Published online Dec 21, 2014. doi: 10.3748/wjg.v20.i47.17804
Revised: June 22, 2014
Accepted: July 11, 2014
Published online: December 21, 2014
Processing time: 258 Days and 23.3 Hours
The significant influence of tumor stroma on malignant cells has been extensively investigated in this era of targeted therapy. The tumor microenvironment, as a dynamic system, is orchestrated by various cells including tumor vascular composing cells, inflammatory cells and fibroblasts. As a major and important component in tumor stroma, increasing evidence has shown that spindle-shaped cancer-associated fibroblasts (CAFs) are a significant modifier of cancer evolution, and promote tumorigenesis, tumor invasion and metastasis by stimulating angiogenesis, malignant cell survival, epithelial-mesenchymal transition (EMT) and proliferation via direct cell-to-cell contact or secretion of soluble factors in most digestive solid tumors. CAFs are thought to be activated, characterized by the expression of α-smooth muscle actin, fibroblast activated protein, fibroblast specific protein, vimentin, fibronectin, etc. They are hypothesized to originate from normal or aged fibroblasts, bone marrow-derived mesenchymal cells, or vascular endothelial cells. EMT may also be an important process generating CAFs, and most probably, CAFs may originate from multiple cells. A close link exists between EMT, tumor stem cells, and chemo-resistance of tumor cells, which is largely orchestrated by CAFs. CAFs significantly induce immunosuppression, and may be a prognostic marker in various malignancies. Targeted therapy toward CAFs has displayed promising anticancer efficacy, which further reinforces the necessity to explore the relationship between CAFs and their hosts.
Core tip: As a dominant component in tumor stroma, cancer-associated fibroblasts (CAFs) promote tumorigenesis, and tumor progression by stimulating angiogenesis, malignant cell survival, epithelial-mesenchymal transition (EMT) and proliferation via direct cell-to-cell contact or secretion of soluble factors in most digestive solid tumors. CAFs are characterized by the expression of α-smooth muscle actin, fibroblast activated protein, fibroblast specific protein, vimentin, etc. They are hypothesized to originate from various cells. EMT may also be an important process generating CAFs. A close link exists between CAFs-induced EMT, chemo-resistance of tumor cells, and tumor stem cells. CAFs significantly induce immunosuppression, and may be a prognostic marker. Targeted therapy toward CAFs has displayed promising anticancer efficacy.
- Citation: Huang L, Xu AM, Liu S, Liu W, Li TJ. Cancer-associated fibroblasts in digestive tumors. World J Gastroenterol 2014; 20(47): 17804-17818
- URL: https://www.wjgnet.com/1007-9327/full/v20/i47/17804.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i47.17804
Tumors are made up of heterogeneous cells, and are considered to be wounds that do not heal[1]. Carcinogenesis and tumor progression are not only associated with malignant cells themselves, but also with tumor stroma which is an important participant and regulator. Both interact with each other, forming the tumor-host micro-environment[2]. In tumor stroma there are various types of mesenchymal cells including tumor vascular composing cells (endothelial cells and pericytes), inflammatory cells and fibroblasts, which are mosaicked in extracellular matrix (ECM) secreted by fibroblasts[3]. Stromal cells provide malignant cells with growth and proliferation signals, and participate in angiogenesis within tumor. Tumor cells are to stromal cells what “seeds” are to “soil”. The remarkable influence of tumor stroma on cancer cells has been extensively investigated in this era of targeted therapy.
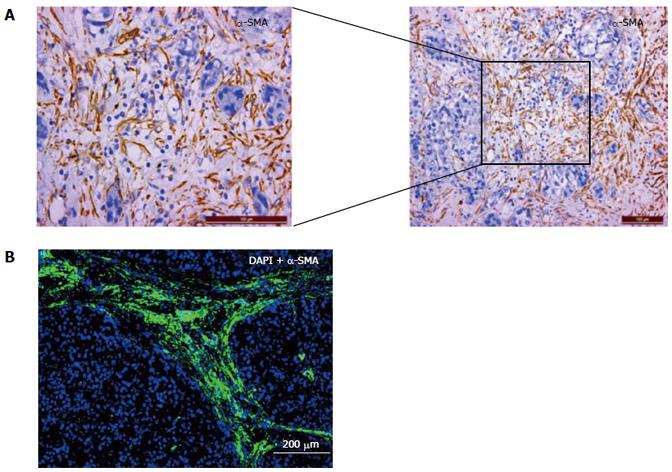
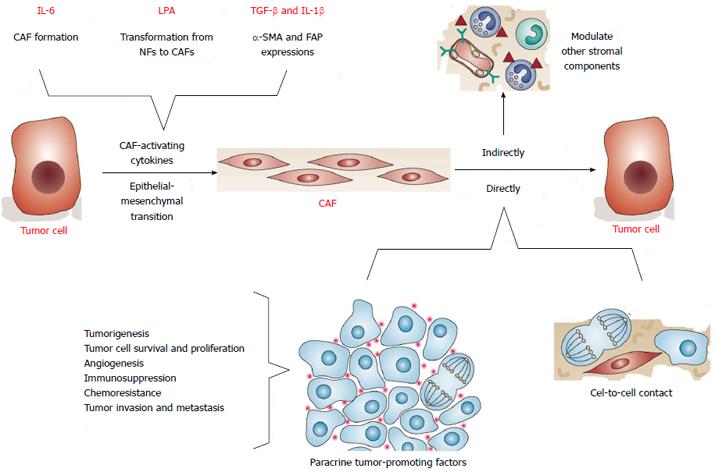
Cancer-associated fibroblasts (CAFs) or tumor-associated fibroblasts (TAFs) are the most abundant with the widest distribution in tumor stroma of most solid tumors, and one of the most important stromal cells mediating tumor-stroma cross-talk (Figure 1). It can not only directly act on malignant cells in a direct cell-to-cell way and by secreting diverse soluble cytokines, regulating tumor evolution, growth, angiogenesis, immunity, chemoresistance, and aggressive behaviors (invasion and metastasis)[4-6], but also interfere with tumor growth indirectly by influencing other stromal components including ECM (Figure 2)[7]. Researchers have proposed the CAFs-centered theory, thinking that CAFs are the hub and control center of tumorigenesis and tumor progression[8]. In recent years, CAFs have become a focus of research, with the hope that they’ll be a novel anti-tumor therapeutic target.
Carcinogenesis resembles injury repair in inflammatory cell infiltration, angiogenesis, fibrogenesis, and fibroblast activation[7]. CAFs were initially identified in tumor stroma of solid tumors with connective tissue generation including breast cancer and pancreatic cancer, and are highly homologous large spindle-like stromal cells with the ability to adhere to plastic[9]. Fibroblasts are versatile, plastic cells that can respond to environmental signals through diverse functional programs. Compared with fibroblasts in normal wound healing, they are fibroblasts with activated phenotypes, which grants CAFs multiple functions in promoting cancer development[10], and share a similar formation process with myofibroblasts[11]. CAFs are characterized by CD34 expression deletion, and abundant expression of α-smooth muscle actin (α-SMA)[11,12]. CAFs also express fibroblast activated protein (FAP), fibroblast specific protein (FSP), neuron glial antigen-2 (NG2), platelet derived growth factor receptor-α (PDGFR-α) and PDGFR-β. Like normal fibroblasts, stromal cell markers including vimentin, fibronectin, podoplanin, prolyl 4-hydroxylase (P4H, 5B5) and stromelysin are also expressed[13].
Research has revealed that paracancerous fibroblasts grow much faster than CAFs segregated and cultured in vitro[14], suggesting that the proliferative ability of CAFs are closely linked with the specific tumor microenvironment, and that CAFs may be activated by various malignant cell-secreted cytokines. In prostate cancer, interleukin (IL)-6 secreted by malignant cells was found to contribute to the formation of CAFs[15]; in hepatocellular carcinoma, lysophostatidic acid (LPA) was reported to transform paracancerous fibroblasts into CAFs[16]; transforming growth factor-β (TGF-β) and IL-1β were also revealed to induce the expression of α-SMA and FAP in normal fibroblasts. Changes in cellular genome, such as global hypomethylation of genomic DNA may also be involved in activation of CAFs[17].
CAFs can synthesize and secrete abundant soluble molecules containing the fibroblast growth factor family such as basic fibroblast growth factor (bFGF), the vascular endothelial growth factor (VEGF) family members, platelet-derived growth factor (PDGF), ligands of epidermal growth factor receptor (EGFR), the IL family members including IL-1, the colony-stimulating factors including granulocyte colony-stimulating factor (G-CSF) and granulocyte-macrophage CSF (GM-CSF), and TGF-β, whose major functions in tumor are breaking the balance of the microenvironment to induce stromal reaction, stimulating angiogenesis via a paracrine, mediating inflammatory reaction and activating surrounding stromal cells to secrete cytokines or proteinases, which resembles wound healing[18,19]. CAFs are therefore also called myofibroblasts in tumor stroma, paracancerous fibroblasts or tumor-derived fibroblasts[20].
The origin of CAFs is still obscure[21]. CAFs are considered to derive from various cells. Fibroblasts in tumor stroma are hypothesized to be the origin because fibroblasts in metastatic foci of colorectal carcinoma share the same protein labeling with the resident fibroblasts[22]. Particularly in hepatocellular carcinoma (HCC) which is usually derived from chronic hepatitis and liver cirrhosis, large amounts of static fibroblasts are activated after repeated inflammatory stimulation, injury repair, and tissue fibrosis, forming a large number of CAFs. The expression of α-SMA in hepatic stellate cells (HSCs) increases gradually indicating their activation, and suggesting them as a possible origin in HCC[23]. Fibroblasts in peritumoral tissue progressively convert into CAFs during the course of tumor progression, and LPA can accelerate HCC progression by recruiting peri-tumor fibroblasts (PTFs) and promoting their transdifferentiation into myofibroblasts[16,24]. FSP and α-SMA are highly expressed in tumor stroma, and during transformation from normal fibroblasts to activated CAFs, the expressions of α-SMA, TGF-β and stromal cell-derived factor-1 (SDF-1) are significantly up-regulated with impressive functions exerted. Bone marrow-derived stromal cells like mesenchymal stem cells (MSCs) which share similar functions with CAFs and express α-SMA and a1 chain of type I collagen are also believed to be the source[25]. Tumor microenvironments dynamically regulate the activation of recruiting MSCs, which leads to formation of activated fibroblasts in tumors[26]. MSCs obtain an analogous phenotype with CAFs after co-culture with tumor cells or treatment with tumor conditioned medium in vitro, expressing higher levels of α-SMA, FSP, vimentin and SDF-1/CXCL 12[26]. Epithelial mesenchymal transition (EMT) of malignant and normal epithelial cells is a possible mechanism, and E-cadherin could be down-regulated by TGF-β[27]. Vascular endothelial cells resemble CAFs in that they both express CD31 as well as α-SMA and FSP, when induced by TGF-β, and are inferred to partly migrate from vascular basement membrane to tumor stroma and transdifferentiate into CAFs[27]. Transformation of senescent fibroblasts may also be an approach. No evidence of clonal somatic genetic alterations has been detected in CAFs[28]. It is likely that CAFs originate from various cells. During co-culture of breast cancer cells and fibroblasts, CAFs were mostly derived from surrounding normal fibroblasts, with a small portion from vascular smooth muscle cells and pericytes[29].
A number of studies have reported crucial roles of CAFs in providing cancer cells with proliferative and survival propensities favoring tumorigenesis[30]. CAFs play important roles in tumorigenesis, and it is possible that before canceration of epithelial cells, fibroblasts in stroma are activated to transform into CAFs, which secrete tumor-promoting factors[30]. Fibroblasts in the skin of individuals susceptible to breast cancer express abnormal phenotypes which reduce their requirements for culture in vitro compared to normal fibroblasts, and enhance their proliferative ability; and skin fibroblasts segregated from patients with melanoma, retinoblastoma, Wilms carcinoma and multiple colon polyps also demonstrate potent proliferation potential, indicating that fibroblasts in vivo may promote tumorigenesis[31]. Olumi et al[32] found that when eternal but not tumorigenic prostate epithelial cells were inoculated into nude mice with/without fibroblasts originating from normal prostate tissue, they proliferated faintly without oncogenic ability; but when they were co-transplanted with CAFs, a tumor was gradually formed. CAFs stimulate malignant cell proliferation by providing various types of growth factors and cytokines, such as hepatocyte growth factor (HGF), epidermal growth factor (EGF) family members, fibroblast growth factor (FGF), Wnt families, SDF-1 (CXCL12), fork-head box F1 (FoxF1) and IL-6[33-35]. Interestingly, HGF stimulates the growth of some tumor cell lines, but inhibits the growth of some other tumor cell lines, and does not promote proliferation all in a dose-dependent manner in diverse cell lines, which could possibly be explained by the fact that HGF activates various signaling pathways including PI3K, pp60c-src, phospholipase Cγ, c-Met and Ras-ERK, and that cells harboring different dominant pathways react differently to HGF with differences existing in the expression of receptors which are responsive to HGF in cells of diverse origins[36]. CAFs are reported to be able to turn on complementary metabolic pathways to buffer and recycle products of anaerobic metabolism, modifying local severe conditions and facilitating the maintenance and enhancement of cancer cell survival in unfavorable environments such as necrosis with low pH and hypoxia, since they prefer to undergo anaerobic glycolysis even in the presence of oxygen during cancer cell proliferation[37]. Our study further supports that CAFs markedly promote malignant cell growth in HCC, and that CAFs-secreted HGF plays a vital role in cancer cell proliferation[38].
Tumor progression is now recognized as the product of evolving crosstalk between different cell types within tumors and in the tumor-surrounding stroma[39]. During tumor progression, stroma contributes a suitable microenvironment facilitating tumor invasion, during which CAFs communicate with malignant cells actively and closely. Increasing evidence has revealed that CAFs facilitate tumor growth and progression by synthesizing and releasing diverse soluble molecules in a context-dependent manner including growth factors, chemokines, proteinases and ECM components, among which SDF-1, EGF, HGF and insulin-like growth factor (IGF) are considered typical[9,40-42]. In particular, HGF plays an important role not only in tumor growth, but also in tumor transformation promotion, facilitating tumor metastasis via classic HGF-cMet signaling pathway activation. It has been proved that blocking HGF secretion by fibroblasts reduces metastasis rates[43]. CAF-secreted prostaglandin E2 (PGE2) has also been proved to promote tumor growth in head and neck tumors[44]. Decreased Pten expression in CAFs in tumor stroma can promote tumor cell growth[20]. In HCC, hepatocellular CAFs have also been proved to promote malignant cell proliferation in vitro[16].
Non-invasive tumor gains invasive ability after co-inoculated with CAFs in nude mice, and CAFs in breast cancer were reported to stimulate angiogenesis by releasing SDF1α+β[45]. After low-invasive cancer cells were inoculated into the skin of nude mice with corresponding CAFs or normal fibroblasts from patients with inclination of metastasis, those co-inoculated with CAFs had significantly more potent proliferative and invasive abilities, with richer surrounding collagen. This was due to the fact that CAFs can recruit bone marrow-derived endothelial progenitor cells into the stroma, facilitating angiogenesis, remodel the ECM by enhancing integrin signaling through matrix crosslinking, and promoting tumor growth and metastasis by secreting abundant soluble tumor-promoting factors such as SDF-1/CXCL12, which are also highly expressed when cultured alone, further demonstrating that CAFs take an active part in tumor progression[46-49]. In a melanoma-liver-metastasis model, the formation of metastases was found to be closely associated with activation of HSCs, also suggesting the tight relationship between CAFs and metastasis[50]. CAFs can also increase the invasive ability of esophageal cancer cells via secretion of HGF[51].
CAFs can also interfere with tumor growth, invasion and metastasis by secreting abundant angiogenic factors and matrix metalloproteinases (MMPs). After fibroblasts are co-cultured with invasive melanoma, they secrete significantly more cytokines including IL-1β, IL-8 and IL-6, and inhibiting the synthesis or secretion of those factors attenuates the invasive ability of malignant cells, suggesting the key role of those molecules[52]. The interaction between cytokines and proteinases secreted by CAFs and ECM components is also a vital progression and metastasis mediator.
MMPs can not only promote tumor invasion and migration by directly acting on cancer cells, but also participate in reconstruction of ECM after degrading it, thus facilitating tumor cells to penetrate the extracellular barrier, infiltrate and escape. For instance, MMP3 can directly act on protein E-cadherin in the extracellular region of tumor cells, decomposing the formed compound with the function of cell adhesion, and facilitating EMT and invasion of tumor cells[53]; MMP1 can activate protease-activated receptor 1 (PAR1) by degrading its extracellular region, which promote invasion and metastasis of tumor cells via PAR1-dependent Ca2+ signaling[54].
IL-6, an inflammatory factor mediating acute inflammation, is now believed to be another key cytokine regulating tumor progression. After the IL-6/STAT3 pathway is activated, malignant cells proliferate much faster and their anti-apoptosis ability increases significantly[55]. In the liver, IL-6 can directly promote the regeneration of hepatic cells, and inhibit apoptosis mediated by Fas[56].
Abundant evidence supports the pro-metastasis role of CAFs in primary tumors, however, there is limited data on CAFs in the corresponding lymph nodes and distant metastases, although accumulating evidence shows crucial roles for CAFs in metastases. Stromal signals resembling those of a distant organ can select for cancer cells that are primed for metastasis in that organ[57]. Metastatic cancer cells can bring their own soil, including CAFs, from the primary tumor to the metastases[58]. MSCs incorporated into the stroma of the primary tumor and metastases both expressed α-SMA and PDGFR-β as CAF markers[59]. Stromal reactions in metastases, probably containing metastasis-associated fibroblasts (MAFs), have been described as reactive and fibrotic tissue with enhanced deposition of vitronectin and fibronectin, desmoplasia, nodal fibrosis and hyaline stroma[60,61]. Kaplan et al[62] showed that tumor-secreted factors promote metastatic spread into specific distant organs. Within days after primary tumor implantation, localized deposition of extra domain (ED)-A or ED-B spliced forms of fibronectin occurs due to resident fibroblasts within target organs that are conventional sites of metastasis, corresponding to the particular primary tumor. It may be that TGF-β responsiveness is equally important at the metastatic site as in the primary tumor, as cellular forms of fibronectin and lysyl oxidase (LOX) are well-known TGF-β target genes[63-65]. Chaiwun et al[66] reported that loss of Glutathione S-transferase Pi (GSTPi) expression was observed in breast cancer cells in paired cases of both the primary invasive breast cancer and the corresponding axillary lymph node metastases compared with benign breast epithelial cells, and that a significant association exists between GSTPi-, vimentin- and α-SMA-positive fibroblasts in the tumor microenvironment at both sites. CAF conversion from ostensibly normal cells is mediated by various factors including TGF-β[67,68], Act A[69], MMP7[70], PDGF[71], prograstin[72], sonic hedgehog[73], and YAP[74], while factors implicated in MAF corruption are osteopontin[75], discoidin domain receptor 2 deficiency[76], IQGAP-1 deficiency[77], exosomal microRNA (miR)-494, miR-542-3p[78], miR-31, miR-214, miR-155[79], Met exosomes[80], and TGF-β exosomes[81]. In the diverse steps of the metastatic cascade including invasion, ectopic survival, stimulation of angiogenesis, adhesion at the metastatic niche and macroscopic metastasis formation[82], CAFs continuously transmit profitable signals interpreted as various factors including CCL2/FGF19[83], CD81 exosomes[84], EGF, IGF-1[85], S100A4[86], stanniocalcin (STC)[87], track formation[88,89], type I collagen alignment[90], and direct cell-cell contacts[91], while factors implicated in MAFs-induced metastasis include CXCL10[92], ED-A/ED-B fibronectin[62], IL-11[65], and periostin[93], with LOX[63,94], neuregulin 1[95], SDF-1[77,96], scatter factor (SF)/HGF[77,97,98], and tenascin-C[97,99] as the shared factors between CAFs and MAFs. Based on CAF-specific signatures present in exosomes, we may detect and monitor CAF reactions, and probably MAF formation allowing optimized prognostic values[82]. The differential gene expression patterns between normal colonic fibroblasts, CAFs from primary tumors and CAFs from hepatic metastasis could be useful for predicting relapse in primary tumors[100].
EMT is physiologically important during the development of multicellular animal embryos and the formation of tissues and organs, and is commonly found in many pathological processes including wound healing, inflammation and invasion. It is considered to be the most important and common process during tumor metastasis, and has become a hot topic in recent years[101]. Epithelial cells undergo EMT when the cells which are closely arranged with weak deformability are gradually transformed into stromal cells which are loosely arranged with strong mobility by triggering and inducing factors[102]. In tumors, EMT occurs in malignant cells when non- or weakly-invasive tumor cells with epithelial phenotype gradually change into cells with strong invasive ability, induced by external factors[103]. Tumor progression is a multi-step process, and EMT is a key link. CAFs or CAF-precursor cells can significantly promote EMT of malignant cells[104]. The major cellular biological behavior change of tumor cells undergoing EMT is enhanced invasive and metastatic abilities[105].
The most important iconic change during tumor cell EMT is the down-regulation of E-cadherin or E-cadherin/β-catenin compound expression, which are important inter-cellular adhesion molecules, and negatively correlate with tumor invasive and metastatic abilities[106]. Reduced expression of E-cadherin would attenuate cellular adhesive ability, promoting tumor migration[107]. However, during EMT, the expression of proteins with stromal phenotypes including fibronectin, N-cadherin, vimentin and α-SMA recurs or increases, and is closely associated with tumor invasive ability[108]. EMT is also accompanied by the increased expression of relative transcription factors including Snail, Slug and Twist[109]. During tumor invasion, tumor cells always lose their epithelial characteristics, and present stromal cell phenotypes, which resembles the EMT during embryo development[103].
Increasing evidence has revealed that EMT of tumor cells is based on the interaction between malignant cells and tumor stroma, during which CAFs play vital roles, by secreting a series of soluble mediators or functioning through the direct cell-to-cell approach[54]. EMT promotes invasion of tumor cells, and it is regulated by various exogenous stimulating factors including the MMP, integrin, and TGF-β factors, which further activate the downstream tyrosine kinase-dependent pathway after binding their corresponding receptors[110]. According to in-depth research, most of the stimulating signals were revealed to be secreted by CAFs, indicating the key role of CAFs during tumor EMT, and CAFs induced EMT of tumor cells by providing them with pre-migration stimulation, generating greater invasive and metastatic abilities[111,112]. During the research in prostate cancer, CAFs were found to induce EMT and stem cell marker expression in cancer cells, degrade ECM, and promote invasion and metastasis by secreting MMP2 and IL-6[15]. CAFs were also found to be closely associated with tumor cell EMT in oral and tongue cancers[10,113]. CAF-precursor cells such as hepatocellular and pancreatic stellate cells can also induce EMT[23]. The significant role of TGF-β released by CAFs during tumor cell EMT was specifically revealed[114], and it has bidirectional functions: in normal tissues, TGF-β can inhibit cell proliferation and promote apoptosis, attenuating carcinogenesis[101]; while during tumor progression after the tumor is formed, TGF-β becomes the ally of tumor, inducing EMT and promoting invasion and metastasis[114]. The conditioned medium of cultured CAFs isolated from invasive breast cancer tissues (CAF-CM) can transform breast cancer cell lines into more aggressive phenotypes by promoting EMT mainly induced by CAF-paracrine TGF-β1 with the TGF-β/Smad signaling pathway activated, and enhancing cell-extracellular matrix adhesion, migration and invasion in breast cancer cells. The EMT phenotype induced could be reversed by blocking TGF-β1 signaling[115]. TGF-β1 does not stimulate CAF with a more divergent expression pattern (CAF-D) migration, but enhances invasion and expression of EMT markers in malignant keratinocytes. Inhibiting TGF-β1 in three-dimensional cultures containing CAF-D impairs keratinocyte invasion, suggesting TGF-β1-induced EMT mediates CAF-D-induced carcinoma cell invasion[68]. Research into other tumors also showed that tumor EMT mediated by TGF-β is usually accompanied by activation of the Smad, PI3K/AKT, and P38 MAPK signaling pathways, the first of which may be major[116]. Other CAFs-secreted growth factors, inflammatory factors and chemokines including HGF, FGF, IGF, tumor necrosis factor (TNF)-α, IL-1β, MCP-1 (CCL2), Rantes (CCL5), MCP-3 (CCL7), endothelin-1 (ET-1) and the integrin family members have also been proved to promote EMT[113,117-119]. Our previous study found that CAFs induce EMT in HCC cells mainly through release of HGF and IL-6, and increase the invasive and migratory properties of the cancer cells[38]. Recently, our ongoing research revealed that during HCC progression, EMT could be induced by CAFs mainly through the transglutaminase 2 (TG2) mediated IL-6/STAT3 signaling pathway.
In research into Lewis sarcoma metastasis, an interesting phenomenon called packaged metastasis was revealed, and tumor cells were found to metastasis alone with its “soil”, mainly consisting of CAFs; after removing CAFs, the lung metastasis rate decreases significantly[58].
Ectopic miR-205 over-expression in cancer cells can counteract CAF-induced EMT, thus impairing enhancement of cell invasion, acquisition of stem cell traits, tumorigenicity, and metastatic dissemination. The evidence that miR-205 replacement in cancer cells is able not only to prevent, but also to revert the oxidative/pro-inflammatory axis leading to EMT induced by CAFs sets the rationale for developing miRNA-based approaches to prevent and treat metastatic disease[120].
Research has shown that after undergoing EMT, malignant cells become more resistant to chemotherapy, and those expressing surface molecules of stem cells increase, suggesting a close link between CAFs-induced EMT, tumor stem cells, and chemo-resistance of tumor cells[42,121-124]. EMT can trigger the transformation of malignant cells to tumor stem cells. In breast cancer research, CD44+CD24- cancer stem cells exhibit activation of the TGF-β signaling pathway, and blocking this pathway results in a decrease in stem cells and a process contrary to EMT, namely mesenchymal-epithelial transition (MET)[121,122]. CAFs are primarily resistant to chemotherapy due to a small proportion of proliferating cells in contrast to malignant cells, which makes CAFs a potential source of tumor progression[125]. CAFs have been proved to promote chemo-resistance of malignant cells in many tumors. Witta et al[42] believe that tumors with stromal phenotypes are more chemo-resistant and share more characteristics with tumor stem cells. After culture in conditioned medium of pancreatic CAFs, cancer cells had greater proliferative, invasive and metastatic abilities, forming a mass, and greater resistance, decreasing the rate of apoptosis induced by chemotherapy by up to 76%. Loeffler et al[126] reported that elimination of CAFs expressing FAP by a DNA vaccine could significantly enhance the antitumor effect of Doxorubicin, inhibit tumor growth and metastasis, and prolong survival time. CAFs can even mediate tumor resistance to anti-VEGF treatment through PDGF-C secretion[127].
Cancer patients exhibit a generalized immunosuppressive status, and there is substantial evidence that stromal activation can foster tumor growth and progression by modulating immunopathogenesis[39]. The role of the tumor environment has been largely studied as a dynamic system orchestrated mainly by inflammatory cells. There is substantial evidence supporting that it is not inflammation per se, but rather the inflammatory “context” that determines the ability of pro-inflammatory factors to facilitate or prevent tumor growth[128]. CAFs can stimulate angiogenesis in tumor stroma to provide malignant cells with more nutrients by releasing VEGF and PDGF[129]; attract immune cells including macrophages and neutrophils to induce inflammation by secreting IL-1, IL-6, IL-8 and TNF-α[4]; and participant in reconstruction of the tumor microenvironment by regulating inflammatory cells such as lymphocytes by secreting uPA and MMPs to mediate tumor progression[130]. They can induce inflammation in tumors by secreting chemokines including CXCL1, CXCL2, CXCL5 and IL-6 which activate cancer-associated macrophages to promote tumor invasion and metastasis[4]. Immune invasion occurring among malignant cells is considered to be one of the important causes of poor prognosis. Immune cells ought to be the barrier killing tumor cells by the function of immune surveillance. However, in many solid tumors, immune cells could be “educated” by malignant cells to be the accomplice during tumor progression[131]. CAFs which can produce significant levels of suppressive mediators have been proved to be involved in immunosuppression and tumor immune privilege and escape through functioning on immune cells in the tumor microenvironment[132], and are found to recruit Th17 cells and up-regulate IL-17 expression via RANTES and MCP-1 secretion, producing a pro-inflammatory cytokine milieu, providing cell-to-cell contact engagement, and participating in cancer immunosuppression in melanoma, breast cancer, and colon carcinoma[133]. CAFs separated from non-small cell lung cancer tissues have reciprocal interactions with T cells, and can induce and up-regulate the expression of IL-17A and INF-γ in tumor-associated T (TAT) cells via IL-6, and when anti-IL-6 is supplied, the regulatory function is weakened[134]. Subpopulations of CAFs can highly express B7H1 (PD-L1) and B&DC (PD-L2), which can induce immune tolerance and be up-regulated by INF-γ; when TATs are co-cultured with CAFs, their function is suppressed, and after anti-B7H1 is added to block the pathway, TATs regain their function completely, suggesting that CAFs can regulate TAT function via the PD-L1/PL-1 axis[132]. In particular, natural killer (NK) cells can be potently regulated by soluble factors derived from CAFs under inflammatory conditions. In breast cancer, CAFs are reported to be unable to stimulate effective antitumor NK cell responses and to suppress NK cell cytotoxicity[135]. In metastatic melanoma, CAFs can trigger NK cell dysfunction by secreting PGE2, which is characterized by suppressed expression of NKp44 and NKp30, also suggesting that CAFs can prevent malignant cells from being eliminated by immune cells, facilitating tumor cell growth and metastasis; interestingly, NK cells can also trigger a paradoxical suppressive loop by enhancing the production of PGE2 by CAFs[136]. Our previous study also indicated that hepatocellular CAFs could trigger NK cell dysfunction and suppress their activation by secreting PGE2 and indoleamine-2,3-dioxygenase, creating an unresponsive condition in tumors. This condition is characterized by low expression of cytotoxic molecules and surface markers for cell activation, impaired production of cytokines, and decreased cytotoxicity against malignant cells[137]. CAFs are frequently present in the stroma of colorectal carcinoma tissues[138], and we also found that colorectal CAFs exhibit activated phenotypes and sharply suppress NK cell functions with secretion of PGE2, indicating a novel mechanism linking the pro-inflammatory response to immune tolerance within the tumor milieu[139]. In contrast and interestingly, NK cells also play an antifibrotic role via an inhibitory effect on myofibroblasts, which secrete TGF-β and PDGF to enhance tumor growth and progression[140], by inducing apoptosis and via the production of INF-γ, and downregulation of NK cells may facilitate liver fibrosis[141]. It is the general view that the tumor microenvironment induces tolerance[142], and this is worthy of further investigation to identify the roles of CAFs in immune editing. Manipulating the expression of and signaling through these molecules may open new rational avenues for developing novel immune-based therapies to enhance antitumor immunity in human cancer.
CAFs are closely associated with prognosis. It was validated in the VICTOR trial that the proportion of intra-tumor stroma can serve as a significant prognosticator for stage II and III colon cancer patients[143]. The overall and disease-free survival periods (OS and DFS) were significantly lower in the stroma-high group [OS, hazard ratio (HR) = 1.96; DFS, HR = 2.15]. The 5-year OS was 69.0% vs 83.4% and DFS 58.6% vs 77.3% for stroma-high vs stroma-low patients with appreciable differences. The protein, FAP, is specifically expressed by CAFs. A retrospective study showed that expression of FAP in tumor stroma was positively correlated with metastatic lymph nodes, metastases and recurrences, and negatively correlated with prognosis[138]. However, research into breast cancer has drawn the opposite conclusion, revealing that high expression of paracancerous FAP was positively correlated with tumor-free survival, and negatively correlated with metastasis, indicating that FAP could be regarded as an independent prognostic marker[144]. It is unknown why diametrically opposite results have been demonstrated in diverse tumors. Research into primary HCC showed that paracancerous activated HSCs were negatively correlated with clinical outcomes, but positively correlated with early metastases, and that HSCs along with Tregs and monocytes could be treated as effective prognostic indicators[25]. The level of IL-6 secreted by CAFs was proved to be correlated with clinical stage of HCC[145]. Our study also suggests the prognostic significance of CAFs in HCC[38]. Our ongoing study revealed that TG2 in CAFs may serve as a novel prognostic biomarker and therapeutic target.
Targeted therapy toward CAFs has displayed promising anticancer efficacy, further strengthening the need to study the correlation between CAFs and their hosts[146]. CAFs can regulate carcinogenesis and tumor progression by secreting soluble mediators including cytokines, chemokines, proteinases, collagens and fibronectins. Nowadays, there are inhibitors and antibodies which target cytokines, chemokines and proteinases, with the advantage that CAFs have a relatively stable genome making it nonsusceptible to various drugs, suggesting that CAFs-targeted therapy is theoretically practicable and clinically operable. Anti-cancer therapy targeting CAFs has been actively investigated recently. An antibody against FAP inhibited the growth of colon cancer[147]. A number of drugs targeting receptors on the cellular surface have been applied clinically, and PDGF receptors such as regarofenib, imatinib (Glivec), sorafenib and sunitinib have been used to treat patients with metastatic gastrointestinal stromal tumor (GIST), renal carcinoma, and hepatocellular carcinoma. An MMP inhibitor (MMPI) with better selectivity has also been investigated in clinical trials[148]. A phase I clinical trial[149] on a mono-antibody targeting PD-1 in the treatment of solid tumors has been completed which showed stable and satisfactory efficacy. Research into CAFs will provide a theoretical basis for novel strategies of tumor stroma-targeted early diagnosis, prognosis-prediction and new preventive and therapeutic methods, which are of great potential clinical value. However, further investigations into CAFs are required.
The current trend in cancer research is the inclusion of the tumor microenvironment as a major contributor to malignant progression[9]. The importance of the stromal tissue in regulating the physiological processes of the body is undeniable. The reviewed studies emphasize the importance of the cross-talk between stroma and malignant cells (Table 1). Key evidence demonstrates that stromal components may modulate cancer progression. The stromal cells of the carcinogenic lesion, especially CAFs, have long been known to be supportive and responsive, and express critical signals that drive proliferation, angiogenesis, and motility. CAFs are thought to be activated, characterized by the expression of various markers including α-SMA, FAP, FSP, vimentin, fibronectin, etc., and may have multiple origins including normal and aged fibroblasts, MSCs, vascular endothelial cells, and importantly, EMT. In most digestive solid tumors, CAFs influence epithelial transformation by direct cell-to-cell contact or by producing paracrine factors that affect both normal epithelia as well as carcinoma cells. The tissue specificity of the stroma-epithelial interaction possibly accounts for the tissue and cell type-specific role of the microenvironment in carcinoma progression. CAFs also play important roles in immunosuppression induction, and may be a significant prognosticator. The recognition of the active role that CAFs play in carcinogenesis not only adds a new level of complexity to cancer biology, but also brings an opportunity for new therapeutic strategies. Targeted therapy towards CAFs has displayed promising anticancer efficacy.
| Function | Soluble molecules involved |
| Tumor cell growth and proliferation | HGF, EGF family members, FGF, Wnt families, SDF-1 (CXCL-12), FoxF1, IL-6, PDGF |
| Tumor invasion and metastasis | SDF-1 (CXCL-12), CXCL10, EGF, SF/HGF, IGF, PGE2, MMPs, IL-1β, IL-6, IL-8, IL-11, CCL2/FGF19, CD81 exosomes, S100A4, STC, type I collagen, ED-A/ED-B fibronectin, periostin, LOX, NRG1, TNC, PDGF |
| Epethelial-mesenchymal transition | MMPs, integrin family members, TGF-β, IL-6, HGF, FGF, IGF, TNF-α, IL-1β, MCP-1 (CCL2), Rantes (CCL5), MCP-3 (CCL7), ET-1 |
| Chemoresistance | PDGF-C, TGF-β |
| Immunosuppression | VEGF, PDGF, IL-1, IL-6, IL-8, TNF-α, uPA, MMPs, CXCL1, CXCL2, CXCL5, Rantes, MCP-1, PGE2, indoleamine-2, 3-IDO |
EMT, which can be induced by CAFs, significantly promotes carcinogenesis, tumor invasion, metastasis and chemo-resistance. It is controlled by a network of regulators, and provides an explanation for the association between inflammation and cancer progression. Progress in understanding EMT has been an exercise in appreciating the level of complexity required to change cellular identity. The mechanism of transition highlights the integration of nuclear regulation and network signaling with alterations in the microenvironment to create a moving cell. Here we have focused on the effects of various stroma-derived paracrine factors on epithelial cells. It is probable that these same factors also have vital effects on other stromal cells, including fibroblasts, endothelial cells and inflammatory cells. The malignant state occurs and is exacerbated by defects in communication pathways which recruit host cells to become vital participants in the heterotypic tissue invasion field. Cross-talk between tumor cells and host cells triggers pro-survival, proliferation and invasion pathways in both the cancer cells and their host. Some of the EMT-associated signal transductions point to potential targets for therapy. A better understanding of the effects of targeting these pathways, however, is required. It is likely that further characterization of these interactions, and the molecular identification of key mediators, will provide novel insights into oncology and indicate new therapeutic options. Pharmacological and biological agents that interfere with signaling between the malignant epithelial cells and the supporting stroma will likely continue to be tested. An important issue for EMT identification to be regarded as having a high prognostic and therapeutic value is to determine the use of specific markers. These should, in theory, be able to recognize a cancer EMT-derived mesenchymal cell from a normal mesenchymal cell.
Recent findings have produced great strides in developing an understanding of the molecular events involved in processes necessary for tumor cell invasion and subsequent metastasis formation. However, it is unclear which signaling pathways should be inhibited in order to most effectively block tumor progression and cause minimal toxicity in normal tissues at the same time. It is also notable that the models described in this review are not mutually exclusive, both in different patients, as well as in different fibroblastic cells in any specific tissue, as fibroblasts are quite heterogeneous. Most of the valuable insights concerning the tissue microenvironment have been derived from co-culture and tissue recombination xenograft experiments, however, these results may not be applicable to the in vivo situation due to the fact that not all key environmental factors and cells are considered. The ability to overexpress specific factors or conditionally knock out specific genes in vivo in stromal cells will further add to our knowledge of the complex interactions involved in cancer progression. Future developments will include a new class of therapies targeting the extracellular and intracellular mediators, which act at the tumor-host communication interface. Future efforts should further focus on how the events of cell attachment, matrix proteolysis, and cell migration are controlled and integrated, which requires a better understanding of the transcriptional regulations and cell signaling mechanisms that are involved in these events. We have relatively poor knowledge regarding the similarities or differences between CAF function in the primary tumor, pre-metastatic niche and metastasis. Future work should also aim to define the function, identities and molecular profiles of diverse CAF subtypes in tumor biopsies from primary tumors and from metastases pre-, during, and post-treatment. In addition, animal models should be carefully designed to allow early identification and to clarify the role of MAFs.
In conclusion, it is necessary to explore the relationship between CAFs and their hosts. In addition, further understanding of the relevant genetics and epigenetics will be especially vital in order to differentiate CAFs as patient-specific therapeutic targets.
P- Reviewer: Becker KF, Ding XW, Zoli W S- Editor: Ding Y L- Editor: Webster JR E- Editor: Liu XM
| 1. | Dvorak HF. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med. 1986;315:1650-1659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3033] [Cited by in RCA: 3099] [Article Influence: 79.5] [Reference Citation Analysis (0)] |
| 2. | Kalluri R. Basement membranes: structure, assembly and role in tumour angiogenesis. Nat Rev Cancer. 2003;3:422-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1236] [Cited by in RCA: 1210] [Article Influence: 55.0] [Reference Citation Analysis (0)] |
| 3. | Marx J. Cancer biology. All in the stroma: cancer’s Cosa Nostra. Science. 2008;320:38-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Erez N, Truitt M, Olson P, Arron ST, Hanahan D. Cancer-Associated Fibroblasts Are Activated in Incipient Neoplasia to Orchestrate Tumor-Promoting Inflammation in an NF-kappaB-Dependent Manner. Cancer Cell. 2010;17:135-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1085] [Cited by in RCA: 1228] [Article Influence: 81.9] [Reference Citation Analysis (0)] |
| 5. | Hwang RF, Moore T, Arumugam T, Ramachandran V, Amos KD, Rivera A, Ji B, Evans DB, Logsdon CD. Cancer-associated stromal fibroblasts promote pancreatic tumor progression. Cancer Res. 2008;68:918-926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 897] [Cited by in RCA: 936] [Article Influence: 55.1] [Reference Citation Analysis (0)] |
| 6. | Ostman A, Augsten M. Cancer-associated fibroblasts and tumor growth--bystanders turning into key players. Curr Opin Genet Dev. 2009;19:67-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 412] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 7. | Parsonage G, Filer AD, Haworth O, Nash GB, Rainger GE, Salmon M, Buckley CD. A stromal address code defined by fibroblasts. Trends Immunol. 2005;26:150-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 223] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 8. | Franco OE, Shaw AK, Strand DW, Hayward SW. Cancer associated fibroblasts in cancer pathogenesis. Semin Cell Dev Biol. 2010;21:33-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 296] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 9. | Kalluri R, Zeisberg M. Fibroblasts in cancer. Nat Rev Cancer. 2006;6:392-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3347] [Cited by in RCA: 3531] [Article Influence: 185.8] [Reference Citation Analysis (1)] |
| 10. | Vered M, Dayan D, Yahalom R, Dobriyan A, Barshack I, Bello IO, Kantola S, Salo T. Cancer-associated fibroblasts and epithelial-mesenchymal transition in metastatic oral tongue squamous cell carcinoma. Int J Cancer. 2010;127:1356-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Tomasek JJ, Gabbiani G, Hinz B, Chaponnier C, Brown RA. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nat Rev Mol Cell Biol. 2002;3:349-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2964] [Cited by in RCA: 3160] [Article Influence: 137.4] [Reference Citation Analysis (0)] |
| 12. | Gabbiani G. The myofibroblast in wound healing and fibrocontractive diseases. J Pathol. 2003;200:500-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1179] [Cited by in RCA: 1201] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 13. | Ramirez-Montagut T, Blachere NE, Sviderskaya EV, Bennett DC, Rettig WJ, Garin-Chesa P, Houghton AN. FAPalpha, a surface peptidase expressed during wound healing, is a tumor suppressor. Oncogene. 2004;23:5435-5446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 92] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Gao MQ, Kim BG, Kang S, Choi YP, Park H, Kang KS, Cho NH. Stromal fibroblasts from the interface zone of human breast carcinomas induce an epithelial-mesenchymal transition-like state in breast cancer cells in vitro. J Cell Sci. 2010;123:3507-3514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 110] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 15. | Giannoni E, Bianchini F, Masieri L, Serni S, Torre E, Calorini L, Chiarugi P. Reciprocal activation of prostate cancer cells and cancer-associated fibroblasts stimulates epithelial-mesenchymal transition and cancer stemness. Cancer Res. 2010;70:6945-6956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 479] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 16. | Mazzocca A, Dituri F, Lupo L, Quaranta M, Antonaci S, Giannelli G. Tumor-secreted lysophostatidic acid accelerates hepatocellular carcinoma progression by promoting differentiation of peritumoral fibroblasts in myofibroblasts. Hepatology. 2011;54:920-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 121] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 17. | Jiang L, Gonda TA, Gamble MV, Salas M, Seshan V, Tu S, Twaddell WS, Hegyi P, Lazar G, Steele I. Global hypomethylation of genomic DNA in cancer-associated myofibroblasts. Cancer Res. 2008;68:9900-9908. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 151] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 18. | Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev. 2003;83:835-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 603] [Cited by in RCA: 566] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 19. | Bergers G, Benjamin LE. Tumorigenesis and the angiogenic switch. Nat Rev Cancer. 2003;3:401-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2432] [Cited by in RCA: 2467] [Article Influence: 112.1] [Reference Citation Analysis (0)] |
| 20. | Trimboli AJ, Cantemir-Stone CZ, Li F, Wallace JA, Merchant A, Creasap N, Thompson JC, Caserta E, Wang H, Chong JL. Pten in stromal fibroblasts suppresses mammary epithelial tumours. Nature. 2009;461:1084-1091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 425] [Cited by in RCA: 459] [Article Influence: 28.7] [Reference Citation Analysis (0)] |
| 21. | Haviv I, Polyak K, Qiu W, Hu M, Campbell I. Origin of carcinoma associated fibroblasts. Cell Cycle. 2009;8:589-595. [PubMed] |
| 22. | Mueller L, Goumas FA, Affeldt M, Sandtner S, Gehling UM, Brilloff S, Walter J, Karnatz N, Lamszus K, Rogiers X. Stromal fibroblasts in colorectal liver metastases originate from resident fibroblasts and generate an inflammatory microenvironment. Am J Pathol. 2007;171:1608-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 134] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 23. | Steiling H, Mühlbauer M, Bataille F, Schölmerich J, Werner S, Hellerbrand C. Activated hepatic stellate cells express keratinocyte growth factor in chronic liver disease. Am J Pathol. 2004;165:1233-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Kojima Y, Acar A, Eaton EN, Mellody KT, Scheel C, Ben-Porath I, Onder TT, Wang ZC, Richardson AL, Weinberg RA. Autocrine TGF-beta and stromal cell-derived factor-1 (SDF-1) signaling drives the evolution of tumor-promoting mammary stromal myofibroblasts. Proc Natl Acad Sci USA. 2010;107:20009-20014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 469] [Cited by in RCA: 687] [Article Influence: 45.8] [Reference Citation Analysis (0)] |
| 25. | Quante M, Tu SP, Tomita H, Gonda T, Wang SS, Takashi S, Baik GH, Shibata W, Diprete B, Betz KS. Bone marrow-derived myofibroblasts contribute to the mesenchymal stem cell niche and promote tumor growth. Cancer Cell. 2011;19:257-272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 857] [Cited by in RCA: 869] [Article Influence: 62.1] [Reference Citation Analysis (0)] |
| 26. | Mishra PJ, Mishra PJ, Humeniuk R, Medina DJ, Alexe G, Mesirov JP, Ganesan S, Glod JW, Banerjee D. Carcinoma-associated fibroblast-like differentiation of human mesenchymal stem cells. Cancer Res. 2008;68:4331-4339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 715] [Cited by in RCA: 725] [Article Influence: 42.6] [Reference Citation Analysis (0)] |
| 27. | Zeisberg EM, Potenta S, Xie L, Zeisberg M, Kalluri R. Discovery of endothelial to mesenchymal transition as a source for carcinoma-associated fibroblasts. Cancer Res. 2007;67:10123-10128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 632] [Cited by in RCA: 765] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 28. | Qiu W, Hu M, Sridhar A, Opeskin K, Fox S, Shipitsin M, Trivett M, Thompson ER, Ramakrishna M, Gorringe KL. No evidence of clonal somatic genetic alterations in cancer-associated fibroblasts from human breast and ovarian carcinomas. Nat Genet. 2008;40:650-655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 245] [Cited by in RCA: 263] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 29. | Rønnov-Jessen L, Petersen OW, Koteliansky VE, Bissell MJ. The origin of the myofibroblasts in breast cancer. Recapitulation of tumor environment in culture unravels diversity and implicates converted fibroblasts and recruited smooth muscle cells. J Clin Invest. 1995;95:859-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 312] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 30. | Liotta LA, Kohn EC. The microenvironment of the tumour-host interface. Nature. 2001;411:375-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1724] [Cited by in RCA: 1699] [Article Influence: 70.8] [Reference Citation Analysis (0)] |
| 31. | Schor SL, Haggie JA, Durning P, Howell A, Smith L, Sellwood RA, Crowther D. Occurrence of a fetal fibroblast phenotype in familial breast cancer. Int J Cancer. 1986;37:831-836. [PubMed] |
| 32. | Olumi AF, Grossfeld GD, Hayward SW, Carroll PR, Tlsty TD, Cunha GR. Carcinoma-associated fibroblasts direct tumor progression of initiated human prostatic epithelium. Cancer Res. 1999;59:5002-5011. [PubMed] |
| 33. | Giulianelli S, Cerliani JP, Lamb CA, Fabris VT, Bottino MC, Gorostiaga MA, Novaro V, Góngora A, Baldi A, Molinolo A. Carcinoma-associated fibroblasts activate progesterone receptors and induce hormone independent mammary tumor growth: A role for the FGF-2/FGFR-2 axis. Int J Cancer. 2008;123:2518-2531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 34. | Fu L, Zhang C, Zhang LY, Dong SS, Lu LH, Chen J, Dai Y, Li Y, Kong KL, Kwong DL. Wnt2 secreted by tumour fibroblasts promotes tumour progression in oesophageal cancer by activation of the Wnt/β-catenin signalling pathway. Gut. 2011;60:1635-1643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 100] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 35. | Saito RA, Micke P, Paulsson J, Augsten M, Peña C, Jönsson P, Botling J, Edlund K, Johansson L, Carlsson P. Forkhead box F1 regulates tumor-promoting properties of cancer-associated fibroblasts in lung cancer. Cancer Res. 2010;70:2644-2654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 36. | Jiang WG, Martin TA, Parr C, Davies G, Matsumoto K, Nakamura T. Hepatocyte growth factor, its receptor, and their potential value in cancer therapies. Crit Rev Oncol Hematol. 2005;53:35-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 189] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 37. | Koukourakis MI, Giatromanolaki A, Harris AL, Sivridis E. Comparison of metabolic pathways between cancer cells and stromal cells in colorectal carcinomas: a metabolic survival role for tumor-associated stroma. Cancer Res. 2006;66:632-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 361] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 38. | Jia CC, Wang TT, Liu W, Fu BS, Hua X, Wang GY, Li TJ, Li X, Wu XY, Tai Y. Cancer-associated fibroblasts from hepatocellular carcinoma promote malignant cell proliferation by HGF secretion. PLoS One. 2013;8:e63243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 39. | Kuang DM, Zhao Q, Peng C, Xu J, Zhang JP, Wu C, Zheng L. Activated monocytes in peritumoral stroma of hepatocellular carcinoma foster immune privilege and disease progression through PD-L1. J Exp Med. 2009;206:1327-1337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 591] [Cited by in RCA: 724] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 40. | Orimo A, Weinberg RA. Stromal fibroblasts in cancer: a novel tumor-promoting cell type. Cell Cycle. 2006;5:1597-1601. [PubMed] |
| 41. | Verras M, Lee J, Xue H, Li TH, Wang Y, Sun Z. The androgen receptor negatively regulates the expression of c-Met: implications for a novel mechanism of prostate cancer progression. Cancer Res. 2007;67:967-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 158] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 42. | Witta SE, Gemmill RM, Hirsch FR, Coldren CD, Hedman K, Ravdel L, Helfrich B, Dziadziuszko R, Chan DC, Sugita M. Restoring E-cadherin expression increases sensitivity to epidermal growth factor receptor inhibitors in lung cancer cell lines. Cancer Res. 2006;66:944-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 410] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 43. | Jego G, Bataille R, Geffroy-Luseau A, Descamps G, Pellat-Deceunynck C. Pathogen-associated molecular patterns are growth and survival factors for human myeloma cells through Toll-like receptors. Leukemia. 2006;20:1130-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 122] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 44. | Alcolea S, Antón R, Camacho M, Soler M, Alfranca A, Avilés-Jurado FX, Redondo JM, Quer M, León X, Vila L. Interaction between head and neck squamous cell carcinoma cells and fibroblasts in the biosynthesis of PGE2. J Lipid Res. 2012;53:630-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 45. | Dimanche-Boitrel MT, Vakaet L, Pujuguet P, Chauffert B, Martin MS, Hammann A, Van Roy F, Mareel M, Martin F. In vivo and in vitro invasiveness of a rat colon-cancer cell line maintaining E-cadherin expression: an enhancing role of tumor-associated myofibroblasts. Int J Cancer. 1994;56:512-521. [PubMed] |
| 46. | Orimo A, Gupta PB, Sgroi DC, Arenzana-Seisdedos F, Delaunay T, Naeem R, Carey VJ, Richardson AL, Weinberg RA. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 2005;121:335-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2625] [Cited by in RCA: 2886] [Article Influence: 144.3] [Reference Citation Analysis (0)] |
| 47. | Levental KR, Yu H, Kass L, Lakins JN, Egeblad M, Erler JT, Fong SF, Csiszar K, Giaccia A, Weninger W. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;139:891-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2671] [Cited by in RCA: 3087] [Article Influence: 192.9] [Reference Citation Analysis (0)] |
| 48. | Littlepage LE, Egeblad M, Werb Z. Coevolution of cancer and stromal cellular responses. Cancer Cell. 2005;7:499-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 96] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 49. | Pietras K, Pahler J, Bergers G, Hanahan D. Functions of paracrine PDGF signaling in the proangiogenic tumor stroma revealed by pharmacological targeting. PLoS Med. 2008;5:e19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 390] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 50. | Olaso E, Santisteban A, Bidaurrazaga J, Gressner AM, Rosenbaum J, Vidal-Vanaclocha F. Tumor-dependent activation of rodent hepatic stellate cells during experimental melanoma metastasis. Hepatology. 1997;26:634-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 104] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 51. | Grugan KD, Miller CG, Yao Y, Michaylira CZ, Ohashi S, Klein-Szanto AJ, Diehl JA, Herlyn M, Han M, Nakagawa H. Fibroblast-secreted hepatocyte growth factor plays a functional role in esophageal squamous cell carcinoma invasion. Proc Natl Acad Sci USA. 2010;107:11026-11031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 146] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 52. | Li L, Dragulev B, Zigrino P, Mauch C, Fox JW. The invasive potential of human melanoma cell lines correlates with their ability to alter fibroblast gene expression in vitro and the stromal microenvironment in vivo. Int J Cancer. 2009;125:1796-1804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 53. | Kessenbrock K, Plaks V, Werb Z. Matrix metalloproteinases: regulators of the tumor microenvironment. Cell. 2010;141:52-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3948] [Cited by in RCA: 3800] [Article Influence: 253.3] [Reference Citation Analysis (0)] |
| 54. | Boire A, Covic L, Agarwal A, Jacques S, Sherifi S, Kuliopulos A. PAR1 is a matrix metalloprotease-1 receptor that promotes invasion and tumorigenesis of breast cancer cells. Cell. 2005;120:303-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 625] [Cited by in RCA: 660] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 55. | Haura EB, Turkson J, Jove R. Mechanisms of disease: Insights into the emerging role of signal transducers and activators of transcription in cancer. Nat Clin Pract Oncol. 2005;2:315-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 349] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 56. | Cressman DE, Greenbaum LE, DeAngelis RA, Ciliberto G, Furth EE, Poli V, Taub R. Liver failure and defective hepatocyte regeneration in interleukin-6-deficient mice. Science. 1996;274:1379-1383. [PubMed] |
| 57. | Zhang XH, Jin X, Malladi S, Zou Y, Wen YH, Brogi E, Smid M, Foekens JA, Massagué J. Selection of bone metastasis seeds by mesenchymal signals in the primary tumor stroma. Cell. 2013;154:1060-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 352] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 58. | Duda DG, Duyverman AM, Kohno M, Snuderl M, Steller EJ, Fukumura D, Jain RK. Malignant cells facilitate lung metastasis by bringing their own soil. Proc Natl Acad Sci USA. 2010;107:21677-21682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 491] [Cited by in RCA: 500] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 59. | Shinagawa K, Kitadai Y, Tanaka M, Sumida T, Kodama M, Higashi Y, Tanaka S, Yasui W, Chayama K. Mesenchymal stem cells enhance growth and metastasis of colon cancer. Int J Cancer. 2010;127:2323-2333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 221] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 60. | De Wever O, Van Bockstal M, Mareel M, Hendrix A, Bracke M. Carcinoma-associated fibroblasts provide operational flexibility in metastasis. Semin Cancer Biol. 2014;25:33-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 61. | Thariat J, Ahamad A, El-Naggar AK, Williams MD, Holsinger FC, Glisson BS, Allen PK, Morrison WH, Weber RS, Ang KK. Outcomes after radiotherapy for basaloid squamous cell carcinoma of the head and neck: a case-control study. Cancer. 2008;112:2698-2709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 62. | Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C, MacDonald DD, Jin DK, Shido K, Kerns SA. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature. 2005;438:820-827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2613] [Cited by in RCA: 2396] [Article Influence: 119.8] [Reference Citation Analysis (0)] |
| 63. | Erler JT, Bennewith KL, Cox TR, Lang G, Bird D, Koong A, Le QT, Giaccia AJ. Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the premetastatic niche. Cancer Cell. 2009;15:35-44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1012] [Cited by in RCA: 949] [Article Influence: 59.3] [Reference Citation Analysis (0)] |
| 64. | Zhao L, Lim SY, Gordon-Weeks AN, Tapmeier TT, Im JH, Cao Y, Beech J, Allen D, Smart S, Muschel RJ. Recruitment of a myeloid cell subset (CD11b/Gr1 mid) via CCL2/CCR2 promotes the development of colorectal cancer liver metastasis. Hepatology. 2013;57:829-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 189] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 65. | Calon A, Espinet E, Palomo-Ponce S, Tauriello DV, Iglesias M, Céspedes MV, Sevillano M, Nadal C, Jung P, Zhang XH. Dependency of colorectal cancer on a TGF-β-driven program in stromal cells for metastasis initiation. Cancer Cell. 2012;22:571-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 745] [Cited by in RCA: 900] [Article Influence: 69.2] [Reference Citation Analysis (0)] |
| 66. | Chaiwun B, Sukhamwang N, Trakultivakorn H, Saha B, Young L, Tsao-Wei D, Naritoku WY, Groshen S, Taylor CR, Imam SA. GSTPi-positive tumour microenvironment-associated fibroblasts are significantly associated with GSTPi-negative cancer cells in paired cases of primary invasive breast cancer and axillary lymph node metastases. Br J Cancer. 2011;105:1224-1229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 67. | Kiskowski MA, Jackson RS, Banerjee J, Li X, Kang M, Iturregui JM, Franco OE, Hayward SW, Bhowmick NA. Role for stromal heterogeneity in prostate tumorigenesis. Cancer Res. 2011;71:3459-3470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 68. | Costea DE, Hills A, Osman AH, Thurlow J, Kalna G, Huang X, Pena Murillo C, Parajuli H, Suliman S, Kulasekara KK. Identification of two distinct carcinoma-associated fibroblast subtypes with differential tumor-promoting abilities in oral squamous cell carcinoma. Cancer Res. 2013;73:3888-3901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 133] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 69. | Fordyce CA, Patten KT, Fessenden TB, DeFilippis R, Hwang ES, Zhao J, Tlsty TD. Cell-extrinsic consequences of epithelial stress: activation of protumorigenic tissue phenotypes. Breast Cancer Res. 2012;14:R155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 70. | McCaig C, Duval C, Hemers E, Steele I, Pritchard DM, Przemeck S, Dimaline R, Ahmed S, Bodger K, Kerrigan DD. The role of matrix metalloproteinase-7 in redefining the gastric microenvironment in response to Helicobacter pylori. Gastroenterology. 2006;130:1754-1763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 71. | Ostman A, Heldin CH. PDGF receptors as targets in tumor treatment. Adv Cancer Res. 2007;97:247-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 172] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 72. | Duckworth CA, Clyde D, Worthley DL, Wang TC, Varro A, Pritchard DM. Progastrin-induced secretion of insulin-like growth factor 2 from colonic myofibroblasts stimulates colonic epithelial proliferation in mice. Gastroenterology. 2013;145:197-208, e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 73. | Walter K, Omura N, Hong SM, Griffith M, Vincent A, Borges M, Goggins M. Overexpression of smoothened activates the sonic hedgehog signaling pathway in pancreatic cancer-associated fibroblasts. Clin Cancer Res. 2010;16:1781-1789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 147] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 74. | Calvo F, Ege N, Grande-Garcia A, Hooper S, Jenkins RP, Chaudhry SI, Harrington K, Williamson P, Moeendarbary E, Charras G. Mechanotransduction and YAP-dependent matrix remodelling is required for the generation and maintenance of cancer-associated fibroblasts. Nat Cell Biol. 2013;15:637-646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1018] [Cited by in RCA: 1080] [Article Influence: 90.0] [Reference Citation Analysis (0)] |
| 75. | Mi Z, Bhattacharya SD, Kim VM, Guo H, Talbot LJ, Kuo PC. Osteopontin promotes CCL5-mesenchymal stromal cell-mediated breast cancer metastasis. Carcinogenesis. 2011;32:477-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 142] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 76. | Badiola I, Olaso E, Crende O, Friedman SL, Vidal-Vanaclocha F. Discoidin domain receptor 2 deficiency predisposes hepatic tissue to colon carcinoma metastasis. Gut. 2012;61:1465-1472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 77. | Liu C, Billadeau DD, Abdelhakim H, Leof E, Kaibuchi K, Bernabeu C, Bloom GS, Yang L, Boardman L, Shah VH. IQGAP1 suppresses TβRII-mediated myofibroblastic activation and metastatic growth in liver. J Clin Invest. 2013;123:1138-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 78. | Rana S, Malinowska K, Zöller M. Exosomal tumor microRNA modulates premetastatic organ cells. Neoplasia. 2013;15:281-295. [PubMed] |
| 79. | Mitra AK, Zillhardt M, Hua Y, Tiwari P, Murmann AE, Peter ME, Lengyel E. MicroRNAs reprogram normal fibroblasts into cancer-associated fibroblasts in ovarian cancer. Cancer Discov. 2012;2:1100-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 337] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 80. | Peinado H, Alečković M, Lavotshkin S, Matei I, Costa-Silva B, Moreno-Bueno G, Hergueta-Redondo M, Williams C, García-Santos G, Ghajar C. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat Med. 2012;18:883-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2866] [Cited by in RCA: 2946] [Article Influence: 226.6] [Reference Citation Analysis (0)] |
| 81. | Webber J, Steadman R, Mason MD, Tabi Z, Clayton A. Cancer exosomes trigger fibroblast to myofibroblast differentiation. Cancer Res. 2010;70:9621-9630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 544] [Cited by in RCA: 672] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 82. | Özdemir BC, Pentcheva-Hoang T, Carstens JL, Zheng X, Wu CC, Simpson TR, Laklai H, Sugimoto H, Kahlert C, Novitskiy SV. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014;25:719-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1955] [Cited by in RCA: 1912] [Article Influence: 173.8] [Reference Citation Analysis (1)] |
| 83. | Liu R, Li J, Xie K, Zhang T, Lei Y, Chen Y, Zhang L, Huang K, Wang K, Wu H. FGFR4 promotes stroma-induced epithelial-to-mesenchymal transition in colorectal cancer. Cancer Res. 2013;73:5926-5935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 84. | Luga V, Zhang L, Viloria-Petit AM, Ogunjimi AA, Inanlou MR, Chiu E, Buchanan M, Hosein AN, Basik M, Wrana JL. Exosomes mediate stromal mobilization of autocrine Wnt-PCP signaling in breast cancer cell migration. Cell. 2012;151:1542-1556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 886] [Cited by in RCA: 1076] [Article Influence: 89.7] [Reference Citation Analysis (0)] |
| 85. | Castaño Z, Marsh T, Tadipatri R, Kuznetsov HS, Al-Shahrour F, Paktinat M, Greene-Colozzi A, Nilsson B, Richardson AL, McAllister SS. Stromal EGF and igf-I together modulate plasticity of disseminated triple-negative breast tumors. Cancer Discov. 2013;3:922-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 86. | Yan XL, Jia YL, Chen L, Zeng Q, Zhou JN, Fu CJ, Chen HX, Yuan HF, Li ZW, Shi L. Hepatocellular carcinoma-associated mesenchymal stem cells promote hepatocarcinoma progression: role of the S100A4-miR155-SOCS1-MMP9 axis. Hepatology. 2013;57:2274-2286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 141] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 87. | Peña C, Céspedes MV, Lindh MB, Kiflemariam S, Mezheyeuski A, Edqvist PH, Hägglöf C, Birgisson H, Bojmar L, Jirström K. STC1 expression by cancer-associated fibroblasts drives metastasis of colorectal cancer. Cancer Res. 2013;73:1287-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 145] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 88. | Scott RW, Hooper S, Crighton D, Li A, König I, Munro J, Trivier E, Wickman G, Morin P, Croft DR. LIM kinases are required for invasive path generation by tumor and tumor-associated stromal cells. J Cell Biol. 2010;191:169-185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 147] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 89. | Gaggioli C, Hooper S, Hidalgo-Carcedo C, Grosse R, Marshall JF, Harrington K, Sahai E. Fibroblast-led collective invasion of carcinoma cells with differing roles for RhoGTPases in leading and following cells. Nat Cell Biol. 2007;9:1392-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1053] [Cited by in RCA: 1209] [Article Influence: 67.2] [Reference Citation Analysis (0)] |
| 90. | Shieh AC, Rozansky HA, Hinz B, Swartz MA. Tumor cell invasion is promoted by interstitial flow-induced matrix priming by stromal fibroblasts. Cancer Res. 2011;71:790-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 141] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 91. | Lin HJ, Zuo T, Lin CH, Kuo CT, Liyanarachchi S, Sun S, Shen R, Deatherage DE, Potter D, Asamoto L. Breast cancer-associated fibroblasts confer AKT1-mediated epigenetic silencing of Cystatin M in epithelial cells. Cancer Res. 2008;68:10257-10266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 92. | Chaturvedi P, Gilkes DM, Wong CC, Luo W, Zhang H, Wei H, Takano N, Schito L, Levchenko A, Semenza GL. Hypoxia-inducible factor-dependent breast cancer-mesenchymal stem cell bidirectional signaling promotes metastasis. J Clin Invest. 2013;123:189-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 141] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 93. | Malanchi I, Santamaria-Martínez A, Susanto E, Peng H, Lehr HA, Delaloye JF, Huelsken J. Interactions between cancer stem cells and their niche govern metastatic colonization. Nature. 2012;481:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 943] [Cited by in RCA: 1075] [Article Influence: 76.8] [Reference Citation Analysis (0)] |
| 94. | Barry-Hamilton V, Spangler R, Marshall D, McCauley S, Rodriguez HM, Oyasu M, Mikels A, Vaysberg M, Ghermazien H, Wai C. Allosteric inhibition of lysyl oxidase-like-2 impedes the development of a pathologic microenvironment. Nat Med. 2010;16:1009-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 618] [Cited by in RCA: 670] [Article Influence: 44.7] [Reference Citation Analysis (0)] |
| 95. | De Boeck A, Pauwels P, Hensen K, Rummens JL, Westbroek W, Hendrix A, Maynard D, Denys H, Lambein K, Braems G. Bone marrow-derived mesenchymal stem cells promote colorectal cancer progression through paracrine neuregulin 1/HER3 signalling. Gut. 2013;62:550-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 132] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 96. | Jung Y, Kim JK, Shiozawa Y, Wang J, Mishra A, Joseph J, Berry JE, McGee S, Lee E, Sun H. Recruitment of mesenchymal stem cells into prostate tumours promotes metastasis. Nat Commun. 2013;4:1795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 262] [Cited by in RCA: 336] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 97. | De Wever O, Nguyen QD, Van Hoorde L, Bracke M, Bruyneel E, Gespach C, Mareel M. Tenascin-C and SF/HGF produced by myofibroblasts in vitro provide convergent pro-invasive signals to human colon cancer cells through RhoA and Rac. FASEB J. 2004;18:1016-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 289] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 98. | Vermeulen L, De Sousa E Melo F, van der Heijden M, Cameron K, de Jong JH, Borovski T, Tuynman JB, Todaro M, Merz C, Rodermond H. Wnt activity defines colon cancer stem cells and is regulated by the microenvironment. Nat Cell Biol. 2010;12:468-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1301] [Cited by in RCA: 1446] [Article Influence: 96.4] [Reference Citation Analysis (1)] |
| 99. | Saupe F, Schwenzer A, Jia Y, Gasser I, Spenlé C, Langlois B, Kammerer M, Lefebvre O, Hlushchuk R, Rupp T. Tenascin-C downregulates wnt inhibitor dickkopf-1, promoting tumorigenesis in a neuroendocrine tumor model. Cell Rep. 2013;5:482-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 100. | Berdiel-Acer M, Cuadras D, Díaz-Maroto NG, Sanjuan X, Serrano T, Berenguer A, Moreno V, Gonçalves-Ribeiro S, Salazar R, Villanueva A. A monotonic and prognostic genomic signature from fibroblasts for colorectal cancer initiation, progression, and metastasis. Mol Cancer Res. 2014;12:1254-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 101. | Bhowmick NA, Neilson EG, Moses HL. Stromal fibroblasts in cancer initiation and progression. Nature. 2004;432:332-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1649] [Cited by in RCA: 1729] [Article Influence: 82.3] [Reference Citation Analysis (0)] |
| 102. | Kalluri R, Neilson EG. Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest. 2003;112:1776-1784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 1051] [Article Influence: 50.0] [Reference Citation Analysis (0)] |
| 103. | Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002;2:442-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4877] [Cited by in RCA: 5118] [Article Influence: 222.5] [Reference Citation Analysis (0)] |
| 104. | Lee TK, Poon RT, Yuen AP, Ling MT, Kwok WK, Wang XH, Wong YC, Guan XY, Man K, Chau KL. Twist overexpression correlates with hepatocellular carcinoma metastasis through induction of epithelial-mesenchymal transition. Clin Cancer Res. 2006;12:5369-5376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 328] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 105. | Alonso SR, Tracey L, Ortiz P, Pérez-Gómez B, Palacios J, Pollán M, Linares J, Serrano S, Sáez-Castillo AI, Sánchez L. A high-throughput study in melanoma identifies epithelial-mesenchymal transition as a major determinant of metastasis. Cancer Res. 2007;67:3450-3460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 253] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 106. | Chen L, Chan TH, Yuan YF, Hu L, Huang J, Ma S, Wang J, Dong SS, Tang KH, Xie D. CHD1L promotes hepatocellular carcinoma progression and metastasis in mice and is associated with these processes in human patients. J Clin Invest. 2010;120:1178-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 126] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 107. | Tepass U, Truong K, Godt D, Ikura M, Peifer M. Cadherins in embryonic and neural morphogenesis. Nat Rev Mol Cell Biol. 2000;1:91-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 347] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 108. | Thiery JP. Epithelial-mesenchymal transitions in development and pathologies. Curr Opin Cell Biol. 2003;15:740-746. [PubMed] |
| 109. | Fu J, Chen Y, Cao J, Luo T, Qian YW, Yang W, Ren YB, Su B, Cao GW, Yang Y. p28GANK overexpression accelerates hepatocellular carcinoma invasiveness and metastasis via phosphoinositol 3-kinase/AKT/hypoxia-inducible factor-1α pathways. Hepatology. 2011;53:181-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 112] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 110. | Mueller MM, Fusenig NE. Friends or foes - bipolar effects of the tumour stroma in cancer. Nat Rev Cancer. 2004;4:839-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1323] [Cited by in RCA: 1315] [Article Influence: 62.6] [Reference Citation Analysis (0)] |
| 111. | Kalluri R. EMT: when epithelial cells decide to become mesenchymal-like cells. J Clin Invest. 2009;119:1417-1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 643] [Cited by in RCA: 735] [Article Influence: 45.9] [Reference Citation Analysis (0)] |
| 112. | Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6805] [Cited by in RCA: 7751] [Article Influence: 484.4] [Reference Citation Analysis (0)] |
| 113. | Jung DW, Che ZM, Kim J, Kim K, Kim KY, Williams D, Kim J. Tumor-stromal crosstalk in invasion of oral squamous cell carcinoma: a pivotal role of CCL7. Int J Cancer. 2010;127:332-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 114. | Siegel PM, Massagué J. Cytostatic and apoptotic actions of TGF-beta in homeostasis and cancer. Nat Rev Cancer. 2003;3:807-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1240] [Cited by in RCA: 1258] [Article Influence: 57.2] [Reference Citation Analysis (0)] |
| 115. | Yu Y, Xiao CH, Tan LD, Wang QS, Li XQ, Feng YM. Cancer-associated fibroblasts induce epithelial-mesenchymal transition of breast cancer cells through paracrine TGF-β signalling. Br J Cancer. 2014;110:724-732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 365] [Cited by in RCA: 518] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 116. | Derynck R, Akhurst RJ, Balmain A. TGF-beta signaling in tumor suppression and cancer progression. Nat Genet. 2001;29:117-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1726] [Cited by in RCA: 1776] [Article Influence: 74.0] [Reference Citation Analysis (0)] |
| 117. | Nagai T, Arao T, Furuta K, Sakai K, Kudo K, Kaneda H, Tamura D, Aomatsu K, Kimura H, Fujita Y. Sorafenib inhibits the hepatocyte growth factor-mediated epithelial mesenchymal transition in hepatocellular carcinoma. Mol Cancer Ther. 2011;10:169-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 118. | Liao CP, Adisetiyo H, Liang M, Roy-Burman P. Cancer-associated fibroblasts enhance the gland-forming capability of prostate cancer stem cells. Cancer Res. 2010;70:7294-7303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 85] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 119. | Acloque H, Adams MS, Fishwick K, Bronner-Fraser M, Nieto MA. Epithelial-mesenchymal transitions: the importance of changing cell state in development and disease. J Clin Invest. 2009;119:1438-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 947] [Cited by in RCA: 1069] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 120. | Gandellini P, Giannoni E, Casamichele A, Taddei ML, Callari M, Piovan C, Valdagni R, Pierotti MA, Zaffaroni N, Chiarugi P. miR-205 hinders the malignant interplay between prostate cancer cells and associated fibroblasts. Antioxid Redox Signal. 2014;20:1045-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 121. | Liedtke C, Mazouni C, Hess KR, André F, Tordai A, Mejia JA, Symmans WF, Gonzalez-Angulo AM, Hennessy B, Green M. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26:1275-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2098] [Cited by in RCA: 2126] [Article Influence: 125.1] [Reference Citation Analysis (0)] |
| 122. | Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, Ollila DW, Sartor CI, Graham ML, Perou CM. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13:2329-2334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1438] [Cited by in RCA: 1540] [Article Influence: 85.6] [Reference Citation Analysis (0)] |
| 123. | Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133:704-715. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6972] [Cited by in RCA: 6810] [Article Influence: 400.6] [Reference Citation Analysis (0)] |
| 124. | Polyak K, Weinberg RA. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer. 2009;9:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2456] [Cited by in RCA: 2573] [Article Influence: 160.8] [Reference Citation Analysis (0)] |
| 125. | Hawsawi NM, Ghebeh H, Hendrayani SF, Tulbah A, Al-Eid M, Al-Tweigeri T, Ajarim D, Alaiya A, Dermime S, Aboussekhra A. Breast carcinoma-associated fibroblasts and their counterparts display neoplastic-specific changes. Cancer Res. 2008;68:2717-2725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 123] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 126. | Loeffler M, Krüger JA, Niethammer AG, Reisfeld RA. Targeting tumor-associated fibroblasts improves cancer chemotherapy by increasing intratumoral drug uptake. J Clin Invest. 2006;116:1955-1962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 534] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 127. | Crawford Y, Kasman I, Yu L, Zhong C, Wu X, Modrusan Z, Kaminker J, Ferrara N. PDGF-C mediates the angiogenic and tumorigenic properties of fibroblasts associated with tumors refractory to anti-VEGF treatment. Cancer Cell. 2009;15:21-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 504] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 128. | Kim S, Takahashi H, Lin WW, Descargues P, Grivennikov S, Kim Y, Luo JL, Karin M. Carcinoma-produced factors activate myeloid cells through TLR2 to stimulate metastasis. Nature. 2009;457:102-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 918] [Cited by in RCA: 876] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 129. | Lu Y, Yang W, Qin C, Zhang L, Deng J, Liu S, Qin Z. Responsiveness of stromal fibroblasts to IFN-gamma blocks tumor growth via angiostasis. J Immunol. 2009;183:6413-6421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 130. | Danø K, Behrendt N, Høyer-Hansen G, Johnsen M, Lund LR, Ploug M, Rømer J. Plasminogen activation and cancer. Thromb Haemost. 2005;93:676-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 131. | Kuang DM, Zhao Q, Wu Y, Peng C, Wang J, Xu Z, Yin XY, Zheng L. Peritumoral neutrophils link inflammatory response to disease progression by fostering angiogenesis in hepatocellular carcinoma. J Hepatol. 2011;54:948-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 391] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 132. | Nazareth MR, Broderick L, Simpson-Abelson MR, Kelleher RJ, Yokota SJ, Bankert RB. Characterization of human lung tumor-associated fibroblasts and their ability to modulate the activation of tumor-associated T cells. J Immunol. 2007;178:5552-5562. [PubMed] |
| 133. | Su X, Ye J, Hsueh EC, Zhang Y, Hoft DF, Peng G. Tumor microenvironments direct the recruitment and expansion of human Th17 cells. J Immunol. 2010;184:1630-1641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 254] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 134. | Barnas JL, Simpson-Abelson MR, Brooks SP, Kelleher RJ, Bankert RB. Reciprocal functional modulation of the activation of T lymphocytes and fibroblasts derived from human solid tumors. J Immunol. 2010;185:2681-2692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 135. | Brown JR, DuBois RN. COX-2: a molecular target for colorectal cancer prevention. J Clin Oncol. 2005;23:2840-2855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 413] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 136. | Balsamo M, Scordamaglia F, Pietra G, Manzini C, Cantoni C, Boitano M, Queirolo P, Vermi W, Facchetti F, Moretta A. Melanoma-associated fibroblasts modulate NK cell phenotype and antitumor cytotoxicity. Proc Natl Acad Sci USA. 2009;106:20847-20852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 276] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 137. | Li T, Yang Y, Hua X, Wang G, Liu W, Jia C, Tai Y, Zhang Q, Chen G. Hepatocellular carcinoma-associated fibroblasts trigger NK cell dysfunction via PGE2 and IDO. Cancer Lett. 2012;318:154-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 295] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 138. | Henry LR, Lee HO, Lee JS, Klein-Szanto A, Watts P, Ross EA, Chen WT, Cheng JD. Clinical implications of fibroblast activation protein in patients with colon cancer. Clin Cancer Res. 2007;13:1736-1741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 284] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 139. | Li T, Yi S, Liu W, Jia C, Wang G, Hua X, Tai Y, Zhang Q, Chen G. Colorectal carcinoma-derived fibroblasts modulate natural killer cell phenotype and antitumor cytotoxicity. Med Oncol. 2013;30:663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 140. | van Zijl F, Mair M, Csiszar A, Schneller D, Zulehner G, Huber H, Eferl R, Beug H, Dolznig H, Mikulits W. Hepatic tumor-stroma crosstalk guides epithelial to mesenchymal transition at the tumor edge. Oncogene. 2009;28:4022-4033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 139] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 141. | Muhanna N, Abu Tair L, Doron S, Amer J, Azzeh M, Mahamid M, Friedman S, Safadi R. Amelioration of hepatic fibrosis by NK cell activation. Gut. 2011;60:90-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 142. | Kuang DM, Peng C, Zhao Q, Wu Y, Chen MS, Zheng L. Activated monocytes in peritumoral stroma of hepatocellular carcinoma promote expansion of memory T helper 17 cells. Hepatology. 2010;51:154-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 216] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 143. | Huijbers A, Tollenaar RA, v Pelt GW, Zeestraten EC, Dutton S, McConkey CC, Domingo E, Smit VT, Midgley R, Warren BF. The proportion of tumor-stroma as a strong prognosticator for stage II and III colon cancer patients: validation in the VICTOR trial. Ann Oncol. 2013;24:179-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 249] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 144. | Ariga N, Sato E, Ohuchi N, Nagura H, Ohtani H. Stromal expression of fibroblast activation protein/seprase, a cell membrane serine proteinase and gelatinase, is associated with longer survival in patients with invasive ductal carcinoma of breast. Int J Cancer. 2001;95:67-72. [PubMed] |
| 145. | Porta C, De Amici M, Quaglini S, Paglino C, Tagliani F, Boncimino A, Moratti R, Corazza GR. Circulating interleukin-6 as a tumor marker for hepatocellular carcinoma. Ann Oncol. 2008;19:353-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 125] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 146. | Gonda TA, Varro A, Wang TC, Tycko B. Molecular biology of cancer-associated fibroblasts: can these cells be targeted in anti-cancer therapy? Semin Cell Dev Biol. 2010;21:2-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 137] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 147. | Cheng JD, Dunbrack RL, Valianou M, Rogatko A, Alpaugh RK, Weiner LM. Promotion of tumor growth by murine fibroblast activation protein, a serine protease, in an animal model. Cancer Res. 2002;62:4767-4772. [PubMed] |
| 148. | Tu G, Xu W, Huang H, Li S. Progress in the development of matrix metalloproteinase inhibitors. Curr Med Chem. 2008;15:1388-1395. [PubMed] |
| 149. | Brahmer JR, Drake CG, Wollner I, Powderly JD, Picus J, Sharfman WH, Stankevich E, Pons A, Salay TM, McMiller TL. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol. 2010;28:3167-3175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2330] [Cited by in RCA: 2415] [Article Influence: 161.0] [Reference Citation Analysis (0)] |