Published online Jul 7, 2015. doi: 10.3748/wjg.v21.i25.7764
Peer-review started: December 6, 2014
First decision: December 22, 2014
Revised: January 12, 2015
Accepted: March 19, 2015
Article in press: March 19, 2015
Published online: July 7, 2015
Processing time: 215 Days and 11.9 Hours
AIM: To investigate the inhibitory effects and mechanism of high mobility group box (HMGB)1 A-box in lipopolysaccharide (LPS)-induced intestinal inflammation.
METHODS: Overexpression of HMGB1 A-box in human intestinal epithelial cell lines (SW480 cells) was achieved using the plasmid pEGFP-N1. HMGB1 A-box-overexpressing SW480 cells were stimulated with LPS and co-culturing with human monocyte-like cell lines (THP-1 cells) using a Transwell system, compared with another HMGB1 inhibitor ethyl pyruvate (EP). The mRNA and protein levels of HMGB1/toll-like receptor (TLR) 4 signaling pathways [including HMGB1, TLR4, myeloid differentiation factor88 (MYD88), Phosphorylated Nuclear Factor κB (pNF-κB) p65] in the stimulated cells were determined by real-time polymerase chain reaction and Western blotting. The levels of the proinflammatory mediators [including HMGB1, interleukin (IL)-1β, IL-6 and tumor necrosis factor (TNF)-α] in the supernatants of the stimulated cells were determined by ELISA.
RESULTS: EP downregulated the mRNA and protein levels of HMGB1, inhibited the TLR4 signaling pathways (TLR4, MYD88 and pNF-κB p65) and reduced the secretion of proinflammatory mediators (HMGB1, IL-1β, IL-6 and TNF-α) in the SW480 and THP-1 cells activated by LPS but not in the unstimulated cells. Activated by LPS, the overexpression of HMGB1 A-box in the SW480 cells also inhibited the HMGB1/TLR4 signaling pathways and reduced the secretion of these proinflammatory mediators in the THP-1 cells but not in the transfected and unstimulated cells.
CONCLUSION: HMGB1 A-box, not only EP, can reduce LPS-induced intestinal inflammation through inhibition of the HMGB1/TLR4 signaling pathways.
Core tip: We have provided the first report that high mobility group box (HMGB)1 A-box, not only ethyl pyruvate, can specifically inhibit HMGB1/toll-like receptor 4 signaling pathways and reduce lipopolysaccharide-induced intestinal inflammation. Our findings indicate the potential of the HMGB1 A-box as a novel approach in the treatment of inflammatory bowel disease.
-
Citation: Wang FC, Pei JX, Zhu J, Zhou NJ, Liu DS, Xiong HF, Liu XQ, Lin DJ, Xie Y. Overexpression of HMGB1 A-box reduced lipopolysaccharide-induced intestinal inflammation
via HMGB1/TLR4 signalingin vitro . World J Gastroenterol 2015; 21(25): 7764-7776 - URL: https://www.wjgnet.com/1007-9327/full/v21/i25/7764.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i25.7764
Inflammatory bowel disease (IBD) comprises the chronic relapsing inflammatory disorders Crohn’s disease and ulcerative colitis. IBD is thought to result from an inappropriate and continuing inflammatory response to commensal microbes in a genetically susceptible host[1]. Although the etiologies of IBD remain unclear, available evidence suggests that an abnormal immune response to microorganisms of the intestinal flora is responsible for the disease in genetically susceptible individuals. Therefore, this abnormal immune response plays a major role in the pathogenesis of IBD[2].
Intestinal epithelial cell lines constitutively express several members of a novel family of transmembrane receptors designated toll-like receptors (TLRs) that may serve as major links between the innate and adaptive mucosal immune responses. Within a susceptible individual, aberrant or dysfunctional TLR signaling may impair commensal-mucosal homeostasis, thereby contributing to the amplification and perpetuation of tissue injury, consequently leading to the chronic inflammation that occurs in IBD[3]. TLR4 is the primary receptor needed for the promotion of macrophage activation, cytokine release, and tissue damage. The presence of this receptor may indicate the anomalous regulation of innate immunity, and it contributes to the production of proinflammatory mediators and disease development[4]. TLR4 mediates the recognition of antigens in the intestinal lumen as lipopolysaccharides (LPS) due to the activation of NF-κB via myeloid differentiation factor (MYD)88, thereby increasing the production of proinflammatory cytokines, such as interleukin (IL)-1β, IL-6 and IL-8, and the susceptibility to invasion by pathogens in the lamina propria, perpetuating the inflammatory process[5]. Numerous reports have indicated that TLR4 plays a pivotal role in IBD, but the underlying mechanism remains to be elucidated.
Recent extensive studies have demonstrated that high mobility group box (HMGB)1 is a novel endogenous ligand for TLR4. HMGB1, which is an evolutionarily highly conserved and abundant nuclear protein, also functions within the cytoplasm and as an extracellular damage-associated molecular pattern (DAMP) molecule. Extracellular HMGB1 is the prototypic endogenous “danger signal” that triggers inflammation and immunity[6]. This protein is either actively secreted by monocytes/macrophages or passively released from necrotic cells from any tissue. It has recently been implicated in the pathogenesis of IBD. In IBD patients and mice with colitis, HMGB1 is secreted by inflamed intestinal tissues, and it is present at high levels in feces. The large quantities of HMGB1 in the gastrointestinal tract mediate inflammation and gastrointestinal barrier failure[7]. This protein is abundantly secreted by the inflamed intestinal tissues of pediatric patients with IBD. Once released, it behaves as a cytokine-like proinflammatory molecule by upregulating other proinflammatory mediators[8]. HMGB1 also alters intestinal epithelial cell permeability[9]. It has been implicated in the pathogenesis of diseases in which excessive inflammation plays a key role, such as IBD. Therefore, the targeting of the HMGB1/TLR4 signaling pathways may represent a novel approach for the treatment of IBD. A growing number of HMGB1 inhibitors, including neutralizing antibodies, endogenous hormones, medicinal-herb-derived small molecules and ethyl pyruvate (EP), have been developed. Studies have shown that the neutralization of HMGB1 activity by the administration of anti-HMGB1 antibodies or EP attenuates colon injury, reduces weight loss, and improves colon scores in animal models of colitis[7]. Interestingly, recent studies have shown that HMGB1 A-box alone, as a natural antagonist of HMGB1, can competitively inhibit the binding of HMGB1 to its receptors and attenuate the proinflammatory effect of the full-length HMGB1 and the B-box peptide. The A-box is thus considered to be a specific blockade for endogenous HMGB1[10,11]. However, it is unknown whether the A-box can be used to treat IBD.
To investigate the effects of two HMGB1 inhibitors (HMGB1 A-box and EP) in IBD in vitro, we assumed that the targeting of the HMGB1/TLR4 signaling pathways would reveal whether the HMGB1 A-box represents a novel approach to the treatment of IBD. Therefore, in this study, we constructed human intestinal epithelial cell lines (SW480 cells) overexpressing HMGB1 A-box using gene transfection technology, and observed changes in the HMGB1/TLR4 signaling pathways in human monocyte-like cell lines (THP-1 cells) co-cultured with SW480 cells overexpressing HMGB1 A-box that were activated by LPS. We also investigated the effects of the specific inhibition of HMGB1 A-box on the HMGB1/TLR4 signaling pathways compared with those of EP. We aimed to provide theoretical and experimental evidence of HMGB1 A-box as a potential therapeutic target for IBD.
The human intestinal epithelial cell line SW480 (ATCC NO.CCL-228) and human acute monocytic leukemia cell line THP-1 (ATCC NO.TIB-202) were obtained from the Gastroenterology Institute of Jiangxi Province. The cells were maintained in RPMI-1640 medium (HyClone, Logan, UT, United States) supplemented with 10% (v/v) fetal bovine serum (FBS) (HyClone) at 37 °C and incubated in a humidified 5% (v/v) CO2 incubator. Lipopolysaccharide (LPS) from Escherichia coli was used for the stimulation of the SW480 cells. SW480 cells were pretreated with EP (Sigma-Aldrich, St. Louis, MO, United States) for 1 h before LPS stimulation.
Overexpression of the truncated intracellular form of HMGB1 A-box in SW480 cells was achieved using the plasmid pEGFP-N1 (Generay, Shanghai, China). To eliminate endotoxin contamination, all plasmids were prepared using an Endo-free Plasmid Mini Kit II (Omega, San Carlos, CA, United States). Transient transfection was performed with FuGENE 6 Transfection Reagent (Promega, Sunnyvale, CA, United States). Overexpression of HMGB1 A-box was confirmed with dual-endonuclease digestion and sequencing.
A Transwell system was used to prevent direct contact between SW480 cells and THP-1 cells. Our Transwell culture plates (Corning, Corning, NY, United States) had six wells composed of upper and lower chambers separated by polycarbonate membrane with a pore diameter of 0.4 mm. SW480 cells were prepared in the lower chamber and pretreated with EP (Sigma-Aldrich) for 1 h before LPS stimulation. THP-1 cells were loaded into the upper chamber.
Total RNA was extracted from the cells using TRIzol reagent (Tiangen, Beijing, China). The obtained total RNA (500 ng to 1 μg) was reverse transcribed following the removal of genomic DNA using a PrimeScrip RT Reagent Kit with gDNA Eraser (Takara, Dalian, China). Quantitative polymerase chain reaction (qPCR) amplification was performed using a thermal cycler (BioRad, Richmond, VA, United States) with SYBR Premix Ex Ta (Tli RNase H Plus). A total of 2 μL of cDNA was amplified. Relative expression levels were calculated and analyzed by the 2-ΔΔCt equation. The primer sequences used were as follows:
HMGB1 A-box forward: 5’-ACCCAGATGCTTCAGTCAACTT-3’, reverse: 5’-CTCTTTCATAACGGGCCTTGT-3’; HMGB1 forward: 5’-GGAGATCCTAAGAAGCCGAGA-3’, reverse: 5’-CATGGTCTTCCACCTCTCTGA-3’; TLR4 forward: 5’-AGGACTGGGTAAGGAATGAGC-3’, reverse: 5’-ATCACCTTTCGGCTTTTATGG-3’; MYD88 forward: 5’-AAGAAAGAGTTCCCCAGCATC-3’, reverse: 5’-GCGAGTCCAGAACCAAGATTT-3’; and β-actin forward: 5’-TGACGTGGACATCCGCAAAG-3’, reverse: 5’-TGACGTGGACATCCGCAAAG-3’.
Cells were subjected to cell lysis, and the total protein was extracted as previously described[8]. Protein concentrations were measured using the BCA protein assay (Generay, Shanghai, China). Lysates were separated using SDS-PAGE and transferred to a nitrocellulose membrane. The membranes were incubated with a rabbit anti-HMGB1 antibody (ab18256, 1:1000; Abcam, Cambridge, MA, United States), mouse anti-TLR4 antibody (ab22048, 1:1000; Abcam), rabbit anti-MYD88 antibody (HFL-296) (Santa Cruz Biotechnology, Santa Cruz, CA, United States), rabbit anti-phospho-NF-κB p65 antibody (Cell Signaling Technology, Beverly, MA, United States) and rabbit anti-β-actin antibody (ab1801, 1:1000; Abcam). Goat anti-rabbit IgG-horseradish peroxidase (HRP) or donkey anti-mouse IgG-HRP (both 1:2000) served as secondary antibodies. Immunoreactive proteins were visualized, and band intensity was quantified using a ChemiDo MP System with Image La Software (BioRad, Richmond, VA, United States). The data were normalized to the β-actin levels.
The concentrations of IL-1β, IL-6, TNF-α and HMGB1 in the cell culture supernatants from the SW480 cells alone or those co-cultured with THP-1 were determined by ELISA using a commercial human multiplex kit (IL-1β, IL-6 and TNF-α) (Aushon Biosystems, Wuxi, China) or human HMGB1 kit (Uscn Life Science, Wuhan, China).
The data are expressed as the mean ± SD of three independent experiments. The data were statistically analyzed as indicated in the figure legends using GraphPad Prism version 5.0. Differences between any two groups were determined by the t test. Differences among multiple groups were determined by one-way ANOVA. P < 0.05 was considered statistically significant.
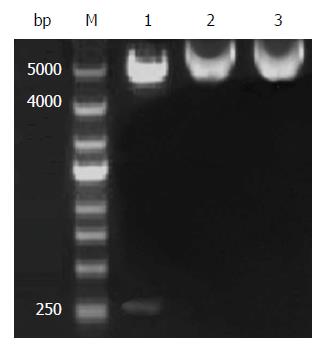
To construct the HMGB1 A-box recombinant expression plasmid and identify HMGB1 A-box, the pEGFP-N1-HMGB1 A-box recombinant plasmid was digested with XhoI and BamHI. After 2% agarose gel electrophoresis, the fragments in the agarose gel resulting from the enzymatic digestion were observed. Restriction analysis of pEGFP-N1-HMGB1 A-box is shown in Figure 1. The HMGB1 A-box fragment was 256 bp, consistent with the expected size. The inserted HMGB1 A-box fragments were consistent with published data (Gen-Bank Accession: NM_002128.4).
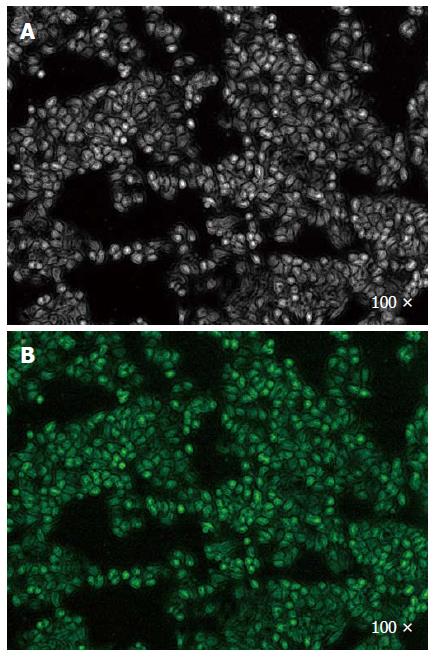
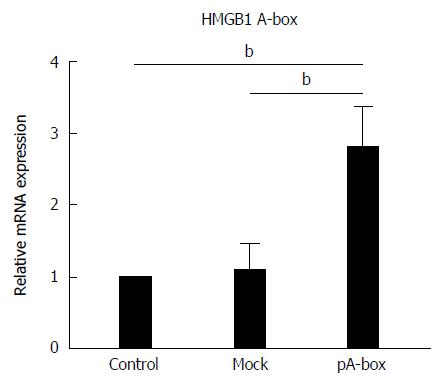
To evaluate the expression of the HMGB1 A-box recombinant eukaryotic plasmid in SW480 cells, these cells were assessed by fluorescence microscopy (Olympus IX71, Tokyo, Japan). Those transfected with the HMGB1 A-box recombinant plasmid fluoresced green, and photographs were obtained using a digital camera. Green fluorescence of the transfected cells was observed at 48 h after transfection (Figure 2). The expression of HMGB1 A-box mRNA in the pA-box-transfected SW480 cells was higher than that in the control and mock-transfection groups (bP < 0.01) (Figure 3). These results suggested that the SW480 cells were successfully transfected.
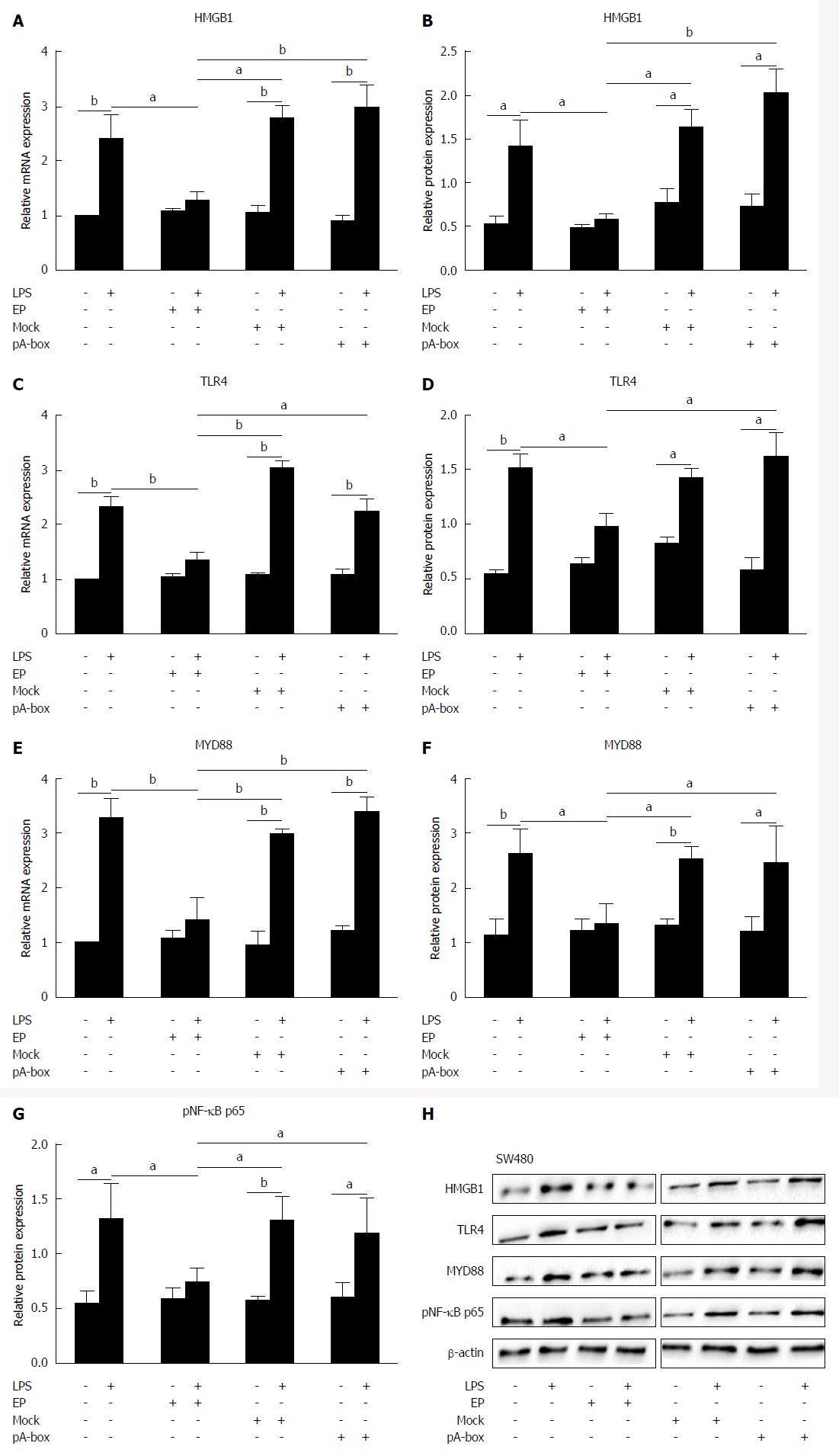
To elucidate the roles of HMGB1 and TLR4 in intestinal epithelial cells activated by LPS, we observed the effects of HMGB1 inhibitors (HMGB1 A-box and EP) on the HMGB1 and TLR4 signaling pathways in stimulated SW480 cells.
The HMGB1, TLR4, MYD88, pNF-κB p65 mRNA and protein levels in stimulated SW480 cells were determined by real-time PCR and western blotting (Figure 4A-H). There were no significant differences in the HMGB1/TLR4/MYD88/pNF-κB p65 mRNA and protein levels among the groups without the LPS treatment (P > 0.05). In the LPS-treated groups, HMGB1/TLR4/MYD88/pNF-κB p65 mRNA and protein levels in the EP group were significantly lower than those in the control group, mock-transfection group and pA-box-transfection group (aP < 0.05 and bP < 0.01), but there were no significant differences detected among the control group, mock-transfection group and pA-box-transfection group (P > 0.05). All LPS treatment groups except the EP group showed significantly higher levels of these mRNAs and proteins compared with the corresponding groups without LPS treatment (aP < 0.05, bP < 0.01).
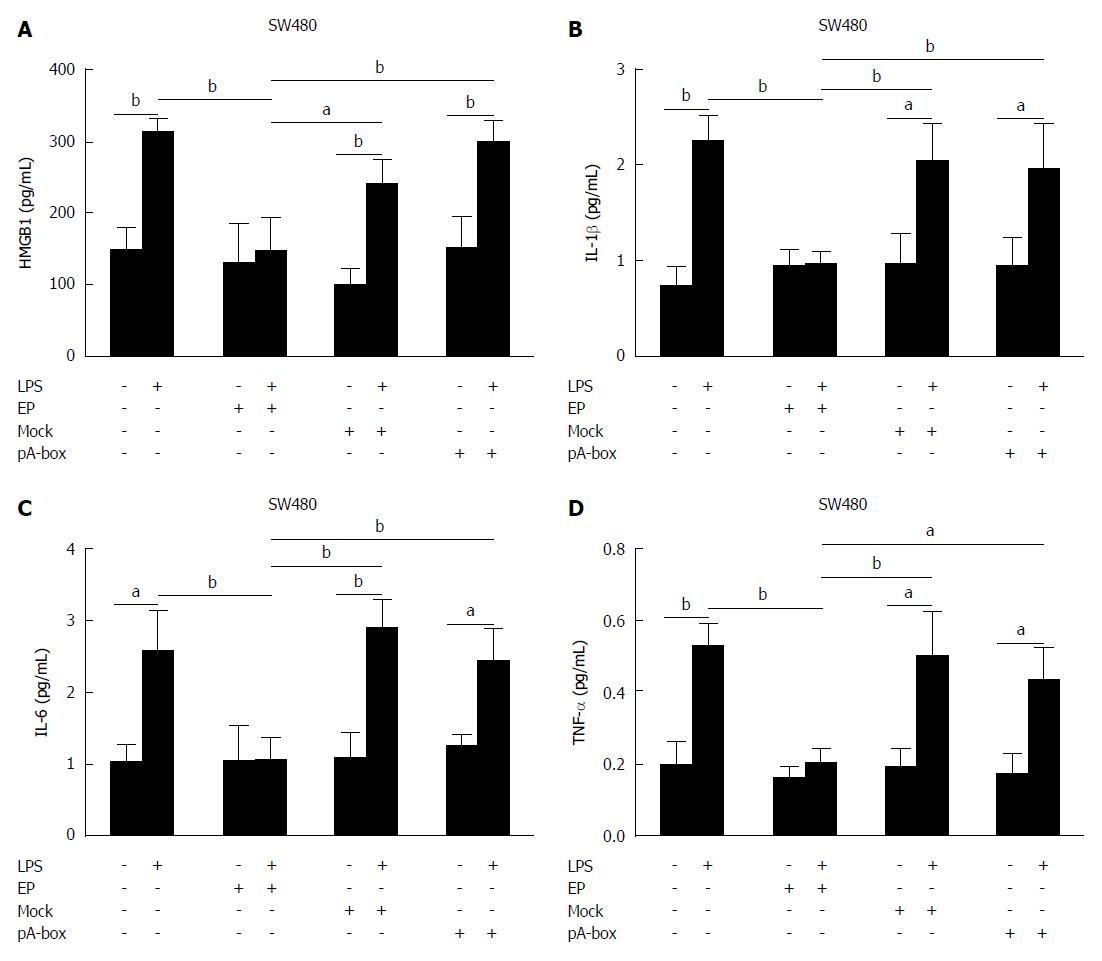
The cytokine levels of HMGB1, IL-1β, IL-6 and TNF-α in the supernatants of stimulated SW480 cells were determined by ELISA (Figure 5A-D). There were no significant differences in the levels of HMGB1, IL-1β, IL-6 and TNF-α among the groups without LPS treatment (P > 0.05). In the LPS treatment groups, the levels of HMGB1, IL-1β, IL-6 and TNF-α in the EP group were significantly lower than those in the control group, mock-transfection group and pA-box-transfection group (aP < 0.05, bP < 0.01), but there were no significant differences among the control group, mock-transfection group and pA-box-transfection group (P > 0.05). All LPS treatment groups except the EP group showed significantly higher levels of these mRNAs and proteins than the corresponding groups without the LPS treatment (aP < 0.05, bP < 0.01).
To further elucidate the roles of HMGB1 and TLR4 in IBD, we observed the effects of HMGB1 inhibitors (HMGB1 A-box and EP) on the HMGB1 and TLR4 signaling pathways in THP-1 cells co-cultured with SW480 cells.
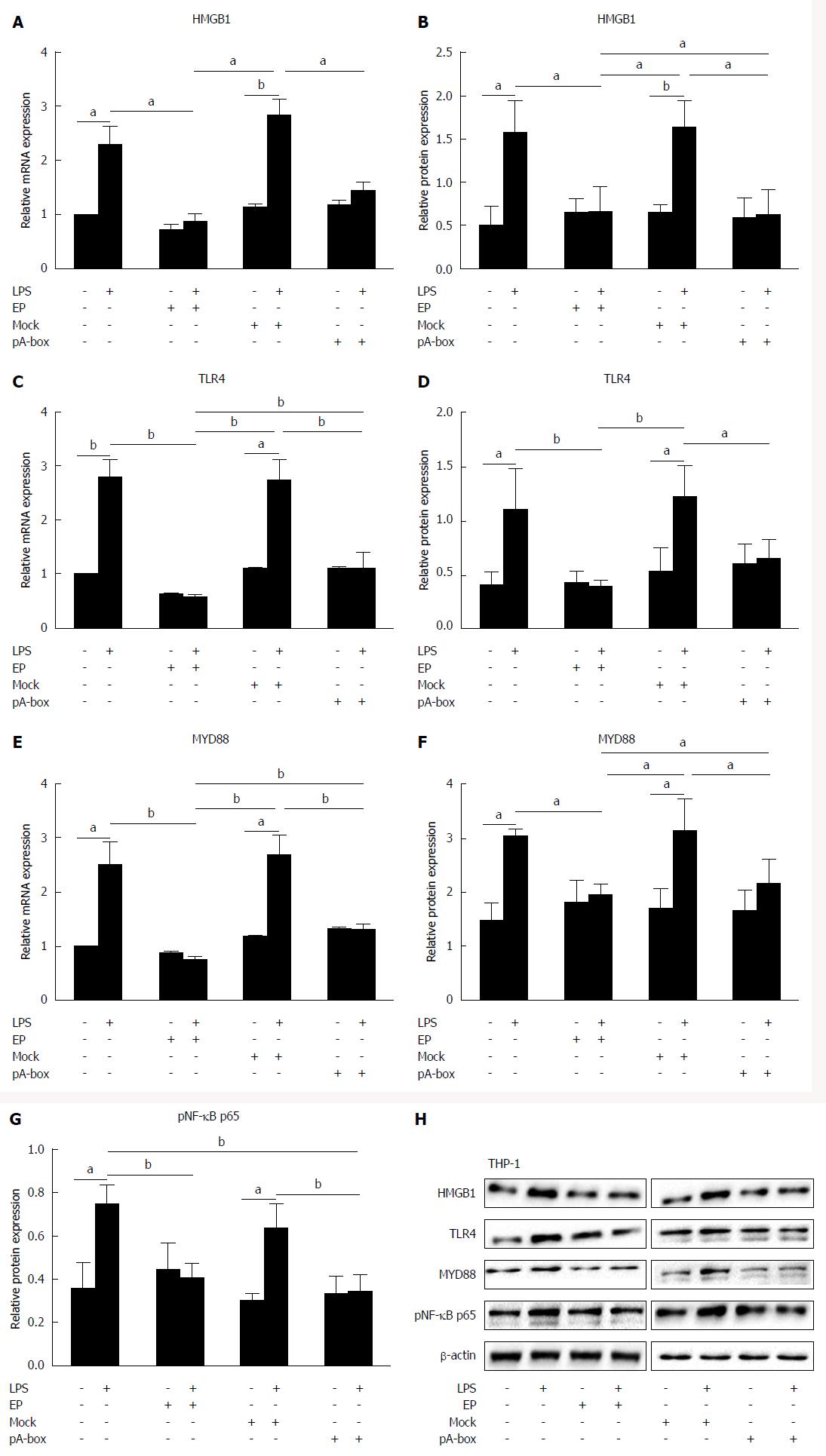
Following co-culturing with SW480 cells, the HMGB1, TLR4, MYD88, and pNF-κB p65 mRNA and protein levels in the THP-1 cells were determined by real-time PCR and western blotting (Figure 6A-H). There were no significant differences in the HMGB1/TLR4/MYD88/pNF-κB p65 mRNA and protein levels among the groups without LPS treatment (P > 0.05). In the LPS treatment groups, the HMGB1/TLR4/MYD88/pNF-κB p65 mRNA and protein levels in the EP group and pA-box-transfection group were significantly lower than those in the control group and mock-transfection group (aP < 0.05, bP < 0.01). All LPS treatment groups except the EP group and pA-box-transfection group were significantly higher than the corresponding groups without LPS treatment (aP < 0.05, bP < 0.01).
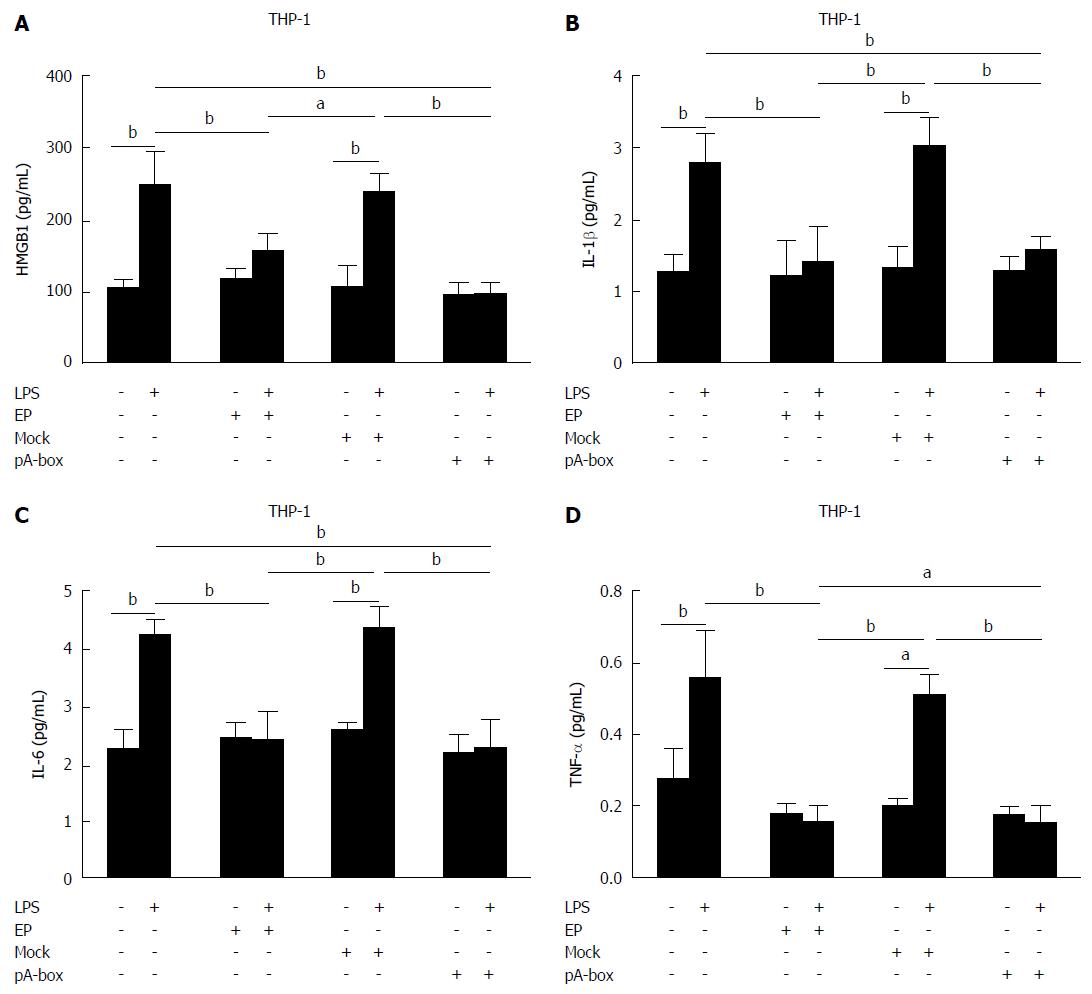
Following co-culturing with SW480 cells, the cytokine levels of HMGB1, IL-1β, TNF-α and IL-6 in the supernatants of the THP-1 cells were determined by ELISA (Figure 7A-D). There were no significant differences in the levels of HMGB1, IL-1β, TNF-α and IL-6 among the groups without LPS treatment (P > 0.05). In the LPS treatment groups, the levels of HMGB1, IL-1β, TNF-α and IL-6 in the EP and pA-box-transfection groups were significantly lower than those in the control and mock-transfection groups (aP < 0.05, bP < 0.01). All LPS treatment groups except the EP and pA-box-transfection groups showed significantly higher levels of these mRNAs and proteins compared with the corresponding groups without LPS treatment (aP < 0.05, bP < 0.01).
The intestinal microbiota and gut immune system must communicate to maintain a balance between tolerance and activation. Although the immune system provides protection against pathogenic microbes, the human body is a host to trillions of microbes, symbionts, and mutualists; some of which are essential to human health[12]. The maintenance of immune tolerance and the inflammatory response depend on interactions between symbiotic bacteria, intestinal mucosa epithelial cells and immune cells[13]. If any of these components are disturbed, inflammation imbalances can occur that develop into inflammatory disease. TLRs can recognize some intrinsic molecules that are present in bacteria, viruses, epithelial cells and immune cells and play significant roles in maintaining symbiotic bacterial resistance and inducing the anti-inflammatory response to pathogens[14]. In IBD, the intestinal mucosa becomes intolerant of symbiotic bacteria and their products, leading to the excessive activation of the TLR signaling pathways, triggering an intracellular signaling cascade, producing chemokines, launching and controlling key transcription factors, and triggering and amplifying the inflammatory reaction[15]. TLR4 signaling pathways are activated by the recruitment of MYD88, resulting in the activation of phosphorylated IL-1-related kinases and tumor necrosis factor-associated receptor factor 6, further activating NF-κB transcription factors and releasing a series of inflammatory factors, such as interferon-γ[3,16]. LPS is an outer membrane glycolipid of Gram-negative bacteria and a major ligand for TLR4. When there is an imbalance in intestinal mucosal immune responses in IBD, the LPS-induced excessive activation of TLR4 in the bowel mucosa triggers inflammation. In this study, after treating the SW480 and THP-1 cells for 24 h, LPS was able to upregulate the expression of TLR4 and the downstream molecules MYD88 and pNF-κB p65 and promote the secretion of proinflammatory cytokines, such as IL-1β, IL-6 and TNF-α, in cell culture supernatants. These findings suggest that LPS can produce proinflammatory factors and cause inflammation by activating the intracellular MYD88-dependent TLR4 signaling pathway.
HMGB1 is ubiquitously present in the nuclei of all mammalian cells, where it displays dual functions. Under normal conditions, HMGB1 binds to DNA and bends it to facilitate gene transcription. Under stress conditions, such as injury or infection, it is released and promotes inflammation, taking part in the pathogeneses of a variety of inflammatory diseases. During inflammatory reactions, the activation of monocytes/macrophages is the main source of HMGB1. When the production of exogenous bacterial endotoxins (e.g., LPS) or endogenous inflammatory cytokines is stimulated, HMGB1, which is mainly concentrated in the nucleus, is released from activated monocytes/macrophages in a time- and dose-dependent manner. This study found that LPS treatment not only upregulated HMGB1 expression and the secretion of human mononuclear cell THP-1, but also time- and dose-dependently increased HMGB1 expression and the secretion of intestinal epithelial SW480 cells. These findings showed that intestinal epithelial cells could also secrete HMGB1 following exposure to an exogenous stimulus. It has been established that the excessive activation of the TLR signaling pathways in intestinal epithelial cells and inflammatory cells play an important role in the pathogenesis of IBD. LPS within the lumen is a major cause of the excessive activation of the TLR signaling pathways. This study showed that LPS not only activated these pathways, but also promoted the expression and release of HMGB1. HMGB1, which is an important DAMP, can bind to TLR4 and reactivate the TLR4 signaling pathways. Thus, HMGB1 is not only an endogenous ligand for TLR4, but also an amplifier of TLR-mediated inflammatory responses[17]. This function may be important for the persistent inflammation reaction that occurs in IBD. HMGB1 release is a dynamic process, involving exit from the nucleus into the cytoplasm, translocation from the cytosol into cytoplasmic organelles, and exocytosis[18]. In this study, after 24 h of LPS treatment, HMGB1 expression in the THP-1 and SW480 cells and HMGB1 secretion in the supernatants were markedly increased over time. In contrast with other proinflammatory cytokines, HMGB1 production and release continuously increased over 24 h, which may be related to the circulation cycles of the LPS/TLR4/HMGB1 signaling pathways.
EP, which is a stable fatty ester, is derived from the endogenous metabolite pyruvic acid. The pharmacological effects of EP include the downregulation of proinflammatory factors, the improvement of redox reaction-mediated cell and tissue damage, and the inhibition of apoptosis. EP protects inflammatory tissues from damage, such as fatal sepsis, systemic inflammation, uncontrolled hemorrhagic shock, and stroke[19-21]. Studies of various types of in vivo and in vitro models have proven that EP can downregulate the activation of the proinflammatory transcription factors NF-κB and reduce the expression of all types of proinflammatory factors[22,23]. In recent years, studies have shown that EP is an effective inhibitor of HMGB1 release.
Our data revealed that EP inhibited the secretion and release of HMGB1 and the activation of the LPS/TLR4 signaling pathways as well as the release of inflammatory cytokines in the SW480 and THP-1 cells. Studies have found that in the traumatic brain injury (TBI) model, EP can inhibit the expression of HMGB1, TLR4, and NF-κB and the secretion of proinflammatory cytokines, such as IL-1β, IL-6 and TNF-α, in brain tissue following TBI, showing that EP can inhibit the HMGB1/TLR4/NF-κB signaling pathways[24]. It can effectively inhibit inducible nitric oxide synthase (iNOS) expression and HMGB1 release in RAW264.7 cells following LPS stimulation[25]. EP also regulates HMGB1 release from macrophages following LPS stimulation by inhibiting the NF-κB and (or) p38 mitogen-activated protein kinase (MAPK) pathways[26]. In this study, in addition to its inhibition of the LPS-activated HMGB1/TLR4 signaling pathways, there may be other mechanisms by which EP inhibited the release of proinflammatory cytokines. Moreover, the group not receiving LPS treatment in this study exhibited a lack of effect of EP on HMGB1 expression and secretion, the activation of the HMGB1/TLR4 signaling pathways and the release of proinflammatory cytokines in the SW480 and THP-1 cells. These findings suggest that EP was inhibitory only under pathological and not physiological conditions.
The structure of HMGB1 is subdivided into two homologous HMG boxes, the A-box and B-box. As described previously, the truncation of HMGB1 into individual structural domains has revealed that the B box induces strong proinflammatory activities. Inversely, the A-box may act as an antagonist of HMGB1[27]. The A-box protein dose-dependently inhibits HMGB1-induced TNF and IL-1β release in macrophage cultures and is stimulated by HMGB1[28]. It is possible that these anti-inflammatory effects occur due to competition with receptors for HMGB1[29]. Animal experiments have shown that after the recombinant HMGB1 A-box protein is administered by intraperitoneal injection, a significant decrease in mortality occurs and the abnormal release of inflammatory cytokines is blocked compared with a control group[30]. After recombinant A-box protein is injected into mice with collagen-induced arthritis, its systemic administration significantly reduces the mean arthritis score, disease-induced weight loss, and the histological severity of arthritis[31,32]. Therefore, the A-box is considered a natural antagonist of HMGB1. Studies have reported that HMGB1 and the LPS/TLR4 signaling pathways have important associations with the pathogenesis of IBD[9,33,34] and that positive regulation may occur between them[35,36]. However, there are no reports of an influence of HMGB1 A-box overexpression on HMGB1 and the LPS/TLR4 signaling pathways.
Our data revealed that the overexpression of HMGB1 A-box had no effect on the HMGB1 or LPS/TLR4 signaling pathways in the SW480 cells themselves. However, using a Transwell co-culturing system, we further observed the effects of changes in the above-mentioned molecules on HMGB1 A-box-overexpressing SW480 cells co-cultured with THP-1 cells. Following the LPS treatment of the THP-1 cells, we found that the expression and secretion of HMGB1, the expression of TLR4 and the downstream molecules MYD88 and pNF-κB p65, and the secretion of proinflammatory cytokines, such as IL-1β, IL-6 and TNF-α, in the cell culture supernatants of the pA-box-transfection group were significantly lower compared with the control and mock-transfection groups. In addition, there were no significant differences compared with the corresponding LPS-untreated group in the THP-1 cells. These findings suggest that HMGB1 A-box-overexpressing SW480 cells can inhibit the secretion and release of HMGB1 and the activation of the HMGB1/TLR4 signaling pathways by LPS after co-culturing with THP-1 cells. Therefore, we hypothesize that HMGB1 A-box-overexpressing SW480 cells do not possess an autocrine function that suppresses the activation of their own HMGB1/TLR4 signaling pathways following LPS exposure, but they may have a paracrine function that inhibits the activation of the LPS/TLR4 signaling pathways and the proinflammatory activities of HMGB1 in THP-1 cells. This study also found that in the absence of LPS, HMGB1 A-box-overexpressing SW480 cells do not show alterations in the expression or secretion of HMGB1 or activation of the LPS/TLR4 signaling pathways after co-culturing with THP-1 cells. These results indicate that HMGB1 A-box antagonized HMGB1-induced inflammation only under pathological and not physiological conditions. Therefore, HMGB1 A-box may represent a new therapeutic target for the treatment of IBD.
In conclusion, in the co-culture system of SW480 and THP-1 cells, LPS can not only activate HMGB1/TLR4 signaling pathways, but also promote the secretion of proinflammatory cytokines. EP, which is a potent inhibitor of HMGB1 release, can inhibit the HMGB1/TLR4 signaling pathways and the secretion of proinflammatory cytokines activated by LPS, but its mechanism remains unclear. Unlike EP, HMGB1 A-box, as a specific antagonist of HMGB1, can specifically inhibit the HMGB1/TLR4 signaling pathways and the secretion of LPS-activated proinflammatory cytokines. Taken together, HMGB1 A-box may represent a novel therapeutic HMGB1-targeting agent for IBD treatment.
Inflammatory bowel disease (IBD) is thought to result from an inappropriate and continuing inflammatory response to commensal microbes in a genetically susceptible host. Although numerous reports have indicated that high mobility group box (HMGB)1/toll-like receptor (TLR)4 signaling pathways play a important role in IBD, but the possible regulatory mechanism remains to be elucidated yet.
The authors aimed to investigate the effects of two HMGB1 inhibitors (HMGB1 A-box and ethyl pyruvate) on the HMGB1/TLR-4 signaling pathway and the secretion of some proinflammatory cytokines in SW480 and THP-1 cells after activation by lipopolysaccharides (LPS).
The authors have managed to describe theoretical and experimental evidence of HMGB1 A-box as a potential inhibitor of HMGB1/TLR-4 signaling pathways convincingly.
The authors hypothesize that HMGB1 A-box, as a natural antagonist of HMGB1, can competitively inhibit the binding of HMGB1 to its receptors and attenuate the proinflammatory effect. The authors have managed to describe theoretical and experimental evidence of HMGB1 A-box as a potential inhibitor of HMGB1/TLR-4 signaling pathways convincingly. Therefore it could be a possible therapeutic strategy for some patients with IBD.
HMGB1 is a non-histone nuclear protein that, depending on its location and post-translational modifications, has several functions. HMGB1 is ubiquitously expressed in nuclei, where it binds and stabilizes DNA. HMGB1 can be translocated from the nucleus to the cytoplasm and extracellular space. When released, it has been shown to act as a damage-associated molecular pattern (DAMP). HMGB1 is subdivided into A-box and B-box. A-box is the most used antagonist of HMGB1, which competes with receptors for binding with HMGB1.
The purpose of the paper to investigate the effects of two HMGB1 inhibitors (HMGB1 A-box and ethyl pyruvate) on the HMGB1/TLR4 signaling pathway and the secretion of some proinflammatory cytokines in SW480 and THP-1 cells after activation by LPS, is well established and consecutively unfolded. The hypothesis of the potential role of the HMGB1 A-box as a novel approach to the treatment of IBD is presented in an interesting manner. They have determined HMGB1, TLR4 and its downstream signaling molecules MyD88 and NF-κB p65 protein and mRNA levels by RT-PCR, densitometry and Western blot, and also studied the cytokine levels in the culture supernatants. The authors conclude that HMGB1 A-box and ethyl pyruvate both inhibit HMGB1/TLR4 and downstream signaling molecules MyD88 as well as NF-κB p65 and the secretion of several important pro-inflammatory cytokines induced by LPS stimulation. In general, this study is methodologically well performed, the paper well written and has a clear message. The authors have used intestinal epithelial cell line to study the potential effect of above-mentioned compounds and to clarify some pathogenetic molecular mechanisms in IBD. Therefore, the objective of this study is relevant.
P- Reviewer: Nakov VN, Pullerits R, Westra J S- Editor: Yu J L- Editor: Kerr C E- Editor: Wang CH
| 1. | Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011;474:307-317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2019] [Cited by in RCA: 1878] [Article Influence: 134.1] [Reference Citation Analysis (2)] |
| 2. | Geremia A, Biancheri P, Allan P, Corazza GR, Di Sabatino A. Innate and adaptive immunity in inflammatory bowel disease. Autoimmun Rev. 2014;13:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 484] [Cited by in RCA: 703] [Article Influence: 58.6] [Reference Citation Analysis (1)] |
| 3. | Cario E. Toll-like receptors in inflammatory bowel diseases: a decade later. Inflamm Bowel Dis. 2010;16:1583-1597. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 242] [Cited by in RCA: 259] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 4. | Leal RF, Milanski M, Ayrizono Mde L, Coope A, Rodrigues VS, Portovedo M, Oliveira LM, Fagundes JJ, Coy CS, Velloso LA. Toll-like receptor 4, F4/80 and pro-inflammatory cytokines in intestinal and mesenteric fat tissue of Crohn’s disease. Int J Clin Exp Med. 2013;6:98-104. [PubMed] |
| 5. | Watanabe T, Higuchi K, Kobata A, Nishio H, Tanigawa T, Shiba M, Tominaga K, Fujiwara Y, Oshitani N, Asahara T. Non-steroidal anti-inflammatory drug-induced small intestinal damage is Toll-like receptor 4 dependent. Gut. 2008;57:181-187. [PubMed] |
| 6. | Andersson U, Erlandsson-Harris H, Yang H, Tracey KJ. HMGB1 as a DNA-binding cytokine. J Leukoc Biol. 2002;72:1084-1091. [PubMed] |
| 7. | Ju Z, Chavan SS, Antoine DJ, Dancho M, Tsaava T, Li J, Lu B, Levine YA, Stiegler A, Tamari Y. Sequestering HMGB1 via DNA-conjugated beads ameliorates murine colitis. PLoS One. 2014;9:e103992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Vitali R, Palone F, Cucchiara S, Negroni A, Cavone L, Costanzo M, Aloi M, Dilillo A, Stronati L. Dipotassium Glycyrrhizate Inhibits HMGB1-Dependent Inflammation and Ameliorates Colitis in Mice. PLoS One. 2013;8:e66527. [PubMed] |
| 9. | Davé SH, Tilstra JS, Matsuoka K, Li F, DeMarco RA, Beer-Stolz D, Sepulveda AR, Fink MP, Lotze MT, Plevy SE. Ethyl pyruvate decreases HMGB1 release and ameliorates murine colitis. J Leukoc Biol. 2009;86:633-643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 148] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 10. | Gong W, Zheng Y, Chao F, Li Y, Xu Z, Huang G, Gao X, Li S, He F. The anti-inflammatory activity of HMGB1 A box is enhanced when fused with C-terminal acidic tail. J Biomed Biotechnol. 2010;2010:915234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Gong Q, Xu JF, Yin H, Liu SF, Duan LH, Bian ZL. Protective effect of antagonist of high-mobility group box 1 on lipopolysaccharide-induced acute lung injury in mice. Scand J Immunol. 2009;69:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Yamamoto ML, Schiestl RH. Intestinal microbiome and lymphoma development. Cancer J. 2014;20:190-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Xiang YT, Mei L. Research progress in pathogenesis of IBD: the role of gut flora. Sheng Li Ke Xue Jin Zhan. 2013;44:247-252. [PubMed] |
| 14. | Saito K, Katakura K, Suzuki R, Suzuki T, Ohira H. Modulating Toll-like receptor 4 signaling pathway protects mice from experimental colitis. Fukushima J Med Sci. 2013;59:81-88. [PubMed] |
| 15. | Chen L, Lin MJ, Zhan LL, Lv XP. Analysis of TLR4 and TLR2 polymorphisms in inflammatory bowel disease in a Guangxi Zhuang population. World J Gastroenterol. 2012;18:6856-6860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Fukata M, Arditi M. The role of pattern recognition receptors in intestinal inflammation. Mucosal Immunol. 2013;6:451-463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 143] [Cited by in RCA: 169] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 17. | Li G, Liang X, Lotze MT. HMGB1: The Central Cytokine for All Lymphoid Cells. Front Immunol. 2013;4:68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 134] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 18. | Gardella S, Andrei C, Ferrera D, Lotti LV, Torrisi MR, Bianchi ME, Rubartelli A. The nuclear protein HMGB1 is secreted by monocytes via a non-classical, vesicle-mediated secretory pathway. EMBO Rep. 2002;3:995-1001. [PubMed] |
| 19. | Wang LK, Wang LW, Li X, Han XQ, Gong ZJ. Ethyl pyruvate prevents inflammatory factors release and decreases intestinal permeability in rats with D-galactosamine-induced acute liver failure. Hepatobiliary Pancreat Dis Int. 2013;12:180-188. [PubMed] |
| 20. | Entezari M, Javdan M, Antoine DJ, Morrow DM, Sitapara RA, Patel V, Wang M, Sharma L, Gorasiya S, Zur M. Inhibition of extracellular HMGB1 attenuates hyperoxia-induced inflammatory acute lung injury. Redox Biol. 2014;2:314-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 21. | Tang J, Deng P, Jiang Y, Tang Y, Chen B, Su L, Liu Z. Role of HMGB1 in propofol protection of rat intestinal epithelial cells injured by heat shock. Cell Biol Int. 2013;37:262-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Wu CX, Sun H, Liu Q, Guo H, Gong JP. LPS induces HMGB1 relocation and release by activating the NF-κB-CBP signal transduction pathway in the murine macrophage-like cell line RAW264.7. J Surg Res. 2012;175:88-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 23. | Huang W, Tang Y, Li L. HMGB1, a potent proinflammatory cytokine in sepsis. Cytokine. 2010;51:119-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 179] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 24. | Su X, Wang H, Zhao J, Pan H, Mao L. Beneficial effects of ethyl pyruvate through inhibiting high-mobility group box 1 expression and TLR4/NF-κB pathway after traumatic brain injury in the rat. Mediators Inflamm. 2011;2011:807142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 100] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 25. | Janko C, Filipović M, Munoz LE, Schorn C, Schett G, Ivanović-Burmazović I, Herrmann M. Redox modulation of HMGB1-related signaling. Antioxid Redox Signal. 2014;20:1075-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 131] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 26. | Ulloa L, Ochani M, Yang H, Tanovic M, Halperin D, Yang R, Czura CJ, Fink MP, Tracey KJ. Ethyl pyruvate prevents lethality in mice with established lethal sepsis and systemic inflammation. Proc Natl Acad Sci USA. 2002;99:12351-12356. [PubMed] |
| 27. | Johansson L, Snäll J, Sendi P, Linnér A, Thulin P, Linder A, Treutiger CJ, Norrby-Teglund A. HMGB1 in severe soft tissue infections caused by Streptococcus pyogenes. Front Cell Infect Microbiol. 2014;4:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Jia L, Clear A, Liu FT, Matthews J, Uddin N, McCarthy A, Hoxha E, Durance C, Iqbal S, Gribben JG. Extracellular HMGB1 promotes differentiation of nurse-like cells in chronic lymphocytic leukemia. Blood. 2014;123:1709-1719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 29. | Zhang CL, Shu MG, Qi HW, Li LW. Inhibition of tumor angiogenesis by HMGB1 A box peptide. Med Hypotheses. 2008;70:343-345. [PubMed] |
| 30. | LeBlanc PM, Doggett TA, Choi J, Hancock MA, Durocher Y, Frank F, Nagar B, Ferguson TA, Saleh M. An immunogenic peptide in the A-box of HMGB1 protein reverses apoptosis-induced tolerance through RAGE receptor. J Biol Chem. 2014;289:7777-7786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 31. | Kokkola R, Li J, Sundberg E, Aveberger AC, Palmblad K, Yang H, Tracey KJ, Andersson U, Harris HE. Successful treatment of collagen-induced arthritis in mice and rats by targeting extracellular high mobility group box chromosomal protein 1 activity. Arthritis Rheum. 2003;48:2052-2058. [PubMed] |
| 32. | Andersson U, Wang H, Palmblad K, Aveberger AC, Bloom O, Erlandsson-Harris H, Janson A, Kokkola R, Zhang M, Yang H. High mobility group 1 protein (HMG-1) stimulates proinflammatory cytokine synthesis in human monocytes. J Exp Med. 2000;192:565-570. [PubMed] |
| 33. | Yang H, Tracey KJ. Targeting HMGB1 in inflammation. Biochim Biophys Acta. 2010;1799:149-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 282] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 34. | Trøseid M, Lind A, Nowak P, Barqasho B, Heger B, Lygren I, Pedersen KK, Kanda T, Funaoka H, Damås JK. Circulating levels of HMGB1 are correlated strongly with MD2 in HIV-infection: possible implication for TLR4-signalling and chronic immune activation. Innate Immun. 2013;19:290-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 35. | Maeda S, Hikiba Y, Shibata W, Ohmae T, Yanai A, Ogura K, Yamada S, Omata M. Essential roles of high-mobility group box 1 in the development of murine colitis and colitis-associated cancer. Biochem Biophys Res Commun. 2007;360:394-400. [PubMed] |
| 36. | He ZW, Qin YH, Wang ZW, Chen Y, Shen Q, Dai SM. HMGB1 acts in synergy with lipopolysaccharide in activating rheumatoid synovial fibroblasts via p38 MAPK and NF-κB signaling pathways. Mediators Inflamm. 2013;2013:596716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |