum, is not uncommon. However, colonic intussusception related to mobile cecum is rare in adults.
Colonic intussusception secondary to a mobile cecum is uncommon, and the surgical procedure for treatment is controversial. In this case, we performed laparoscopic cecopexy using a barbed wound suture device. This surgical procedure produces a good cosmetic outcome, while a barbed wound suture device is useful for laparoscopic cecopexy, as it is easy to handle and results in a shorter operation time.
The paper is an interesting Case Report of colonic intussusception secondary to mobile cecum syndrome and is suitable for publication.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Tovey FI S- Editor: Qi Y L- Editor: Filipodia
E- Editor: Xu XR
| 1. | Katoh T, Shigemori T, Fukaya R, Suzuki H. Cecal volvulus: report of a case and review of Japanese literature. World J Gastroenterol. 2009;15:2547-2549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Rogers RL, Harford FJ. Mobile cecum syndrome. Dis Colon Rectum. 1984;27:399-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 45] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Agha FP. Intussusception in adults. AJR Am J Roentgenol. 1986;146:527-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 168] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | de Clerck F, Vanderstraeten E, De Vos M, Van Steenkiste C. Adult intussusception: 10-year experience in two Belgian centres. Acta Gastroenterol Belg. 2016;79:301-308. [PubMed] |
| 5. | Yakan S, Caliskan C, Makay O, Denecli AG, Korkut MA. Intussusception in adults: clinical characteristics, diagnosis and operative strategies. World J Gastroenterol. 2009;15:1985-1989. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 6. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 384] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 7. | Wang LT, Wu CC, Yu JC, Hsiao CW, Hsu CC, Jao SW. Clinical entity and treatment strategies for adult intussusceptions: 20 years’ experience. Dis Colon Rectum. 2007;50:1941-1949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 112] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Sachs M, Encke A. [Entero-enteral invagination of the small intestine in adults. A rare cause of “uncertain abdomen”]. Langenbecks Arch Chir. 1993;378:288-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Tan KY, Tan SM, Tan AG, Chen CY, Chng HC, Hoe MN. Adult intussusception: experience in Singapore. ANZ J Surg. 2003;73:1044-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Eisen LK, Cunningham JD, Aufses AH Jr. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 243] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 11. | Consorti ET, Liu TH. Diagnosis and treatment of caecal volvulus. Postgrad Med J. 2005;81:772-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 107] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 12. | Solanke TF. Intestinal obstruction in Ibadan. West Afr Med J Niger Pract. 1968;17:191-193. [PubMed] |
| 13. | Frydman J, Ben-Ishay O, Kluger Y. Total ileocolic intussusception with rectal prolapse presenting in an adult: a case report and review of the literature. World J Emerg Surg. 2013;8:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Kuzmich S, Connelly JP, Howlett DC, Kuzmich T, Basit R, Doctor C. Ileocolocolic intussusception secondary to a submucosal lipoma: an unusual cause of intermittent abdominal pain in a 62-year-old woman. J Clin Ultrasound. 2010;38:48-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Drnovsek V, Ruff MB, Riehl PA, Plavsic BM. Gastrointestinal case of the day. Chronic ileocolocolic intussusception secondary to a mobile cecum and a benign fibrovascular mass. Radiographics. 1999;19:1102-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Hamdi M, Blondio JV, Algaba R, Van Gysel JP. Adult intussusception. A case report. Acta Chir Belg. 1996;96:284-286. [PubMed] |
| 17. | Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 666] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 18. | Gayer G, Zissin R, Apter S, Papa M, Hertz M. Pictorial review: adult intussusception--a CT diagnosis. Br J Radiol. 2002;75:185-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 164] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 19. | Ajao OG. Non-infantile intussusception. J Natl Med Assoc. 1979;71:65-67. [PubMed] |
| 20. | Remes-Troche JM, Pérez-Martínez C, Rembis V, Arch Ferrer J, Ayala González M, Takahashi T. [Surgical treatment of colonic volvulus. 10-year experience at the Instituto Nacional de la Nutrición Salvador Zubirán]. Rev Gastroenterol Mex. 1997;62:276-280. [PubMed] |
| 21. | Meyers JR, Heifetz CJ, Baue AE. Cecal volvulus: a lesion requiring resection. Arch Surg. 1972;104:594-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Howard RS, Catto J. Cecal volvulus. A case for nonresectional therapy. Arch Surg. 1980;115:273-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 23. | Rabinovici R, Simansky DA, Kaplan O, Mavor E, Manny J. Cecal volvulus. Dis Colon Rectum. 1990;33:765-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 120] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Gomes CA, Soares C Jr, Catena F, Di Saverio S, Sartelli M, Gomes CC, Gomes FC. Laparoscopic Management of Mobile Cecum. JSLS. 2016;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Kakizoe S, Kakizoe Y, Kakizoe H, Kakizoe T, Kakizoe K. Experience of laparoscopic cecoplication for mobile cecum. Endoscopy. 2000;32:S4-S5. [PubMed] |
| 26. | Greenberg JA, Goldman RH. Barbed suture: a review of the technology and clinical uses in obstetrics and gynecology. Rev Obstet Gynecol. 2013;6:107-115. [PubMed] |
| 27. | Facy O, De Blasi V, Goergen M, Arru L, De Magistris L, Azagra JS. Laparoscopic gastrointestinal anastomoses using knotless barbed sutures are safe and reproducible: a single-center experience with 201 patients. Surg Endosc. 2013;27:3841-3845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |